User login
2019 Update on bone health
Prior to last year, this column was titled “Update on osteoporosis.” My observation, however, is that too many ObGyn providers simply measure bone mass (known as bone mineral density, or BMD), label a patient as normal, osteopenic, or osteoporotic, and then consider pharmacotherapy. The FRAX fracture prediction algorithm, which incorporates age, weight, height, history of any previous fracture, family history of hip fracture, current smoking, use of glucocorticoid medications, and any history of rheumatoid arthritis, has refined the screening process somewhat, if and when it is utilized. As clinicians, we should never lose sight of our goal: to prevent fragility fractures. Having osteoporosis increases that risk, but not having osteoporosis does not eliminate it.
In this Update, I highlight various ways in which work published this past year may help us to improve our patients’ bone health and reduce fragility fractures.
Updated ISCD guidance emphasizes appropriate BMD testing, use of the
Z-score, and terminology
International Society for Clinical Densitometry. 2019 ISCD Official Positions-Adult. June 2019. https://www.iscd.org/official-positions/2019-ISCD-official-positions-adult.
Continue to: Indications for BMD testing...
Indications for BMD testing
The ISCD's indications for BMD testing remain for women age 65 and older. For postmenopausal women younger than age 65, a BMD test is indicated if they have a risk factor for low bone mass, such as 1) low body weight, 2) prior fracture, 3) high-risk medication use, or 4) a disease or condition associated with bone loss. A BMD test also is indicated for women during the menopausal transition with clinical risk factors for fracture, such as low body weight, prior fracture, or high-risk medication use. Interestingly, the ISCD recommendation for men is similar but uses age 70 for this group.
In addition, the ISCD recommends BMD testing in adults with a fragility fracture, with a disease or condition associated with low bone mass, or taking medications associated with low bone mass, as well as for anyone being considered for pharmacologic therapy, being treated (to monitor treatment effect), not receiving therapy in whom evidence of bone loss would lead to treatment, and in women discontinuing estrogen who should be considered for BMD testing according to the indications already mentioned.
Sites to assess for osteoporosis. The World Health Organization international reference standard for osteoporosis diagnosis is a T-score of -2.5 or less at the femoral neck. The reference standard, from which the T-score is calculated, is for white women aged 20 to 29 years of age from the database of the Third National Health and Nutrition Examination Survey. Osteoporosis also may be diagnosed in postmenopausal women if the T-score of the lumbar spine, total hip, or femoral neck is -2.5 or less. In certain circumstances, the 33% radius (also called the one-third radius) may be utilized. Other hip regions of interest, including Ward's area and the greater trochanter, should not be used for diagnosis.
The skeletal sites at which to measure BMD include the anteroposterior of the spine and hip in all patients. In terms of the spine, use L1-L4 for spine BMD measurement. However, exclude vertebrae that are affected by local structural changes or artifact. Use 3 vertebrae if 4 cannot be used, and 2 if 3 cannot be used. BMD-based diagnostic classification should not be made using a single vertebra. Anatomically abnormal vertebrae may be excluded from analysis if they are clearly abnormal and nonassessable within the resolution of the system, or if there is more than a 1.0 T-score difference between the vertebra in question and adjacent vertebrae. When vertebrae are excluded, the BMD of the remaining vertebrae are used to derive the T-score.
For BMD measurement at the hip, the femoral neck or total proximal femur—whichever is lowest—should be used. Either hip may be measured. Data are insufficient on whether mean T-scores for bilateral hip BMD should be used for diagnosis.
Terminology. While the ISCD retains the term osteopenia, the term low bone mass or low bone density is preferred. People with low bone mass or density are not necessarily at high fracture risk.
Concerning BMD reporting in women prior to menopause, Z-scores, not T-scores, are preferred. A Z-score of -2.0 or lower is defined as "below the expected range for age"; a Z-score above -2.0 is "within the expected range for age."
Use of serial BMD testing
Finally, regarding serial BMD measurements, such testing in combination with clinical assessment of fracture risk can be used to determine whether treatment should be initiated in untreated patients. Furthermore, serial BMD testing can monitor a patient's response to therapy by finding an increase or stability of bone density. It should be used to monitor individuals following cessation of osteoporosis drug therapy. Serial BMD testing can detect loss of bone density, indicating the need to assess treatment adherence, evaluate possible secondary causes of osteoporosis, and possibly re-evaluate therapeutic options.
Intervals between BMD testing should be determined according to each patient's clinical status. Typically, 1 year after initiating or changing therapy is appropriate, with longer intervals once therapeutic effect is established.
Patients commonly ask for BMD testing and ObGyn providers commonly order it. Understanding appropriate use of BMD testing in terms of who to scan, what sites to evaluate, when there may be spurious results of vertebrae due to artifacts, avoiding T-scores in premenopausal women in favor of Z-scores, understanding that low bone mass is a preferred term to osteopenia, and knowing how to order and use serial BMD testing will likely improve our role as the frontline providers to improving bone health in our patients.
Continue to: Dyspareunia drug has positive effects on bone...
Dyspareunia drug has positive effects on bone
de Villiers TJ, Altomare C, Particco M, et al. Effects of ospemifene on bone in postmenopausal women. Climacteric. 2019;22:442-447.
Previously, ospemifene effectively reduced bone loss in ovariectomized rats, with activity comparable to that of estradiol and raloxifene.3 Clinical data from 3 phase 1 or 2 clinical trials found that ospemifene 60 mg/day had a positive effect on biochemical markers for bone turnover in healthy postmenopausal women, with significant improvements relative to placebo and effects comparable to those of raloxifene.4
Effects on bone formation/resorption biomarkers
In a recent study, de Villiers and colleagues reported the first phase 3 trial that looked at markers of bone formation and bone resorption.5 A total of 316 women were randomly assigned to receive ospemifene, and 315 received placebo.
Demographic and baseline characteristics were similar between treatment groups. Participants' mean age was approximately 60 years, mean body mass index (BMI) was 27.2 kg/m2, and mean duration of VVA was 8 to 9 years. Serum levels of 9 bone biomarkers were similar between groups at baseline.
At week 12, all 5 markers of bone resorption improved with ospemifene treatment, and 3 of the 5 (NTX, CTX, and TRACP-5b) did so in a statistically significant fashion compared with placebo (P≤.02). In addition, at week 12, all 4 markers of bone formation improved with ospemifene treatment compared with placebo (P≤.008). Furthermore, lower bone resorption markers with ospemifene were observed regardless of time since menopause (≤ 5 years or
> 5 years) or baseline BMD, whether normal, osteopenic, or osteoporotic.
Interpret results cautiously
The authors caution that the data are limited to biochemical markers rather than fracture or BMD. It is known that there is good correlation between biochemical markers for bone turnover and the occurrence of fracture.6
Ospemifene is an oral SERM approved for the treatment of moderate to severe dyspareunia as well as dryness from VVA due to menopause. The preclinical animal data and human markers of bone turnover all support the antiresorptive action of ospemifene on bones. Thus, one may safely surmise that ospemifene's direction of activity in bone is virtually indisputable. The magnitude of that activity is, however, unstudied. Therefore, when choosing an agent to treat women with dyspareunia or vaginal dryness from VVA of menopause, determining any potential add-on benefit in bone may be appropriate for that particular patient, although one would not use it as a stand-alone agent for bone only.
Continue to: Sarcopenia adds to osteoporotic risk for fractures...
Sarcopenia adds to osteoporotic risk for fractures
Lima RM, de Oliveira RJ, Raposo R, et al. Stages of sarcopenia, bone mineral density, and the prevalence of osteoporosis in older women. Arch Osteoporos. 2019;14:38.
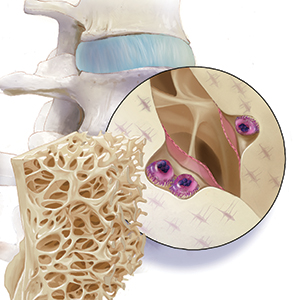
In 1989, the term sarcopenia was introduced to refer to the age-related decline in skeletal muscle mass.8 Currently, sarcopenia is defined as a progressive decline in muscle mass, strength, and physical function, thus increasing the risk for various adverse outcomes, including osteoporosis.9 Although muscle and bone tissues differ morphologically, their functioning is closely interconnected.
The sarcopenia-osteoporosis connection
Lima and colleagues sought to investigate the relationship between sarcopenia and osteoporosis.10 They measured women's fat free mass with dual-energy x-ray absorptiometry (DXA) scanning, muscle strength using a dynamometer to measure knee extension torque while participants were seated, and functional performance using the timed "up and go test" in which participants were timed as they got up from a chair, walked 3 meters around a cone, and returned to sit in the chair.10,11
The authors used definitions from the European Working Group on Sarcopenia in Older People (EWGSOP). Participants who had normal results in all 3 domains were considered nonsarcopenic. Presarcopenia was defined as having low fat free mass on DXA scanning but normal strength and function. Participants who had low fat free mass and either low strength or low function were labeled as having sarcopenia. Severe sarcopenia was defined as abnormal results in all 3 domains.
Two hundred thirty-four women (mean age, 68.3 years; range, 60-80) underwent BMD testing and were evaluated according to the 3 domains of possible sarcopenia. All were community dwelling and did not have cognitive impairment or functional dependency.
The rates of osteoporosis were 15.8%, 19.2%, 35.3%, and 46.2% for nonsarcopenia, presarcopenia, sarcopenia, and severe sarcopenia, respectively (P=.002). Whole-body and femoral neck BMD values were significantly lower among all sarcopenia stages when compared with nonsarcopenia (P<.05). The severe sarcopenia group showed the lowest lumbar spine T-scores (P<.05). When clustered, sarcopenia and severe sarcopenia presented a significantly higher risk for osteoporosis (odds ratio, 3.4; 95% confidence interval [CI], 1.5-7.8).
Consider sarcopenia a risk factor
The authors concluded that these "results provide support for the concept that a dose-response relationship exists between sarcopenia stages, BMD, and the presence of osteoporosis. These findings strengthen the clinical significance of the EWGSOP sarcopenia definitions and indicate that severe sarcopenia should be viewed with attention by healthcare professionals."
Osteoporotic fractures are defined as fragility fractures. While "frailty" has been a risk factor for such fractures in the past, increasing evidence now suggests that what we previously called frailty includes a significant component of loss of muscle mass, strength, and function—referred to as sarcopenia. While it is not likely that many ObGyns will perform objective testing for sarcopenia, conducting even a subjective assessment of such status should be considered in addition to BMD determinations in making decisions about pharmacotherapy.
Continue to: Certain characteristics may offset fracture risk in aromatase inhibitor users...
Certain characteristics may offset fracture risk in aromatase inhibitor users
Leslie WD, Morin SN, Lix LM, et al. Fracture risk in women with breast cancer initiating aromatase inhibitor therapy: a registry-based cohort study. Oncologist. 2019;24:1432-1438.
The use of AIs increases bone turnover and induces bone loss at trabecular-rich bone sites at an average rate of 1% to 3% per year, with reports of up to a threefold increased fracture incidence.13 By contrast, a large nationwide population-based cohort study using US Medicare data identified minimal fracture risk from AI use compared with tamoxifen use (11% higher for nonvertebral fractures, not significantly increased for hip fractures).14
An article published previously in this column reported that women on AIs treated with intravenous zoledronic acid had improvements in BMD, while women treated with denosumab had statistically significant fewer fractures compared with those receiving placebo, whether they had normal bone mass, osteopenia, or osteoporosis at
baseline.15-17
Data derived from a population-based BMD registry
In a recent cohort study, Leslie and colleagues offer the opinion that "observations in the clinical trial setting may differ from routine clinical practice."18 The authors examined fracture outcomes using a large clinical registry of BMD results from women in Manitoba, Canada. They identified women at least 40 years of age initiating AI therapy for breast cancer (n = 1,775), women with breast cancer not receiving AI therapy (n = 1,016), and women from the general population without breast cancer (n = 34,205).
Fracture outcomes were assessed after a mean of 6.2 years for the AI users, all of whom had at least 12 months of AI exposure. At baseline, AI users had higher BMI, higher BMD, lower osteoporosis prevalence, and fewer prior fractures than women from the general population or women with breast cancer without AI use (all P<.001). After adjusting for all covariates, AI users were not at significantly greater risk for major osteoporotic fractures (hazard ratio [HR], 1.15; 95% CI, 0.93-1.42), hip fracture (HR, 0.90; 95% CI, 0.56-1.43), or any fracture (HR, 1.06; 95% CI, 0.88-1.28) compared with the general population.
Results challenge prevailing view
Thus, the authors concluded that higher baseline BMI, BMD, and lower prevalence of prior fracture at baseline may offset the adverse effects of AI exposure. Although confirmatory data from large cohort studies are required, the authors stated that their findings challenge the view that all women with breast cancer initiating AI therapy should be considered at high risk for fracture.
It is well known that women with estrogen receptor-positive breast cancers tend to be more obese than noncancer patients and have higher levels of circulating estrogens. The study by Leslie and colleagues shows that such patients will have fewer previous fractures and better baseline bone mass values than the general population. This may prompt us to rethink whether all women initiating AI therapy need to be treated for fracture prevention, as some previous studies have suggested. Clearly, further study is necessary.
- International Society for Clinical Densitometry. 2019 ISCD Official Positions-Adult. June 2019. https://www.iscd.org/official-positions/2019-iscd-official-positions-adult. Accessed November 22, 2019.
- Goldstein SR, Neven P, Cummings S, et al. Postmenopausal evaluation and risk reduction with lasofoxifene (PEARL) trial: 5-year gynecological outcomes. Menopause. 2011;18:17-22.
- Kangas L, Unkila M. Tissue selectivity of ospemifene: pharmacologic profile and clinical implications. Steroids. 2013;78:1273-1280.
- Constantine GD, Kagan R, Miller PD. Effects of ospemifene on bone parameters including clinical biomarkers in postmenopausal women. Menopause. 2016;23:638-644.
- de Villiers TJ, Altomare C, Particco M, et al. Effects of ospemifene on bone in postmenopausal women. Climacteric. 2019;22:442-447.
- Gerdhem P, Ivaska KK, Alatalo SL, et al. Biochemical markers of bone metabolism and prediction of fracture in elderly women. J Bone Miner Res. 2004;19:386-393.
- Siris ES, Adler R, Bilezikian J, et al. The clinical diagnosis of osteoporosis: a position statement from the National Bone Health Alliance Working Group. Osteoporos Int. 2014;25:1439-1443.
- Epidemiologic and methodologic problems in determining nutritional status of older persons. Proceedings of a conference. Albuquerque, New Mexico, October 19-21, 1988. Am J Clin Nutr. 1989;50(5 suppl):1121-1235.
- Drey M, Sieber CC, Bertsch T, et al. Osteosarcopenia is more than sarcopenia and osteopenia alone. Aging Clin Exp Res. 2016;28:895-899.
- Lima RM, de Oliveira RJ, Raposo R, et al. Stages of sarcopenia, bone mineral density, and the prevalence of osteoporosis in older women. Arch Osteoporos. 2019;14:38.
- Mathias S, Nayak U, Isaacs B. Balance in elderly patients: the "get-up and go" test. Arch Phys Med Rehabil. 1986;67:387-389.
- Burstein HJ, Temin S, Anderson H, et al. Adjuvant endocrine therapy for women with hormone receptor-positive breast cancer: American Society of Clinical Oncology clinical practice guideline focused update. J Clin Oncol. 2014;32:2255-2269.
- Schmidt N, Jacob L, Coleman R, et al. The impact of treatment compliance on fracture risk in women with breast cancer treated with aromatase inhibitors in the United Kingdom. Breast Cancer Res Treat. 2016;155:151-157.
- Neuner JM, Shi Y, Kong AL, et al. Fractures in a nationwide population-based cohort of users of breast cancer hormonal therapy. J Cancer Surviv. 2018;12:268-275.
- Goldstein SR. 2015 Update on osteoporosis. OBG Manag. 2015;27:31-39.
- Majithia N, Atherton PJ, Lafky JM, et al. Zoledronic acid for treatment of osteopenia and osteoporosis in women with primary breast cancer undergoing adjuvant aromatase inhibitor therapy: a 5-year follow-up. Support Care Cancer. 2016;24:1219-1226.
- Gnant M, Pfeiler G, Dubsky PC, et al; Austrian Breast and Colorectal Cancer Study Group. Adjuvant denosumab in breast cancer (ABCSG-18): a multicenter, randomized, double-blind, placebo-controlled trial. Lancet. 2015;386:433-443.
- Leslie WD, Morin SN, Lix LM, et al. Fracture risk in women with breast cancer initiating aromatase inhibitor therapy: a registry-based cohort study. Oncologist. 2019;24:1432-1438.
Prior to last year, this column was titled “Update on osteoporosis.” My observation, however, is that too many ObGyn providers simply measure bone mass (known as bone mineral density, or BMD), label a patient as normal, osteopenic, or osteoporotic, and then consider pharmacotherapy. The FRAX fracture prediction algorithm, which incorporates age, weight, height, history of any previous fracture, family history of hip fracture, current smoking, use of glucocorticoid medications, and any history of rheumatoid arthritis, has refined the screening process somewhat, if and when it is utilized. As clinicians, we should never lose sight of our goal: to prevent fragility fractures. Having osteoporosis increases that risk, but not having osteoporosis does not eliminate it.
In this Update, I highlight various ways in which work published this past year may help us to improve our patients’ bone health and reduce fragility fractures.
Updated ISCD guidance emphasizes appropriate BMD testing, use of the
Z-score, and terminology
International Society for Clinical Densitometry. 2019 ISCD Official Positions-Adult. June 2019. https://www.iscd.org/official-positions/2019-ISCD-official-positions-adult.
Continue to: Indications for BMD testing...
Indications for BMD testing
The ISCD's indications for BMD testing remain for women age 65 and older. For postmenopausal women younger than age 65, a BMD test is indicated if they have a risk factor for low bone mass, such as 1) low body weight, 2) prior fracture, 3) high-risk medication use, or 4) a disease or condition associated with bone loss. A BMD test also is indicated for women during the menopausal transition with clinical risk factors for fracture, such as low body weight, prior fracture, or high-risk medication use. Interestingly, the ISCD recommendation for men is similar but uses age 70 for this group.
In addition, the ISCD recommends BMD testing in adults with a fragility fracture, with a disease or condition associated with low bone mass, or taking medications associated with low bone mass, as well as for anyone being considered for pharmacologic therapy, being treated (to monitor treatment effect), not receiving therapy in whom evidence of bone loss would lead to treatment, and in women discontinuing estrogen who should be considered for BMD testing according to the indications already mentioned.
Sites to assess for osteoporosis. The World Health Organization international reference standard for osteoporosis diagnosis is a T-score of -2.5 or less at the femoral neck. The reference standard, from which the T-score is calculated, is for white women aged 20 to 29 years of age from the database of the Third National Health and Nutrition Examination Survey. Osteoporosis also may be diagnosed in postmenopausal women if the T-score of the lumbar spine, total hip, or femoral neck is -2.5 or less. In certain circumstances, the 33% radius (also called the one-third radius) may be utilized. Other hip regions of interest, including Ward's area and the greater trochanter, should not be used for diagnosis.
The skeletal sites at which to measure BMD include the anteroposterior of the spine and hip in all patients. In terms of the spine, use L1-L4 for spine BMD measurement. However, exclude vertebrae that are affected by local structural changes or artifact. Use 3 vertebrae if 4 cannot be used, and 2 if 3 cannot be used. BMD-based diagnostic classification should not be made using a single vertebra. Anatomically abnormal vertebrae may be excluded from analysis if they are clearly abnormal and nonassessable within the resolution of the system, or if there is more than a 1.0 T-score difference between the vertebra in question and adjacent vertebrae. When vertebrae are excluded, the BMD of the remaining vertebrae are used to derive the T-score.
For BMD measurement at the hip, the femoral neck or total proximal femur—whichever is lowest—should be used. Either hip may be measured. Data are insufficient on whether mean T-scores for bilateral hip BMD should be used for diagnosis.
Terminology. While the ISCD retains the term osteopenia, the term low bone mass or low bone density is preferred. People with low bone mass or density are not necessarily at high fracture risk.
Concerning BMD reporting in women prior to menopause, Z-scores, not T-scores, are preferred. A Z-score of -2.0 or lower is defined as "below the expected range for age"; a Z-score above -2.0 is "within the expected range for age."
Use of serial BMD testing
Finally, regarding serial BMD measurements, such testing in combination with clinical assessment of fracture risk can be used to determine whether treatment should be initiated in untreated patients. Furthermore, serial BMD testing can monitor a patient's response to therapy by finding an increase or stability of bone density. It should be used to monitor individuals following cessation of osteoporosis drug therapy. Serial BMD testing can detect loss of bone density, indicating the need to assess treatment adherence, evaluate possible secondary causes of osteoporosis, and possibly re-evaluate therapeutic options.
Intervals between BMD testing should be determined according to each patient's clinical status. Typically, 1 year after initiating or changing therapy is appropriate, with longer intervals once therapeutic effect is established.
Patients commonly ask for BMD testing and ObGyn providers commonly order it. Understanding appropriate use of BMD testing in terms of who to scan, what sites to evaluate, when there may be spurious results of vertebrae due to artifacts, avoiding T-scores in premenopausal women in favor of Z-scores, understanding that low bone mass is a preferred term to osteopenia, and knowing how to order and use serial BMD testing will likely improve our role as the frontline providers to improving bone health in our patients.
Continue to: Dyspareunia drug has positive effects on bone...
Dyspareunia drug has positive effects on bone
de Villiers TJ, Altomare C, Particco M, et al. Effects of ospemifene on bone in postmenopausal women. Climacteric. 2019;22:442-447.
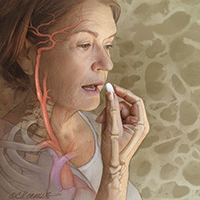
Previously, ospemifene effectively reduced bone loss in ovariectomized rats, with activity comparable to that of estradiol and raloxifene.3 Clinical data from 3 phase 1 or 2 clinical trials found that ospemifene 60 mg/day had a positive effect on biochemical markers for bone turnover in healthy postmenopausal women, with significant improvements relative to placebo and effects comparable to those of raloxifene.4
Effects on bone formation/resorption biomarkers
In a recent study, de Villiers and colleagues reported the first phase 3 trial that looked at markers of bone formation and bone resorption.5 A total of 316 women were randomly assigned to receive ospemifene, and 315 received placebo.
Demographic and baseline characteristics were similar between treatment groups. Participants' mean age was approximately 60 years, mean body mass index (BMI) was 27.2 kg/m2, and mean duration of VVA was 8 to 9 years. Serum levels of 9 bone biomarkers were similar between groups at baseline.
