User login
Just three words—“My tummy hurts”—can mobilize a child’s parents into a high state of worry, especially on school days. They wonder: Is our child sick? Should he or she stay home? Why is this happening so often?
Although recurrent abdominal pain (RAP) is real, it usually is not caused by tissue damage or serious physical disease. When children with RAP are referred for psychiatric evaluation—often after extensive medical workups—we can help them and their parents manage the problem and function more normally. This article:
- describes physiologic mechanisms that may underlie recurrent GI distress
- discusses the high correlation of psychiatric comorbidities with RAP
- recommends judicious laboratory testing
- reviews evidence on medications and psychotherapies to improve RAP symptoms
- offers advice on building a therapeutic alliance with the patient and family.
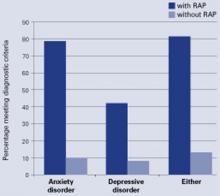
Figure Comorbid anxiety and depressive disorders in children with RAP
Children with functional RAP are much more likely to be anxious or depressed than similar pain-free children. A recent blinded study followed 80 children ages 8 to 15 (42 with RAP and 38 controls) identified through screening at primary care pediatric offices. Each was assessed using the Schedule for Affective Disorders and Schizophrenia for School Age Children, Present and Lifetime version (K-SADS-PL). Percentage meeting diagnostic criteria
Source: Reference 5.
RAP: A ‘Functional’ disorder
RAP is a somatoform (or “functional”) disorder, defined as physical symptoms not fully explained by a medical condition, effects of a substance, or another mental disorder. Symptoms cause distress and/or functional impairment and are not intentionally produced.1
A patient with RAP experiences at least three episodes of abdominal pain over 3 months that interfere with daily activities.2 RAP affects 7% to 25% of school-aged children and adolescents,3 most of whom have a functional disorder.4
RAP is equally common among prepubertal boys and girls but more common among girls during adolescence.3 RAP can impair school attendance and performance and stigmatize a child as “sickly.”
Common comorbid symptoms
Physical. Besides stomach pain, children with RAP often experience headaches (including migraines), other GI symptoms, general aches and pains, dizziness, and fatigue.
Patients with RAP who do not experience GI bleeding, anemia, fever, weight loss, growth failure, or persistent vomiting most likely do not have a serious underlying disease.
Psychiatric. Children with RAP have much higher rates of anxiety (80%) and depressive (40%) disorders than do their unaffected peers (Figure).5 We have also seen higher levels of suicidal thinking in children with RAP in primary care settings compared with pain-free controls (14% vs. 4%, P = 0.04; unpublished data).
In most cases, psychiatric comorbidities appear to precede or coincide with RAP onset. Separation fears, generalized anxiety, and social anxiety in particular are common in patients with RAP yet are seldom recognized in medical settings.
Having childhood RAP increases the risk of anxiety, depression, and hypochondriacal fears in adulthood.6 We do not know whether early intervention prevents later disability.
Use of medical services. Abdominal pain accounts for 2% to 4% of all pediatric office visits.7 In one study, 8% of middle school and high school students said they had visited a physician for evaluation of stomach pain during the previous year.8 Children with RAP make more ambulatory health and mental health visits than peers9 and are at risk for unnecessary and potentially dangerous medical tests, procedures, and treatments, including abdominal surgery.10
Four functional GI disorders
To better characterize youths with functional RAP, symptom-based criteria have been developed and applied for functional GI disorders, defined as chronic or recurrent GI symptoms without explanatory structural or biochemical abnormalities.11 Four such disorders are relevant in children with RAP.
Irritable bowel syndrome (IBS): RAP with at least two of the following symptoms: relief with defecation, change in stool frequency, and change in stool form or appearance (occurs in approximately 50% of RAP cases).
Functional dyspepsia: RAP centered in the upper abdomen that is not associated with changes in bowel habits.
Abdominal migraine: Paroxysmal midline abdominal pain lasting 2 hours to several days with symptom-free intervals of weeks to months and at least two of the following: headache during episodes, photophobia during episodes, unilateral headache, aura, and a family history of migraine.
Functional abdominal pain: Continuous or nearly continuous abdominal pain for 6 months or more.
The reliability, validity, and clinical relevance of these criteria have not been demonstrated. Some children with RAP do not meet any criteria for a specific functional GI disorder.
Gut-brain connections. RAP may be associated with a heightened sensitivity to visceral sensations (visceral hyperalgesia) and a low pressure-pain threshold, leading to speculation that these children are hypersensitive to pain.
High rates of anxiety disorders and temperamental harm avoidance also are seen in patients with RAP, along with a tendency to develop pain when faced with unexpected events. Whether these children are more likely than others to perceive novel internal or external perceptions as threatening is open to debate.
Table 1
Recurrent abdominal pain: 8 steps to assessment and diagnosis
|
Serotonin communicates nociceptive information between the gut and brain and may mediate visceral hyperalgesia. Gut enterochromaffin cells contain more than 90% of the body’s total serotonin. They act as sensory transducers, releasing serotonin in response to increased intraluminal pressure or inflammation.
The released serotonin can cause abdominal discomfort by stimulating 5-HT 3 receptors on vagal afferents and can influence gut peristaltic activity by stimulating enteric afferents. The same serotonin transporter responsible for CNS serotonin reuptake is expressed throughout the gut.
A constellation of clues
The ideal RAP evaluation includes information from the child, parents, educators, and other health care professionals (Table 1).
Begin by acknowledging the patient’s suffering and the parent’s concerns; do not challenge the pain’s subjective reality. Rather than prejudging its cause, document the pain’s timing, context, and characteristics, and review the patient’s history. A constellation of clues is most suggestive of RAP (Table 2); single clues are not definitive.12,13
Table 2
Clues that suggest functional pain*
|
| * No single clue is definitive. |
| Source: Adapted from reference 12. |
Diagnostic testing. Be judicious in selecting diagnostic tests and procedures. Continuing to order studies in a haphazard effort to rule out disease can generate concerns that “the doctor doesn’t know what’s wrong” and heighten the family’s fear that a disease has been missed.
The process of “ruling out” physical disease may have no apparent end. Unless you are reasonably comfortable that a serious physical disease has not been missed, it is difficult to explain RAP to the patient and family and lay the foundation for intervention.
On the other hand, you must balance the importance of minimizing your own and the family’s anxiety about unrecognized disease against the physical and psychological risks and costs associated with medical tests and procedures.
Social assessment. Assess social and familial reinforcement (secondary gain) of the pain. Parents sometimes inadvertently encourage their children’s sick-role behaviors by providing excessive attention, rewards, or opportunities to avoid uncomfortable situations. RAP can become an excuse for poor performance (self-handicapping), particularly in children with a learning disorder.
How to deliver the diagnosis
Functional abdominal pain is essentially a clinical diagnosis that relies on presentation, course, and findings. As mentioned, a constellation of “clues” is most supportive, as is having typical IBS symptoms.
Before declaring the diagnosis, discuss with the family the patient’s physical, emotional, and behavioral symptoms and the context in which RAP developed. Doing so can help maintain your credibility and establish a consensus.
