User login
IBD surveillance: Quality not quantity
Optimizing colonoscopy quality in patients with ulcerative colitis or Crohn’s disease involving the colon is important. Their risk for the development of colorectal cancer (CRC) and of interval CRC is significantly higher compared with the non–inflammatory bowel disease (IBD) population.
Most CRC cases in IBD are believed to arise from dysplasia, and thus, surveillance colonoscopy is recommended to detect dysplasia. Key factors that influence the success of surveillance colonoscopy in IBD patients include: 1) endoscopic recognition of dysplasia, 2) adequacy of mucosal sampling, 3) awareness of interfering anatomy, such as strictures and pseudopolyps, 4) appropriate differentiation of dysplastic lesions as endoscopically resectable, 5) complete removal of endoscopically resectable dysplasia, and 6) patient compliance.
Over a decade ago, we learned that most dysplasia discovered in patients with IBD is actually visible. The use of high-definition video-endoscopy and newer methods, such as chromoendoscopy with mucosal dye spraying, enhance the detection of dysplasia. Today, with the widespread use of newer technologies and techniques, the literature indicates that targeted biopsies of visible lesions account for approximately 90% of cases, whereas random biopsy (resulting in detection of an endoscopically invisible lesion) accounts for only 10% of cases of identified dysplasia.
The endoscopic recognition of dysplastic colorectal lesions may have important implications for the surveillance and management of dysplasia, and shift it away from the traditional random biopsy technique, where less than 0.1% of the colonic mucosal surface area is sampled, and from colectomy for any diagnosis of dysplasia.
Enhanced endoscopy techniques such as chromoendoscopy can have a substantial impact upon IBD surveillance, increasing the dysplasia detection rates, as well as informing management decisions. Chromoendoscopy, using a dye solution of either methylene blue or indigo carmine applied onto the colonic mucosa to enhance contrast during surveillance colonoscopy, is performed either in a pancolonic fashion to detect lesions or in a targeted fashion to allow for detailed viewing of an identified lesion (Figure 1).
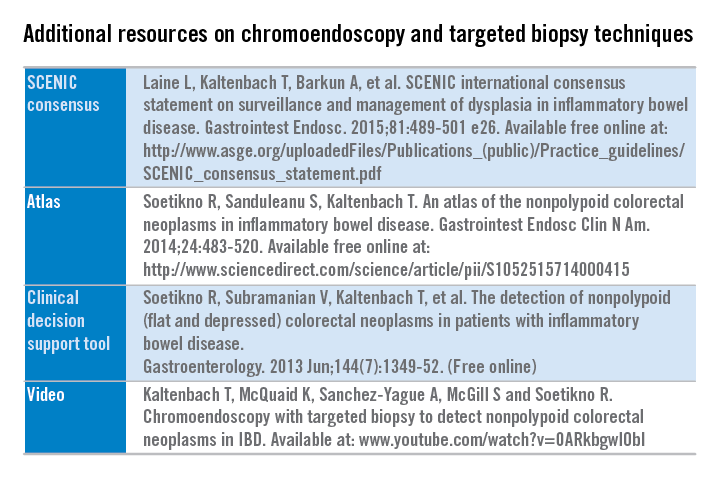
Additional resources are freely available detailing the technique and suggested steps to implement chromoendoscopy into practice. (See additional resources on chromoendoscopy and targeted biopsy techniques.)
An international multidisciplinary group, SCENIC (Surveillance for Colorectal Endoscopic Neoplasia Detection and Management in Inflammatory Bowel Disease Patients: International Consensus), which represents a wide spectrum of stakeholders and attitudes regarding IBD surveillance, sought to develop unifying consensus recommendations addressing two issues: 1) how should surveillance colonoscopy to detect dysplasia be performed, and 2) how should dysplasia identified at colonoscopy be managed. The SCENIC group adhered to suggested standards for guideline development from the Institute of Medicine and others and that incorporated the GRADE methodology. A systematic review was performed for each focused clinical question, followed by a review of a full synthesis of evidence by panelists.
SCENIC key summary recommendations
Detection
• High definition is recommended over standard definition for performance of surveillance colonoscopy.
• Routine performance of chromoendoscopy during IBD surveillance is suggested as an adjunct to high-definition colonoscopy.
• Narrowband imaging is not recommended as an alternative for high-definition, white-light colonoscopy or chromoendoscopy.
• No specific recommendation on performance of random biopsies was made in patients undergoing high-definition, white-light colonoscopy plus chromoendoscopy. The panel did not reach consensus on this topic because 60% of the panel members disagreed with performing random biopsies during chromoendoscopy, and a recommendation required 80% agreement or disagreement.