At week 12, all 5 markers of bone resorption improved with ospemifene treatment, and 3 of the 5 (NTX, CTX, and TRACP-5b) did so in a statistically significant fashion compared with placebo (P≤.02). In addition, at week 12, all 4 markers of bone formation improved with ospemifene treatment compared with placebo (P≤.008). Furthermore, lower bone resorption markers with ospemifene were observed regardless of time since menopause (≤ 5 years or
> 5 years) or baseline BMD, whether normal, osteopenic, or osteoporotic.
Interpret results cautiously
The authors caution that the data are limited to biochemical markers rather than fracture or BMD. It is known that there is good correlation between biochemical markers for bone turnover and the occurrence of fracture.6
Ospemifene is an oral SERM approved for the treatment of moderate to severe dyspareunia as well as dryness from VVA due to menopause. The preclinical animal data and human markers of bone turnover all support the antiresorptive action of ospemifene on bones. Thus, one may safely surmise that ospemifene's direction of activity in bone is virtually indisputable. The magnitude of that activity is, however, unstudied. Therefore, when choosing an agent to treat women with dyspareunia or vaginal dryness from VVA of menopause, determining any potential add-on benefit in bone may be appropriate for that particular patient, although one would not use it as a stand-alone agent for bone only.
Continue to: Sarcopenia adds to osteoporotic risk for fractures...
Sarcopenia adds to osteoporotic risk for fractures
Lima RM, de Oliveira RJ, Raposo R, et al. Stages of sarcopenia, bone mineral density, and the prevalence of osteoporosis in older women. Arch Osteoporos. 2019;14:38.
In 1989, the term sarcopenia was introduced to refer to the age-related decline in skeletal muscle mass.8 Currently, sarcopenia is defined as a progressive decline in muscle mass, strength, and physical function, thus increasing the risk for various adverse outcomes, including osteoporosis.9 Although muscle and bone tissues differ morphologically, their functioning is closely interconnected.
The sarcopenia-osteoporosis connection
Lima and colleagues sought to investigate the relationship between sarcopenia and osteoporosis.10 They measured women's fat free mass with dual-energy x-ray absorptiometry (DXA) scanning, muscle strength using a dynamometer to measure knee extension torque while participants were seated, and functional performance using the timed "up and go test" in which participants were timed as they got up from a chair, walked 3 meters around a cone, and returned to sit in the chair.10,11
The authors used definitions from the European Working Group on Sarcopenia in Older People (EWGSOP). Participants who had normal results in all 3 domains were considered nonsarcopenic. Presarcopenia was defined as having low fat free mass on DXA scanning but normal strength and function. Participants who had low fat free mass and either low strength or low function were labeled as having sarcopenia. Severe sarcopenia was defined as abnormal results in all 3 domains.
Two hundred thirty-four women (mean age, 68.3 years; range, 60-80) underwent BMD testing and were evaluated according to the 3 domains of possible sarcopenia. All were community dwelling and did not have cognitive impairment or functional dependency.
The rates of osteoporosis were 15.8%, 19.2%, 35.3%, and 46.2% for nonsarcopenia, presarcopenia, sarcopenia, and severe sarcopenia, respectively (P=.002). Whole-body and femoral neck BMD values were significantly lower among all sarcopenia stages when compared with nonsarcopenia (P<.05). The severe sarcopenia group showed the lowest lumbar spine T-scores (P<.05). When clustered, sarcopenia and severe sarcopenia presented a significantly higher risk for osteoporosis (odds ratio, 3.4; 95% confidence interval [CI], 1.5-7.8).
Consider sarcopenia a risk factor
The authors concluded that these "results provide support for the concept that a dose-response relationship exists between sarcopenia stages, BMD, and the presence of osteoporosis. These findings strengthen the clinical significance of the EWGSOP sarcopenia definitions and indicate that severe sarcopenia should be viewed with attention by healthcare professionals."
Osteoporotic fractures are defined as fragility fractures. While "frailty" has been a risk factor for such fractures in the past, increasing evidence now suggests that what we previously called frailty includes a significant component of loss of muscle mass, strength, and function—referred to as sarcopenia. While it is not likely that many ObGyns will perform objective testing for sarcopenia, conducting even a subjective assessment of such status should be considered in addition to BMD determinations in making decisions about pharmacotherapy.
Continue to: Certain characteristics may offset fracture risk in aromatase inhibitor users...
Certain characteristics may offset fracture risk in aromatase inhibitor users
Leslie WD, Morin SN, Lix LM, et al. Fracture risk in women with breast cancer initiating aromatase inhibitor therapy: a registry-based cohort study. Oncologist. 2019;24:1432-1438.
The use of AIs increases bone turnover and induces bone loss at trabecular-rich bone sites at an average rate of 1% to 3% per year, with reports of up to a threefold increased fracture incidence.13 By contrast, a large nationwide population-based cohort study using US Medicare data identified minimal fracture risk from AI use compared with tamoxifen use (11% higher for nonvertebral fractures, not significantly increased for hip fractures).14
An article published previously in this column reported that women on AIs treated with intravenous zoledronic acid had improvements in BMD, while women treated with denosumab had statistically significant fewer fractures compared with those receiving placebo, whether they had normal bone mass, osteopenia, or osteoporosis at
baseline.15-17
Data derived from a population-based BMD registry
In a recent cohort study, Leslie and colleagues offer the opinion that "observations in the clinical trial setting may differ from routine clinical practice."18 The authors examined fracture outcomes using a large clinical registry of BMD results from women in Manitoba, Canada. They identified women at least 40 years of age initiating AI therapy for breast cancer (n = 1,775), women with breast cancer not receiving AI therapy (n = 1,016), and women from the general population without breast cancer (n = 34,205).
Fracture outcomes were assessed after a mean of 6.2 years for the AI users, all of whom had at least 12 months of AI exposure. At baseline, AI users had higher BMI, higher BMD, lower osteoporosis prevalence, and fewer prior fractures than women from the general population or women with breast cancer without AI use (all P<.001). After adjusting for all covariates, AI users were not at significantly greater risk for major osteoporotic fractures (hazard ratio [HR], 1.15; 95% CI, 0.93-1.42), hip fracture (HR, 0.90; 95% CI, 0.56-1.43), or any fracture (HR, 1.06; 95% CI, 0.88-1.28) compared with the general population.
Results challenge prevailing view
Thus, the authors concluded that higher baseline BMI, BMD, and lower prevalence of prior fracture at baseline may offset the adverse effects of AI exposure. Although confirmatory data from large cohort studies are required, the authors stated that their findings challenge the view that all women with breast cancer initiating AI therapy should be considered at high risk for fracture.
It is well known that women with estrogen receptor-positive breast cancers tend to be more obese than noncancer patients and have higher levels of circulating estrogens. The study by Leslie and colleagues shows that such patients will have fewer previous fractures and better baseline bone mass values than the general population. This may prompt us to rethink whether all women initiating AI therapy need to be treated for fracture prevention, as some previous studies have suggested. Clearly, further study is necessary.
Prior to last year, this column was titled “Update on osteoporosis.” My observation, however, is that too many ObGyn providers simply measure bone mass (known as bone mineral density, or BMD), label a patient as normal, osteopenic, or osteoporotic, and then consider pharmacotherapy. The FRAX fracture prediction algorithm, which incorporates age, weight, height, history of any previous fracture, family history of hip fracture, current smoking, use of glucocorticoid medications, and any history of rheumatoid arthritis, has refined the screening process somewhat, if and when it is utilized. As clinicians, we should never lose sight of our goal: to prevent fragility fractures. Having osteoporosis increases that risk, but not having osteoporosis does not eliminate it.
In this Update, I highlight various ways in which work published this past year may help us to improve our patients’ bone health and reduce fragility fractures.
Updated ISCD guidance emphasizes appropriate BMD testing, use of the
Z-score, and terminology
International Society for Clinical Densitometry. 2019 ISCD Official Positions-Adult. June 2019. https://www.iscd.org/official-positions/2019-ISCD-official-positions-adult.
Continue to: Indications for BMD testing...
Indications for BMD testing
The ISCD's indications for BMD testing remain for women age 65 and older. For postmenopausal women younger than age 65, a BMD test is indicated if they have a risk factor for low bone mass, such as 1) low body weight, 2) prior fracture, 3) high-risk medication use, or 4) a disease or condition associated with bone loss. A BMD test also is indicated for women during the menopausal transition with clinical risk factors for fracture, such as low body weight, prior fracture, or high-risk medication use. Interestingly, the ISCD recommendation for men is similar but uses age 70 for this group.
In addition, the ISCD recommends BMD testing in adults with a fragility fracture, with a disease or condition associated with low bone mass, or taking medications associated with low bone mass, as well as for anyone being considered for pharmacologic therapy, being treated (to monitor treatment effect), not receiving therapy in whom evidence of bone loss would lead to treatment, and in women discontinuing estrogen who should be considered for BMD testing according to the indications already mentioned.
Sites to assess for osteoporosis. The World Health Organization international reference standard for osteoporosis diagnosis is a T-score of -2.5 or less at the femoral neck. The reference standard, from which the T-score is calculated, is for white women aged 20 to 29 years of age from the database of the Third National Health and Nutrition Examination Survey. Osteoporosis also may be diagnosed in postmenopausal women if the T-score of the lumbar spine, total hip, or femoral neck is -2.5 or less. In certain circumstances, the 33% radius (also called the one-third radius) may be utilized. Other hip regions of interest, including Ward's area and the greater trochanter, should not be used for diagnosis.
The skeletal sites at which to measure BMD include the anteroposterior of the spine and hip in all patients. In terms of the spine, use L1-L4 for spine BMD measurement. However, exclude vertebrae that are affected by local structural changes or artifact. Use 3 vertebrae if 4 cannot be used, and 2 if 3 cannot be used. BMD-based diagnostic classification should not be made using a single vertebra. Anatomically abnormal vertebrae may be excluded from analysis if they are clearly abnormal and nonassessable within the resolution of the system, or if there is more than a 1.0 T-score difference between the vertebra in question and adjacent vertebrae. When vertebrae are excluded, the BMD of the remaining vertebrae are used to derive the T-score.
For BMD measurement at the hip, the femoral neck or total proximal femur—whichever is lowest—should be used. Either hip may be measured. Data are insufficient on whether mean T-scores for bilateral hip BMD should be used for diagnosis.
Terminology. While the ISCD retains the term osteopenia, the term low bone mass or low bone density is preferred. People with low bone mass or density are not necessarily at high fracture risk.
Concerning BMD reporting in women prior to menopause, Z-scores, not T-scores, are preferred. A Z-score of -2.0 or lower is defined as "below the expected range for age"; a Z-score above -2.0 is "within the expected range for age."
Use of serial BMD testing
Finally, regarding serial BMD measurements, such testing in combination with clinical assessment of fracture risk can be used to determine whether treatment should be initiated in untreated patients. Furthermore, serial BMD testing can monitor a patient's response to therapy by finding an increase or stability of bone density. It should be used to monitor individuals following cessation of osteoporosis drug therapy. Serial BMD testing can detect loss of bone density, indicating the need to assess treatment adherence, evaluate possible secondary causes of osteoporosis, and possibly re-evaluate therapeutic options.
Intervals between BMD testing should be determined according to each patient's clinical status. Typically, 1 year after initiating or changing therapy is appropriate, with longer intervals once therapeutic effect is established.
Patients commonly ask for BMD testing and ObGyn providers commonly order it. Understanding appropriate use of BMD testing in terms of who to scan, what sites to evaluate, when there may be spurious results of vertebrae due to artifacts, avoiding T-scores in premenopausal women in favor of Z-scores, understanding that low bone mass is a preferred term to osteopenia, and knowing how to order and use serial BMD testing will likely improve our role as the frontline providers to improving bone health in our patients.
Continue to: Dyspareunia drug has positive effects on bone...
Dyspareunia drug has positive effects on bone
de Villiers TJ, Altomare C, Particco M, et al. Effects of ospemifene on bone in postmenopausal women. Climacteric. 2019;22:442-447.
Previously, ospemifene effectively reduced bone loss in ovariectomized rats, with activity comparable to that of estradiol and raloxifene.3 Clinical data from 3 phase 1 or 2 clinical trials found that ospemifene 60 mg/day had a positive effect on biochemical markers for bone turnover in healthy postmenopausal women, with significant improvements relative to placebo and effects comparable to those of raloxifene.4
Effects on bone formation/resorption biomarkers
In a recent study, de Villiers and colleagues reported the first phase 3 trial that looked at markers of bone formation and bone resorption.5 A total of 316 women were randomly assigned to receive ospemifene, and 315 received placebo.
Demographic and baseline characteristics were similar between treatment groups. Participants' mean age was approximately 60 years, mean body mass index (BMI) was 27.2 kg/m2, and mean duration of VVA was 8 to 9 years. Serum levels of 9 bone biomarkers were similar between groups at baseline.
At week 12, all 5 markers of bone resorption improved with ospemifene treatment, and 3 of the 5 (NTX, CTX, and TRACP-5b) did so in a statistically significant fashion compared with placebo (P≤.02). In addition, at week 12, all 4 markers of bone formation improved with ospemifene treatment compared with placebo (P≤.008). Furthermore, lower bone resorption markers with ospemifene were observed regardless of time since menopause (≤ 5 years or
> 5 years) or baseline BMD, whether normal, osteopenic, or osteoporotic.
Interpret results cautiously
The authors caution that the data are limited to biochemical markers rather than fracture or BMD. It is known that there is good correlation between biochemical markers for bone turnover and the occurrence of fracture.6
Ospemifene is an oral SERM approved for the treatment of moderate to severe dyspareunia as well as dryness from VVA due to menopause. The preclinical animal data and human markers of bone turnover all support the antiresorptive action of ospemifene on bones. Thus, one may safely surmise that ospemifene's direction of activity in bone is virtually indisputable. The magnitude of that activity is, however, unstudied. Therefore, when choosing an agent to treat women with dyspareunia or vaginal dryness from VVA of menopause, determining any potential add-on benefit in bone may be appropriate for that particular patient, although one would not use it as a stand-alone agent for bone only.
Continue to: Sarcopenia adds to osteoporotic risk for fractures...
Sarcopenia adds to osteoporotic risk for fractures
Lima RM, de Oliveira RJ, Raposo R, et al. Stages of sarcopenia, bone mineral density, and the prevalence of osteoporosis in older women. Arch Osteoporos. 2019;14:38.
In 1989, the term sarcopenia was introduced to refer to the age-related decline in skeletal muscle mass.8 Currently, sarcopenia is defined as a progressive decline in muscle mass, strength, and physical function, thus increasing the risk for various adverse outcomes, including osteoporosis.9 Although muscle and bone tissues differ morphologically, their functioning is closely interconnected.
The sarcopenia-osteoporosis connection
Lima and colleagues sought to investigate the relationship between sarcopenia and osteoporosis.10 They measured women's fat free mass with dual-energy x-ray absorptiometry (DXA) scanning, muscle strength using a dynamometer to measure knee extension torque while participants were seated, and functional performance using the timed "up and go test" in which participants were timed as they got up from a chair, walked 3 meters around a cone, and returned to sit in the chair.10,11
The authors used definitions from the European Working Group on Sarcopenia in Older People (EWGSOP). Participants who had normal results in all 3 domains were considered nonsarcopenic. Presarcopenia was defined as having low fat free mass on DXA scanning but normal strength and function. Participants who had low fat free mass and either low strength or low function were labeled as having sarcopenia. Severe sarcopenia was defined as abnormal results in all 3 domains.
Two hundred thirty-four women (mean age, 68.3 years; range, 60-80) underwent BMD testing and were evaluated according to the 3 domains of possible sarcopenia. All were community dwelling and did not have cognitive impairment or functional dependency.
The rates of osteoporosis were 15.8%, 19.2%, 35.3%, and 46.2% for nonsarcopenia, presarcopenia, sarcopenia, and severe sarcopenia, respectively (P=.002). Whole-body and femoral neck BMD values were significantly lower among all sarcopenia stages when compared with nonsarcopenia (P<.05). The severe sarcopenia group showed the lowest lumbar spine T-scores (P<.05). When clustered, sarcopenia and severe sarcopenia presented a significantly higher risk for osteoporosis (odds ratio, 3.4; 95% confidence interval [CI], 1.5-7.8).
Consider sarcopenia a risk factor
The authors concluded that these "results provide support for the concept that a dose-response relationship exists between sarcopenia stages, BMD, and the presence of osteoporosis. These findings strengthen the clinical significance of the EWGSOP sarcopenia definitions and indicate that severe sarcopenia should be viewed with attention by healthcare professionals."
Osteoporotic fractures are defined as fragility fractures. While "frailty" has been a risk factor for such fractures in the past, increasing evidence now suggests that what we previously called frailty includes a significant component of loss of muscle mass, strength, and function—referred to as sarcopenia. While it is not likely that many ObGyns will perform objective testing for sarcopenia, conducting even a subjective assessment of such status should be considered in addition to BMD determinations in making decisions about pharmacotherapy.
Continue to: Certain characteristics may offset fracture risk in aromatase inhibitor users...
Certain characteristics may offset fracture risk in aromatase inhibitor users
Leslie WD, Morin SN, Lix LM, et al. Fracture risk in women with breast cancer initiating aromatase inhibitor therapy: a registry-based cohort study. Oncologist. 2019;24:1432-1438.
The use of AIs increases bone turnover and induces bone loss at trabecular-rich bone sites at an average rate of 1% to 3% per year, with reports of up to a threefold increased fracture incidence.13 By contrast, a large nationwide population-based cohort study using US Medicare data identified minimal fracture risk from AI use compared with tamoxifen use (11% higher for nonvertebral fractures, not significantly increased for hip fractures).14
An article published previously in this column reported that women on AIs treated with intravenous zoledronic acid had improvements in BMD, while women treated with denosumab had statistically significant fewer fractures compared with those receiving placebo, whether they had normal bone mass, osteopenia, or osteoporosis at
baseline.15-17
Data derived from a population-based BMD registry
In a recent cohort study, Leslie and colleagues offer the opinion that "observations in the clinical trial setting may differ from routine clinical practice."18 The authors examined fracture outcomes using a large clinical registry of BMD results from women in Manitoba, Canada. They identified women at least 40 years of age initiating AI therapy for breast cancer (n = 1,775), women with breast cancer not receiving AI therapy (n = 1,016), and women from the general population without breast cancer (n = 34,205).
Fracture outcomes were assessed after a mean of 6.2 years for the AI users, all of whom had at least 12 months of AI exposure. At baseline, AI users had higher BMI, higher BMD, lower osteoporosis prevalence, and fewer prior fractures than women from the general population or women with breast cancer without AI use (all P<.001). After adjusting for all covariates, AI users were not at significantly greater risk for major osteoporotic fractures (hazard ratio [HR], 1.15; 95% CI, 0.93-1.42), hip fracture (HR, 0.90; 95% CI, 0.56-1.43), or any fracture (HR, 1.06; 95% CI, 0.88-1.28) compared with the general population.
Results challenge prevailing view
Thus, the authors concluded that higher baseline BMI, BMD, and lower prevalence of prior fracture at baseline may offset the adverse effects of AI exposure. Although confirmatory data from large cohort studies are required, the authors stated that their findings challenge the view that all women with breast cancer initiating AI therapy should be considered at high risk for fracture.
It is well known that women with estrogen receptor-positive breast cancers tend to be more obese than noncancer patients and have higher levels of circulating estrogens. The study by Leslie and colleagues shows that such patients will have fewer previous fractures and better baseline bone mass values than the general population. This may prompt us to rethink whether all women initiating AI therapy need to be treated for fracture prevention, as some previous studies have suggested. Clearly, further study is necessary.
- International Society for Clinical Densitometry. 2019 ISCD Official Positions-Adult. June 2019. https://www.iscd.org/official-positions/2019-iscd-official-positions-adult. Accessed November 22, 2019.
- Goldstein SR, Neven P, Cummings S, et al. Postmenopausal evaluation and risk reduction with lasofoxifene (PEARL) trial: 5-year gynecological outcomes. Menopause. 2011;18:17-22.
- Kangas L, Unkila M. Tissue selectivity of ospemifene: pharmacologic profile and clinical implications. Steroids. 2013;78:1273-1280.
- Constantine GD, Kagan R, Miller PD. Effects of ospemifene on bone parameters including clinical biomarkers in postmenopausal women. Menopause. 2016;23:638-644.
- de Villiers TJ, Altomare C, Particco M, et al. Effects of ospemifene on bone in postmenopausal women. Climacteric. 2019;22:442-447.
- Gerdhem P, Ivaska KK, Alatalo SL, et al. Biochemical markers of bone metabolism and prediction of fracture in elderly women. J Bone Miner Res. 2004;19:386-393.
- Siris ES, Adler R, Bilezikian J, et al. The clinical diagnosis of osteoporosis: a position statement from the National Bone Health Alliance Working Group. Osteoporos Int. 2014;25:1439-1443.
- Epidemiologic and methodologic problems in determining nutritional status of older persons. Proceedings of a conference. Albuquerque, New Mexico, October 19-21, 1988. Am J Clin Nutr. 1989;50(5 suppl):1121-1235.
- Drey M, Sieber CC, Bertsch T, et al. Osteosarcopenia is more than sarcopenia and osteopenia alone. Aging Clin Exp Res. 2016;28:895-899.
- Lima RM, de Oliveira RJ, Raposo R, et al. Stages of sarcopenia, bone mineral density, and the prevalence of osteoporosis in older women. Arch Osteoporos. 2019;14:38.
- Mathias S, Nayak U, Isaacs B. Balance in elderly patients: the "get-up and go" test. Arch Phys Med Rehabil. 1986;67:387-389.
- Burstein HJ, Temin S, Anderson H, et al. Adjuvant endocrine therapy for women with hormone receptor-positive breast cancer: American Society of Clinical Oncology clinical practice guideline focused update. J Clin Oncol. 2014;32:2255-2269.
- Schmidt N, Jacob L, Coleman R, et al. The impact of treatment compliance on fracture risk in women with breast cancer treated with aromatase inhibitors in the United Kingdom. Breast Cancer Res Treat. 2016;155:151-157.
- Neuner JM, Shi Y, Kong AL, et al. Fractures in a nationwide population-based cohort of users of breast cancer hormonal therapy. J Cancer Surviv. 2018;12:268-275.
- Goldstein SR. 2015 Update on osteoporosis. OBG Manag. 2015;27:31-39.
- Majithia N, Atherton PJ, Lafky JM, et al. Zoledronic acid for treatment of osteopenia and osteoporosis in women with primary breast cancer undergoing adjuvant aromatase inhibitor therapy: a 5-year follow-up. Support Care Cancer. 2016;24:1219-1226.