Once you declare the diagnosis, discuss it clearly and frankly. Families are not likely to be reassured if you do not offer a plausible explanation for the lack of physical findings.
Precautions. When a definitive diagnosis is not possible, acknowledge that uncertainty. Although you must discuss any recognized psychiatric comorbidity, attempting to “explain” that the disorder is causing the pain is usually impractical and intellectually dishonest.
Also, given the pervasive nature of stigma, do not convey embarrassment or unease about diagnosing functional RAP or any comorbid psychiatric disorder.
Follow-up testing. Once you diagnose functional RAP, further testing is generally not necessary. Tests might be indicated if you:
- receive new information
- observe a change in clinical status
- or are convinced that treatment will not work unless the family is reassured by further investigation.
Collaborative treatment
Reassurance and education. Reassurance that the patient does not have a serious physical disease is necessary but rarely sufficient. Explain that the child’s pain does not appear to reflect tissue damage and is not threatening. On the other hand, avoid giving excessive reassurance, particularly when obsessional illness worry and hypochondriacal fears are prominent. Address illness worry as a problem to be solved together.
Discuss with the patient and family what is known and not known about functional RAP, and encourage them to ask questions. This is an opportunity for you to instill hope and cultivate positive expectations, but avoid promising cure. Discuss the gut-brain connection and relevance of visceral hyperalgesia, including serotonin’s potential roles in RAP pathogenesis.
Partners in care. Collaborative treatment increases the likelihood of success. Discuss the importance of a therapeutic partnership, and clarify any areas of disagreement with the diagnosis or treatment plan.
Clearly delineate your roles and responsibilities and those of the patient, family, and other health care team members. Poor communication is pediatricians’ most common complaint about psychiatrists.14 Good interdisciplinary communication decreases the chance that treatment strategies will be duplicated, diluted, or misinterpreted.
Consolidate medical care with a single clinician—often the primary care physician—based on discussions with the patient, family, and health care team. The coordinating clinician can mediate between the school and family when tensions develop over poor attendance or requests for special treatment. It is often useful for this clinician to spell out:
- what constitutes a legitimate medical excuse for school absence
- who will legitimize excuses.
All parties should understand that the school will view an unexcused absence as truancy and act appropriately.
Diet and lifestyle. Encourage the patient to maintain a regular schedule and a healthy diet. Specific dietary interventions have not been proven effective, despite speculation that lack of dietary fiber or lactose intolerance might cause RAP.15,16 Also encourage adequate sleep and regular exercise.
Medication and psychotherapy
Because no strong evidence-based guidelines address pediatric RAP intervention, family preferences usually guide initial treatment decisions. This highlights the importance of good communication and a therapeutic partnership among the clinician, family, and patient.
Antispasmodics, acid reducers, and antidepressants are commonly prescribed for RAP, though none are well-supported in the literature and no controlled studies have gauged medication’s impact on psychiatric comorbidity.16
Antidepressants. Selective serotonin reuptake inhibitors (SSRIs) might help relieve RAP symptoms, but the evidence is inconclusive. SSRIs are considered potentially beneficial in RAP because they may help communicate nociceptive information between the gut and brain and mediate visceral hyperalgesia.
SSRIs at first may increase serotonin at the synapse, which one might assume would to worsen abdominal symptoms. However, ongoing SSRI use could “down-regulate” postsynaptic 5-HT3 receptors and desensitize postsynaptic cells to the effects of local serotonin.
Our group recently conducted a 12-week open trial of citalopram for functional pediatric RAP.17 The 25 participants received 10 mg/d the first week, then 20 mg/d thereafter if tolerated. At week 4, nonresponders and partial responders who were tolerating the medication began receiving 40 mg/d.
Table 3
SSRI daily dosing for pediatric RAP
| Drug | Starting dosage* | Target dosage† | Maximum dosage‡ |
|---|---|---|---|
| Citalopram | 10 mg | 20 mg | 40 to 60 mg |
| Escitalopram | 5 mg | 10 mg | 20 to 30 mg |
| Fluoxetine | 10 mg | 20 mg | 40 mg |
| Fluvoxamine | 50 mg | 100 mg | 300 mg |
| Sertraline | 25 mg | 50 mg | 200 mg |
| * First 3 to 7 days. | |||
| † If patient tolerates starting dosage, increase to target dosage. | |||
| ‡ If patient does not respond to target dosage in 2 to 3 weeks, consider increasing the dosage. | |||
At trial’s end, more than two-thirds of participants were taking 40 mg/d. We rated 21 of 25 patients (84%) as “much improved” or “very much improved,” using the Clinical Global Impression-Improvement scale. Abdominal pain, anxiety, depression, other somatic symptoms, and functional impairment all improved significantly during treatment. Suicidal thoughts diminished progressively from baseline, and no patient reported suicidal thinking at study’s end. Citalopram was generally well tolerated.
With SSRI treatment, start at a low dosage for 3 to 7 days (Table 3). If tolerated, increase to a typical therapeutic dosage. If symptoms fail to respond after 2 or 3 weeks, consider a higher dosage. A short course of an oral benzodiazepine (such as clonazepam, 0.25 mg bid) during the first weeks of SSRI treatment sometimes helps particularly anxious patients or those whose pain appears closely associated with anxiety or “stress.”
Pediatric gastroenterologists often prescribe a low-dose tricyclic antidepressant as first-line therapy, but we discourage this. TCAs lack efficacy in pediatric depression and pose a greater risk of side effects and safety concerns than SSRIs.18
Other agents have been tried for RAP-associated conditions:
Famotidine, a histamine type 2 receptor blocker, may reduce pain in children with dyspepsia and RAP.19
Peppermint oil reduced abdominal pain in one study of children with IBS but had little effect on other symptoms.20
Medications such as alosetron and tegaserod that interrupt serotonergic neurotransmission in the gut have shown benefit in adults with IBS but have not been studied in children.
Psychotherapy. A few small studies suggest that cognitive-behavioral therapies (CBT) are helpful in RAP, but CBT may be difficult to deliver in medical settings.21,22 A simplified “rehabilitative” approach that incorporates CBT principles involves having the clinician and patient view RAP as a challenge to be overcome, rather than a burden to be endured. Such an approach emphasizes the child’s fundamental strength and adaptability rather than vulnerabilities.
The goal of therapy is redirected from finding a cure to coping with and overcoming the problem. This approach challenges the notion that the child cannot resume normal function until the pain is completely gone. It encourages active, problem-focused coping, and discourages passive acceptance—which is associated with greater symptom burden and functional impairment.
Work with parents to reinforce the child’s health-promoting behaviors and minimize negative and social reinforcements (secondary gain) associated with RAP. Advise parents to:
- encourage and reward full school attendance
- avoid home-bound instruction
- expect the child to function despite physical distress
- insist that the child perform age-appropriate household chores and other responsibilities.
Self-management skills—such as relaxation training, hypnosis, biofeedback, and guided imagery—may help reduce pain and manage physiologic arousal.16 Deception strategies such as placebo or sham interventions are unethical and impractical.
Related resources
- Campo JV. Functional recurrent abdominal pain in children and adolescents. Digestive Health Matters 2003;12(3):15-7.