Management
• When dysplasia is detected, it should be characterized as “endoscopically resectable” or “nonendoscopically resectable” (The terms “dysplasia-associated lesion or mass (DALM),” “adenoma-like,” and “nonadenoma-like” should be abandoned).
• Visible dysplasia should be characterized according to the Paris classification polypoid or nonpolypoid, with modifications including the addition of terms for ulceration and border of the lesion.
• The term endoscopically resectable indicates that 1) distinct margins of the lesion could be identified, 2) the lesion appears to be completely removed on visual inspection after endoscopic resection, 3) histologic examination of the resected specimen is consistent with complete removal, and 4) biopsy specimens taken from mucosa immediately adjacent to the resection site are free of dysplasia on histologic examination.
• After complete removal of endoscopically resectable polypoid or nonpolypoid dysplasia, surveillance colonoscopy is recommended rather than colectomy.
• For patients with endoscopically invisible dysplasia (confirmed by a GI pathologist), referral is suggested to an endoscopist with expertise in IBD surveillance using chromoendoscopy with high-definition colonoscopy.
The SCENIC recommendations aim to optimize the detection and management of dysplasia in IBD patients. Future research in IBD surveillance should assess the potential for chromoendoscopy to improve risk stratification to elucidate optimal surveillance intervals, and the impact on CRC incidence and mortality. In addition, the role of resection of nonpolypoid dysplasia in the reduction in CRC incidence or need for colectomy requires further investigation.
Dr. Kaltenbach is a gastroenterologist at Veterans Affairs, and a clinical assistant professor of medicine at Stanford (Calif.) University. She has no conflicts of interest. Her comments were made during the ASGE and AGA joint Presidential Plenary at the annual Digestive Disease Week.
Optimizing colonoscopy quality in patients with ulcerative colitis or Crohn’s disease involving the colon is important. Their risk for the development of colorectal cancer (CRC) and of interval CRC is significantly higher compared with the non–inflammatory bowel disease (IBD) population.
Most CRC cases in IBD are believed to arise from dysplasia, and thus, surveillance colonoscopy is recommended to detect dysplasia. Key factors that influence the success of surveillance colonoscopy in IBD patients include: 1) endoscopic recognition of dysplasia, 2) adequacy of mucosal sampling, 3) awareness of interfering anatomy, such as strictures and pseudopolyps, 4) appropriate differentiation of dysplastic lesions as endoscopically resectable, 5) complete removal of endoscopically resectable dysplasia, and 6) patient compliance.
Over a decade ago, we learned that most dysplasia discovered in patients with IBD is actually visible. The use of high-definition video-endoscopy and newer methods, such as chromoendoscopy with mucosal dye spraying, enhance the detection of dysplasia. Today, with the widespread use of newer technologies and techniques, the literature indicates that targeted biopsies of visible lesions account for approximately 90% of cases, whereas random biopsy (resulting in detection of an endoscopically invisible lesion) accounts for only 10% of cases of identified dysplasia.
The endoscopic recognition of dysplastic colorectal lesions may have important implications for the surveillance and management of dysplasia, and shift it away from the traditional random biopsy technique, where less than 0.1% of the colonic mucosal surface area is sampled, and from colectomy for any diagnosis of dysplasia.
Enhanced endoscopy techniques such as chromoendoscopy can have a substantial impact upon IBD surveillance, increasing the dysplasia detection rates, as well as informing management decisions. Chromoendoscopy, using a dye solution of either methylene blue or indigo carmine applied onto the colonic mucosa to enhance contrast during surveillance colonoscopy, is performed either in a pancolonic fashion to detect lesions or in a targeted fashion to allow for detailed viewing of an identified lesion (Figure 1).
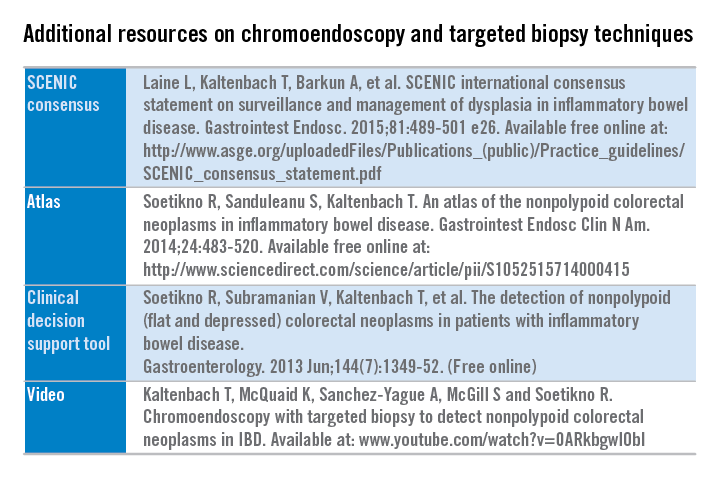
Additional resources are freely available detailing the technique and suggested steps to implement chromoendoscopy into practice. (See additional resources on chromoendoscopy and targeted biopsy techniques.)