- Gnant M, Pfeiler G, Dubsky PC, et al; Austrian Breast and Colorectal Cancer Study Group. Adjuvant denosumab in breast cancer (ABCSG-18): a multicenter, randomized, double-blind, placebo-controlled trial. Lancet. 2015;386:433-443.
- Leslie WD, Morin SN, Lix LM, et al. Fracture risk in women with breast cancer initiating aromatase inhibitor therapy: a registry-based cohort study. Oncologist. 2019;24:1432-1438.
- International Society for Clinical Densitometry. 2019 ISCD Official Positions-Adult. June 2019. https://www.iscd.org/official-positions/2019-iscd-official-positions-adult. Accessed November 22, 2019.
- Goldstein SR, Neven P, Cummings S, et al. Postmenopausal evaluation and risk reduction with lasofoxifene (PEARL) trial: 5-year gynecological outcomes. Menopause. 2011;18:17-22.
- Kangas L, Unkila M. Tissue selectivity of ospemifene: pharmacologic profile and clinical implications. Steroids. 2013;78:1273-1280.
- Constantine GD, Kagan R, Miller PD. Effects of ospemifene on bone parameters including clinical biomarkers in postmenopausal women. Menopause. 2016;23:638-644.
- de Villiers TJ, Altomare C, Particco M, et al. Effects of ospemifene on bone in postmenopausal women. Climacteric. 2019;22:442-447.
- Gerdhem P, Ivaska KK, Alatalo SL, et al. Biochemical markers of bone metabolism and prediction of fracture in elderly women. J Bone Miner Res. 2004;19:386-393.
- Siris ES, Adler R, Bilezikian J, et al. The clinical diagnosis of osteoporosis: a position statement from the National Bone Health Alliance Working Group. Osteoporos Int. 2014;25:1439-1443.
- Epidemiologic and methodologic problems in determining nutritional status of older persons. Proceedings of a conference. Albuquerque, New Mexico, October 19-21, 1988. Am J Clin Nutr. 1989;50(5 suppl):1121-1235.
- Drey M, Sieber CC, Bertsch T, et al. Osteosarcopenia is more than sarcopenia and osteopenia alone. Aging Clin Exp Res. 2016;28:895-899.
- Lima RM, de Oliveira RJ, Raposo R, et al. Stages of sarcopenia, bone mineral density, and the prevalence of osteoporosis in older women. Arch Osteoporos. 2019;14:38.
- Mathias S, Nayak U, Isaacs B. Balance in elderly patients: the "get-up and go" test. Arch Phys Med Rehabil. 1986;67:387-389.
- Burstein HJ, Temin S, Anderson H, et al. Adjuvant endocrine therapy for women with hormone receptor-positive breast cancer: American Society of Clinical Oncology clinical practice guideline focused update. J Clin Oncol. 2014;32:2255-2269.
- Schmidt N, Jacob L, Coleman R, et al. The impact of treatment compliance on fracture risk in women with breast cancer treated with aromatase inhibitors in the United Kingdom. Breast Cancer Res Treat. 2016;155:151-157.
- Neuner JM, Shi Y, Kong AL, et al. Fractures in a nationwide population-based cohort of users of breast cancer hormonal therapy. J Cancer Surviv. 2018;12:268-275.
- Goldstein SR. 2015 Update on osteoporosis. OBG Manag. 2015;27:31-39.
- Majithia N, Atherton PJ, Lafky JM, et al. Zoledronic acid for treatment of osteopenia and osteoporosis in women with primary breast cancer undergoing adjuvant aromatase inhibitor therapy: a 5-year follow-up. Support Care Cancer. 2016;24:1219-1226.
- Gnant M, Pfeiler G, Dubsky PC, et al; Austrian Breast and Colorectal Cancer Study Group. Adjuvant denosumab in breast cancer (ABCSG-18): a multicenter, randomized, double-blind, placebo-controlled trial. Lancet. 2015;386:433-443.
- Leslie WD, Morin SN, Lix LM, et al. Fracture risk in women with breast cancer initiating aromatase inhibitor therapy: a registry-based cohort study. Oncologist. 2019;24:1432-1438.
2018 Update on bone health
As ObGyns, we are the first-line health care providers for our menopausal patients in terms of identifying, preventing, and initiating treatment for women at risk for fragility fractures. Osteoporosis is probably the most important risk factor for bone health, although sarcopenia, frailty, poor eyesight, and falls also play a significant role in bone health and fragility fracture.
In 2005, more than 2 million incident fractures were reported in the United States, with a total cost of $17 billion.1 By 2025, annual fractures and costs are expected to rise by almost 50%. People who are 65 to 74 years of age will likely experience the largest increase in fracture—greater than 87%.1
Findings from the Women’s Health Initiative study showed that the number of women who had a clinical fracture in 1 year exceeded all the cases of myocardial infarction, stroke, and breast cancer combined.2 Furthermore, the morbidity and mortality rates for fractures are staggering. Thirty percent of women with a hip fracture will be dead within 1 year.3 So, although many patients fear developing breast cancer, and cardiovascular disease remains the number 1 cause of death, the impact of maintaining and protecting bone health cannot be emphasized enough.

_
WHI incidental findings: Hormone-treated menopausal women had decreased hip fracture rate
Manson JE, Aragaki AK, Rossouw JE, et al; WHI Investigators. Menopausal hormone therapy and long-term all-cause and cause-specific mortality: the Women’s Health Initiative randomized trials. JAMA. 2017;318:927-938.
Manson and colleagues examined the total and cause-specific cumulative mortality of the 2 Women’s Health Initiative (WHI) hormone therapy trials. This was an observational follow-up of US multiethnic postmenopausal women aged 50 to 79 years (mean age at baseline, 63.4 years) enrolled in 2 randomized clinical trials between 1993 and 1998 and followed up through December 31, 2014. A total of 27,347 women were randomly assigned to treatment.
Treatment groups
Depending on the presence or absence of a uterus, women received conjugated equine estrogens (CEE, 0.625 mg/d) plus medroxyprogesterone acetate (MPA, 2.5 mg/d) (n = 8,506) or placebo (n = 8,102) for a median of 5.6 years or CEE alone (n = 5,310) versus placebo (n = 5,429) for a median of 7.2 years. All-cause mortality (the primary outcome) and cause-specific mortality (cardiovascular disease mortality, cancer mortality, and other major causes of mortality) were analyzed in the 2 trials pooled and in each trial individually.
All-cause and cause-specific mortality findings
Mortality follow-up was available for more than 98% of participants. During the cumulative 18-year follow-up, 7,489 deaths occurred. In the overall pooled cohort, all-cause mortality in the hormone therapy group was 27.1% compared with 27.6% in the placebo group (hazard ratio [HR], 0.99 [95% confidence interval (CI), 0.94–1.03]). In the CEE plus MPA group, the HR was 1.02 (95% CI, 0.96–1.08). For those in the CEE-alone group, the HR was 0.94 (95% CI, 0.88–1.01).
In the pooled cohort for cardiovascular mortality, the HR was 1.00 (95% CI, 0.92–1.08 [8.9% with hormone therapy vs 9.0% with placebo]). For total cancer mortality, the HR was 1.03 (95% CI, 0.95–1.12 [8.2% with hormone therapy vs 8.0% with placebo]). For other causes, the HR was 0.95 (95% CI, 0.88–1.02 [10.0% with hormone therapy vs 10.7% with placebo]). Results did not differ significantly between trials.
Key takeaway
The study authors concluded that among postmenopausal women, hormone therapy with CEE plus MPA for a median of 5.6 years or with CEE alone for a median of 7.2 years was not associated with risk of all-cause, cardiovascular, or cancer mortality during a cumulative follow-up of 18 years.
Postmenopausal hormone therapy is arguably the most effective “bone drug” available. While all other antiresorptive agents show hip fracture efficacy only in subgroup analyses of the highest-risk patients (women with established osteoporosis, who often already have pre-existing vertebral fractures), the hormone-treated women in the WHI—who were not chosen for having low bone mass (in fact, dual-energy x-ray absorptiometry [DXA] scores were not even recorded)—still had a statistically significant decrease in hip fracture as an adverse event when compared with placebo-treated women. Increasing data on the long-term safety of hormone therapy in menopausal patients will perhaps encourage its greater use from a bone health perspective.
Continue to: Appropriate to defer DXA testing to age 65...
Appropriate to defer DXA testing to age 65 when baseline FRAX score is below treatment level
Gourlay ML, Overman RA, Fine JP, et al; Women’s Health Initiative Investigators. Time to clinically relevant fracture risk scores in postmenopausal women. Am J Med. 2017;130:862.e15-862.e23.
Gourlay ML, Fine JP, Preisser JS, et al; Study of Osteoporotic Fractures Research Group. Bone-density testing interval and transition to osteoporosis in older women. N Engl J Med. 2012;366:225-233.
Many clinicians used to (and still do) order bone mineral density (BMD) testing at 23-month intervals because that was what insurance would allow. Gourlay and colleagues previously published a study on BMD testing intervals and the time it takes to develop osteoporosis. I covered that information in previous Updates.4,5
To recap, Gourlay and colleagues studied 4,957 women, 67 years of age or older, with normal BMD or osteopenia and with no history of hip or clinical vertebral fracture or of treatment for osteoporosis; the women were followed prospectively for up to 15 years. The estimated time for 10% of women to make the transition to osteoporosis was 16.8 years for those with normal BMD, 4.7 years for those with moderate osteopenia, and 1.1 years for women with advanced osteopenia.
Today, FRAX is recommended to assess need for treatment
Older treatment recommendations involved determining various osteopenic BMD levels and the presence or absence of certain risk factors. More recently, the National Osteoporosis Foundation and many medical societies, including the American College of Obstetricians and Gynecologists, have recommended using the FRAX fracture prediction algorithm (available at https://www.sheffield.ac.uk/FRAX/) instead of T-scores to consider initiating pharmacotherapy.
The FRAX calculation tool uses information such as the country where the patient lives, age, sex, height, weight, history of previous fracture, parental fracture, current smoking, glucocorticoid use, rheumatoid arthritis, secondary osteoporosis, alcohol use of 3 or more units per day, and, if available, BMD determination at the femoral neck. It then yields the 10-year absolute risk of hip fracture and any major osteoporotic fracture for that individual or, more precisely, for an individual like that.
In the United States, accepted levels for cost-effective pharmacotherapy are a 10-year absolute risk of hip fracture of 3% or major osteoporotic fracture of 20%.
Continue to: Age also is a key factor in fracture risk assessment
Age also is a key factor in fracture risk assessment
Gourlay and colleagues more recently conducted a retrospective analysis of new occurrence of treatment-level fracture risk scores in postmenopausal women (50 years of age and older) before they received pharmacologic treatment and before they experienced a first hip or clinical vertebral fracture.
In 54,280 postmenopausal women aged 50 to 64 without a BMD test, the time for 10% to develop a treatment-level FRAX score could not be estimated accurately because of the rarity of treatment-level scores. In 6,096 women who had FRAX scores calculated with their BMD score, the estimated time to treatment-level FRAX was 7.6 years for those 65 to 69 and 5.1 years for 75 to 79 year olds. Furthermore, of 17,967 women aged 50 to 64 with a screening-level FRAX at baseline, only 100 (0.6%) experienced a hip or clinical vertebral fracture by age 65.
The investigators concluded that, “Postmenopausal women with sub-threshold fracture risk scores at baseline were unlikely to develop a treatment-level FRAX score between ages 50 and 64 years. After age 65, the increased incidence of treatment-level fracture risk scores, osteoporosis, and major osteoporotic fracture supports more frequent consideration of FRAX and bone mineral density testing.”
Many health care providers begin BMD testing early in menopause. Bone mass results may motivate patients to initiate healthy lifestyle choices, such as adequate dietary calcium, vitamin D supplementation, exercise, moderate alcohol use, smoking cessation, and fall prevention strategies. However, providers and their patients should be aware that if the fracture risk is beneath the threshold score at baseline, the risk of experiencing an osteoporotic fracture prior to age 65 is extremely low, and this should be taken into account before prescribing pharmacotherapy. Furthermore, as stated, FRAX can be performed without a DXA score. When the result is beneath a treatment level in a woman under 65, DXA testing may be deferred until age 65.
Continue to: USPSTF offers updated recommendations for osteoporosis screening
USPSTF offers updated recommendations for osteoporosis screening
US Preventive Services Task Force, Curry SJ, Krist AH, Owens DK, et al. Screening for osteoporosis to prevent fractures: US Preventive Services Task Force recommendation statement. JAMA. 2018;319:2521-2531.
The 2018 updated osteoporosis screening recommendations from the United States Preventative Services Task Force (USPSTF) may seem contradictory to the conclusions of Gourlay and colleagues discussed above. They are not.
The USPSTF authors point out that by 2020, about 12.3 million US individuals older than 50 years are expected to have osteoporosis. Osteoporotic fractures (especially hip fractures) are associated with limitations in ambulation, chronic pain and disability, loss of independence, and decreased quality of life. In fact, 21% to 30% of people who sustain a hip fracture die within 1 year. As the US population continues to age, the potential preventable burden will likely increase.
_
Evidence on bone measurement tests, risk assessment tools, and drug therapy efficacy
The USPSTF conducted an evidence review on screening for and treatment of osteoporotic fractures in women as well as risk assessment tools. The task force found the evidence convincing that bone measurement tests are accurate for detecting osteoporosis and predicting osteoporotic fractures. In addition, there is adequate evidence that clinical risk assessment tools are moderately accurate in identifying risk of osteoporosis and osteoporotic fractures. Furthermore, there is convincing evidence that drug therapies reduce subsequent fracture rates in postmenopausal women.
The USPSTF recommends the following:
- For women aged 65 and older, screen for osteoporosis with bone measurement testing to prevent osteoporotic fractures.
- For women younger than 65 who are at increased risk for osteoporosis based on formal clinical risk assessment tools, screen for osteoporosis with bone measurement testing to prevent osteoporotic fractures.
We all agree that women older than 65 years of age should be screened with DXA measurements of bone mass. The USPSTF says that in women under 65, a fracture assessment tool like FRAX, which does not require bone density testing to yield an individual’s absolute 10-year fracture risk, should be used to determine if bone mass measurement by DXA is, in fact, warranted. This recommendation is further supported by the article by Gourlay and colleagues, in which women aged 50 to 64 with subthreshold FRAX scores had a very low risk of fracture prior to age 65.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Burge R, Dawson-Hughes B, Solomon DH, et al. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005-2025. J Bone Miner Res. 2007;22:465-475.
- Cauley JA, Wampler NS, Barnhart JM, et al; Women’s Health Initiative Observational Study. Incidence of fractures compared to cardiovascular disease and breast cancer: the Women’s Health Initiative Observational Study. Osteoporos Int. 2008;19:1717-1723.
- Brauer CA, Coca-Perraillon M, Cutler DM, et al. Incidence and mortality of hip fractures in the United States. JAMA. 2009;302:1573-1579.
- Goldstein SR. Update on osteoporosis. OBG Manag. 2012;24:16-21.
- Goldstein SR. 2017 update on bone health. OBG Manag. 2017;29-32, 48.
As ObGyns, we are the first-line health care providers for our menopausal patients in terms of identifying, preventing, and initiating treatment for women at risk for fragility fractures. Osteoporosis is probably the most important risk factor for bone health, although sarcopenia, frailty, poor eyesight, and falls also play a significant role in bone health and fragility fracture.
In 2005, more than 2 million incident fractures were reported in the United States, with a total cost of $17 billion.1 By 2025, annual fractures and costs are expected to rise by almost 50%. People who are 65 to 74 years of age will likely experience the largest increase in fracture—greater than 87%.1
Findings from the Women’s Health Initiative study showed that the number of women who had a clinical fracture in 1 year exceeded all the cases of myocardial infarction, stroke, and breast cancer combined.2 Furthermore, the morbidity and mortality rates for fractures are staggering. Thirty percent of women with a hip fracture will be dead within 1 year.3 So, although many patients fear developing breast cancer, and cardiovascular disease remains the number 1 cause of death, the impact of maintaining and protecting bone health cannot be emphasized enough.

_
WHI incidental findings: Hormone-treated menopausal women had decreased hip fracture rate
Manson JE, Aragaki AK, Rossouw JE, et al; WHI Investigators. Menopausal hormone therapy and long-term all-cause and cause-specific mortality: the Women’s Health Initiative randomized trials. JAMA. 2017;318:927-938.
Manson and colleagues examined the total and cause-specific cumulative mortality of the 2 Women’s Health Initiative (WHI) hormone therapy trials. This was an observational follow-up of US multiethnic postmenopausal women aged 50 to 79 years (mean age at baseline, 63.4 years) enrolled in 2 randomized clinical trials between 1993 and 1998 and followed up through December 31, 2014. A total of 27,347 women were randomly assigned to treatment.
Treatment groups
Depending on the presence or absence of a uterus, women received conjugated equine estrogens (CEE, 0.625 mg/d) plus medroxyprogesterone acetate (MPA, 2.5 mg/d) (n = 8,506) or placebo (n = 8,102) for a median of 5.6 years or CEE alone (n = 5,310) versus placebo (n = 5,429) for a median of 7.2 years. All-cause mortality (the primary outcome) and cause-specific mortality (cardiovascular disease mortality, cancer mortality, and other major causes of mortality) were analyzed in the 2 trials pooled and in each trial individually.
All-cause and cause-specific mortality findings
Mortality follow-up was available for more than 98% of participants. During the cumulative 18-year follow-up, 7,489 deaths occurred. In the overall pooled cohort, all-cause mortality in the hormone therapy group was 27.1% compared with 27.6% in the placebo group (hazard ratio [HR], 0.99 [95% confidence interval (CI), 0.94–1.03]). In the CEE plus MPA group, the HR was 1.02 (95% CI, 0.96–1.08). For those in the CEE-alone group, the HR was 0.94 (95% CI, 0.88–1.01).
In the pooled cohort for cardiovascular mortality, the HR was 1.00 (95% CI, 0.92–1.08 [8.9% with hormone therapy vs 9.0% with placebo]). For total cancer mortality, the HR was 1.03 (95% CI, 0.95–1.12 [8.2% with hormone therapy vs 8.0% with placebo]). For other causes, the HR was 0.95 (95% CI, 0.88–1.02 [10.0% with hormone therapy vs 10.7% with placebo]). Results did not differ significantly between trials.
Key takeaway
The study authors concluded that among postmenopausal women, hormone therapy with CEE plus MPA for a median of 5.6 years or with CEE alone for a median of 7.2 years was not associated with risk of all-cause, cardiovascular, or cancer mortality during a cumulative follow-up of 18 years.
Postmenopausal hormone therapy is arguably the most effective “bone drug” available. While all other antiresorptive agents show hip fracture efficacy only in subgroup analyses of the highest-risk patients (women with established osteoporosis, who often already have pre-existing vertebral fractures), the hormone-treated women in the WHI—who were not chosen for having low bone mass (in fact, dual-energy x-ray absorptiometry [DXA] scores were not even recorded)—still had a statistically significant decrease in hip fracture as an adverse event when compared with placebo-treated women. Increasing data on the long-term safety of hormone therapy in menopausal patients will perhaps encourage its greater use from a bone health perspective.
Continue to: Appropriate to defer DXA testing to age 65...
Appropriate to defer DXA testing to age 65 when baseline FRAX score is below treatment level
Gourlay ML, Overman RA, Fine JP, et al; Women’s Health Initiative Investigators. Time to clinically relevant fracture risk scores in postmenopausal women. Am J Med. 2017;130:862.e15-862.e23.
Gourlay ML, Fine JP, Preisser JS, et al; Study of Osteoporotic Fractures Research Group. Bone-density testing interval and transition to osteoporosis in older women. N Engl J Med. 2012;366:225-233.
Many clinicians used to (and still do) order bone mineral density (BMD) testing at 23-month intervals because that was what insurance would allow. Gourlay and colleagues previously published a study on BMD testing intervals and the time it takes to develop osteoporosis. I covered that information in previous Updates.4,5
To recap, Gourlay and colleagues studied 4,957 women, 67 years of age or older, with normal BMD or osteopenia and with no history of hip or clinical vertebral fracture or of treatment for osteoporosis; the women were followed prospectively for up to 15 years. The estimated time for 10% of women to make the transition to osteoporosis was 16.8 years for those with normal BMD, 4.7 years for those with moderate osteopenia, and 1.1 years for women with advanced osteopenia.
Today, FRAX is recommended to assess need for treatment
Older treatment recommendations involved determining various osteopenic BMD levels and the presence or absence of certain risk factors. More recently, the National Osteoporosis Foundation and many medical societies, including the American College of Obstetricians and Gynecologists, have recommended using the FRAX fracture prediction algorithm (available at https://www.sheffield.ac.uk/FRAX/) instead of T-scores to consider initiating pharmacotherapy.
The FRAX calculation tool uses information such as the country where the patient lives, age, sex, height, weight, history of previous fracture, parental fracture, current smoking, glucocorticoid use, rheumatoid arthritis, secondary osteoporosis, alcohol use of 3 or more units per day, and, if available, BMD determination at the femoral neck. It then yields the 10-year absolute risk of hip fracture and any major osteoporotic fracture for that individual or, more precisely, for an individual like that.
In the United States, accepted levels for cost-effective pharmacotherapy are a 10-year absolute risk of hip fracture of 3% or major osteoporotic fracture of 20%.
Continue to: Age also is a key factor in fracture risk assessment
Age also is a key factor in fracture risk assessment
Gourlay and colleagues more recently conducted a retrospective analysis of new occurrence of treatment-level fracture risk scores in postmenopausal women (50 years of age and older) before they received pharmacologic treatment and before they experienced a first hip or clinical vertebral fracture.
In 54,280 postmenopausal women aged 50 to 64 without a BMD test, the time for 10% to develop a treatment-level FRAX score could not be estimated accurately because of the rarity of treatment-level scores. In 6,096 women who had FRAX scores calculated with their BMD score, the estimated time to treatment-level FRAX was 7.6 years for those 65 to 69 and 5.1 years for 75 to 79 year olds. Furthermore, of 17,967 women aged 50 to 64 with a screening-level FRAX at baseline, only 100 (0.6%) experienced a hip or clinical vertebral fracture by age 65.
The investigators concluded that, “Postmenopausal women with sub-threshold fracture risk scores at baseline were unlikely to develop a treatment-level FRAX score between ages 50 and 64 years. After age 65, the increased incidence of treatment-level fracture risk scores, osteoporosis, and major osteoporotic fracture supports more frequent consideration of FRAX and bone mineral density testing.”