- International Foundation for Functional Gastrointestinal Disorders. www.iffgd.org
- University of Pittsburgh. Advanced Center for Interventions and Services Research on Early Onset Mood and Anxiety Disorders. www.moodykids.org
Drug brand names
- Alosetron • Lotronex
- Citalopram • Celexa
- Clonazepam • Klonopin
- Escitalopram • Lexapro
- Famotidine • Pepcid
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Sertraline • Zoloft
- Tegaserod • Zelnorm
Disclosure
Dr. Campo’s work has been supported by the National Institute of Mental Health (grant MH01780) and in part by the Advanced Center for Interventions and Services Research on Early Onset Mood and Anxiety Disorders (grant MH66371). He also receives grants from Forest Pharmaceuticals and is a consultant to Eli Lilly and Co.
1. American Psychiatric Association Diagnostic and statistical manual of mental disorders (4th ed, revised). Washington, DC: American Psychiatric Association, 2000.
2. Apley J, Naish N. Recurrent abdominal pains: a field survey of 1,000 school children. Arch Dis Child 1958;33(168):165-70.
3. Scharff L. Recurrent abdominal pain in children: a review of psychological factors and treatment. Clin Psychol Rev 1997;17(2):145-66.
4. Boyle JT. Recurrent abdominal pain: an update. Pediatr Rev 1997;18(9):310-20.
5. Campo JV, Bridge J, Ehmann M, et al. Recurrent abdominal pain, anxiety, and depression in primary care. Pediatrics 2004;113(4):817-24.
6. Campo JV, Di Lorenzo C, Chiappetta L, et al. Adult outcomes of pediatric recurrent abdominal pain: do they just grow out of it? Pediatrics 2001;108(1):E1.-
7. Starfield B, Gross E, Wood M, et al. Psychosocial and psychosomatic diagnoses in primary care of children. Pediatrics 1980;66(2):159-67.
8. Hyams JS, Burke G, Davis PM, et al. Abdominal pain and irritable bowel syndrome in adolescents: a community-based study. J Pediatr 1996;129(2):220-6.
9. Campo JV, Comer DM, Jansen-McWilliams L, et al. Recurrent pain, emotional distress, and health service use in childhood. J Pediatr 2002;141(1):76-83.
10. Stickler GB, Murphy DB. Recurrent abdominal pain. Am J Dis Child 1979;133(5):486-9.
11. Rasquin-Weber A, Hyman PE, Cucchiara S, et al. Childhood functional gastrointestinal disorders. Gut 1999;45(suppl 2):II60-8.
12. Campo JV, Fritz G. A management model for pediatric somatization. Psychosomatics 2001;42(6):467-76.
13. Campo JV, Garber J. Somatization. In: Ammerman RT, Campo JV (eds). Handbook of pediatric psychology and psychiatry. Vol 1 Boston: Allyn and Bacon, 1998;137-61.
14. Fritz GK, Bergman AS. Child psychiatrists seen through pediatricians’ eyes: results of a national survey. J Am Acad Child Psychiatry 1985;24(1):81-6.
15. Huertas-Ceballos A, Macarthur C, Logan S. Dietary interventions for recurrent abdominal pain (RAP) in childhood. Cochrane Database Syst Rev 2002;(2):CD003019.-
16. Weydert JA, Ball TM, Davis MF. Systematic review of treatments for recurrent abdominal pain. Pediatrics 2003;111(1):e1-11.
17. Campo JV, Perel J, Lucas A, et al. Citalopram treatment of pediatric recurrent abdominal pain and comorbid internalizing disorders: An exploratory study (poster). Miami Beach, FL: American Academy of Child and Adolescent Psychiatry annual meeting, October 2003.
18. Geller B, Reising D, Leonard HL, et al. Critical review of tricyclic antidepressant use in children and adolescents. J Am Acad Child Adolesc Psychiatry 1999;38(5):513-6.
19. See MC, Birnbaum AH, Schechter CB, et al. Double-blind, placebo-controlled trial of famotidine in children with abdominal pain and dyspepsia: global and quantitative assessment. Dig Dis Sci 2001;46(5):985-92.
20. Kline RM, Kline JJ, Di Palma J, Barbero GJ. Enteric-coated, pH-dependent peppermint oil capsules for the treatment of irritable bowel syndrome in children. J Pediatr 2001;138(1):125-8.
21. Sanders MR, Rebgetz M, Morrison M, et al. Cognitive-behavioral treatment of recurrent nonspecific abdominal pain in children: an analysis of generalization, maintenance, and side effects. J Consult Clin Psychol 1989;57(2):294-300.
22. Sanders MR, Shepherd RW, Cleghorn G, Woolford H. The treatment of recurrent abdominal pain in children: a controlled comparison of cognitive-behavioral family intervention and standard pediatric care. J Consult Clin Psychol 1994;62(2):306-14.
Just three words—“My tummy hurts”—can mobilize a child’s parents into a high state of worry, especially on school days. They wonder: Is our child sick? Should he or she stay home? Why is this happening so often?
Although recurrent abdominal pain (RAP) is real, it usually is not caused by tissue damage or serious physical disease. When children with RAP are referred for psychiatric evaluation—often after extensive medical workups—we can help them and their parents manage the problem and function more normally. This article:
- describes physiologic mechanisms that may underlie recurrent GI distress
- discusses the high correlation of psychiatric comorbidities with RAP
- recommends judicious laboratory testing
- reviews evidence on medications and psychotherapies to improve RAP symptoms
- offers advice on building a therapeutic alliance with the patient and family.
Figure Comorbid anxiety and depressive disorders in children with RAP
Children with functional RAP are much more likely to be anxious or depressed than similar pain-free children. A recent blinded study followed 80 children ages 8 to 15 (42 with RAP and 38 controls) identified through screening at primary care pediatric offices. Each was assessed using the Schedule for Affective Disorders and Schizophrenia for School Age Children, Present and Lifetime version (K-SADS-PL). Percentage meeting diagnostic criteria
Source: Reference 5.
RAP: A ‘Functional’ disorder
RAP is a somatoform (or “functional”) disorder, defined as physical symptoms not fully explained by a medical condition, effects of a substance, or another mental disorder. Symptoms cause distress and/or functional impairment and are not intentionally produced.1
A patient with RAP experiences at least three episodes of abdominal pain over 3 months that interfere with daily activities.2 RAP affects 7% to 25% of school-aged children and adolescents,3 most of whom have a functional disorder.4
RAP is equally common among prepubertal boys and girls but more common among girls during adolescence.3 RAP can impair school attendance and performance and stigmatize a child as “sickly.”
Common comorbid symptoms
Physical. Besides stomach pain, children with RAP often experience headaches (including migraines), other GI symptoms, general aches and pains, dizziness, and fatigue.
Patients with RAP who do not experience GI bleeding, anemia, fever, weight loss, growth failure, or persistent vomiting most likely do not have a serious underlying disease.
Psychiatric. Children with RAP have much higher rates of anxiety (80%) and depressive (40%) disorders than do their unaffected peers (Figure).5 We have also seen higher levels of suicidal thinking in children with RAP in primary care settings compared with pain-free controls (14% vs. 4%, P = 0.04; unpublished data).