An international multidisciplinary group, SCENIC (Surveillance for Colorectal Endoscopic Neoplasia Detection and Management in Inflammatory Bowel Disease Patients: International Consensus), which represents a wide spectrum of stakeholders and attitudes regarding IBD surveillance, sought to develop unifying consensus recommendations addressing two issues: 1) how should surveillance colonoscopy to detect dysplasia be performed, and 2) how should dysplasia identified at colonoscopy be managed. The SCENIC group adhered to suggested standards for guideline development from the Institute of Medicine and others and that incorporated the GRADE methodology. A systematic review was performed for each focused clinical question, followed by a review of a full synthesis of evidence by panelists.
SCENIC key summary recommendations
Detection
• High definition is recommended over standard definition for performance of surveillance colonoscopy.
• Routine performance of chromoendoscopy during IBD surveillance is suggested as an adjunct to high-definition colonoscopy.
• Narrowband imaging is not recommended as an alternative for high-definition, white-light colonoscopy or chromoendoscopy.
• No specific recommendation on performance of random biopsies was made in patients undergoing high-definition, white-light colonoscopy plus chromoendoscopy. The panel did not reach consensus on this topic because 60% of the panel members disagreed with performing random biopsies during chromoendoscopy, and a recommendation required 80% agreement or disagreement.
Management
• When dysplasia is detected, it should be characterized as “endoscopically resectable” or “nonendoscopically resectable” (The terms “dysplasia-associated lesion or mass (DALM),” “adenoma-like,” and “nonadenoma-like” should be abandoned).
• Visible dysplasia should be characterized according to the Paris classification polypoid or nonpolypoid, with modifications including the addition of terms for ulceration and border of the lesion.
• The term endoscopically resectable indicates that 1) distinct margins of the lesion could be identified, 2) the lesion appears to be completely removed on visual inspection after endoscopic resection, 3) histologic examination of the resected specimen is consistent with complete removal, and 4) biopsy specimens taken from mucosa immediately adjacent to the resection site are free of dysplasia on histologic examination.
• After complete removal of endoscopically resectable polypoid or nonpolypoid dysplasia, surveillance colonoscopy is recommended rather than colectomy.
• For patients with endoscopically invisible dysplasia (confirmed by a GI pathologist), referral is suggested to an endoscopist with expertise in IBD surveillance using chromoendoscopy with high-definition colonoscopy.
The SCENIC recommendations aim to optimize the detection and management of dysplasia in IBD patients. Future research in IBD surveillance should assess the potential for chromoendoscopy to improve risk stratification to elucidate optimal surveillance intervals, and the impact on CRC incidence and mortality. In addition, the role of resection of nonpolypoid dysplasia in the reduction in CRC incidence or need for colectomy requires further investigation.
Dr. Kaltenbach is a gastroenterologist at Veterans Affairs, and a clinical assistant professor of medicine at Stanford (Calif.) University. She has no conflicts of interest. Her comments were made during the ASGE and AGA joint Presidential Plenary at the annual Digestive Disease Week.
Optimizing colonoscopy quality in patients with ulcerative colitis or Crohn’s disease involving the colon is important. Their risk for the development of colorectal cancer (CRC) and of interval CRC is significantly higher compared with the non–inflammatory bowel disease (IBD) population.
Most CRC cases in IBD are believed to arise from dysplasia, and thus, surveillance colonoscopy is recommended to detect dysplasia. Key factors that influence the success of surveillance colonoscopy in IBD patients include: 1) endoscopic recognition of dysplasia, 2) adequacy of mucosal sampling, 3) awareness of interfering anatomy, such as strictures and pseudopolyps, 4) appropriate differentiation of dysplastic lesions as endoscopically resectable, 5) complete removal of endoscopically resectable dysplasia, and 6) patient compliance.
Over a decade ago, we learned that most dysplasia discovered in patients with IBD is actually visible. The use of high-definition video-endoscopy and newer methods, such as chromoendoscopy with mucosal dye spraying, enhance the detection of dysplasia. Today, with the widespread use of newer technologies and techniques, the literature indicates that targeted biopsies of visible lesions account for approximately 90% of cases, whereas random biopsy (resulting in detection of an endoscopically invisible lesion) accounts for only 10% of cases of identified dysplasia.
The endoscopic recognition of dysplastic colorectal lesions may have important implications for the surveillance and management of dysplasia, and shift it away from the traditional random biopsy technique, where less than 0.1% of the colonic mucosal surface area is sampled, and from colectomy for any diagnosis of dysplasia.