Many health care providers begin BMD testing early in menopause. Bone mass results may motivate patients to initiate healthy lifestyle choices, such as adequate dietary calcium, vitamin D supplementation, exercise, moderate alcohol use, smoking cessation, and fall prevention strategies. However, providers and their patients should be aware that if the fracture risk is beneath the threshold score at baseline, the risk of experiencing an osteoporotic fracture prior to age 65 is extremely low, and this should be taken into account before prescribing pharmacotherapy. Furthermore, as stated, FRAX can be performed without a DXA score. When the result is beneath a treatment level in a woman under 65, DXA testing may be deferred until age 65.
Continue to: USPSTF offers updated recommendations for osteoporosis screening
USPSTF offers updated recommendations for osteoporosis screening
US Preventive Services Task Force, Curry SJ, Krist AH, Owens DK, et al. Screening for osteoporosis to prevent fractures: US Preventive Services Task Force recommendation statement. JAMA. 2018;319:2521-2531.
The 2018 updated osteoporosis screening recommendations from the United States Preventative Services Task Force (USPSTF) may seem contradictory to the conclusions of Gourlay and colleagues discussed above. They are not.
The USPSTF authors point out that by 2020, about 12.3 million US individuals older than 50 years are expected to have osteoporosis. Osteoporotic fractures (especially hip fractures) are associated with limitations in ambulation, chronic pain and disability, loss of independence, and decreased quality of life. In fact, 21% to 30% of people who sustain a hip fracture die within 1 year. As the US population continues to age, the potential preventable burden will likely increase.
_
Evidence on bone measurement tests, risk assessment tools, and drug therapy efficacy
The USPSTF conducted an evidence review on screening for and treatment of osteoporotic fractures in women as well as risk assessment tools. The task force found the evidence convincing that bone measurement tests are accurate for detecting osteoporosis and predicting osteoporotic fractures. In addition, there is adequate evidence that clinical risk assessment tools are moderately accurate in identifying risk of osteoporosis and osteoporotic fractures. Furthermore, there is convincing evidence that drug therapies reduce subsequent fracture rates in postmenopausal women.
The USPSTF recommends the following:
- For women aged 65 and older, screen for osteoporosis with bone measurement testing to prevent osteoporotic fractures.
- For women younger than 65 who are at increased risk for osteoporosis based on formal clinical risk assessment tools, screen for osteoporosis with bone measurement testing to prevent osteoporotic fractures.
We all agree that women older than 65 years of age should be screened with DXA measurements of bone mass. The USPSTF says that in women under 65, a fracture assessment tool like FRAX, which does not require bone density testing to yield an individual’s absolute 10-year fracture risk, should be used to determine if bone mass measurement by DXA is, in fact, warranted. This recommendation is further supported by the article by Gourlay and colleagues, in which women aged 50 to 64 with subthreshold FRAX scores had a very low risk of fracture prior to age 65.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
As ObGyns, we are the first-line health care providers for our menopausal patients in terms of identifying, preventing, and initiating treatment for women at risk for fragility fractures. Osteoporosis is probably the most important risk factor for bone health, although sarcopenia, frailty, poor eyesight, and falls also play a significant role in bone health and fragility fracture.
In 2005, more than 2 million incident fractures were reported in the United States, with a total cost of $17 billion.1 By 2025, annual fractures and costs are expected to rise by almost 50%. People who are 65 to 74 years of age will likely experience the largest increase in fracture—greater than 87%.1
Findings from the Women’s Health Initiative study showed that the number of women who had a clinical fracture in 1 year exceeded all the cases of myocardial infarction, stroke, and breast cancer combined.2 Furthermore, the morbidity and mortality rates for fractures are staggering. Thirty percent of women with a hip fracture will be dead within 1 year.3 So, although many patients fear developing breast cancer, and cardiovascular disease remains the number 1 cause of death, the impact of maintaining and protecting bone health cannot be emphasized enough.

_
WHI incidental findings: Hormone-treated menopausal women had decreased hip fracture rate
Manson JE, Aragaki AK, Rossouw JE, et al; WHI Investigators. Menopausal hormone therapy and long-term all-cause and cause-specific mortality: the Women’s Health Initiative randomized trials. JAMA. 2017;318:927-938.
Manson and colleagues examined the total and cause-specific cumulative mortality of the 2 Women’s Health Initiative (WHI) hormone therapy trials. This was an observational follow-up of US multiethnic postmenopausal women aged 50 to 79 years (mean age at baseline, 63.4 years) enrolled in 2 randomized clinical trials between 1993 and 1998 and followed up through December 31, 2014. A total of 27,347 women were randomly assigned to treatment.
Treatment groups
Depending on the presence or absence of a uterus, women received conjugated equine estrogens (CEE, 0.625 mg/d) plus medroxyprogesterone acetate (MPA, 2.5 mg/d) (n = 8,506) or placebo (n = 8,102) for a median of 5.6 years or CEE alone (n = 5,310) versus placebo (n = 5,429) for a median of 7.2 years. All-cause mortality (the primary outcome) and cause-specific mortality (cardiovascular disease mortality, cancer mortality, and other major causes of mortality) were analyzed in the 2 trials pooled and in each trial individually.
All-cause and cause-specific mortality findings
Mortality follow-up was available for more than 98% of participants. During the cumulative 18-year follow-up, 7,489 deaths occurred. In the overall pooled cohort, all-cause mortality in the hormone therapy group was 27.1% compared with 27.6% in the placebo group (hazard ratio [HR], 0.99 [95% confidence interval (CI), 0.94–1.03]). In the CEE plus MPA group, the HR was 1.02 (95% CI, 0.96–1.08). For those in the CEE-alone group, the HR was 0.94 (95% CI, 0.88–1.01).
In the pooled cohort for cardiovascular mortality, the HR was 1.00 (95% CI, 0.92–1.08 [8.9% with hormone therapy vs 9.0% with placebo]). For total cancer mortality, the HR was 1.03 (95% CI, 0.95–1.12 [8.2% with hormone therapy vs 8.0% with placebo]). For other causes, the HR was 0.95 (95% CI, 0.88–1.02 [10.0% with hormone therapy vs 10.7% with placebo]). Results did not differ significantly between trials.
Key takeaway
The study authors concluded that among postmenopausal women, hormone therapy with CEE plus MPA for a median of 5.6 years or with CEE alone for a median of 7.2 years was not associated with risk of all-cause, cardiovascular, or cancer mortality during a cumulative follow-up of 18 years.
Postmenopausal hormone therapy is arguably the most effective “bone drug” available. While all other antiresorptive agents show hip fracture efficacy only in subgroup analyses of the highest-risk patients (women with established osteoporosis, who often already have pre-existing vertebral fractures), the hormone-treated women in the WHI—who were not chosen for having low bone mass (in fact, dual-energy x-ray absorptiometry [DXA] scores were not even recorded)—still had a statistically significant decrease in hip fracture as an adverse event when compared with placebo-treated women. Increasing data on the long-term safety of hormone therapy in menopausal patients will perhaps encourage its greater use from a bone health perspective.
Continue to: Appropriate to defer DXA testing to age 65...
Appropriate to defer DXA testing to age 65 when baseline FRAX score is below treatment level
Gourlay ML, Overman RA, Fine JP, et al; Women’s Health Initiative Investigators. Time to clinically relevant fracture risk scores in postmenopausal women. Am J Med. 2017;130:862.e15-862.e23.
Gourlay ML, Fine JP, Preisser JS, et al; Study of Osteoporotic Fractures Research Group. Bone-density testing interval and transition to osteoporosis in older women. N Engl J Med. 2012;366:225-233.
Many clinicians used to (and still do) order bone mineral density (BMD) testing at 23-month intervals because that was what insurance would allow. Gourlay and colleagues previously published a study on BMD testing intervals and the time it takes to develop osteoporosis. I covered that information in previous Updates.4,5
To recap, Gourlay and colleagues studied 4,957 women, 67 years of age or older, with normal BMD or osteopenia and with no history of hip or clinical vertebral fracture or of treatment for osteoporosis; the women were followed prospectively for up to 15 years. The estimated time for 10% of women to make the transition to osteoporosis was 16.8 years for those with normal BMD, 4.7 years for those with moderate osteopenia, and 1.1 years for women with advanced osteopenia.
Today, FRAX is recommended to assess need for treatment
Older treatment recommendations involved determining various osteopenic BMD levels and the presence or absence of certain risk factors. More recently, the National Osteoporosis Foundation and many medical societies, including the American College of Obstetricians and Gynecologists, have recommended using the FRAX fracture prediction algorithm (available at https://www.sheffield.ac.uk/FRAX/) instead of T-scores to consider initiating pharmacotherapy.
The FRAX calculation tool uses information such as the country where the patient lives, age, sex, height, weight, history of previous fracture, parental fracture, current smoking, glucocorticoid use, rheumatoid arthritis, secondary osteoporosis, alcohol use of 3 or more units per day, and, if available, BMD determination at the femoral neck. It then yields the 10-year absolute risk of hip fracture and any major osteoporotic fracture for that individual or, more precisely, for an individual like that.
In the United States, accepted levels for cost-effective pharmacotherapy are a 10-year absolute risk of hip fracture of 3% or major osteoporotic fracture of 20%.
Continue to: Age also is a key factor in fracture risk assessment
Age also is a key factor in fracture risk assessment
Gourlay and colleagues more recently conducted a retrospective analysis of new occurrence of treatment-level fracture risk scores in postmenopausal women (50 years of age and older) before they received pharmacologic treatment and before they experienced a first hip or clinical vertebral fracture.
In 54,280 postmenopausal women aged 50 to 64 without a BMD test, the time for 10% to develop a treatment-level FRAX score could not be estimated accurately because of the rarity of treatment-level scores. In 6,096 women who had FRAX scores calculated with their BMD score, the estimated time to treatment-level FRAX was 7.6 years for those 65 to 69 and 5.1 years for 75 to 79 year olds. Furthermore, of 17,967 women aged 50 to 64 with a screening-level FRAX at baseline, only 100 (0.6%) experienced a hip or clinical vertebral fracture by age 65.
The investigators concluded that, “Postmenopausal women with sub-threshold fracture risk scores at baseline were unlikely to develop a treatment-level FRAX score between ages 50 and 64 years. After age 65, the increased incidence of treatment-level fracture risk scores, osteoporosis, and major osteoporotic fracture supports more frequent consideration of FRAX and bone mineral density testing.”
Many health care providers begin BMD testing early in menopause. Bone mass results may motivate patients to initiate healthy lifestyle choices, such as adequate dietary calcium, vitamin D supplementation, exercise, moderate alcohol use, smoking cessation, and fall prevention strategies. However, providers and their patients should be aware that if the fracture risk is beneath the threshold score at baseline, the risk of experiencing an osteoporotic fracture prior to age 65 is extremely low, and this should be taken into account before prescribing pharmacotherapy. Furthermore, as stated, FRAX can be performed without a DXA score. When the result is beneath a treatment level in a woman under 65, DXA testing may be deferred until age 65.
Continue to: USPSTF offers updated recommendations for osteoporosis screening
USPSTF offers updated recommendations for osteoporosis screening
US Preventive Services Task Force, Curry SJ, Krist AH, Owens DK, et al. Screening for osteoporosis to prevent fractures: US Preventive Services Task Force recommendation statement. JAMA. 2018;319:2521-2531.
The 2018 updated osteoporosis screening recommendations from the United States Preventative Services Task Force (USPSTF) may seem contradictory to the conclusions of Gourlay and colleagues discussed above. They are not.
The USPSTF authors point out that by 2020, about 12.3 million US individuals older than 50 years are expected to have osteoporosis. Osteoporotic fractures (especially hip fractures) are associated with limitations in ambulation, chronic pain and disability, loss of independence, and decreased quality of life. In fact, 21% to 30% of people who sustain a hip fracture die within 1 year. As the US population continues to age, the potential preventable burden will likely increase.
_
Evidence on bone measurement tests, risk assessment tools, and drug therapy efficacy
The USPSTF conducted an evidence review on screening for and treatment of osteoporotic fractures in women as well as risk assessment tools. The task force found the evidence convincing that bone measurement tests are accurate for detecting osteoporosis and predicting osteoporotic fractures. In addition, there is adequate evidence that clinical risk assessment tools are moderately accurate in identifying risk of osteoporosis and osteoporotic fractures. Furthermore, there is convincing evidence that drug therapies reduce subsequent fracture rates in postmenopausal women.
The USPSTF recommends the following:
- For women aged 65 and older, screen for osteoporosis with bone measurement testing to prevent osteoporotic fractures.
- For women younger than 65 who are at increased risk for osteoporosis based on formal clinical risk assessment tools, screen for osteoporosis with bone measurement testing to prevent osteoporotic fractures.
We all agree that women older than 65 years of age should be screened with DXA measurements of bone mass. The USPSTF says that in women under 65, a fracture assessment tool like FRAX, which does not require bone density testing to yield an individual’s absolute 10-year fracture risk, should be used to determine if bone mass measurement by DXA is, in fact, warranted. This recommendation is further supported by the article by Gourlay and colleagues, in which women aged 50 to 64 with subthreshold FRAX scores had a very low risk of fracture prior to age 65.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Burge R, Dawson-Hughes B, Solomon DH, et al. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005-2025. J Bone Miner Res. 2007;22:465-475.
- Cauley JA, Wampler NS, Barnhart JM, et al; Women’s Health Initiative Observational Study. Incidence of fractures compared to cardiovascular disease and breast cancer: the Women’s Health Initiative Observational Study. Osteoporos Int. 2008;19:1717-1723.
- Brauer CA, Coca-Perraillon M, Cutler DM, et al. Incidence and mortality of hip fractures in the United States. JAMA. 2009;302:1573-1579.
- Goldstein SR. Update on osteoporosis. OBG Manag. 2012;24:16-21.
- Goldstein SR. 2017 update on bone health. OBG Manag. 2017;29-32, 48.
- Burge R, Dawson-Hughes B, Solomon DH, et al. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005-2025. J Bone Miner Res. 2007;22:465-475.
- Cauley JA, Wampler NS, Barnhart JM, et al; Women’s Health Initiative Observational Study. Incidence of fractures compared to cardiovascular disease and breast cancer: the Women’s Health Initiative Observational Study. Osteoporos Int. 2008;19:1717-1723.
- Brauer CA, Coca-Perraillon M, Cutler DM, et al. Incidence and mortality of hip fractures in the United States. JAMA. 2009;302:1573-1579.
- Goldstein SR. Update on osteoporosis. OBG Manag. 2012;24:16-21.
- Goldstein SR. 2017 update on bone health. OBG Manag. 2017;29-32, 48.
2017 Update on bone health
Bone health remains one of the most important health care concerns in the United States today. In 2004, the Surgeon General released a report on bone health and osteoporosis. According to the report’s introduction:
This first-ever Surgeon General’s Report on bone health and osteoporosis illustrates the large burden that bone disease places on our Nation and its citizens. Like other chronic diseases that disproportionately affect the elderly, the prevalence of bone disease and fractures is projected to increase markedly as the population ages. If these predictions come true, bone disease and fractures will have a tremendous negative impact on the future well-being of Americans. But as this report makes clear, they need not come true: by working together we can change the picture of aging in America. Osteoporosis and fractures…no longer should be thought of as an inevitable part of growing old. By focusing on prevention and lifestyle changes, including physical activity and nutrition, as well as early diagnosis and appropriate treatment, Americans can avoid much of the damaging impact of bone disease.1
Related article:
2016 Update on bone health
Although men also experience osteoporosis as they age, in women the rapid loss of bone at menopause makes their disease burden much greater. As women’s health care providers, we stand at the front line for preventing, diagnosing, and treating osteoporosis to reduce the impact of this disease. In this Update I focus on important information that has emerged in the past year.
Read about new ACP guidelines to assess fracture risk
Guidelines for therapy: How to assess fracture risk and when to treat
American College of Obstetricians and Gynecologists Committee on Practice Bulletins--Gynecology. ACOG Practice Bulletin No. 129: Osteoporosis. Obstet Gynecol. 2012;120(3):718-734.
Qaseem A, Forciea MA, McLean RM, Denberg TD; Clinical Guidelines Committee of the American College of Physicians. Treatment of low bone density or osteoporosis to prevent fractures in men and women: a clinical practice guideline update from the American College of Physicians. Ann Intern Med. 2017;166(11):818-839.
A crucial component for good bone health maintenance and osteoporotic fracture prevention is understanding the current guidelines for therapy. The most recent practice bulletin of the American College of Obstetricians and Gynecologists (ACOG) on osteoporosis was published in 2012. ACOG states that treatment be recommended for women who have a bone mineral density (BMD) T-score of -2.5 or lower.
For women in the low bone mass category (T-score between -1 and -2.5), use of the Fracture Risk Assessment Tool (FRAX) calculator can assist in making an informed treatment decision.2 Based on the FRAX calculator, women who have a 10-year risk of major osteoporotic fracture of 20% or greater, or a risk of hip fracture of 3% or greater, are candidates for pharmacologic therapy.
Women who have experienced a low-trauma fracture (especially of the vertebra or hip) also are candidates for treatment, even in the absence of osteoporosis on a dual-energy x-ray absorptiometry (DXA) report.
Related article:
Women’s Preventive Services Initiative Guidelines provide consensus for practicing ObGyns
Updated recommendations from the ACP
The 2017 guideline published by the American College of Physicians (ACP), whose target audience is "all clinicians," recommends that, for women who have known osteoporosis, clinicians offer pharmacologic treatment with alendronate, risedronate, zoledronic acid, or denosumab to reduce the risk for hip and vertebral fractures.
In addition, the ACP recommends that clinicians make the decision whether or not to treat osteopenic women 65 years of age or older who are at a high risk for fracture based on a discussion of patient preferences, fracture risk profile, and benefits, harms, and costs of medications. This may seem somewhat contradictory to ACOG's guidance vis-a-vis women younger than 65 years of age.
The ACP further states that given the limited evidence supporting the benefit of treatment, the balance of benefits and harms in treating osteopenic women is most favorable when the risk for fracture is high. Women younger than 65 years with osteopenia and women older than 65 years with mild osteopenia (T-score between -1.0 and -1.5) will benefit less than women who are 65 years of age or older with severe osteopenia (T-score <-2.0).
Risk factors and risk assessment tools
Clinicians can use their own judgment based on risk factors for fracture (lower body weight, smoking, weight loss, family history of fractures, decreased physical activity, alcohol or caffeine use, low calcium and vitamin D intake, corticosteroid use), or they can use a risk assessment tool. Several risk assessment tools, such as the FRAX calculator mentioned earlier, are available to predict fracture risk among untreated people with low bone density. Although the FRAX calculator is widely used, there is no evidence from randomized controlled trials demonstrating a benefit of fracture reduction when FRAX scores are used in treatment decision making.
Duration of therapy. The ACP recommends that clinicians treat osteoporotic women with pharmacologic therapy for 5 years. Bone density monitoring is not recommended during the 5-year treatment period for osteoporosis in women; current evidence does not show any benefit for bone density monitoring during treatment.
Moderate-quality evidence demonstrated that women treated with antiresorptive therapies (including bisphosphonates, raloxifene, and teriparatide) benefited from reduced fractures, even if no increase in BMD occurred or if BMD decreased.
As before, all women with osteoporosis or a previous low-trauma fracture should be treated. Use of the FRAX calculator should involve clinician judgment, and other risk factors should be taken into account. For most women, treatment should be continued for 5 years. There is no benefit in continued bone mass assessment (DXA testing) while a patient is on pharmacologic therapy.
Read about fracture risk after stopping HT
Another WHI update: No increase in fractures after stopping HT
Watts NB, Cauley JA, Jackson RD, et al; Women's Health Initiative Investigators. No increase in fractures after stopping hormone therapy: results from the Women's Health Initiative. J Clin Endocrinol Metab. 2017;102(1):302-308.
The analysis and reanalysis of the Women's Health Initiative (WHI) trial data seems never-ending, yet the article by Watts and colleagues is important. Although the WHI hormone therapy (HT) trials showed that treatment protects against hip and total fractures, a later observational report suggested loss of benefit and rebound increased risk after HT was discontinued.3 The purpose of the Watts' study was to examine fractures after stopping HT.
Related article:
Did long-term follow-up of WHI participants reveal any mortality increase among women who received HT?
Details of the study
Two placebo-controlled randomized trials served as the study setting. The study included WHI participants (n = 15,187) who continued to take active HT or placebo through the intervention period and who did not take HT in the postintervention period. The trial interventions included conjugated equine estrogen (CEE) plus medroxyprogesterone acetate (MPA) for women with natural menopause and CEE alone for women with prior hysterectomy. The investigators recorded total fractures and hip fractures through 5 years after HT discontinuation.
Findings on fractures. Hip fractures occurred infrequently, with approximately 2.5 per 1,000 person-years. This finding was similar between trials and in former HT users and placebo groups.
No difference was found in total fractures in the CEE plus MPA trial for former HT users compared with former placebo users (28.9 per 1,000 person-years and 29.9 per 1,000 person-years, respectively; hazard ratio [HR], 0.97; 95% confidence interval [CI], 0.87-1.09; P = .63). In the CEE-alone trial, however, total fractures were higher in former placebo users (36.9 per 1,000 person-years) compared with the former active-treatment group (31.1 per 1,000 person-years). This finding suggests a residual benefit of CEE in reducing total fractures (HR, 0.85; 95% CI, 0.73-0.98; P = .03).
Investigators' takeaway. The authors concluded that, after discontinuing HT, there was no evidence of increased fracture risk (sustained or transient) in former HT users compared with former placebo users. In the CEE-alone trial, there was a residual benefit for total fracture reduction in former HT users compared with placebo users.
Gynecologists have long believed that on stopping HT, the loss of bone mass will follow at the same rate as it would at natural menopause. These WHI trials demonstrate, however, that through 5 years, women who stopped HT had no increase in hip or total fractures, and hysterectomized women who stopped estrogen therapy actually had fewer fractures than the placebo group. Keep in mind that this large cohort was not chosen based on risk of osteoporotic fractures. In fact, baseline bone mass was not even measured in these women, making the results even more "real world."
Read about reassessing FRAX scores
A new look at fracture risk assessment scores
Gourlay ML, Overman RA, Fine JP, et al; Women's Health Initiative Investigators. Time to clinically relevant fracture risk scores in postmenopausal women. Am J Med. 2017;130:862.e15-e23.
Jiang X, Gruner M, Trémollieres F, et al. Diagnostic accuracy of FRAX in predicting the 10-year risk of osteoporotic fractures using the USA treatment thresholds: a systematic review and meta-analysis. Bone. 2017;99:20-25.