In most cases, psychiatric comorbidities appear to precede or coincide with RAP onset. Separation fears, generalized anxiety, and social anxiety in particular are common in patients with RAP yet are seldom recognized in medical settings.
Having childhood RAP increases the risk of anxiety, depression, and hypochondriacal fears in adulthood.6 We do not know whether early intervention prevents later disability.
Use of medical services. Abdominal pain accounts for 2% to 4% of all pediatric office visits.7 In one study, 8% of middle school and high school students said they had visited a physician for evaluation of stomach pain during the previous year.8 Children with RAP make more ambulatory health and mental health visits than peers9 and are at risk for unnecessary and potentially dangerous medical tests, procedures, and treatments, including abdominal surgery.10
Four functional GI disorders
To better characterize youths with functional RAP, symptom-based criteria have been developed and applied for functional GI disorders, defined as chronic or recurrent GI symptoms without explanatory structural or biochemical abnormalities.11 Four such disorders are relevant in children with RAP.
Irritable bowel syndrome (IBS): RAP with at least two of the following symptoms: relief with defecation, change in stool frequency, and change in stool form or appearance (occurs in approximately 50% of RAP cases).
Functional dyspepsia: RAP centered in the upper abdomen that is not associated with changes in bowel habits.
Abdominal migraine: Paroxysmal midline abdominal pain lasting 2 hours to several days with symptom-free intervals of weeks to months and at least two of the following: headache during episodes, photophobia during episodes, unilateral headache, aura, and a family history of migraine.
Functional abdominal pain: Continuous or nearly continuous abdominal pain for 6 months or more.
The reliability, validity, and clinical relevance of these criteria have not been demonstrated. Some children with RAP do not meet any criteria for a specific functional GI disorder.
Gut-brain connections. RAP may be associated with a heightened sensitivity to visceral sensations (visceral hyperalgesia) and a low pressure-pain threshold, leading to speculation that these children are hypersensitive to pain.
High rates of anxiety disorders and temperamental harm avoidance also are seen in patients with RAP, along with a tendency to develop pain when faced with unexpected events. Whether these children are more likely than others to perceive novel internal or external perceptions as threatening is open to debate.
Table 1
Recurrent abdominal pain: 8 steps to assessment and diagnosis
|
Serotonin communicates nociceptive information between the gut and brain and may mediate visceral hyperalgesia. Gut enterochromaffin cells contain more than 90% of the body’s total serotonin. They act as sensory transducers, releasing serotonin in response to increased intraluminal pressure or inflammation.
The released serotonin can cause abdominal discomfort by stimulating 5-HT 3 receptors on vagal afferents and can influence gut peristaltic activity by stimulating enteric afferents. The same serotonin transporter responsible for CNS serotonin reuptake is expressed throughout the gut.
A constellation of clues
The ideal RAP evaluation includes information from the child, parents, educators, and other health care professionals (Table 1).
Begin by acknowledging the patient’s suffering and the parent’s concerns; do not challenge the pain’s subjective reality. Rather than prejudging its cause, document the pain’s timing, context, and characteristics, and review the patient’s history. A constellation of clues is most suggestive of RAP (Table 2); single clues are not definitive.12,13
Table 2
Clues that suggest functional pain*
|
| * No single clue is definitive. |
| Source: Adapted from reference 12. |
Diagnostic testing. Be judicious in selecting diagnostic tests and procedures. Continuing to order studies in a haphazard effort to rule out disease can generate concerns that “the doctor doesn’t know what’s wrong” and heighten the family’s fear that a disease has been missed.
The process of “ruling out” physical disease may have no apparent end. Unless you are reasonably comfortable that a serious physical disease has not been missed, it is difficult to explain RAP to the patient and family and lay the foundation for intervention.
On the other hand, you must balance the importance of minimizing your own and the family’s anxiety about unrecognized disease against the physical and psychological risks and costs associated with medical tests and procedures.
Social assessment. Assess social and familial reinforcement (secondary gain) of the pain. Parents sometimes inadvertently encourage their children’s sick-role behaviors by providing excessive attention, rewards, or opportunities to avoid uncomfortable situations. RAP can become an excuse for poor performance (self-handicapping), particularly in children with a learning disorder.
How to deliver the diagnosis
Functional abdominal pain is essentially a clinical diagnosis that relies on presentation, course, and findings. As mentioned, a constellation of “clues” is most supportive, as is having typical IBS symptoms.
Before declaring the diagnosis, discuss with the family the patient’s physical, emotional, and behavioral symptoms and the context in which RAP developed. Doing so can help maintain your credibility and establish a consensus.
Once you declare the diagnosis, discuss it clearly and frankly. Families are not likely to be reassured if you do not offer a plausible explanation for the lack of physical findings.
Precautions. When a definitive diagnosis is not possible, acknowledge that uncertainty. Although you must discuss any recognized psychiatric comorbidity, attempting to “explain” that the disorder is causing the pain is usually impractical and intellectually dishonest.
Also, given the pervasive nature of stigma, do not convey embarrassment or unease about diagnosing functional RAP or any comorbid psychiatric disorder.
Follow-up testing. Once you diagnose functional RAP, further testing is generally not necessary. Tests might be indicated if you:
- receive new information
- observe a change in clinical status
- or are convinced that treatment will not work unless the family is reassured by further investigation.
Collaborative treatment
Reassurance and education. Reassurance that the patient does not have a serious physical disease is necessary but rarely sufficient. Explain that the child’s pain does not appear to reflect tissue damage and is not threatening. On the other hand, avoid giving excessive reassurance, particularly when obsessional illness worry and hypochondriacal fears are prominent. Address illness worry as a problem to be solved together.
Discuss with the patient and family what is known and not known about functional RAP, and encourage them to ask questions. This is an opportunity for you to instill hope and cultivate positive expectations, but avoid promising cure. Discuss the gut-brain connection and relevance of visceral hyperalgesia, including serotonin’s potential roles in RAP pathogenesis.
Partners in care. Collaborative treatment increases the likelihood of success. Discuss the importance of a therapeutic partnership, and clarify any areas of disagreement with the diagnosis or treatment plan.
Clearly delineate your roles and responsibilities and those of the patient, family, and other health care team members. Poor communication is pediatricians’ most common complaint about psychiatrists.14 Good interdisciplinary communication decreases the chance that treatment strategies will be duplicated, diluted, or misinterpreted.
Consolidate medical care with a single clinician—often the primary care physician—based on discussions with the patient, family, and health care team. The coordinating clinician can mediate between the school and family when tensions develop over poor attendance or requests for special treatment. It is often useful for this clinician to spell out:
- what constitutes a legitimate medical excuse for school absence
- who will legitimize excuses.
All parties should understand that the school will view an unexcused absence as truancy and act appropriately.
Diet and lifestyle. Encourage the patient to maintain a regular schedule and a healthy diet. Specific dietary interventions have not been proven effective, despite speculation that lack of dietary fiber or lactose intolerance might cause RAP.15,16 Also encourage adequate sleep and regular exercise.
