User login
Adequate adherence to antipsychotics is critical for most patients with a chronic psychotic disorder. Therefore, appraisal of medication adherence—also called compliance in the older literature—is crucial at all visits.
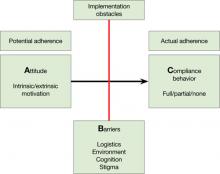
Medication adherence is both an attitude and a behavior,1 and you need to assess both. Without some motivation to take medications (ie, a positive drug attitude), adherence is unlikely. On the other hand, motivation alone does not guarantee compliance behavior, and you need to assess barriers to adherence even in motivated patients.
To arrive at a clinical estimate of adherence to antipsychotics, ask yourself:
A What is my patient’s Attitude toward antipsychotics?
Expect a positive drug attitude if the medication is perceived as warranted, potentially effective, and tolerable. Inquire about prior experience with medications and psychiatrists, including unpleasant somatic experiences, periods of coercion, specific benefits, and fears. Remember that the perceived harm from—vs the perceived need for—medications is judged from the patient’s point of view, not the clinician’s. For example, some patients are motivated to take an antipsychotic because it helps them sleep. Make note if motivation is intrinsic or extrinsic. You might start by asking, “Why do you think taking this medication is a good idea?”
Figure: Attitude, Barriers, and Compliance behavior
B Are there Barriers for a motivated patient to implement optimal adherence?
Ask, “What gets in the way of taking your medication?” Identifying barriers for the motivated patient forces you to look at the individual’s real-life situation. Can the patient afford the co-pay? Is the family against the patient taking an antipsychotic? Does the patient lack a routine that would help him or her remember to take pills? Is the patient too ashamed of the stigma of taking psychiatric medications? Does the patient have cognitive impairment that leads to forgetting to take pills?
C What is my best quantitative estimate of Compliance behavior?
Ask your patient, “In the last 7 days, how many pills have you missed?” Inquire also about names of pills and dosages, number of pills prescribed, and how they are taken to get a sense of your patient’s routines and cognitive competence. This is the time to get collateral information, such as when the last prescription was filled. After collecting this information, you should be able to estimate a patient’s level of adherence (eg, almost 100%, partial 50% to 75%, none). Be aware that both clinicians and patients overestimate actual adherence.
Disclosures
Drs. Kontos and Querques report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Freudenreich receives grant/research support from Pfizer Inc. He is a consultant to Transcept Pharmaceuticals, Inc. and Beacon Health Strategies, LLC and a speaker for Reed Medical Education.
1. Velligan DI, Weiden PJ, Sajatovic M, et al. The expert consensus guideline series: adherence problems in patients with serious and persistent mental illness. J Clin Psychiatry. 2009;70(suppl 4):1-46.
Adequate adherence to antipsychotics is critical for most patients with a chronic psychotic disorder. Therefore, appraisal of medication adherence—also called compliance in the older literature—is crucial at all visits.
Medication adherence is both an attitude and a behavior,1 and you need to assess both. Without some motivation to take medications (ie, a positive drug attitude), adherence is unlikely. On the other hand, motivation alone does not guarantee compliance behavior, and you need to assess barriers to adherence even in motivated patients.
To arrive at a clinical estimate of adherence to antipsychotics, ask yourself:
A What is my patient’s Attitude toward antipsychotics?
Expect a positive drug attitude if the medication is perceived as warranted, potentially effective, and tolerable. Inquire about prior experience with medications and psychiatrists, including unpleasant somatic experiences, periods of coercion, specific benefits, and fears. Remember that the perceived harm from—vs the perceived need for—medications is judged from the patient’s point of view, not the clinician’s. For example, some patients are motivated to take an antipsychotic because it helps them sleep. Make note if motivation is intrinsic or extrinsic. You might start by asking, “Why do you think taking this medication is a good idea?”
Figure: Attitude, Barriers, and Compliance behavior
B Are there Barriers for a motivated patient to implement optimal adherence?