The FRAX score has become a popular form of triage for women who do not yet meet the bone mass criteria of osteoporosis. Current practice guidelines recommend use of fracture risk scores for screening and pharmacologic therapeutic decision making. Some newer data, however, may give rise to questions about its utility, especially in younger women.
Fracture risk analysis in a large postmenopausal population
Gourlay and colleagues conducted a retrospective competing risk analysis of new occurrence of treatment-level and screening-level fracture risk scores. Study participants were postmenopausal women aged 50 years and older who had not previously received pharmacologic treatment and had not had a first hip or clinical vertebral facture.
Details of the study
In 54,280 postmenopausal women aged 50 to 64 years who did not have a bone mineral density test, the time for 10% to develop a treatment-level FRAX score could not be estimated accurately because the incidence of treatment-level scores was rare.
A total of 6,096 women had FRAX scores calculated with bone mineral density testing. In this group, the estimated unadjusted time to treatment-level FRAX scores was 7.6 years (95% CI, 6.6-8.7) for those aged 65 to 69, and 5.1 years (95% CI, 3.5-7.5) for women aged 75 to 79 at baseline.
Of 17,967 women aged 50 to 64 who had a screening-level FRAX at baseline, 100 (0.6%) experienced a hip or clinical vertebral fracture by age 65 years.
Age is key factor. Gourlay and colleagues concluded that postmenopausal women who had subthreshold fracture risk scores at baseline would be unlikely to develop a treatment-level FRAX score between ages 50 and 64. The increased incidence of treatment-level fracture risk scores, osteoporosis, and major osteoporotic fracture after age 65, however, supports more frequent consideration of FRAX assessment and bone mineral density testing.
Related article:
2015 Update on osteoporosis
Meta-analysis of FRAX tool accuracy
In another study, Jiang and colleagues conducted a systematic review and meta-analysis to determine how the FRAX score performed in predicting the 10-year risk of major osteoporotic fractures and hip fractures. The investigators used the US treatment thresholds.
Details of the study
Seven studies (n = 57,027) were analyzed to assess the diagnostic accuracy of FRAX in predicting major osteoporotic fractures; 20% was used as the 10-year fracture risk threshold for intervention. The mean sensitivity and specificity, along with their 95% CIs, were 10.25% (3.76%-25.06%) and 97.02% (91.17%-99.03%), respectively.
For hip fracture prediction, 6 studies (n = 50,944) were analyzed, and 3% was used as the 10-year fracture risk threshold. The mean sensitivity and specificity, along with their 95% CIs, were 45.70% (24.88%-68.13%) and 84.70% (76.41%-90.44%), respectively.
Predictive value of FRAX. The authors concluded that, using the 10-year intervention thresholds of 20% for major osteoporotic fracture and 3% for hip fracture, FRAX performed better in identifying individuals who will not have a major osteoporotic fracture or hip fracture within 10 years than in identifying those who will experience a fracture. A substantial number of those who developed fractures, especially major osteoporotic fracture within 10 years of follow up, were missed by the baseline FRAX assessment.
Increasing age is still arguably among the most important factors for decreasing bone health. Older women are more likely to develop treatment-level FRAX scores more quickly than younger women. In addition, the FRAX tool is better in predicting which women will not develop a fracture in the next 10 years than in predicting those who will experience a fracture.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- United States Office of the Surgeon General. Bone health and osteoporosis: a report of the Surgeon General. Rockville, Maryland: Office of the Surgeon General (US); 2004. https://www.ncbi.nlm.nih.gov/books/NBK45513/. Accessed November 6, 2017.
- Centre for Metabolic Bone Diseases, University of Sheffield, United Kingdom. FRAX Fracture Risk Assessment Tool website. www.sheffield.ac.uk/FRAX. Accessed November 6, 2017.
- Yates J, Barrett-Connor E, Barlas S, Chen YT, Miller PD, Siris ES. Rapid loss of hip fracture protection after estrogen cessation: evidence from the National Osteoporosis Risk Assessment. Obstet Gynecol. 2004;103(3):440–446.
Bone health remains one of the most important health care concerns in the United States today. In 2004, the Surgeon General released a report on bone health and osteoporosis. According to the report’s introduction:
This first-ever Surgeon General’s Report on bone health and osteoporosis illustrates the large burden that bone disease places on our Nation and its citizens. Like other chronic diseases that disproportionately affect the elderly, the prevalence of bone disease and fractures is projected to increase markedly as the population ages. If these predictions come true, bone disease and fractures will have a tremendous negative impact on the future well-being of Americans. But as this report makes clear, they need not come true: by working together we can change the picture of aging in America. Osteoporosis and fractures…no longer should be thought of as an inevitable part of growing old. By focusing on prevention and lifestyle changes, including physical activity and nutrition, as well as early diagnosis and appropriate treatment, Americans can avoid much of the damaging impact of bone disease.1
Related article:
2016 Update on bone health
Although men also experience osteoporosis as they age, in women the rapid loss of bone at menopause makes their disease burden much greater. As women’s health care providers, we stand at the front line for preventing, diagnosing, and treating osteoporosis to reduce the impact of this disease. In this Update I focus on important information that has emerged in the past year.
Read about new ACP guidelines to assess fracture risk
Guidelines for therapy: How to assess fracture risk and when to treat
American College of Obstetricians and Gynecologists Committee on Practice Bulletins--Gynecology. ACOG Practice Bulletin No. 129: Osteoporosis. Obstet Gynecol. 2012;120(3):718-734.
Qaseem A, Forciea MA, McLean RM, Denberg TD; Clinical Guidelines Committee of the American College of Physicians. Treatment of low bone density or osteoporosis to prevent fractures in men and women: a clinical practice guideline update from the American College of Physicians. Ann Intern Med. 2017;166(11):818-839.
A crucial component for good bone health maintenance and osteoporotic fracture prevention is understanding the current guidelines for therapy. The most recent practice bulletin of the American College of Obstetricians and Gynecologists (ACOG) on osteoporosis was published in 2012. ACOG states that treatment be recommended for women who have a bone mineral density (BMD) T-score of -2.5 or lower.
For women in the low bone mass category (T-score between -1 and -2.5), use of the Fracture Risk Assessment Tool (FRAX) calculator can assist in making an informed treatment decision.2 Based on the FRAX calculator, women who have a 10-year risk of major osteoporotic fracture of 20% or greater, or a risk of hip fracture of 3% or greater, are candidates for pharmacologic therapy.
Women who have experienced a low-trauma fracture (especially of the vertebra or hip) also are candidates for treatment, even in the absence of osteoporosis on a dual-energy x-ray absorptiometry (DXA) report.
Related article:
Women’s Preventive Services Initiative Guidelines provide consensus for practicing ObGyns
Updated recommendations from the ACP
The 2017 guideline published by the American College of Physicians (ACP), whose target audience is "all clinicians," recommends that, for women who have known osteoporosis, clinicians offer pharmacologic treatment with alendronate, risedronate, zoledronic acid, or denosumab to reduce the risk for hip and vertebral fractures.
In addition, the ACP recommends that clinicians make the decision whether or not to treat osteopenic women 65 years of age or older who are at a high risk for fracture based on a discussion of patient preferences, fracture risk profile, and benefits, harms, and costs of medications. This may seem somewhat contradictory to ACOG's guidance vis-a-vis women younger than 65 years of age.
The ACP further states that given the limited evidence supporting the benefit of treatment, the balance of benefits and harms in treating osteopenic women is most favorable when the risk for fracture is high. Women younger than 65 years with osteopenia and women older than 65 years with mild osteopenia (T-score between -1.0 and -1.5) will benefit less than women who are 65 years of age or older with severe osteopenia (T-score <-2.0).
Risk factors and risk assessment tools
Clinicians can use their own judgment based on risk factors for fracture (lower body weight, smoking, weight loss, family history of fractures, decreased physical activity, alcohol or caffeine use, low calcium and vitamin D intake, corticosteroid use), or they can use a risk assessment tool. Several risk assessment tools, such as the FRAX calculator mentioned earlier, are available to predict fracture risk among untreated people with low bone density. Although the FRAX calculator is widely used, there is no evidence from randomized controlled trials demonstrating a benefit of fracture reduction when FRAX scores are used in treatment decision making.
Duration of therapy. The ACP recommends that clinicians treat osteoporotic women with pharmacologic therapy for 5 years. Bone density monitoring is not recommended during the 5-year treatment period for osteoporosis in women; current evidence does not show any benefit for bone density monitoring during treatment.
Moderate-quality evidence demonstrated that women treated with antiresorptive therapies (including bisphosphonates, raloxifene, and teriparatide) benefited from reduced fractures, even if no increase in BMD occurred or if BMD decreased.
As before, all women with osteoporosis or a previous low-trauma fracture should be treated. Use of the FRAX calculator should involve clinician judgment, and other risk factors should be taken into account. For most women, treatment should be continued for 5 years. There is no benefit in continued bone mass assessment (DXA testing) while a patient is on pharmacologic therapy.
Read about fracture risk after stopping HT
Another WHI update: No increase in fractures after stopping HT
Watts NB, Cauley JA, Jackson RD, et al; Women's Health Initiative Investigators. No increase in fractures after stopping hormone therapy: results from the Women's Health Initiative. J Clin Endocrinol Metab. 2017;102(1):302-308.
The analysis and reanalysis of the Women's Health Initiative (WHI) trial data seems never-ending, yet the article by Watts and colleagues is important. Although the WHI hormone therapy (HT) trials showed that treatment protects against hip and total fractures, a later observational report suggested loss of benefit and rebound increased risk after HT was discontinued.3 The purpose of the Watts' study was to examine fractures after stopping HT.
Related article:
Did long-term follow-up of WHI participants reveal any mortality increase among women who received HT?
Details of the study
Two placebo-controlled randomized trials served as the study setting. The study included WHI participants (n = 15,187) who continued to take active HT or placebo through the intervention period and who did not take HT in the postintervention period. The trial interventions included conjugated equine estrogen (CEE) plus medroxyprogesterone acetate (MPA) for women with natural menopause and CEE alone for women with prior hysterectomy. The investigators recorded total fractures and hip fractures through 5 years after HT discontinuation.
Findings on fractures. Hip fractures occurred infrequently, with approximately 2.5 per 1,000 person-years. This finding was similar between trials and in former HT users and placebo groups.
No difference was found in total fractures in the CEE plus MPA trial for former HT users compared with former placebo users (28.9 per 1,000 person-years and 29.9 per 1,000 person-years, respectively; hazard ratio [HR], 0.97; 95% confidence interval [CI], 0.87-1.09; P = .63). In the CEE-alone trial, however, total fractures were higher in former placebo users (36.9 per 1,000 person-years) compared with the former active-treatment group (31.1 per 1,000 person-years). This finding suggests a residual benefit of CEE in reducing total fractures (HR, 0.85; 95% CI, 0.73-0.98; P = .03).
Investigators' takeaway. The authors concluded that, after discontinuing HT, there was no evidence of increased fracture risk (sustained or transient) in former HT users compared with former placebo users. In the CEE-alone trial, there was a residual benefit for total fracture reduction in former HT users compared with placebo users.
Gynecologists have long believed that on stopping HT, the loss of bone mass will follow at the same rate as it would at natural menopause. These WHI trials demonstrate, however, that through 5 years, women who stopped HT had no increase in hip or total fractures, and hysterectomized women who stopped estrogen therapy actually had fewer fractures than the placebo group. Keep in mind that this large cohort was not chosen based on risk of osteoporotic fractures. In fact, baseline bone mass was not even measured in these women, making the results even more "real world."
Read about reassessing FRAX scores
A new look at fracture risk assessment scores
Gourlay ML, Overman RA, Fine JP, et al; Women's Health Initiative Investigators. Time to clinically relevant fracture risk scores in postmenopausal women. Am J Med. 2017;130:862.e15-e23.
Jiang X, Gruner M, Trémollieres F, et al. Diagnostic accuracy of FRAX in predicting the 10-year risk of osteoporotic fractures using the USA treatment thresholds: a systematic review and meta-analysis. Bone. 2017;99:20-25.
The FRAX score has become a popular form of triage for women who do not yet meet the bone mass criteria of osteoporosis. Current practice guidelines recommend use of fracture risk scores for screening and pharmacologic therapeutic decision making. Some newer data, however, may give rise to questions about its utility, especially in younger women.
Fracture risk analysis in a large postmenopausal population
Gourlay and colleagues conducted a retrospective competing risk analysis of new occurrence of treatment-level and screening-level fracture risk scores. Study participants were postmenopausal women aged 50 years and older who had not previously received pharmacologic treatment and had not had a first hip or clinical vertebral facture.
Details of the study
In 54,280 postmenopausal women aged 50 to 64 years who did not have a bone mineral density test, the time for 10% to develop a treatment-level FRAX score could not be estimated accurately because the incidence of treatment-level scores was rare.
A total of 6,096 women had FRAX scores calculated with bone mineral density testing. In this group, the estimated unadjusted time to treatment-level FRAX scores was 7.6 years (95% CI, 6.6-8.7) for those aged 65 to 69, and 5.1 years (95% CI, 3.5-7.5) for women aged 75 to 79 at baseline.
Of 17,967 women aged 50 to 64 who had a screening-level FRAX at baseline, 100 (0.6%) experienced a hip or clinical vertebral fracture by age 65 years.
Age is key factor. Gourlay and colleagues concluded that postmenopausal women who had subthreshold fracture risk scores at baseline would be unlikely to develop a treatment-level FRAX score between ages 50 and 64. The increased incidence of treatment-level fracture risk scores, osteoporosis, and major osteoporotic fracture after age 65, however, supports more frequent consideration of FRAX assessment and bone mineral density testing.
Related article:
2015 Update on osteoporosis
Meta-analysis of FRAX tool accuracy
In another study, Jiang and colleagues conducted a systematic review and meta-analysis to determine how the FRAX score performed in predicting the 10-year risk of major osteoporotic fractures and hip fractures. The investigators used the US treatment thresholds.
Details of the study
Seven studies (n = 57,027) were analyzed to assess the diagnostic accuracy of FRAX in predicting major osteoporotic fractures; 20% was used as the 10-year fracture risk threshold for intervention. The mean sensitivity and specificity, along with their 95% CIs, were 10.25% (3.76%-25.06%) and 97.02% (91.17%-99.03%), respectively.
For hip fracture prediction, 6 studies (n = 50,944) were analyzed, and 3% was used as the 10-year fracture risk threshold. The mean sensitivity and specificity, along with their 95% CIs, were 45.70% (24.88%-68.13%) and 84.70% (76.41%-90.44%), respectively.
Predictive value of FRAX. The authors concluded that, using the 10-year intervention thresholds of 20% for major osteoporotic fracture and 3% for hip fracture, FRAX performed better in identifying individuals who will not have a major osteoporotic fracture or hip fracture within 10 years than in identifying those who will experience a fracture. A substantial number of those who developed fractures, especially major osteoporotic fracture within 10 years of follow up, were missed by the baseline FRAX assessment.
Increasing age is still arguably among the most important factors for decreasing bone health. Older women are more likely to develop treatment-level FRAX scores more quickly than younger women. In addition, the FRAX tool is better in predicting which women will not develop a fracture in the next 10 years than in predicting those who will experience a fracture.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Bone health remains one of the most important health care concerns in the United States today. In 2004, the Surgeon General released a report on bone health and osteoporosis. According to the report’s introduction:
This first-ever Surgeon General’s Report on bone health and osteoporosis illustrates the large burden that bone disease places on our Nation and its citizens. Like other chronic diseases that disproportionately affect the elderly, the prevalence of bone disease and fractures is projected to increase markedly as the population ages. If these predictions come true, bone disease and fractures will have a tremendous negative impact on the future well-being of Americans. But as this report makes clear, they need not come true: by working together we can change the picture of aging in America. Osteoporosis and fractures…no longer should be thought of as an inevitable part of growing old. By focusing on prevention and lifestyle changes, including physical activity and nutrition, as well as early diagnosis and appropriate treatment, Americans can avoid much of the damaging impact of bone disease.1
Related article:
2016 Update on bone health
Although men also experience osteoporosis as they age, in women the rapid loss of bone at menopause makes their disease burden much greater. As women’s health care providers, we stand at the front line for preventing, diagnosing, and treating osteoporosis to reduce the impact of this disease. In this Update I focus on important information that has emerged in the past year.
Read about new ACP guidelines to assess fracture risk
Guidelines for therapy: How to assess fracture risk and when to treat
American College of Obstetricians and Gynecologists Committee on Practice Bulletins--Gynecology. ACOG Practice Bulletin No. 129: Osteoporosis. Obstet Gynecol. 2012;120(3):718-734.
Qaseem A, Forciea MA, McLean RM, Denberg TD; Clinical Guidelines Committee of the American College of Physicians. Treatment of low bone density or osteoporosis to prevent fractures in men and women: a clinical practice guideline update from the American College of Physicians. Ann Intern Med. 2017;166(11):818-839.
A crucial component for good bone health maintenance and osteoporotic fracture prevention is understanding the current guidelines for therapy. The most recent practice bulletin of the American College of Obstetricians and Gynecologists (ACOG) on osteoporosis was published in 2012. ACOG states that treatment be recommended for women who have a bone mineral density (BMD) T-score of -2.5 or lower.
For women in the low bone mass category (T-score between -1 and -2.5), use of the Fracture Risk Assessment Tool (FRAX) calculator can assist in making an informed treatment decision.2 Based on the FRAX calculator, women who have a 10-year risk of major osteoporotic fracture of 20% or greater, or a risk of hip fracture of 3% or greater, are candidates for pharmacologic therapy.
Women who have experienced a low-trauma fracture (especially of the vertebra or hip) also are candidates for treatment, even in the absence of osteoporosis on a dual-energy x-ray absorptiometry (DXA) report.
Related article:
Women’s Preventive Services Initiative Guidelines provide consensus for practicing ObGyns
Updated recommendations from the ACP
The 2017 guideline published by the American College of Physicians (ACP), whose target audience is "all clinicians," recommends that, for women who have known osteoporosis, clinicians offer pharmacologic treatment with alendronate, risedronate, zoledronic acid, or denosumab to reduce the risk for hip and vertebral fractures.
In addition, the ACP recommends that clinicians make the decision whether or not to treat osteopenic women 65 years of age or older who are at a high risk for fracture based on a discussion of patient preferences, fracture risk profile, and benefits, harms, and costs of medications. This may seem somewhat contradictory to ACOG's guidance vis-a-vis women younger than 65 years of age.
The ACP further states that given the limited evidence supporting the benefit of treatment, the balance of benefits and harms in treating osteopenic women is most favorable when the risk for fracture is high. Women younger than 65 years with osteopenia and women older than 65 years with mild osteopenia (T-score between -1.0 and -1.5) will benefit less than women who are 65 years of age or older with severe osteopenia (T-score <-2.0).
Risk factors and risk assessment tools
Clinicians can use their own judgment based on risk factors for fracture (lower body weight, smoking, weight loss, family history of fractures, decreased physical activity, alcohol or caffeine use, low calcium and vitamin D intake, corticosteroid use), or they can use a risk assessment tool. Several risk assessment tools, such as the FRAX calculator mentioned earlier, are available to predict fracture risk among untreated people with low bone density. Although the FRAX calculator is widely used, there is no evidence from randomized controlled trials demonstrating a benefit of fracture reduction when FRAX scores are used in treatment decision making.
Duration of therapy. The ACP recommends that clinicians treat osteoporotic women with pharmacologic therapy for 5 years. Bone density monitoring is not recommended during the 5-year treatment period for osteoporosis in women; current evidence does not show any benefit for bone density monitoring during treatment.
Moderate-quality evidence demonstrated that women treated with antiresorptive therapies (including bisphosphonates, raloxifene, and teriparatide) benefited from reduced fractures, even if no increase in BMD occurred or if BMD decreased.
As before, all women with osteoporosis or a previous low-trauma fracture should be treated. Use of the FRAX calculator should involve clinician judgment, and other risk factors should be taken into account. For most women, treatment should be continued for 5 years. There is no benefit in continued bone mass assessment (DXA testing) while a patient is on pharmacologic therapy.
Read about fracture risk after stopping HT
Another WHI update: No increase in fractures after stopping HT
Watts NB, Cauley JA, Jackson RD, et al; Women's Health Initiative Investigators. No increase in fractures after stopping hormone therapy: results from the Women's Health Initiative. J Clin Endocrinol Metab. 2017;102(1):302-308.
The analysis and reanalysis of the Women's Health Initiative (WHI) trial data seems never-ending, yet the article by Watts and colleagues is important. Although the WHI hormone therapy (HT) trials showed that treatment protects against hip and total fractures, a later observational report suggested loss of benefit and rebound increased risk after HT was discontinued.3 The purpose of the Watts' study was to examine fractures after stopping HT.
Related article:
Did long-term follow-up of WHI participants reveal any mortality increase among women who received HT?
Details of the study
Two placebo-controlled randomized trials served as the study setting. The study included WHI participants (n = 15,187) who continued to take active HT or placebo through the intervention period and who did not take HT in the postintervention period. The trial interventions included conjugated equine estrogen (CEE) plus medroxyprogesterone acetate (MPA) for women with natural menopause and CEE alone for women with prior hysterectomy. The investigators recorded total fractures and hip fractures through 5 years after HT discontinuation.
Findings on fractures. Hip fractures occurred infrequently, with approximately 2.5 per 1,000 person-years. This finding was similar between trials and in former HT users and placebo groups.
No difference was found in total fractures in the CEE plus MPA trial for former HT users compared with former placebo users (28.9 per 1,000 person-years and 29.9 per 1,000 person-years, respectively; hazard ratio [HR], 0.97; 95% confidence interval [CI], 0.87-1.09; P = .63). In the CEE-alone trial, however, total fractures were higher in former placebo users (36.9 per 1,000 person-years) compared with the former active-treatment group (31.1 per 1,000 person-years). This finding suggests a residual benefit of CEE in reducing total fractures (HR, 0.85; 95% CI, 0.73-0.98; P = .03).
Investigators' takeaway. The authors concluded that, after discontinuing HT, there was no evidence of increased fracture risk (sustained or transient) in former HT users compared with former placebo users. In the CEE-alone trial, there was a residual benefit for total fracture reduction in former HT users compared with placebo users.
Gynecologists have long believed that on stopping HT, the loss of bone mass will follow at the same rate as it would at natural menopause. These WHI trials demonstrate, however, that through 5 years, women who stopped HT had no increase in hip or total fractures, and hysterectomized women who stopped estrogen therapy actually had fewer fractures than the placebo group. Keep in mind that this large cohort was not chosen based on risk of osteoporotic fractures. In fact, baseline bone mass was not even measured in these women, making the results even more "real world."