Medication and psychotherapy
Because no strong evidence-based guidelines address pediatric RAP intervention, family preferences usually guide initial treatment decisions. This highlights the importance of good communication and a therapeutic partnership among the clinician, family, and patient.
Antispasmodics, acid reducers, and antidepressants are commonly prescribed for RAP, though none are well-supported in the literature and no controlled studies have gauged medication’s impact on psychiatric comorbidity.16
Antidepressants. Selective serotonin reuptake inhibitors (SSRIs) might help relieve RAP symptoms, but the evidence is inconclusive. SSRIs are considered potentially beneficial in RAP because they may help communicate nociceptive information between the gut and brain and mediate visceral hyperalgesia.
SSRIs at first may increase serotonin at the synapse, which one might assume would to worsen abdominal symptoms. However, ongoing SSRI use could “down-regulate” postsynaptic 5-HT3 receptors and desensitize postsynaptic cells to the effects of local serotonin.
Our group recently conducted a 12-week open trial of citalopram for functional pediatric RAP.17 The 25 participants received 10 mg/d the first week, then 20 mg/d thereafter if tolerated. At week 4, nonresponders and partial responders who were tolerating the medication began receiving 40 mg/d.
Table 3
SSRI daily dosing for pediatric RAP
| Drug | Starting dosage* | Target dosage† | Maximum dosage‡ |
|---|---|---|---|
| Citalopram | 10 mg | 20 mg | 40 to 60 mg |
| Escitalopram | 5 mg | 10 mg | 20 to 30 mg |
| Fluoxetine | 10 mg | 20 mg | 40 mg |
| Fluvoxamine | 50 mg | 100 mg | 300 mg |
| Sertraline | 25 mg | 50 mg | 200 mg |
| * First 3 to 7 days. | |||
| † If patient tolerates starting dosage, increase to target dosage. | |||
| ‡ If patient does not respond to target dosage in 2 to 3 weeks, consider increasing the dosage. | |||
At trial’s end, more than two-thirds of participants were taking 40 mg/d. We rated 21 of 25 patients (84%) as “much improved” or “very much improved,” using the Clinical Global Impression-Improvement scale. Abdominal pain, anxiety, depression, other somatic symptoms, and functional impairment all improved significantly during treatment. Suicidal thoughts diminished progressively from baseline, and no patient reported suicidal thinking at study’s end. Citalopram was generally well tolerated.
With SSRI treatment, start at a low dosage for 3 to 7 days (Table 3). If tolerated, increase to a typical therapeutic dosage. If symptoms fail to respond after 2 or 3 weeks, consider a higher dosage. A short course of an oral benzodiazepine (such as clonazepam, 0.25 mg bid) during the first weeks of SSRI treatment sometimes helps particularly anxious patients or those whose pain appears closely associated with anxiety or “stress.”
Pediatric gastroenterologists often prescribe a low-dose tricyclic antidepressant as first-line therapy, but we discourage this. TCAs lack efficacy in pediatric depression and pose a greater risk of side effects and safety concerns than SSRIs.18
Other agents have been tried for RAP-associated conditions:
Famotidine, a histamine type 2 receptor blocker, may reduce pain in children with dyspepsia and RAP.19
Peppermint oil reduced abdominal pain in one study of children with IBS but had little effect on other symptoms.20
Medications such as alosetron and tegaserod that interrupt serotonergic neurotransmission in the gut have shown benefit in adults with IBS but have not been studied in children.
Psychotherapy. A few small studies suggest that cognitive-behavioral therapies (CBT) are helpful in RAP, but CBT may be difficult to deliver in medical settings.21,22 A simplified “rehabilitative” approach that incorporates CBT principles involves having the clinician and patient view RAP as a challenge to be overcome, rather than a burden to be endured. Such an approach emphasizes the child’s fundamental strength and adaptability rather than vulnerabilities.
The goal of therapy is redirected from finding a cure to coping with and overcoming the problem. This approach challenges the notion that the child cannot resume normal function until the pain is completely gone. It encourages active, problem-focused coping, and discourages passive acceptance—which is associated with greater symptom burden and functional impairment.
Work with parents to reinforce the child’s health-promoting behaviors and minimize negative and social reinforcements (secondary gain) associated with RAP. Advise parents to:
- encourage and reward full school attendance
- avoid home-bound instruction
- expect the child to function despite physical distress
- insist that the child perform age-appropriate household chores and other responsibilities.
Self-management skills—such as relaxation training, hypnosis, biofeedback, and guided imagery—may help reduce pain and manage physiologic arousal.16 Deception strategies such as placebo or sham interventions are unethical and impractical.
Related resources
- Campo JV. Functional recurrent abdominal pain in children and adolescents. Digestive Health Matters 2003;12(3):15-7.
- International Foundation for Functional Gastrointestinal Disorders. www.iffgd.org
- University of Pittsburgh. Advanced Center for Interventions and Services Research on Early Onset Mood and Anxiety Disorders. www.moodykids.org
Drug brand names
- Alosetron • Lotronex
- Citalopram • Celexa
- Clonazepam • Klonopin
- Escitalopram • Lexapro
- Famotidine • Pepcid
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Sertraline • Zoloft
- Tegaserod • Zelnorm
Disclosure
Dr. Campo’s work has been supported by the National Institute of Mental Health (grant MH01780) and in part by the Advanced Center for Interventions and Services Research on Early Onset Mood and Anxiety Disorders (grant MH66371). He also receives grants from Forest Pharmaceuticals and is a consultant to Eli Lilly and Co.
Just three words—“My tummy hurts”—can mobilize a child’s parents into a high state of worry, especially on school days. They wonder: Is our child sick? Should he or she stay home? Why is this happening so often?
Although recurrent abdominal pain (RAP) is real, it usually is not caused by tissue damage or serious physical disease. When children with RAP are referred for psychiatric evaluation—often after extensive medical workups—we can help them and their parents manage the problem and function more normally. This article:
- describes physiologic mechanisms that may underlie recurrent GI distress
- discusses the high correlation of psychiatric comorbidities with RAP
- recommends judicious laboratory testing
- reviews evidence on medications and psychotherapies to improve RAP symptoms
- offers advice on building a therapeutic alliance with the patient and family.
Figure Comorbid anxiety and depressive disorders in children with RAP
Children with functional RAP are much more likely to be anxious or depressed than similar pain-free children. A recent blinded study followed 80 children ages 8 to 15 (42 with RAP and 38 controls) identified through screening at primary care pediatric offices. Each was assessed using the Schedule for Affective Disorders and Schizophrenia for School Age Children, Present and Lifetime version (K-SADS-PL). Percentage meeting diagnostic criteria
Source: Reference 5.
RAP: A ‘Functional’ disorder
RAP is a somatoform (or “functional”) disorder, defined as physical symptoms not fully explained by a medical condition, effects of a substance, or another mental disorder. Symptoms cause distress and/or functional impairment and are not intentionally produced.1
A patient with RAP experiences at least three episodes of abdominal pain over 3 months that interfere with daily activities.2 RAP affects 7% to 25% of school-aged children and adolescents,3 most of whom have a functional disorder.4
RAP is equally common among prepubertal boys and girls but more common among girls during adolescence.3 RAP can impair school attendance and performance and stigmatize a child as “sickly.”