Ask, “What gets in the way of taking your medication?” Identifying barriers for the motivated patient forces you to look at the individual’s real-life situation. Can the patient afford the co-pay? Is the family against the patient taking an antipsychotic? Does the patient lack a routine that would help him or her remember to take pills? Is the patient too ashamed of the stigma of taking psychiatric medications? Does the patient have cognitive impairment that leads to forgetting to take pills?
C What is my best quantitative estimate of Compliance behavior?
Ask your patient, “In the last 7 days, how many pills have you missed?” Inquire also about names of pills and dosages, number of pills prescribed, and how they are taken to get a sense of your patient’s routines and cognitive competence. This is the time to get collateral information, such as when the last prescription was filled. After collecting this information, you should be able to estimate a patient’s level of adherence (eg, almost 100%, partial 50% to 75%, none). Be aware that both clinicians and patients overestimate actual adherence.
Disclosures
Drs. Kontos and Querques report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Freudenreich receives grant/research support from Pfizer Inc. He is a consultant to Transcept Pharmaceuticals, Inc. and Beacon Health Strategies, LLC and a speaker for Reed Medical Education.
Adequate adherence to antipsychotics is critical for most patients with a chronic psychotic disorder. Therefore, appraisal of medication adherence—also called compliance in the older literature—is crucial at all visits.
Medication adherence is both an attitude and a behavior,1 and you need to assess both. Without some motivation to take medications (ie, a positive drug attitude), adherence is unlikely. On the other hand, motivation alone does not guarantee compliance behavior, and you need to assess barriers to adherence even in motivated patients.
To arrive at a clinical estimate of adherence to antipsychotics, ask yourself:
A What is my patient’s Attitude toward antipsychotics?
Expect a positive drug attitude if the medication is perceived as warranted, potentially effective, and tolerable. Inquire about prior experience with medications and psychiatrists, including unpleasant somatic experiences, periods of coercion, specific benefits, and fears. Remember that the perceived harm from—vs the perceived need for—medications is judged from the patient’s point of view, not the clinician’s. For example, some patients are motivated to take an antipsychotic because it helps them sleep. Make note if motivation is intrinsic or extrinsic. You might start by asking, “Why do you think taking this medication is a good idea?”
Figure: Attitude, Barriers, and Compliance behavior
B Are there Barriers for a motivated patient to implement optimal adherence?
Ask, “What gets in the way of taking your medication?” Identifying barriers for the motivated patient forces you to look at the individual’s real-life situation. Can the patient afford the co-pay? Is the family against the patient taking an antipsychotic? Does the patient lack a routine that would help him or her remember to take pills? Is the patient too ashamed of the stigma of taking psychiatric medications? Does the patient have cognitive impairment that leads to forgetting to take pills?
C What is my best quantitative estimate of Compliance behavior?
Ask your patient, “In the last 7 days, how many pills have you missed?” Inquire also about names of pills and dosages, number of pills prescribed, and how they are taken to get a sense of your patient’s routines and cognitive competence. This is the time to get collateral information, such as when the last prescription was filled. After collecting this information, you should be able to estimate a patient’s level of adherence (eg, almost 100%, partial 50% to 75%, none). Be aware that both clinicians and patients overestimate actual adherence.
Disclosures
Drs. Kontos and Querques report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Freudenreich receives grant/research support from Pfizer Inc. He is a consultant to Transcept Pharmaceuticals, Inc. and Beacon Health Strategies, LLC and a speaker for Reed Medical Education.
1. Velligan DI, Weiden PJ, Sajatovic M, et al. The expert consensus guideline series: adherence problems in patients with serious and persistent mental illness. J Clin Psychiatry. 2009;70(suppl 4):1-46.
1. Velligan DI, Weiden PJ, Sajatovic M, et al. The expert consensus guideline series: adherence problems in patients with serious and persistent mental illness. J Clin Psychiatry. 2009;70(suppl 4):1-46.