Read about reassessing FRAX scores
A new look at fracture risk assessment scores
Gourlay ML, Overman RA, Fine JP, et al; Women's Health Initiative Investigators. Time to clinically relevant fracture risk scores in postmenopausal women. Am J Med. 2017;130:862.e15-e23.
Jiang X, Gruner M, Trémollieres F, et al. Diagnostic accuracy of FRAX in predicting the 10-year risk of osteoporotic fractures using the USA treatment thresholds: a systematic review and meta-analysis. Bone. 2017;99:20-25.
The FRAX score has become a popular form of triage for women who do not yet meet the bone mass criteria of osteoporosis. Current practice guidelines recommend use of fracture risk scores for screening and pharmacologic therapeutic decision making. Some newer data, however, may give rise to questions about its utility, especially in younger women.
Fracture risk analysis in a large postmenopausal population
Gourlay and colleagues conducted a retrospective competing risk analysis of new occurrence of treatment-level and screening-level fracture risk scores. Study participants were postmenopausal women aged 50 years and older who had not previously received pharmacologic treatment and had not had a first hip or clinical vertebral facture.
Details of the study
In 54,280 postmenopausal women aged 50 to 64 years who did not have a bone mineral density test, the time for 10% to develop a treatment-level FRAX score could not be estimated accurately because the incidence of treatment-level scores was rare.
A total of 6,096 women had FRAX scores calculated with bone mineral density testing. In this group, the estimated unadjusted time to treatment-level FRAX scores was 7.6 years (95% CI, 6.6-8.7) for those aged 65 to 69, and 5.1 years (95% CI, 3.5-7.5) for women aged 75 to 79 at baseline.
Of 17,967 women aged 50 to 64 who had a screening-level FRAX at baseline, 100 (0.6%) experienced a hip or clinical vertebral fracture by age 65 years.
Age is key factor. Gourlay and colleagues concluded that postmenopausal women who had subthreshold fracture risk scores at baseline would be unlikely to develop a treatment-level FRAX score between ages 50 and 64. The increased incidence of treatment-level fracture risk scores, osteoporosis, and major osteoporotic fracture after age 65, however, supports more frequent consideration of FRAX assessment and bone mineral density testing.
Related article:
2015 Update on osteoporosis
Meta-analysis of FRAX tool accuracy
In another study, Jiang and colleagues conducted a systematic review and meta-analysis to determine how the FRAX score performed in predicting the 10-year risk of major osteoporotic fractures and hip fractures. The investigators used the US treatment thresholds.
Details of the study
Seven studies (n = 57,027) were analyzed to assess the diagnostic accuracy of FRAX in predicting major osteoporotic fractures; 20% was used as the 10-year fracture risk threshold for intervention. The mean sensitivity and specificity, along with their 95% CIs, were 10.25% (3.76%-25.06%) and 97.02% (91.17%-99.03%), respectively.
For hip fracture prediction, 6 studies (n = 50,944) were analyzed, and 3% was used as the 10-year fracture risk threshold. The mean sensitivity and specificity, along with their 95% CIs, were 45.70% (24.88%-68.13%) and 84.70% (76.41%-90.44%), respectively.
Predictive value of FRAX. The authors concluded that, using the 10-year intervention thresholds of 20% for major osteoporotic fracture and 3% for hip fracture, FRAX performed better in identifying individuals who will not have a major osteoporotic fracture or hip fracture within 10 years than in identifying those who will experience a fracture. A substantial number of those who developed fractures, especially major osteoporotic fracture within 10 years of follow up, were missed by the baseline FRAX assessment.
Increasing age is still arguably among the most important factors for decreasing bone health. Older women are more likely to develop treatment-level FRAX scores more quickly than younger women. In addition, the FRAX tool is better in predicting which women will not develop a fracture in the next 10 years than in predicting those who will experience a fracture.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- United States Office of the Surgeon General. Bone health and osteoporosis: a report of the Surgeon General. Rockville, Maryland: Office of the Surgeon General (US); 2004. https://www.ncbi.nlm.nih.gov/books/NBK45513/. Accessed November 6, 2017.
- Centre for Metabolic Bone Diseases, University of Sheffield, United Kingdom. FRAX Fracture Risk Assessment Tool website. www.sheffield.ac.uk/FRAX. Accessed November 6, 2017.
- Yates J, Barrett-Connor E, Barlas S, Chen YT, Miller PD, Siris ES. Rapid loss of hip fracture protection after estrogen cessation: evidence from the National Osteoporosis Risk Assessment. Obstet Gynecol. 2004;103(3):440–446.
- United States Office of the Surgeon General. Bone health and osteoporosis: a report of the Surgeon General. Rockville, Maryland: Office of the Surgeon General (US); 2004. https://www.ncbi.nlm.nih.gov/books/NBK45513/. Accessed November 6, 2017.
- Centre for Metabolic Bone Diseases, University of Sheffield, United Kingdom. FRAX Fracture Risk Assessment Tool website. www.sheffield.ac.uk/FRAX. Accessed November 6, 2017.
- Yates J, Barrett-Connor E, Barlas S, Chen YT, Miller PD, Siris ES. Rapid loss of hip fracture protection after estrogen cessation: evidence from the National Osteoporosis Risk Assessment. Obstet Gynecol. 2004;103(3):440–446.
2016 Update on bone health
Prioritize bone health, as osteoporotic fracture is a major source of morbidity and mortality among women. In this article: fracture risk with OC use in perimenopause, data that inform calcium’s role in cardiovascular disease, sarcopenia management, and an emerging treatment.
Most women’s health care providers are aware of recent changes and controversies regarding cervical cancer screening, mammography frequency, and whether a pelvic bimanual exam should be part of our annual well woman evaluation.1 However, I believe one of the most important things we as clinicians can do is be frontline in promoting bone health. Osteoporotic fracture is a major source of morbidity and mortality.2,3 Thus, promoting the maintenance of bone health is a priority in my own practice. It is also one of my many academic interests.
What follows is an update on bone health. In past years, this update has been entitled, “Update on osteoporosis,” but what we are trying to accomplish is fracture reduction. Thus, priorities for bone health consist of recognition of risk, lifestyle and dietary counseling, as well as the use of pharmacologic agents when appropriate. Certain research stands out as informative for your practice:
- a recent study on the risk of fracture with oral contraceptive (OC) use in perimenopause
- 3 just-published studies that inform our understanding of calcium’s role in cardiovascular health
- a review on sarcopenia management
- new data on romosozumab.
Oral contraceptive use in perimenopause
Scholes D, LaCroix AZ, Hubbard RA, et al. Oral contraceptive use and fracture risk around the menopausal transition. Menopause. 2016;23(2):166-174.
The use of OCs in women of older reproductive age has increased ever since the cutoff age of 35 years was eliminated.4 Lower doses have continued to be utilized in these "older" women with excellent control of irregular bleeding due to ovulatory dysfunction (and reduction in psychosocial symptoms as well).5
The effect of OC use on risk of fracture remains unclear, and use during later reproductive life may be increasing. To determine the association between OC use during later reproductive life and risk of fracture across the menopausal transition, Scholes and colleagues conducted a population-based case-controlled study in a Pacific Northwest HMO, Group Health Cooperative.
Details of the study
Scholes and colleagues enrolled 1,204 case women aged 45 to 59 years with incident fractures, and 2,275 control women. Potential cases with fracture codes in automated data were adjudicated by electronic health record review. Potential control women without fracture codes were selected concurrently, sampling based on age. Participants received a structured study interview. Using logistic regression, associations between OC use and fracture risk were calculated as odds ratios (ORs) and 95% confidence intervals (CIs).
Participation was 69% for cases and 64% for controls. The study sample was 82% white; mean age was 54 years. The most common fracture site for cases was the wrist/forearm (32%). Adjusted fracture risk did not differ between cases and controls for OC use:
- in the 10 years before menopause (OR, 0.90; 95% CI, 0.74-1.11)
- after age 38 years (OR, 0.94; 95% CI, 0.78-1.14)
- over the duration, or
- for other OC exposures.
Related article:
2016 Update on female sexual dysfunction
Association between fractures and OC use near menopause
The current study does not show an association between fractures near the menopausal transition and OC use in the decade before menopause or after age 38 years. For women considering OC use at these times, fracture risk does not seem to be either reduced or increased.
These results, looking at fracture, seem to be further supported by trials conducted by Gambacciani and colleagues,6 in which researchers randomly assigned irregularly cycling perimenopausal women (aged 40-49 years) to 20 μg ethinyl estradiol OCs or calcium/placebo. Results showed that this low-dose OC use significantly increased bone density at the femoral neck, spine, and other sites relative to control women after 24 months.
In the current Scholes study, the use of OCs in the decade before menopause or after age 38 did not reduce fracture risk in the years around the time of menopause. It is reassuring that their use was not associated with any increased fracture risk.
These findings provide additional clarity and guidance to women and their clinicians at a time of increasing public health concern about fractures. For women who may choose to use OCs during late premenopause (around age 38-48 years), fracture risk around the menopausal transition will not differ from women not choosing this option.
Calcium and calcium supplements: The data continue to grow
Anderson JJ, Kruszka B, Delaney JA, et al. Calcium intake from diet and supplements and the risk of coronary artery calcification and its progression among older adults: 10-year follow-up of the Multi-Ethnic Study of Atherosclerosis (MESA) [published online ahead of print October 11, 2016]. J Am Heart Assoc. pii: e003815.
Billington EO, Bristow SM, Gamble GD, et al. Acute effects of calcium supplements on blood pressure: randomised, crossover trial in postmenopausal women [published online ahead of print August 20, 2016]. Osteoporos Int. doi:10.1007/s00198-016-3744-y.
Crandall CJ, Aragaki AK, LeBoff MS, et al. Calcium plus vitamin D supplementation and height loss: findings from the Women's Health Initiative Calcium and Vitamin D clinical trial [published online ahead of print August 1, 2016]. Menopause. doi:10.1097 /GME.0000000000000704.
In 2001, a National Institutes of Health (NIH) Consensus Development Panel on osteoporosis concluded that calcium intake is crucial to maintain bone mass and should be maintained at 1,000-1,500 mg/day in older adults. The panel acknowledged that the majority of older adults did not meet the recommended intake from dietary sources alone, and therefore would require calcium supplementation. Calcium supplements are one of the most commonly used dietary supplements, and population-based surveys have shown that they are used by the majority of older men and women in the United States.7
More recently results from large randomized controlled trials (RCTs) of calcium supplements have been reported, leading to concerns about calcium efficacy for fracture risk and safety. Bolland and colleagues8 reported that calcium supplements increased the rate of cardiovascular events in healthy older women and suggested that their role in osteoporosis management be reconsidered. More recently, the US Preventive Services Task Force recommended against calcium supplements for the primary prevention of fractures in noninstitutionalized postmenopausal women.9
The association between calcium intake and CVD events
Anderson and colleagues acknowledged that recent randomized data suggest that calcium supplements may be associated with increased risk of cardiovascular disease (CVD) events. Using a longitudinal cohort study, they assessed the association between calcium intake, from both foods and supplements, and atherosclerosis, as measured by coronary artery calcification (CAC).
Details of the study by Anderson and colleagues
The authors studied 5,448 adults free of clinically diagnosed CVD (52% female; age range, 45-84 years) from the Multi-Ethnic Study of Atherosclerosis. Baseline total calcium intake was assessed from diet (using a food frequency questionnaire) and calcium supplements (by a medication inventory) and categorized into quintiles based on overall population distribution. Baseline CAC was measured by computed tomography (CT) scan, and CAC measurements were repeated in 2,742 participants approximately 10 years later. Women had higher calcium intakes than men.
After adjustment for potential confounders, among 1,567 participants without baseline CAC, the relative risk (RR) of developing incident CAC over 10 years, by quintile 1 to 5 of calcium intake is included in the TABLE. After accounting for total calcium intake, calcium supplement use was associated with increased risk for incident CAC (RR, 1.22; 95% CI, 1.07-1.39). No relation was found between baseline calcium intake and 10-year changes in CAC among those participants with baseline CAC less than zero.
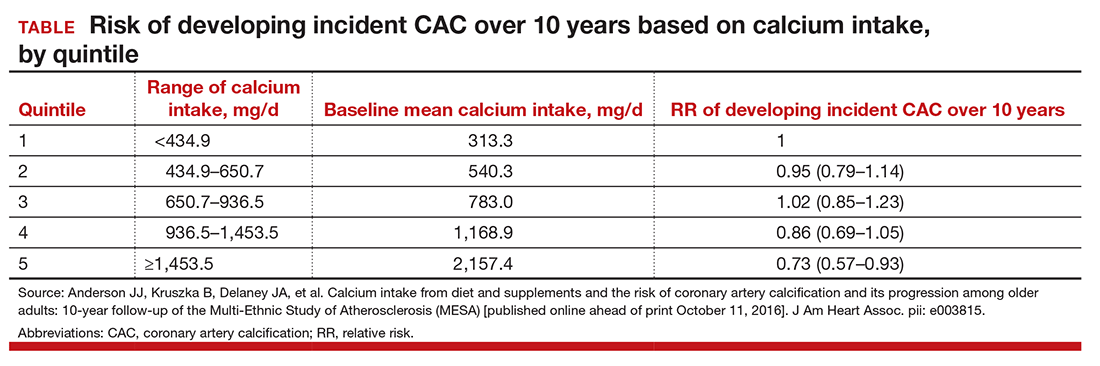
They concluded that high total calcium intake was associated with a decreased risk of incident atherosclerosis over long-term follow-up, particularly if achieved without supplement use. However, calcium supplement use may increase the risk for incident CAC.
Related article:
Does the discontinuation of menopausal hormone therapy affect a woman’s cardiovascular risk?
Calcium supplements and blood pressure
Billington and colleagues acknowledged that calcium supplements appear to increase cardiovascular risk but that the mechanism is unknown. They had previously reported that blood pressure declines over the course of the day in older women.10
Details of the study by Billington and colleagues
In this new study the investigators examined the acute effects of calcium supplements on blood pressure in a randomized controlled crossover trial in 40 healthy postmenopausal women (mean age, 71 years; body mass index [BMI], 27.2 kg/m2). Women attended on 2 occasions, with visits separated by 7 or more days. At each visit, they received either 1 g of calcium as citrate or placebo. Blood pressure and serum calcium concentrations were measured immediately before and 2, 4, and 6 hours after each intervention.
Ionized and total calcium concentrations increased after calcium (P<.0001 vs placebo). Systolic blood pressure (SBP) measurements decreased after both calcium and placebo but significantly less so after calcium (P=.02). The reduction in SBP from baseline was smaller after calcium compared with placebo by 6 mm Hg at 4 hours (P=.036) and by 9 mm Hg at 6 hours (P=.002). The reduction in diastolic blood pressure was similar after calcium and placebo.
These findings indicate that the use of calcium supplements in postmenopausal women attenuates the postbreakfast reduction in SBP by 6 to 9 mm Hg. Whether these changes in blood pressure influence cardiovascular risk requires further study.
Association between calcium, vitamin D, and height loss
Crandall and colleagues looked at the association between calcium and vitamin D supplementation and height loss in 36,282 participants of the Women's Health Initiative Calcium and Vitamin D trial.
Details of the study by Crandall and colleagues
The authors performed a post hoc analysis of data from a double-blind randomized controlled trial of 1,000 mg of elemental calcium as calcium carbonate with 400 IU of vitamin D3 daily (CaD) or placebo in postmenopausal women at 40 US clinical centers. Height was measured annually (mean follow-up, 5.9 years) with a stadiometer.
Average height loss was 1.28 mm/yr among participants assigned to CaD, versus 1.26 mm/yr for women assigned to placebo (P=.35). A strong association (P<.001) was observed between age group and height loss. The study authors concluded that, compared with placebo, calcium and vitamin D supplementation used in this trial did not prevent height loss in healthy postmenopausal women.
Adequate calcium is necessary for bone health. While calcium supplementation may not be adequate to prevent fractures, it is also not involved in the inevitable loss of overall height seen in postmenopausal women. Calcium supplementation has been implicated in an increase in CVD. These data seem to indicate that, while calcium supplementation results in higher systolic blood pressure during the day, as well as higher coronary artery calcium scores, greater dietary calcium actually may decrease the incidence of atherosclerosis.
Sarcopenia: Still important, clinical approaches to easily detect it
Beaudart C, McCloskey E, Bruyére O, et al. Sarcopenia in daily practice: assessment and management. BMC Geriatr. 2016;16(1):170.
In last year's update, I reviewed the article by He and colleagues11 on the relationship between sarcopenia and body composition with osteoporosis. Sarcopenia, which is the age-related loss of muscle mass and strength, is important to address in patients. Body composition and muscle strength are directly correlated with bone density, and this is not surprising since bone and muscle share some common hormonal, genetic, nutritional, and lifestyle determinants.12,13 Sarcopenia can be diagnosed via dual-energy x-ray absorptiometry (DXA) scan looking at lean muscle mass.
The term sarcopenia was first coined by Rosenberg and colleagues in 198914 as a progressive loss of skeletal muscle mass with advancing age. Since then, the definition has expanded to incorporate the notion of impaired muscle strength or physical performance. Sarcopenia is associated with morbidity and mortality from linked physical disability, falls, fractures, poor quality of life, depression, and hospitalization.15
Current research is focusing on nutritional exercise/activity-based and other novel interventions for improving the quality and quantity of skeletal muscle in older people. Some studies demonstrated that resistance training combined with nutritional supplements can improve muscle function.16
Details of the study
Beaudart and colleagues propose some user-friendly and inexpensive methods that can be utilized to assess sarcopenia in real life settings. They acknowledge that in research settings or even specialist clinical settings, DXA or computed tomography (CT) scans are the best assessment of muscle mass.
Anthropometric measurements. In a primary care setting, anthropometric measurement, especially calf circumference and mid-upper arm muscle circumference, correlate with overall muscle mass and reflect both health and nutritional status and predict performance, health, and survival in older people.
However, with advancing age, changes in the distribution of fat and loss of skin elasticity are such that circumference incurs a loss of accuracy and precision in older people. Some studies suggest that an adjustment of anthropometric measurements for age, sex, or BMI results in a better correlation with DXA-measured lean mass.17 Anthropometric measurements are simple clinical prediction tools that can be easily applied for sarcopenia since they offer the most portable, commonly applicable, inexpensive, and noninvasive technique for assessing size, proportions, and composition of the human body. However, their validity is limited when applied to individuals because cutoff points to identify low muscle mass still need to be defined. Still, serial measurements in a patient over time may be valuable.
Related article:
2014 Update on osteoporosis
Handgrip strength, as measured with a dynamometer, appears to be the most widely used method for the measurement of muscle strength. In general, isometric handgrip strength shows a good correlation with leg strength and also with lower extremity power, and calf cross-sectional muscle area. The measurement is easy to perform, inexpensive and does not require a specialist-trained staff.
Standardized conditions for the test include seating the patient in a standard chair with her forearms resting flat on the chair arms. Clinicians should demonstrate the use of the dynamometer and show that gripping very tightly registers the best score. Six measurements should be taken, 3 with each arm. Ideally, patients should be encouraged to squeeze as hard and tightly as possible during 3 to 5 seconds for each of the 6 trials; usually the highest reading of the 6 measurements is reported as the final result. The Jamar dynamometer, or similar hydraulic dynamometer, is the gold standard for this measurement.
Gait speed measurement. The most widely used tool in clinical practice for the assessment of physical performance is the gait speed measurement. The test is highly acceptable for participants and health professionals in clinical settings. No special equipment is required; it needs only a flat floor devoid of obstacles. In the 4-meter gait speed test, men and women with a gait speed of less than 0.8 meters/sec are described as having a poor physical performance. The average extra time added to the consultation by measuring the 4-meter gait speed was only 95 seconds (SD, 20 seconds).
Loss of muscle mass correlates with loss of bone mass as our patients age. In addition, such sarcopenia increases the risk of falls, a significant component of the rising rate of fragility fractures. Anthropometric measures, grip strength, and gait speed are easy, low-cost measures that can identify patients at increased risk.
Romosozumab: An interesting new agent to look forward to
Cosman F, Crittenden DB, Adachi JD, et al. Romosozumab treatment in postmenopausal women with osteoporosis. N Engl J Med. 2016;375(16):1532-1543.
Romosozumab is a monoclonal antibody that binds sclerostin, increasing bone formation and decreasing bone resorption. Cosman and colleagues enrolled 7,180 postmenopausal women with a T score of -2.5 to -3.5 at the total hip or femoral neck. Participants were randomly assigned to receive subcutaneous injections of romosozumab 210 mg or placebo monthly for 12 months. Thereafter, women in each group received subcutaneous denosumab 60 mg for 12 months--administered every 6 months. The coprimary end points were the cumulative incidences of new vertebral fractures at 12 and 24 months. Secondary end points included clinical and nonvertebral fractures.
Details of the study
At 12 months, new vertebral fractures had occurred in 16 of 3,321 women (0.5%) in the romosozumab group, as compared with 59 of 3,322 (1.8%) in the placebo group (representing a 73% lower risk of fracture with romosozumab; P<.001). Clinical fractures had occurred in 58 of 3,589 women (1.6%) in the romosozumab group, as compared with 90 of 3,591 (2.5%) in the placebo group (a 36% lower fracture risk with romosozumab; P = .008). Nonvertebral fractures had occurred in 56 of 3,589 women (1.6%) in the romosozumab group and in 75 of 3,591 (2.1%) in the placebo group (P = .10).
At 24 months, the rates of vertebral fractures were significantly lower in the romosozumab group than in the placebo group after each group made the transition to denosumab (0.6% [21 of 3,325 women] in the romosozumab group vs 2.5% [84 of 3,327 women] in the placebo group, a 75% lower risk with romosozumab; P<.001). Adverse events, including cardiovascular events, osteoarthritis, and cancer, appeared to be balanced between the groups. One atypical femoral fracture and 2 cases of osteonecrosis of the jaw were observed in the romosozumab group.
Lower risk of fracture
Thus, in postmenopausal women with osteoporosis, romosozumab was associated with a lower risk of vertebral fracture than placebo at 12 months and, after the transition to denosumab, at 24 months. The lower risk of clinical fracture that was seen with romosozumab was evident at 1 year.
Of note, the effect of romosozumab on the risk of vertebral fracture was rapid, with only 2 additional vertebral fractures (of a total of 16 such fractures in the romosozumab group) occurring in the second 6 months of the first year of therapy. Because vertebral and clinical fractures are associated with increased morbidity and considerable health care costs, a treatment that would reduce this risk rapidly could offer appropriate patients an important benefit.