Common comorbid symptoms
Physical. Besides stomach pain, children with RAP often experience headaches (including migraines), other GI symptoms, general aches and pains, dizziness, and fatigue.
Patients with RAP who do not experience GI bleeding, anemia, fever, weight loss, growth failure, or persistent vomiting most likely do not have a serious underlying disease.
Psychiatric. Children with RAP have much higher rates of anxiety (80%) and depressive (40%) disorders than do their unaffected peers (Figure).5 We have also seen higher levels of suicidal thinking in children with RAP in primary care settings compared with pain-free controls (14% vs. 4%, P = 0.04; unpublished data).
In most cases, psychiatric comorbidities appear to precede or coincide with RAP onset. Separation fears, generalized anxiety, and social anxiety in particular are common in patients with RAP yet are seldom recognized in medical settings.
Having childhood RAP increases the risk of anxiety, depression, and hypochondriacal fears in adulthood.6 We do not know whether early intervention prevents later disability.
Use of medical services. Abdominal pain accounts for 2% to 4% of all pediatric office visits.7 In one study, 8% of middle school and high school students said they had visited a physician for evaluation of stomach pain during the previous year.8 Children with RAP make more ambulatory health and mental health visits than peers9 and are at risk for unnecessary and potentially dangerous medical tests, procedures, and treatments, including abdominal surgery.10
Four functional GI disorders
To better characterize youths with functional RAP, symptom-based criteria have been developed and applied for functional GI disorders, defined as chronic or recurrent GI symptoms without explanatory structural or biochemical abnormalities.11 Four such disorders are relevant in children with RAP.
Irritable bowel syndrome (IBS): RAP with at least two of the following symptoms: relief with defecation, change in stool frequency, and change in stool form or appearance (occurs in approximately 50% of RAP cases).
Functional dyspepsia: RAP centered in the upper abdomen that is not associated with changes in bowel habits.
Abdominal migraine: Paroxysmal midline abdominal pain lasting 2 hours to several days with symptom-free intervals of weeks to months and at least two of the following: headache during episodes, photophobia during episodes, unilateral headache, aura, and a family history of migraine.
Functional abdominal pain: Continuous or nearly continuous abdominal pain for 6 months or more.
The reliability, validity, and clinical relevance of these criteria have not been demonstrated. Some children with RAP do not meet any criteria for a specific functional GI disorder.
Gut-brain connections. RAP may be associated with a heightened sensitivity to visceral sensations (visceral hyperalgesia) and a low pressure-pain threshold, leading to speculation that these children are hypersensitive to pain.
High rates of anxiety disorders and temperamental harm avoidance also are seen in patients with RAP, along with a tendency to develop pain when faced with unexpected events. Whether these children are more likely than others to perceive novel internal or external perceptions as threatening is open to debate.
Table 1
Recurrent abdominal pain: 8 steps to assessment and diagnosis
|
Serotonin communicates nociceptive information between the gut and brain and may mediate visceral hyperalgesia. Gut enterochromaffin cells contain more than 90% of the body’s total serotonin. They act as sensory transducers, releasing serotonin in response to increased intraluminal pressure or inflammation.
The released serotonin can cause abdominal discomfort by stimulating 5-HT 3 receptors on vagal afferents and can influence gut peristaltic activity by stimulating enteric afferents. The same serotonin transporter responsible for CNS serotonin reuptake is expressed throughout the gut.
A constellation of clues
The ideal RAP evaluation includes information from the child, parents, educators, and other health care professionals (Table 1).
Begin by acknowledging the patient’s suffering and the parent’s concerns; do not challenge the pain’s subjective reality. Rather than prejudging its cause, document the pain’s timing, context, and characteristics, and review the patient’s history. A constellation of clues is most suggestive of RAP (Table 2); single clues are not definitive.12,13
Table 2
Clues that suggest functional pain*
|
| * No single clue is definitive. |
| Source: Adapted from reference 12. |
Diagnostic testing. Be judicious in selecting diagnostic tests and procedures. Continuing to order studies in a haphazard effort to rule out disease can generate concerns that “the doctor doesn’t know what’s wrong” and heighten the family’s fear that a disease has been missed.
The process of “ruling out” physical disease may have no apparent end. Unless you are reasonably comfortable that a serious physical disease has not been missed, it is difficult to explain RAP to the patient and family and lay the foundation for intervention.
On the other hand, you must balance the importance of minimizing your own and the family’s anxiety about unrecognized disease against the physical and psychological risks and costs associated with medical tests and procedures.
Social assessment. Assess social and familial reinforcement (secondary gain) of the pain. Parents sometimes inadvertently encourage their children’s sick-role behaviors by providing excessive attention, rewards, or opportunities to avoid uncomfortable situations. RAP can become an excuse for poor performance (self-handicapping), particularly in children with a learning disorder.
How to deliver the diagnosis
Functional abdominal pain is essentially a clinical diagnosis that relies on presentation, course, and findings. As mentioned, a constellation of “clues” is most supportive, as is having typical IBS symptoms.
Before declaring the diagnosis, discuss with the family the patient’s physical, emotional, and behavioral symptoms and the context in which RAP developed. Doing so can help maintain your credibility and establish a consensus.
Once you declare the diagnosis, discuss it clearly and frankly. Families are not likely to be reassured if you do not offer a plausible explanation for the lack of physical findings.
Precautions. When a definitive diagnosis is not possible, acknowledge that uncertainty. Although you must discuss any recognized psychiatric comorbidity, attempting to “explain” that the disorder is causing the pain is usually impractical and intellectually dishonest.
Also, given the pervasive nature of stigma, do not convey embarrassment or unease about diagnosing functional RAP or any comorbid psychiatric disorder.
Follow-up testing. Once you diagnose functional RAP, further testing is generally not necessary. Tests might be indicated if you:
- receive new information
- observe a change in clinical status
- or are convinced that treatment will not work unless the family is reassured by further investigation.
Collaborative treatment
Reassurance and education. Reassurance that the patient does not have a serious physical disease is necessary but rarely sufficient. Explain that the child’s pain does not appear to reflect tissue damage and is not threatening. On the other hand, avoid giving excessive reassurance, particularly when obsessional illness worry and hypochondriacal fears are prominent. Address illness worry as a problem to be solved together.
Discuss with the patient and family what is known and not known about functional RAP, and encourage them to ask questions. This is an opportunity for you to instill hope and cultivate positive expectations, but avoid promising cure. Discuss the gut-brain connection and relevance of visceral hyperalgesia, including serotonin’s potential roles in RAP pathogenesis.
Partners in care. Collaborative treatment increases the likelihood of success. Discuss the importance of a therapeutic partnership, and clarify any areas of disagreement with the diagnosis or treatment plan.
Clearly delineate your roles and responsibilities and those of the patient, family, and other health care team members. Poor communication is pediatricians’ most common complaint about psychiatrists.14 Good interdisciplinary communication decreases the chance that treatment strategies will be duplicated, diluted, or misinterpreted.