Enhanced endoscopy techniques such as chromoendoscopy can have a substantial impact upon IBD surveillance, increasing the dysplasia detection rates, as well as informing management decisions. Chromoendoscopy, using a dye solution of either methylene blue or indigo carmine applied onto the colonic mucosa to enhance contrast during surveillance colonoscopy, is performed either in a pancolonic fashion to detect lesions or in a targeted fashion to allow for detailed viewing of an identified lesion (Figure 1).
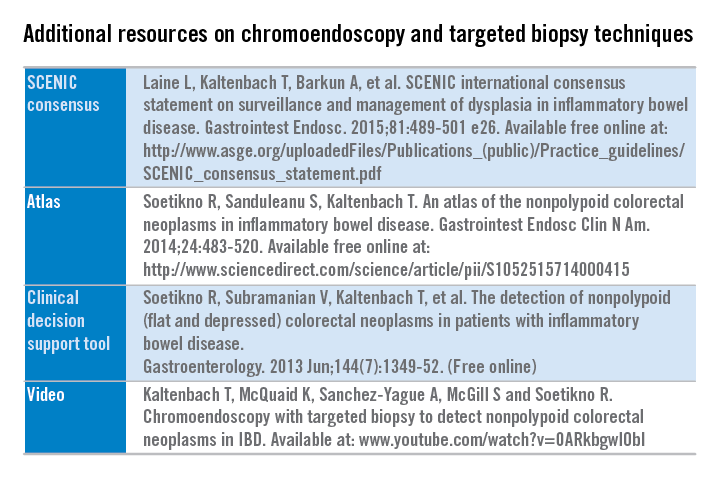
Additional resources are freely available detailing the technique and suggested steps to implement chromoendoscopy into practice. (See additional resources on chromoendoscopy and targeted biopsy techniques.)
An international multidisciplinary group, SCENIC (Surveillance for Colorectal Endoscopic Neoplasia Detection and Management in Inflammatory Bowel Disease Patients: International Consensus), which represents a wide spectrum of stakeholders and attitudes regarding IBD surveillance, sought to develop unifying consensus recommendations addressing two issues: 1) how should surveillance colonoscopy to detect dysplasia be performed, and 2) how should dysplasia identified at colonoscopy be managed. The SCENIC group adhered to suggested standards for guideline development from the Institute of Medicine and others and that incorporated the GRADE methodology. A systematic review was performed for each focused clinical question, followed by a review of a full synthesis of evidence by panelists.
SCENIC key summary recommendations
Detection
• High definition is recommended over standard definition for performance of surveillance colonoscopy.
• Routine performance of chromoendoscopy during IBD surveillance is suggested as an adjunct to high-definition colonoscopy.
• Narrowband imaging is not recommended as an alternative for high-definition, white-light colonoscopy or chromoendoscopy.
• No specific recommendation on performance of random biopsies was made in patients undergoing high-definition, white-light colonoscopy plus chromoendoscopy. The panel did not reach consensus on this topic because 60% of the panel members disagreed with performing random biopsies during chromoendoscopy, and a recommendation required 80% agreement or disagreement.
Management
• When dysplasia is detected, it should be characterized as “endoscopically resectable” or “nonendoscopically resectable” (The terms “dysplasia-associated lesion or mass (DALM),” “adenoma-like,” and “nonadenoma-like” should be abandoned).
• Visible dysplasia should be characterized according to the Paris classification polypoid or nonpolypoid, with modifications including the addition of terms for ulceration and border of the lesion.
• The term endoscopically resectable indicates that 1) distinct margins of the lesion could be identified, 2) the lesion appears to be completely removed on visual inspection after endoscopic resection, 3) histologic examination of the resected specimen is consistent with complete removal, and 4) biopsy specimens taken from mucosa immediately adjacent to the resection site are free of dysplasia on histologic examination.
• After complete removal of endoscopically resectable polypoid or nonpolypoid dysplasia, surveillance colonoscopy is recommended rather than colectomy.
• For patients with endoscopically invisible dysplasia (confirmed by a GI pathologist), referral is suggested to an endoscopist with expertise in IBD surveillance using chromoendoscopy with high-definition colonoscopy.
The SCENIC recommendations aim to optimize the detection and management of dysplasia in IBD patients. Future research in IBD surveillance should assess the potential for chromoendoscopy to improve risk stratification to elucidate optimal surveillance intervals, and the impact on CRC incidence and mortality. In addition, the role of resection of nonpolypoid dysplasia in the reduction in CRC incidence or need for colectomy requires further investigation.
Dr. Kaltenbach is a gastroenterologist at Veterans Affairs, and a clinical assistant professor of medicine at Stanford (Calif.) University. She has no conflicts of interest. Her comments were made during the ASGE and AGA joint Presidential Plenary at the annual Digestive Disease Week.