Romosozumab is a new agent. Though not yet available, it is extremely interesting because it not only decreases bone resorption but also increases bone formation. The results of this large prospective trial show that such an agent reduces both vertebral and clinical fracture and reduces that fracture risk quite rapidly within the first 6 months of therapy.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- MacLaughlin KL, Faubion SS, Long ME, Pruthi S, Casey PM. Should the annual pelvic examination go the way of annual cervical cytology? Womens Health (Lond). 2014;10(4):373–384.
- Wright NC, Looker AC, Saag KG, et al. The recent prevalence of osteoporosis and low bone mass in the United States based on bone mineral density at the femoral neck or lumbar spine. J Bone Miner Res. 2014;29(11):2520–2526.
- Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King AB, Tosterson A. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J Bone Miner Res. 2007;22(3):465–475.
- Kaunitz AM. Hormonal contraception in women of older reproductive age. N Engl J Med. 2008;358:1262–1270.
- Kaunitz AM. Oral contraceptive use in perimenopause. Am J Obstet Gynecol. 2001;185(2 suppl):S32–S37.
- Gambacciani M, Cappagli B, Lazzarini V, Ciaponi M, Fruzzetti F, Genazzani AR. Longitudinal evaluation of perimenopausal bone loss: effects of different low dose oral contraceptive preparations on bone mineral density. Maturitas. 2006;54(2):176–180.
- Bailey R, Dodd K, Goldman J, et al. Estimation of total usual calcium and vitamin D intakes in the United States. J Nutr. 2010;140(4):817–822.
- Bolland MJ, Grey A, Reid IR. Calcium supplements and cardiovascular risk: 5 years on. Ther Adv Drug Saf. 2013;4(5):199–210.
- Moyer VA; U.S. Preventive Services Task Force. Vitamin D and calcium supplementation to prevent fractures in adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2013;158(9):691–696.
- Bristow SM, Gamble GD, Stewart A, Horne AM, Reid IR. Acute effects of calcium supplements on blood pressure and blood coagulation: secondary analysis of a randomised controlled trial in post-menopausal women. Br J Nutr. 2015;114(11):1868–1874.
- He H, Liu Y, Tian Q, Papasian CJ, Hu T, Deng HW. Relationship of sarcopenia and body composition with osteoporosis. Osteoporos Int. 2016;27(2):473–482.
- Coin A, Perissinotto E, Enzi G, et al. Predictors of low bone mineral density in the elderly: the role of dietary intake, nutritional status and sarcopenia. Eur J Clin Nutr. 2008;62(6):802–809.
- Taaffe DR, Cauley JA, Danielson M, et al. Race and sex effects on the association between muscle strength, soft tissue, and bone mineral density in healthy elders: the Health, Aging, and Body Composition Study. J Bone Miner Res. 2001;16(7):1343–1352.
- Rosenberg IH. Sarcopenia: origins and clinical relevance. J Nutr. 1997;127(5 suppl):990S–991S.
- Beaudart C, Rizzoli R, Bruyere O, Reginster JY, Biver E. Sarcopenia: Burden and challenges for Public Health. Arch Public Health. 2014;72(1):45.
- Cruz-Jentoft AJ, Landi F, Schneider SM, et al. Prevalence of and interventions for sarcopenia in ageing adults: a systematic review. Report of the International Sarcopenia Initiative (EWGSOP and IWGS). Age Ageing. 2014;43(6):748–759.
- Kulkarni B, Kuper H, Taylor A, et al. Development and validation of anthropometric prediction equations for estimation of lean body mass and appendicular lean soft tissue in Indian men and women. J Appl Physiol. 2013;115(8):1156–1162.
Prioritize bone health, as osteoporotic fracture is a major source of morbidity and mortality among women. In this article: fracture risk with OC use in perimenopause, data that inform calcium’s role in cardiovascular disease, sarcopenia management, and an emerging treatment.
Most women’s health care providers are aware of recent changes and controversies regarding cervical cancer screening, mammography frequency, and whether a pelvic bimanual exam should be part of our annual well woman evaluation.1 However, I believe one of the most important things we as clinicians can do is be frontline in promoting bone health. Osteoporotic fracture is a major source of morbidity and mortality.2,3 Thus, promoting the maintenance of bone health is a priority in my own practice. It is also one of my many academic interests.
What follows is an update on bone health. In past years, this update has been entitled, “Update on osteoporosis,” but what we are trying to accomplish is fracture reduction. Thus, priorities for bone health consist of recognition of risk, lifestyle and dietary counseling, as well as the use of pharmacologic agents when appropriate. Certain research stands out as informative for your practice:
- a recent study on the risk of fracture with oral contraceptive (OC) use in perimenopause
- 3 just-published studies that inform our understanding of calcium’s role in cardiovascular health
- a review on sarcopenia management
- new data on romosozumab.
Oral contraceptive use in perimenopause
Scholes D, LaCroix AZ, Hubbard RA, et al. Oral contraceptive use and fracture risk around the menopausal transition. Menopause. 2016;23(2):166-174.
The use of OCs in women of older reproductive age has increased ever since the cutoff age of 35 years was eliminated.4 Lower doses have continued to be utilized in these "older" women with excellent control of irregular bleeding due to ovulatory dysfunction (and reduction in psychosocial symptoms as well).5
The effect of OC use on risk of fracture remains unclear, and use during later reproductive life may be increasing. To determine the association between OC use during later reproductive life and risk of fracture across the menopausal transition, Scholes and colleagues conducted a population-based case-controlled study in a Pacific Northwest HMO, Group Health Cooperative.
Details of the study
Scholes and colleagues enrolled 1,204 case women aged 45 to 59 years with incident fractures, and 2,275 control women. Potential cases with fracture codes in automated data were adjudicated by electronic health record review. Potential control women without fracture codes were selected concurrently, sampling based on age. Participants received a structured study interview. Using logistic regression, associations between OC use and fracture risk were calculated as odds ratios (ORs) and 95% confidence intervals (CIs).
Participation was 69% for cases and 64% for controls. The study sample was 82% white; mean age was 54 years. The most common fracture site for cases was the wrist/forearm (32%). Adjusted fracture risk did not differ between cases and controls for OC use:
- in the 10 years before menopause (OR, 0.90; 95% CI, 0.74-1.11)
- after age 38 years (OR, 0.94; 95% CI, 0.78-1.14)
- over the duration, or
- for other OC exposures.
Related article:
2016 Update on female sexual dysfunction
Association between fractures and OC use near menopause
The current study does not show an association between fractures near the menopausal transition and OC use in the decade before menopause or after age 38 years. For women considering OC use at these times, fracture risk does not seem to be either reduced or increased.
These results, looking at fracture, seem to be further supported by trials conducted by Gambacciani and colleagues,6 in which researchers randomly assigned irregularly cycling perimenopausal women (aged 40-49 years) to 20 μg ethinyl estradiol OCs or calcium/placebo. Results showed that this low-dose OC use significantly increased bone density at the femoral neck, spine, and other sites relative to control women after 24 months.
In the current Scholes study, the use of OCs in the decade before menopause or after age 38 did not reduce fracture risk in the years around the time of menopause. It is reassuring that their use was not associated with any increased fracture risk.
These findings provide additional clarity and guidance to women and their clinicians at a time of increasing public health concern about fractures. For women who may choose to use OCs during late premenopause (around age 38-48 years), fracture risk around the menopausal transition will not differ from women not choosing this option.
Calcium and calcium supplements: The data continue to grow
Anderson JJ, Kruszka B, Delaney JA, et al. Calcium intake from diet and supplements and the risk of coronary artery calcification and its progression among older adults: 10-year follow-up of the Multi-Ethnic Study of Atherosclerosis (MESA) [published online ahead of print October 11, 2016]. J Am Heart Assoc. pii: e003815.
Billington EO, Bristow SM, Gamble GD, et al. Acute effects of calcium supplements on blood pressure: randomised, crossover trial in postmenopausal women [published online ahead of print August 20, 2016]. Osteoporos Int. doi:10.1007/s00198-016-3744-y.
Crandall CJ, Aragaki AK, LeBoff MS, et al. Calcium plus vitamin D supplementation and height loss: findings from the Women's Health Initiative Calcium and Vitamin D clinical trial [published online ahead of print August 1, 2016]. Menopause. doi:10.1097 /GME.0000000000000704.
In 2001, a National Institutes of Health (NIH) Consensus Development Panel on osteoporosis concluded that calcium intake is crucial to maintain bone mass and should be maintained at 1,000-1,500 mg/day in older adults. The panel acknowledged that the majority of older adults did not meet the recommended intake from dietary sources alone, and therefore would require calcium supplementation. Calcium supplements are one of the most commonly used dietary supplements, and population-based surveys have shown that they are used by the majority of older men and women in the United States.7
More recently results from large randomized controlled trials (RCTs) of calcium supplements have been reported, leading to concerns about calcium efficacy for fracture risk and safety. Bolland and colleagues8 reported that calcium supplements increased the rate of cardiovascular events in healthy older women and suggested that their role in osteoporosis management be reconsidered. More recently, the US Preventive Services Task Force recommended against calcium supplements for the primary prevention of fractures in noninstitutionalized postmenopausal women.9
The association between calcium intake and CVD events
Anderson and colleagues acknowledged that recent randomized data suggest that calcium supplements may be associated with increased risk of cardiovascular disease (CVD) events. Using a longitudinal cohort study, they assessed the association between calcium intake, from both foods and supplements, and atherosclerosis, as measured by coronary artery calcification (CAC).
Details of the study by Anderson and colleagues
The authors studied 5,448 adults free of clinically diagnosed CVD (52% female; age range, 45-84 years) from the Multi-Ethnic Study of Atherosclerosis. Baseline total calcium intake was assessed from diet (using a food frequency questionnaire) and calcium supplements (by a medication inventory) and categorized into quintiles based on overall population distribution. Baseline CAC was measured by computed tomography (CT) scan, and CAC measurements were repeated in 2,742 participants approximately 10 years later. Women had higher calcium intakes than men.
After adjustment for potential confounders, among 1,567 participants without baseline CAC, the relative risk (RR) of developing incident CAC over 10 years, by quintile 1 to 5 of calcium intake is included in the TABLE. After accounting for total calcium intake, calcium supplement use was associated with increased risk for incident CAC (RR, 1.22; 95% CI, 1.07-1.39). No relation was found between baseline calcium intake and 10-year changes in CAC among those participants with baseline CAC less than zero.
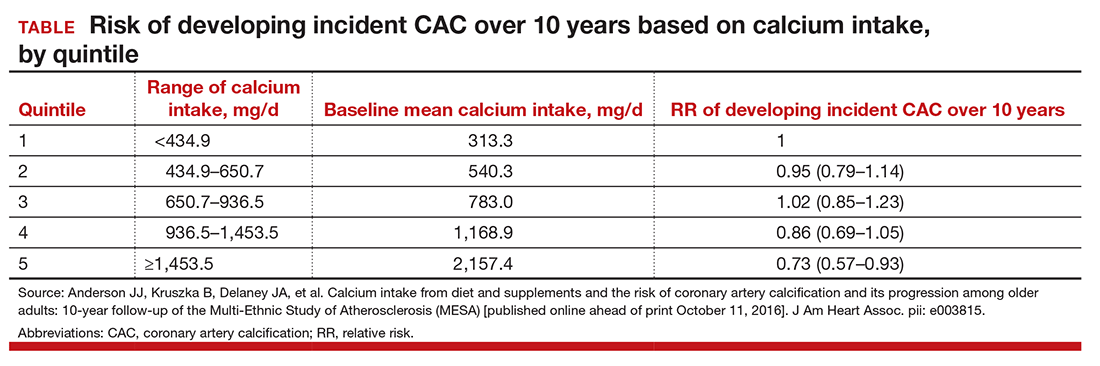
They concluded that high total calcium intake was associated with a decreased risk of incident atherosclerosis over long-term follow-up, particularly if achieved without supplement use. However, calcium supplement use may increase the risk for incident CAC.
Related article:
Does the discontinuation of menopausal hormone therapy affect a woman’s cardiovascular risk?
Calcium supplements and blood pressure
Billington and colleagues acknowledged that calcium supplements appear to increase cardiovascular risk but that the mechanism is unknown. They had previously reported that blood pressure declines over the course of the day in older women.10
Details of the study by Billington and colleagues
In this new study the investigators examined the acute effects of calcium supplements on blood pressure in a randomized controlled crossover trial in 40 healthy postmenopausal women (mean age, 71 years; body mass index [BMI], 27.2 kg/m2). Women attended on 2 occasions, with visits separated by 7 or more days. At each visit, they received either 1 g of calcium as citrate or placebo. Blood pressure and serum calcium concentrations were measured immediately before and 2, 4, and 6 hours after each intervention.
Ionized and total calcium concentrations increased after calcium (P<.0001 vs placebo). Systolic blood pressure (SBP) measurements decreased after both calcium and placebo but significantly less so after calcium (P=.02). The reduction in SBP from baseline was smaller after calcium compared with placebo by 6 mm Hg at 4 hours (P=.036) and by 9 mm Hg at 6 hours (P=.002). The reduction in diastolic blood pressure was similar after calcium and placebo.
These findings indicate that the use of calcium supplements in postmenopausal women attenuates the postbreakfast reduction in SBP by 6 to 9 mm Hg. Whether these changes in blood pressure influence cardiovascular risk requires further study.
Association between calcium, vitamin D, and height loss
Crandall and colleagues looked at the association between calcium and vitamin D supplementation and height loss in 36,282 participants of the Women's Health Initiative Calcium and Vitamin D trial.
Details of the study by Crandall and colleagues
The authors performed a post hoc analysis of data from a double-blind randomized controlled trial of 1,000 mg of elemental calcium as calcium carbonate with 400 IU of vitamin D3 daily (CaD) or placebo in postmenopausal women at 40 US clinical centers. Height was measured annually (mean follow-up, 5.9 years) with a stadiometer.
Average height loss was 1.28 mm/yr among participants assigned to CaD, versus 1.26 mm/yr for women assigned to placebo (P=.35). A strong association (P<.001) was observed between age group and height loss. The study authors concluded that, compared with placebo, calcium and vitamin D supplementation used in this trial did not prevent height loss in healthy postmenopausal women.
Adequate calcium is necessary for bone health. While calcium supplementation may not be adequate to prevent fractures, it is also not involved in the inevitable loss of overall height seen in postmenopausal women. Calcium supplementation has been implicated in an increase in CVD. These data seem to indicate that, while calcium supplementation results in higher systolic blood pressure during the day, as well as higher coronary artery calcium scores, greater dietary calcium actually may decrease the incidence of atherosclerosis.
Sarcopenia: Still important, clinical approaches to easily detect it
Beaudart C, McCloskey E, Bruyére O, et al. Sarcopenia in daily practice: assessment and management. BMC Geriatr. 2016;16(1):170.
In last year's update, I reviewed the article by He and colleagues11 on the relationship between sarcopenia and body composition with osteoporosis. Sarcopenia, which is the age-related loss of muscle mass and strength, is important to address in patients. Body composition and muscle strength are directly correlated with bone density, and this is not surprising since bone and muscle share some common hormonal, genetic, nutritional, and lifestyle determinants.12,13 Sarcopenia can be diagnosed via dual-energy x-ray absorptiometry (DXA) scan looking at lean muscle mass.
The term sarcopenia was first coined by Rosenberg and colleagues in 198914 as a progressive loss of skeletal muscle mass with advancing age. Since then, the definition has expanded to incorporate the notion of impaired muscle strength or physical performance. Sarcopenia is associated with morbidity and mortality from linked physical disability, falls, fractures, poor quality of life, depression, and hospitalization.15
Current research is focusing on nutritional exercise/activity-based and other novel interventions for improving the quality and quantity of skeletal muscle in older people. Some studies demonstrated that resistance training combined with nutritional supplements can improve muscle function.16
Details of the study
Beaudart and colleagues propose some user-friendly and inexpensive methods that can be utilized to assess sarcopenia in real life settings. They acknowledge that in research settings or even specialist clinical settings, DXA or computed tomography (CT) scans are the best assessment of muscle mass.
Anthropometric measurements. In a primary care setting, anthropometric measurement, especially calf circumference and mid-upper arm muscle circumference, correlate with overall muscle mass and reflect both health and nutritional status and predict performance, health, and survival in older people.
However, with advancing age, changes in the distribution of fat and loss of skin elasticity are such that circumference incurs a loss of accuracy and precision in older people. Some studies suggest that an adjustment of anthropometric measurements for age, sex, or BMI results in a better correlation with DXA-measured lean mass.17 Anthropometric measurements are simple clinical prediction tools that can be easily applied for sarcopenia since they offer the most portable, commonly applicable, inexpensive, and noninvasive technique for assessing size, proportions, and composition of the human body. However, their validity is limited when applied to individuals because cutoff points to identify low muscle mass still need to be defined. Still, serial measurements in a patient over time may be valuable.
Related article:
2014 Update on osteoporosis
Handgrip strength, as measured with a dynamometer, appears to be the most widely used method for the measurement of muscle strength. In general, isometric handgrip strength shows a good correlation with leg strength and also with lower extremity power, and calf cross-sectional muscle area. The measurement is easy to perform, inexpensive and does not require a specialist-trained staff.
Standardized conditions for the test include seating the patient in a standard chair with her forearms resting flat on the chair arms. Clinicians should demonstrate the use of the dynamometer and show that gripping very tightly registers the best score. Six measurements should be taken, 3 with each arm. Ideally, patients should be encouraged to squeeze as hard and tightly as possible during 3 to 5 seconds for each of the 6 trials; usually the highest reading of the 6 measurements is reported as the final result. The Jamar dynamometer, or similar hydraulic dynamometer, is the gold standard for this measurement.
Gait speed measurement. The most widely used tool in clinical practice for the assessment of physical performance is the gait speed measurement. The test is highly acceptable for participants and health professionals in clinical settings. No special equipment is required; it needs only a flat floor devoid of obstacles. In the 4-meter gait speed test, men and women with a gait speed of less than 0.8 meters/sec are described as having a poor physical performance. The average extra time added to the consultation by measuring the 4-meter gait speed was only 95 seconds (SD, 20 seconds).
Loss of muscle mass correlates with loss of bone mass as our patients age. In addition, such sarcopenia increases the risk of falls, a significant component of the rising rate of fragility fractures. Anthropometric measures, grip strength, and gait speed are easy, low-cost measures that can identify patients at increased risk.
Romosozumab: An interesting new agent to look forward to
Cosman F, Crittenden DB, Adachi JD, et al. Romosozumab treatment in postmenopausal women with osteoporosis. N Engl J Med. 2016;375(16):1532-1543.
Romosozumab is a monoclonal antibody that binds sclerostin, increasing bone formation and decreasing bone resorption. Cosman and colleagues enrolled 7,180 postmenopausal women with a T score of -2.5 to -3.5 at the total hip or femoral neck. Participants were randomly assigned to receive subcutaneous injections of romosozumab 210 mg or placebo monthly for 12 months. Thereafter, women in each group received subcutaneous denosumab 60 mg for 12 months--administered every 6 months. The coprimary end points were the cumulative incidences of new vertebral fractures at 12 and 24 months. Secondary end points included clinical and nonvertebral fractures.
Details of the study
At 12 months, new vertebral fractures had occurred in 16 of 3,321 women (0.5%) in the romosozumab group, as compared with 59 of 3,322 (1.8%) in the placebo group (representing a 73% lower risk of fracture with romosozumab; P<.001). Clinical fractures had occurred in 58 of 3,589 women (1.6%) in the romosozumab group, as compared with 90 of 3,591 (2.5%) in the placebo group (a 36% lower fracture risk with romosozumab; P = .008). Nonvertebral fractures had occurred in 56 of 3,589 women (1.6%) in the romosozumab group and in 75 of 3,591 (2.1%) in the placebo group (P = .10).
At 24 months, the rates of vertebral fractures were significantly lower in the romosozumab group than in the placebo group after each group made the transition to denosumab (0.6% [21 of 3,325 women] in the romosozumab group vs 2.5% [84 of 3,327 women] in the placebo group, a 75% lower risk with romosozumab; P<.001). Adverse events, including cardiovascular events, osteoarthritis, and cancer, appeared to be balanced between the groups. One atypical femoral fracture and 2 cases of osteonecrosis of the jaw were observed in the romosozumab group.
Lower risk of fracture
Thus, in postmenopausal women with osteoporosis, romosozumab was associated with a lower risk of vertebral fracture than placebo at 12 months and, after the transition to denosumab, at 24 months. The lower risk of clinical fracture that was seen with romosozumab was evident at 1 year.
Of note, the effect of romosozumab on the risk of vertebral fracture was rapid, with only 2 additional vertebral fractures (of a total of 16 such fractures in the romosozumab group) occurring in the second 6 months of the first year of therapy. Because vertebral and clinical fractures are associated with increased morbidity and considerable health care costs, a treatment that would reduce this risk rapidly could offer appropriate patients an important benefit.
Romosozumab is a new agent. Though not yet available, it is extremely interesting because it not only decreases bone resorption but also increases bone formation. The results of this large prospective trial show that such an agent reduces both vertebral and clinical fracture and reduces that fracture risk quite rapidly within the first 6 months of therapy.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Prioritize bone health, as osteoporotic fracture is a major source of morbidity and mortality among women. In this article: fracture risk with OC use in perimenopause, data that inform calcium’s role in cardiovascular disease, sarcopenia management, and an emerging treatment.
Most women’s health care providers are aware of recent changes and controversies regarding cervical cancer screening, mammography frequency, and whether a pelvic bimanual exam should be part of our annual well woman evaluation.1 However, I believe one of the most important things we as clinicians can do is be frontline in promoting bone health. Osteoporotic fracture is a major source of morbidity and mortality.2,3 Thus, promoting the maintenance of bone health is a priority in my own practice. It is also one of my many academic interests.
What follows is an update on bone health. In past years, this update has been entitled, “Update on osteoporosis,” but what we are trying to accomplish is fracture reduction. Thus, priorities for bone health consist of recognition of risk, lifestyle and dietary counseling, as well as the use of pharmacologic agents when appropriate. Certain research stands out as informative for your practice:
- a recent study on the risk of fracture with oral contraceptive (OC) use in perimenopause
- 3 just-published studies that inform our understanding of calcium’s role in cardiovascular health
- a review on sarcopenia management
- new data on romosozumab.
Oral contraceptive use in perimenopause
Scholes D, LaCroix AZ, Hubbard RA, et al. Oral contraceptive use and fracture risk around the menopausal transition. Menopause. 2016;23(2):166-174.
The use of OCs in women of older reproductive age has increased ever since the cutoff age of 35 years was eliminated.4 Lower doses have continued to be utilized in these "older" women with excellent control of irregular bleeding due to ovulatory dysfunction (and reduction in psychosocial symptoms as well).5
The effect of OC use on risk of fracture remains unclear, and use during later reproductive life may be increasing. To determine the association between OC use during later reproductive life and risk of fracture across the menopausal transition, Scholes and colleagues conducted a population-based case-controlled study in a Pacific Northwest HMO, Group Health Cooperative.