Consolidate medical care with a single clinician—often the primary care physician—based on discussions with the patient, family, and health care team. The coordinating clinician can mediate between the school and family when tensions develop over poor attendance or requests for special treatment. It is often useful for this clinician to spell out:
- what constitutes a legitimate medical excuse for school absence
- who will legitimize excuses.
All parties should understand that the school will view an unexcused absence as truancy and act appropriately.
Diet and lifestyle. Encourage the patient to maintain a regular schedule and a healthy diet. Specific dietary interventions have not been proven effective, despite speculation that lack of dietary fiber or lactose intolerance might cause RAP.15,16 Also encourage adequate sleep and regular exercise.
Medication and psychotherapy
Because no strong evidence-based guidelines address pediatric RAP intervention, family preferences usually guide initial treatment decisions. This highlights the importance of good communication and a therapeutic partnership among the clinician, family, and patient.
Antispasmodics, acid reducers, and antidepressants are commonly prescribed for RAP, though none are well-supported in the literature and no controlled studies have gauged medication’s impact on psychiatric comorbidity.16
Antidepressants. Selective serotonin reuptake inhibitors (SSRIs) might help relieve RAP symptoms, but the evidence is inconclusive. SSRIs are considered potentially beneficial in RAP because they may help communicate nociceptive information between the gut and brain and mediate visceral hyperalgesia.
SSRIs at first may increase serotonin at the synapse, which one might assume would to worsen abdominal symptoms. However, ongoing SSRI use could “down-regulate” postsynaptic 5-HT3 receptors and desensitize postsynaptic cells to the effects of local serotonin.
Our group recently conducted a 12-week open trial of citalopram for functional pediatric RAP.17 The 25 participants received 10 mg/d the first week, then 20 mg/d thereafter if tolerated. At week 4, nonresponders and partial responders who were tolerating the medication began receiving 40 mg/d.
Table 3
SSRI daily dosing for pediatric RAP
| Drug | Starting dosage* | Target dosage† | Maximum dosage‡ |
|---|---|---|---|
| Citalopram | 10 mg | 20 mg | 40 to 60 mg |
| Escitalopram | 5 mg | 10 mg | 20 to 30 mg |
| Fluoxetine | 10 mg | 20 mg | 40 mg |
| Fluvoxamine | 50 mg | 100 mg | 300 mg |
| Sertraline | 25 mg | 50 mg | 200 mg |
| * First 3 to 7 days. | |||
| † If patient tolerates starting dosage, increase to target dosage. | |||
| ‡ If patient does not respond to target dosage in 2 to 3 weeks, consider increasing the dosage. | |||
At trial’s end, more than two-thirds of participants were taking 40 mg/d. We rated 21 of 25 patients (84%) as “much improved” or “very much improved,” using the Clinical Global Impression-Improvement scale. Abdominal pain, anxiety, depression, other somatic symptoms, and functional impairment all improved significantly during treatment. Suicidal thoughts diminished progressively from baseline, and no patient reported suicidal thinking at study’s end. Citalopram was generally well tolerated.
With SSRI treatment, start at a low dosage for 3 to 7 days (Table 3). If tolerated, increase to a typical therapeutic dosage. If symptoms fail to respond after 2 or 3 weeks, consider a higher dosage. A short course of an oral benzodiazepine (such as clonazepam, 0.25 mg bid) during the first weeks of SSRI treatment sometimes helps particularly anxious patients or those whose pain appears closely associated with anxiety or “stress.”
Pediatric gastroenterologists often prescribe a low-dose tricyclic antidepressant as first-line therapy, but we discourage this. TCAs lack efficacy in pediatric depression and pose a greater risk of side effects and safety concerns than SSRIs.18
Other agents have been tried for RAP-associated conditions:
Famotidine, a histamine type 2 receptor blocker, may reduce pain in children with dyspepsia and RAP.19
Peppermint oil reduced abdominal pain in one study of children with IBS but had little effect on other symptoms.20
Medications such as alosetron and tegaserod that interrupt serotonergic neurotransmission in the gut have shown benefit in adults with IBS but have not been studied in children.
Psychotherapy. A few small studies suggest that cognitive-behavioral therapies (CBT) are helpful in RAP, but CBT may be difficult to deliver in medical settings.21,22 A simplified “rehabilitative” approach that incorporates CBT principles involves having the clinician and patient view RAP as a challenge to be overcome, rather than a burden to be endured. Such an approach emphasizes the child’s fundamental strength and adaptability rather than vulnerabilities.
The goal of therapy is redirected from finding a cure to coping with and overcoming the problem. This approach challenges the notion that the child cannot resume normal function until the pain is completely gone. It encourages active, problem-focused coping, and discourages passive acceptance—which is associated with greater symptom burden and functional impairment.
Work with parents to reinforce the child’s health-promoting behaviors and minimize negative and social reinforcements (secondary gain) associated with RAP. Advise parents to:
- encourage and reward full school attendance
- avoid home-bound instruction
- expect the child to function despite physical distress
- insist that the child perform age-appropriate household chores and other responsibilities.
Self-management skills—such as relaxation training, hypnosis, biofeedback, and guided imagery—may help reduce pain and manage physiologic arousal.16 Deception strategies such as placebo or sham interventions are unethical and impractical.
Related resources
- Campo JV. Functional recurrent abdominal pain in children and adolescents. Digestive Health Matters 2003;12(3):15-7.
- International Foundation for Functional Gastrointestinal Disorders. www.iffgd.org
- University of Pittsburgh. Advanced Center for Interventions and Services Research on Early Onset Mood and Anxiety Disorders. www.moodykids.org
Drug brand names
- Alosetron • Lotronex
- Citalopram • Celexa
- Clonazepam • Klonopin
- Escitalopram • Lexapro
- Famotidine • Pepcid
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Sertraline • Zoloft
- Tegaserod • Zelnorm
Disclosure
Dr. Campo’s work has been supported by the National Institute of Mental Health (grant MH01780) and in part by the Advanced Center for Interventions and Services Research on Early Onset Mood and Anxiety Disorders (grant MH66371). He also receives grants from Forest Pharmaceuticals and is a consultant to Eli Lilly and Co.
1. American Psychiatric Association Diagnostic and statistical manual of mental disorders (4th ed, revised). Washington, DC: American Psychiatric Association, 2000.
2. Apley J, Naish N. Recurrent abdominal pains: a field survey of 1,000 school children. Arch Dis Child 1958;33(168):165-70.
3. Scharff L. Recurrent abdominal pain in children: a review of psychological factors and treatment. Clin Psychol Rev 1997;17(2):145-66.
4. Boyle JT. Recurrent abdominal pain: an update. Pediatr Rev 1997;18(9):310-20.
5. Campo JV, Bridge J, Ehmann M, et al. Recurrent abdominal pain, anxiety, and depression in primary care. Pediatrics 2004;113(4):817-24.
6. Campo JV, Di Lorenzo C, Chiappetta L, et al. Adult outcomes of pediatric recurrent abdominal pain: do they just grow out of it? Pediatrics 2001;108(1):E1.-
7. Starfield B, Gross E, Wood M, et al. Psychosocial and psychosomatic diagnoses in primary care of children. Pediatrics 1980;66(2):159-67.