Details of the study
Scholes and colleagues enrolled 1,204 case women aged 45 to 59 years with incident fractures, and 2,275 control women. Potential cases with fracture codes in automated data were adjudicated by electronic health record review. Potential control women without fracture codes were selected concurrently, sampling based on age. Participants received a structured study interview. Using logistic regression, associations between OC use and fracture risk were calculated as odds ratios (ORs) and 95% confidence intervals (CIs).
Participation was 69% for cases and 64% for controls. The study sample was 82% white; mean age was 54 years. The most common fracture site for cases was the wrist/forearm (32%). Adjusted fracture risk did not differ between cases and controls for OC use:
- in the 10 years before menopause (OR, 0.90; 95% CI, 0.74-1.11)
- after age 38 years (OR, 0.94; 95% CI, 0.78-1.14)
- over the duration, or
- for other OC exposures.
Related article:
2016 Update on female sexual dysfunction
Association between fractures and OC use near menopause
The current study does not show an association between fractures near the menopausal transition and OC use in the decade before menopause or after age 38 years. For women considering OC use at these times, fracture risk does not seem to be either reduced or increased.
These results, looking at fracture, seem to be further supported by trials conducted by Gambacciani and colleagues,6 in which researchers randomly assigned irregularly cycling perimenopausal women (aged 40-49 years) to 20 μg ethinyl estradiol OCs or calcium/placebo. Results showed that this low-dose OC use significantly increased bone density at the femoral neck, spine, and other sites relative to control women after 24 months.
In the current Scholes study, the use of OCs in the decade before menopause or after age 38 did not reduce fracture risk in the years around the time of menopause. It is reassuring that their use was not associated with any increased fracture risk.
These findings provide additional clarity and guidance to women and their clinicians at a time of increasing public health concern about fractures. For women who may choose to use OCs during late premenopause (around age 38-48 years), fracture risk around the menopausal transition will not differ from women not choosing this option.
Calcium and calcium supplements: The data continue to grow
Anderson JJ, Kruszka B, Delaney JA, et al. Calcium intake from diet and supplements and the risk of coronary artery calcification and its progression among older adults: 10-year follow-up of the Multi-Ethnic Study of Atherosclerosis (MESA) [published online ahead of print October 11, 2016]. J Am Heart Assoc. pii: e003815.
Billington EO, Bristow SM, Gamble GD, et al. Acute effects of calcium supplements on blood pressure: randomised, crossover trial in postmenopausal women [published online ahead of print August 20, 2016]. Osteoporos Int. doi:10.1007/s00198-016-3744-y.
Crandall CJ, Aragaki AK, LeBoff MS, et al. Calcium plus vitamin D supplementation and height loss: findings from the Women's Health Initiative Calcium and Vitamin D clinical trial [published online ahead of print August 1, 2016]. Menopause. doi:10.1097 /GME.0000000000000704.
In 2001, a National Institutes of Health (NIH) Consensus Development Panel on osteoporosis concluded that calcium intake is crucial to maintain bone mass and should be maintained at 1,000-1,500 mg/day in older adults. The panel acknowledged that the majority of older adults did not meet the recommended intake from dietary sources alone, and therefore would require calcium supplementation. Calcium supplements are one of the most commonly used dietary supplements, and population-based surveys have shown that they are used by the majority of older men and women in the United States.7
More recently results from large randomized controlled trials (RCTs) of calcium supplements have been reported, leading to concerns about calcium efficacy for fracture risk and safety. Bolland and colleagues8 reported that calcium supplements increased the rate of cardiovascular events in healthy older women and suggested that their role in osteoporosis management be reconsidered. More recently, the US Preventive Services Task Force recommended against calcium supplements for the primary prevention of fractures in noninstitutionalized postmenopausal women.9
The association between calcium intake and CVD events
Anderson and colleagues acknowledged that recent randomized data suggest that calcium supplements may be associated with increased risk of cardiovascular disease (CVD) events. Using a longitudinal cohort study, they assessed the association between calcium intake, from both foods and supplements, and atherosclerosis, as measured by coronary artery calcification (CAC).
Details of the study by Anderson and colleagues
The authors studied 5,448 adults free of clinically diagnosed CVD (52% female; age range, 45-84 years) from the Multi-Ethnic Study of Atherosclerosis. Baseline total calcium intake was assessed from diet (using a food frequency questionnaire) and calcium supplements (by a medication inventory) and categorized into quintiles based on overall population distribution. Baseline CAC was measured by computed tomography (CT) scan, and CAC measurements were repeated in 2,742 participants approximately 10 years later. Women had higher calcium intakes than men.
After adjustment for potential confounders, among 1,567 participants without baseline CAC, the relative risk (RR) of developing incident CAC over 10 years, by quintile 1 to 5 of calcium intake is included in the TABLE. After accounting for total calcium intake, calcium supplement use was associated with increased risk for incident CAC (RR, 1.22; 95% CI, 1.07-1.39). No relation was found between baseline calcium intake and 10-year changes in CAC among those participants with baseline CAC less than zero.
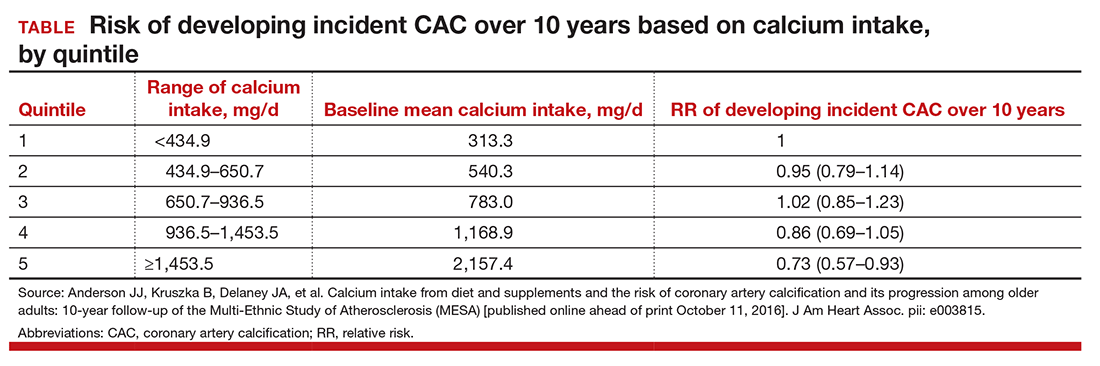
They concluded that high total calcium intake was associated with a decreased risk of incident atherosclerosis over long-term follow-up, particularly if achieved without supplement use. However, calcium supplement use may increase the risk for incident CAC.
Related article:
Does the discontinuation of menopausal hormone therapy affect a woman’s cardiovascular risk?
Calcium supplements and blood pressure
Billington and colleagues acknowledged that calcium supplements appear to increase cardiovascular risk but that the mechanism is unknown. They had previously reported that blood pressure declines over the course of the day in older women.10
Details of the study by Billington and colleagues
In this new study the investigators examined the acute effects of calcium supplements on blood pressure in a randomized controlled crossover trial in 40 healthy postmenopausal women (mean age, 71 years; body mass index [BMI], 27.2 kg/m2). Women attended on 2 occasions, with visits separated by 7 or more days. At each visit, they received either 1 g of calcium as citrate or placebo. Blood pressure and serum calcium concentrations were measured immediately before and 2, 4, and 6 hours after each intervention.
Ionized and total calcium concentrations increased after calcium (P<.0001 vs placebo). Systolic blood pressure (SBP) measurements decreased after both calcium and placebo but significantly less so after calcium (P=.02). The reduction in SBP from baseline was smaller after calcium compared with placebo by 6 mm Hg at 4 hours (P=.036) and by 9 mm Hg at 6 hours (P=.002). The reduction in diastolic blood pressure was similar after calcium and placebo.
These findings indicate that the use of calcium supplements in postmenopausal women attenuates the postbreakfast reduction in SBP by 6 to 9 mm Hg. Whether these changes in blood pressure influence cardiovascular risk requires further study.
Association between calcium, vitamin D, and height loss
Crandall and colleagues looked at the association between calcium and vitamin D supplementation and height loss in 36,282 participants of the Women's Health Initiative Calcium and Vitamin D trial.
Details of the study by Crandall and colleagues
The authors performed a post hoc analysis of data from a double-blind randomized controlled trial of 1,000 mg of elemental calcium as calcium carbonate with 400 IU of vitamin D3 daily (CaD) or placebo in postmenopausal women at 40 US clinical centers. Height was measured annually (mean follow-up, 5.9 years) with a stadiometer.
Average height loss was 1.28 mm/yr among participants assigned to CaD, versus 1.26 mm/yr for women assigned to placebo (P=.35). A strong association (P<.001) was observed between age group and height loss. The study authors concluded that, compared with placebo, calcium and vitamin D supplementation used in this trial did not prevent height loss in healthy postmenopausal women.
Adequate calcium is necessary for bone health. While calcium supplementation may not be adequate to prevent fractures, it is also not involved in the inevitable loss of overall height seen in postmenopausal women. Calcium supplementation has been implicated in an increase in CVD. These data seem to indicate that, while calcium supplementation results in higher systolic blood pressure during the day, as well as higher coronary artery calcium scores, greater dietary calcium actually may decrease the incidence of atherosclerosis.
Sarcopenia: Still important, clinical approaches to easily detect it
Beaudart C, McCloskey E, Bruyére O, et al. Sarcopenia in daily practice: assessment and management. BMC Geriatr. 2016;16(1):170.
In last year's update, I reviewed the article by He and colleagues11 on the relationship between sarcopenia and body composition with osteoporosis. Sarcopenia, which is the age-related loss of muscle mass and strength, is important to address in patients. Body composition and muscle strength are directly correlated with bone density, and this is not surprising since bone and muscle share some common hormonal, genetic, nutritional, and lifestyle determinants.12,13 Sarcopenia can be diagnosed via dual-energy x-ray absorptiometry (DXA) scan looking at lean muscle mass.
The term sarcopenia was first coined by Rosenberg and colleagues in 198914 as a progressive loss of skeletal muscle mass with advancing age. Since then, the definition has expanded to incorporate the notion of impaired muscle strength or physical performance. Sarcopenia is associated with morbidity and mortality from linked physical disability, falls, fractures, poor quality of life, depression, and hospitalization.15
Current research is focusing on nutritional exercise/activity-based and other novel interventions for improving the quality and quantity of skeletal muscle in older people. Some studies demonstrated that resistance training combined with nutritional supplements can improve muscle function.16
Details of the study
Beaudart and colleagues propose some user-friendly and inexpensive methods that can be utilized to assess sarcopenia in real life settings. They acknowledge that in research settings or even specialist clinical settings, DXA or computed tomography (CT) scans are the best assessment of muscle mass.
Anthropometric measurements. In a primary care setting, anthropometric measurement, especially calf circumference and mid-upper arm muscle circumference, correlate with overall muscle mass and reflect both health and nutritional status and predict performance, health, and survival in older people.
However, with advancing age, changes in the distribution of fat and loss of skin elasticity are such that circumference incurs a loss of accuracy and precision in older people. Some studies suggest that an adjustment of anthropometric measurements for age, sex, or BMI results in a better correlation with DXA-measured lean mass.17 Anthropometric measurements are simple clinical prediction tools that can be easily applied for sarcopenia since they offer the most portable, commonly applicable, inexpensive, and noninvasive technique for assessing size, proportions, and composition of the human body. However, their validity is limited when applied to individuals because cutoff points to identify low muscle mass still need to be defined. Still, serial measurements in a patient over time may be valuable.
Related article:
2014 Update on osteoporosis
Handgrip strength, as measured with a dynamometer, appears to be the most widely used method for the measurement of muscle strength. In general, isometric handgrip strength shows a good correlation with leg strength and also with lower extremity power, and calf cross-sectional muscle area. The measurement is easy to perform, inexpensive and does not require a specialist-trained staff.
Standardized conditions for the test include seating the patient in a standard chair with her forearms resting flat on the chair arms. Clinicians should demonstrate the use of the dynamometer and show that gripping very tightly registers the best score. Six measurements should be taken, 3 with each arm. Ideally, patients should be encouraged to squeeze as hard and tightly as possible during 3 to 5 seconds for each of the 6 trials; usually the highest reading of the 6 measurements is reported as the final result. The Jamar dynamometer, or similar hydraulic dynamometer, is the gold standard for this measurement.
Gait speed measurement. The most widely used tool in clinical practice for the assessment of physical performance is the gait speed measurement. The test is highly acceptable for participants and health professionals in clinical settings. No special equipment is required; it needs only a flat floor devoid of obstacles. In the 4-meter gait speed test, men and women with a gait speed of less than 0.8 meters/sec are described as having a poor physical performance. The average extra time added to the consultation by measuring the 4-meter gait speed was only 95 seconds (SD, 20 seconds).
Loss of muscle mass correlates with loss of bone mass as our patients age. In addition, such sarcopenia increases the risk of falls, a significant component of the rising rate of fragility fractures. Anthropometric measures, grip strength, and gait speed are easy, low-cost measures that can identify patients at increased risk.
Romosozumab: An interesting new agent to look forward to
Cosman F, Crittenden DB, Adachi JD, et al. Romosozumab treatment in postmenopausal women with osteoporosis. N Engl J Med. 2016;375(16):1532-1543.
Romosozumab is a monoclonal antibody that binds sclerostin, increasing bone formation and decreasing bone resorption. Cosman and colleagues enrolled 7,180 postmenopausal women with a T score of -2.5 to -3.5 at the total hip or femoral neck. Participants were randomly assigned to receive subcutaneous injections of romosozumab 210 mg or placebo monthly for 12 months. Thereafter, women in each group received subcutaneous denosumab 60 mg for 12 months--administered every 6 months. The coprimary end points were the cumulative incidences of new vertebral fractures at 12 and 24 months. Secondary end points included clinical and nonvertebral fractures.
Details of the study
At 12 months, new vertebral fractures had occurred in 16 of 3,321 women (0.5%) in the romosozumab group, as compared with 59 of 3,322 (1.8%) in the placebo group (representing a 73% lower risk of fracture with romosozumab; P<.001). Clinical fractures had occurred in 58 of 3,589 women (1.6%) in the romosozumab group, as compared with 90 of 3,591 (2.5%) in the placebo group (a 36% lower fracture risk with romosozumab; P = .008). Nonvertebral fractures had occurred in 56 of 3,589 women (1.6%) in the romosozumab group and in 75 of 3,591 (2.1%) in the placebo group (P = .10).
At 24 months, the rates of vertebral fractures were significantly lower in the romosozumab group than in the placebo group after each group made the transition to denosumab (0.6% [21 of 3,325 women] in the romosozumab group vs 2.5% [84 of 3,327 women] in the placebo group, a 75% lower risk with romosozumab; P<.001). Adverse events, including cardiovascular events, osteoarthritis, and cancer, appeared to be balanced between the groups. One atypical femoral fracture and 2 cases of osteonecrosis of the jaw were observed in the romosozumab group.
Lower risk of fracture
Thus, in postmenopausal women with osteoporosis, romosozumab was associated with a lower risk of vertebral fracture than placebo at 12 months and, after the transition to denosumab, at 24 months. The lower risk of clinical fracture that was seen with romosozumab was evident at 1 year.
Of note, the effect of romosozumab on the risk of vertebral fracture was rapid, with only 2 additional vertebral fractures (of a total of 16 such fractures in the romosozumab group) occurring in the second 6 months of the first year of therapy. Because vertebral and clinical fractures are associated with increased morbidity and considerable health care costs, a treatment that would reduce this risk rapidly could offer appropriate patients an important benefit.
Romosozumab is a new agent. Though not yet available, it is extremely interesting because it not only decreases bone resorption but also increases bone formation. The results of this large prospective trial show that such an agent reduces both vertebral and clinical fracture and reduces that fracture risk quite rapidly within the first 6 months of therapy.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- MacLaughlin KL, Faubion SS, Long ME, Pruthi S, Casey PM. Should the annual pelvic examination go the way of annual cervical cytology? Womens Health (Lond). 2014;10(4):373–384.
- Wright NC, Looker AC, Saag KG, et al. The recent prevalence of osteoporosis and low bone mass in the United States based on bone mineral density at the femoral neck or lumbar spine. J Bone Miner Res. 2014;29(11):2520–2526.
- Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King AB, Tosterson A. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J Bone Miner Res. 2007;22(3):465–475.
- Kaunitz AM. Hormonal contraception in women of older reproductive age. N Engl J Med. 2008;358:1262–1270.
- Kaunitz AM. Oral contraceptive use in perimenopause. Am J Obstet Gynecol. 2001;185(2 suppl):S32–S37.
- Gambacciani M, Cappagli B, Lazzarini V, Ciaponi M, Fruzzetti F, Genazzani AR. Longitudinal evaluation of perimenopausal bone loss: effects of different low dose oral contraceptive preparations on bone mineral density. Maturitas. 2006;54(2):176–180.
- Bailey R, Dodd K, Goldman J, et al. Estimation of total usual calcium and vitamin D intakes in the United States. J Nutr. 2010;140(4):817–822.
- Bolland MJ, Grey A, Reid IR. Calcium supplements and cardiovascular risk: 5 years on. Ther Adv Drug Saf. 2013;4(5):199–210.
- Moyer VA; U.S. Preventive Services Task Force. Vitamin D and calcium supplementation to prevent fractures in adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2013;158(9):691–696.
- Bristow SM, Gamble GD, Stewart A, Horne AM, Reid IR. Acute effects of calcium supplements on blood pressure and blood coagulation: secondary analysis of a randomised controlled trial in post-menopausal women. Br J Nutr. 2015;114(11):1868–1874.
- He H, Liu Y, Tian Q, Papasian CJ, Hu T, Deng HW. Relationship of sarcopenia and body composition with osteoporosis. Osteoporos Int. 2016;27(2):473–482.
- Coin A, Perissinotto E, Enzi G, et al. Predictors of low bone mineral density in the elderly: the role of dietary intake, nutritional status and sarcopenia. Eur J Clin Nutr. 2008;62(6):802–809.
- Taaffe DR, Cauley JA, Danielson M, et al. Race and sex effects on the association between muscle strength, soft tissue, and bone mineral density in healthy elders: the Health, Aging, and Body Composition Study. J Bone Miner Res. 2001;16(7):1343–1352.
- Rosenberg IH. Sarcopenia: origins and clinical relevance. J Nutr. 1997;127(5 suppl):990S–991S.
- Beaudart C, Rizzoli R, Bruyere O, Reginster JY, Biver E. Sarcopenia: Burden and challenges for Public Health. Arch Public Health. 2014;72(1):45.
- Cruz-Jentoft AJ, Landi F, Schneider SM, et al. Prevalence of and interventions for sarcopenia in ageing adults: a systematic review. Report of the International Sarcopenia Initiative (EWGSOP and IWGS). Age Ageing. 2014;43(6):748–759.
- Kulkarni B, Kuper H, Taylor A, et al. Development and validation of anthropometric prediction equations for estimation of lean body mass and appendicular lean soft tissue in Indian men and women. J Appl Physiol. 2013;115(8):1156–1162.
- MacLaughlin KL, Faubion SS, Long ME, Pruthi S, Casey PM. Should the annual pelvic examination go the way of annual cervical cytology? Womens Health (Lond). 2014;10(4):373–384.
- Wright NC, Looker AC, Saag KG, et al. The recent prevalence of osteoporosis and low bone mass in the United States based on bone mineral density at the femoral neck or lumbar spine. J Bone Miner Res. 2014;29(11):2520–2526.
- Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King AB, Tosterson A. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J Bone Miner Res. 2007;22(3):465–475.
- Kaunitz AM. Hormonal contraception in women of older reproductive age. N Engl J Med. 2008;358:1262–1270.
- Kaunitz AM. Oral contraceptive use in perimenopause. Am J Obstet Gynecol. 2001;185(2 suppl):S32–S37.
- Gambacciani M, Cappagli B, Lazzarini V, Ciaponi M, Fruzzetti F, Genazzani AR. Longitudinal evaluation of perimenopausal bone loss: effects of different low dose oral contraceptive preparations on bone mineral density. Maturitas. 2006;54(2):176–180.
- Bailey R, Dodd K, Goldman J, et al. Estimation of total usual calcium and vitamin D intakes in the United States. J Nutr. 2010;140(4):817–822.
- Bolland MJ, Grey A, Reid IR. Calcium supplements and cardiovascular risk: 5 years on. Ther Adv Drug Saf. 2013;4(5):199–210.
- Moyer VA; U.S. Preventive Services Task Force. Vitamin D and calcium supplementation to prevent fractures in adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2013;158(9):691–696.
- Bristow SM, Gamble GD, Stewart A, Horne AM, Reid IR. Acute effects of calcium supplements on blood pressure and blood coagulation: secondary analysis of a randomised controlled trial in post-menopausal women. Br J Nutr. 2015;114(11):1868–1874.
- He H, Liu Y, Tian Q, Papasian CJ, Hu T, Deng HW. Relationship of sarcopenia and body composition with osteoporosis. Osteoporos Int. 2016;27(2):473–482.
- Coin A, Perissinotto E, Enzi G, et al. Predictors of low bone mineral density in the elderly: the role of dietary intake, nutritional status and sarcopenia. Eur J Clin Nutr. 2008;62(6):802–809.
- Taaffe DR, Cauley JA, Danielson M, et al. Race and sex effects on the association between muscle strength, soft tissue, and bone mineral density in healthy elders: the Health, Aging, and Body Composition Study. J Bone Miner Res. 2001;16(7):1343–1352.
- Rosenberg IH. Sarcopenia: origins and clinical relevance. J Nutr. 1997;127(5 suppl):990S–991S.
- Beaudart C, Rizzoli R, Bruyere O, Reginster JY, Biver E. Sarcopenia: Burden and challenges for Public Health. Arch Public Health. 2014;72(1):45.
- Cruz-Jentoft AJ, Landi F, Schneider SM, et al. Prevalence of and interventions for sarcopenia in ageing adults: a systematic review. Report of the International Sarcopenia Initiative (EWGSOP and IWGS). Age Ageing. 2014;43(6):748–759.
- Kulkarni B, Kuper H, Taylor A, et al. Development and validation of anthropometric prediction equations for estimation of lean body mass and appendicular lean soft tissue in Indian men and women. J Appl Physiol. 2013;115(8):1156–1162.
Top 3 things I learned at the NAMS 2016 annual meeting
- Visit NAMS
- Visit NAMS
- Visit NAMS