8. Hyams JS, Burke G, Davis PM, et al. Abdominal pain and irritable bowel syndrome in adolescents: a community-based study. J Pediatr 1996;129(2):220-6.
9. Campo JV, Comer DM, Jansen-McWilliams L, et al. Recurrent pain, emotional distress, and health service use in childhood. J Pediatr 2002;141(1):76-83.
10. Stickler GB, Murphy DB. Recurrent abdominal pain. Am J Dis Child 1979;133(5):486-9.
11. Rasquin-Weber A, Hyman PE, Cucchiara S, et al. Childhood functional gastrointestinal disorders. Gut 1999;45(suppl 2):II60-8.
12. Campo JV, Fritz G. A management model for pediatric somatization. Psychosomatics 2001;42(6):467-76.
13. Campo JV, Garber J. Somatization. In: Ammerman RT, Campo JV (eds). Handbook of pediatric psychology and psychiatry. Vol 1 Boston: Allyn and Bacon, 1998;137-61.
14. Fritz GK, Bergman AS. Child psychiatrists seen through pediatricians’ eyes: results of a national survey. J Am Acad Child Psychiatry 1985;24(1):81-6.
15. Huertas-Ceballos A, Macarthur C, Logan S. Dietary interventions for recurrent abdominal pain (RAP) in childhood. Cochrane Database Syst Rev 2002;(2):CD003019.-
16. Weydert JA, Ball TM, Davis MF. Systematic review of treatments for recurrent abdominal pain. Pediatrics 2003;111(1):e1-11.
17. Campo JV, Perel J, Lucas A, et al. Citalopram treatment of pediatric recurrent abdominal pain and comorbid internalizing disorders: An exploratory study (poster). Miami Beach, FL: American Academy of Child and Adolescent Psychiatry annual meeting, October 2003.
18. Geller B, Reising D, Leonard HL, et al. Critical review of tricyclic antidepressant use in children and adolescents. J Am Acad Child Adolesc Psychiatry 1999;38(5):513-6.
19. See MC, Birnbaum AH, Schechter CB, et al. Double-blind, placebo-controlled trial of famotidine in children with abdominal pain and dyspepsia: global and quantitative assessment. Dig Dis Sci 2001;46(5):985-92.
20. Kline RM, Kline JJ, Di Palma J, Barbero GJ. Enteric-coated, pH-dependent peppermint oil capsules for the treatment of irritable bowel syndrome in children. J Pediatr 2001;138(1):125-8.
21. Sanders MR, Rebgetz M, Morrison M, et al. Cognitive-behavioral treatment of recurrent nonspecific abdominal pain in children: an analysis of generalization, maintenance, and side effects. J Consult Clin Psychol 1989;57(2):294-300.
22. Sanders MR, Shepherd RW, Cleghorn G, Woolford H. The treatment of recurrent abdominal pain in children: a controlled comparison of cognitive-behavioral family intervention and standard pediatric care. J Consult Clin Psychol 1994;62(2):306-14.
1. American Psychiatric Association Diagnostic and statistical manual of mental disorders (4th ed, revised). Washington, DC: American Psychiatric Association, 2000.
2. Apley J, Naish N. Recurrent abdominal pains: a field survey of 1,000 school children. Arch Dis Child 1958;33(168):165-70.
3. Scharff L. Recurrent abdominal pain in children: a review of psychological factors and treatment. Clin Psychol Rev 1997;17(2):145-66.
4. Boyle JT. Recurrent abdominal pain: an update. Pediatr Rev 1997;18(9):310-20.
5. Campo JV, Bridge J, Ehmann M, et al. Recurrent abdominal pain, anxiety, and depression in primary care. Pediatrics 2004;113(4):817-24.
6. Campo JV, Di Lorenzo C, Chiappetta L, et al. Adult outcomes of pediatric recurrent abdominal pain: do they just grow out of it? Pediatrics 2001;108(1):E1.-
7. Starfield B, Gross E, Wood M, et al. Psychosocial and psychosomatic diagnoses in primary care of children. Pediatrics 1980;66(2):159-67.
8. Hyams JS, Burke G, Davis PM, et al. Abdominal pain and irritable bowel syndrome in adolescents: a community-based study. J Pediatr 1996;129(2):220-6.
9. Campo JV, Comer DM, Jansen-McWilliams L, et al. Recurrent pain, emotional distress, and health service use in childhood. J Pediatr 2002;141(1):76-83.
10. Stickler GB, Murphy DB. Recurrent abdominal pain. Am J Dis Child 1979;133(5):486-9.
11. Rasquin-Weber A, Hyman PE, Cucchiara S, et al. Childhood functional gastrointestinal disorders. Gut 1999;45(suppl 2):II60-8.
12. Campo JV, Fritz G. A management model for pediatric somatization. Psychosomatics 2001;42(6):467-76.
13. Campo JV, Garber J. Somatization. In: Ammerman RT, Campo JV (eds). Handbook of pediatric psychology and psychiatry. Vol 1 Boston: Allyn and Bacon, 1998;137-61.
14. Fritz GK, Bergman AS. Child psychiatrists seen through pediatricians’ eyes: results of a national survey. J Am Acad Child Psychiatry 1985;24(1):81-6.
15. Huertas-Ceballos A, Macarthur C, Logan S. Dietary interventions for recurrent abdominal pain (RAP) in childhood. Cochrane Database Syst Rev 2002;(2):CD003019.-
16. Weydert JA, Ball TM, Davis MF. Systematic review of treatments for recurrent abdominal pain. Pediatrics 2003;111(1):e1-11.
17. Campo JV, Perel J, Lucas A, et al. Citalopram treatment of pediatric recurrent abdominal pain and comorbid internalizing disorders: An exploratory study (poster). Miami Beach, FL: American Academy of Child and Adolescent Psychiatry annual meeting, October 2003.
18. Geller B, Reising D, Leonard HL, et al. Critical review of tricyclic antidepressant use in children and adolescents. J Am Acad Child Adolesc Psychiatry 1999;38(5):513-6.
19. See MC, Birnbaum AH, Schechter CB, et al. Double-blind, placebo-controlled trial of famotidine in children with abdominal pain and dyspepsia: global and quantitative assessment. Dig Dis Sci 2001;46(5):985-92.
20. Kline RM, Kline JJ, Di Palma J, Barbero GJ. Enteric-coated, pH-dependent peppermint oil capsules for the treatment of irritable bowel syndrome in children. J Pediatr 2001;138(1):125-8.
21. Sanders MR, Rebgetz M, Morrison M, et al. Cognitive-behavioral treatment of recurrent nonspecific abdominal pain in children: an analysis of generalization, maintenance, and side effects. J Consult Clin Psychol 1989;57(2):294-300.
22. Sanders MR, Shepherd RW, Cleghorn G, Woolford H. The treatment of recurrent abdominal pain in children: a controlled comparison of cognitive-behavioral family intervention and standard pediatric care. J Consult Clin Psychol 1994;62(2):306-14.