User login
ANSWER
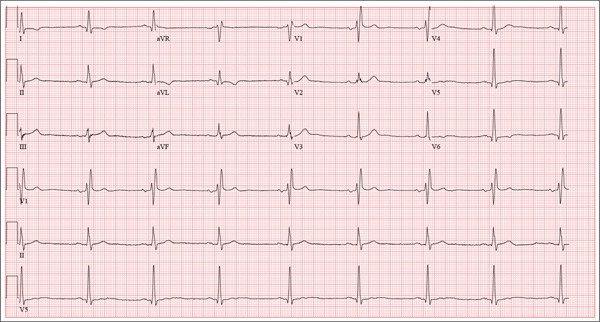
The correct interpretation includes marked sinus bradycardia, a right bundle branch block, and T-wave abnormalities in the lateral leads.
Sinus bradycardia is evidenced by a sinus rate less than 60 beats/min and may be considered “marked” if the rate is less than 50 beats/min.
A right bundle branch block is indicated by a QRS duration ≥ 120 ms, a terminal broad S wave in lead I, and the presence of an RSR’ pattern in lead V1.
Small or nonexistent T waves in leads V5 and V6 are suggestive of lateral ischemia but are not diagnostic in this individual.
His marked bradycardia was attributed to his exceptional athleticism and the fact that the ECG was taken “at rest.” It was not of concern, nor did it require treatment.
ANSWER
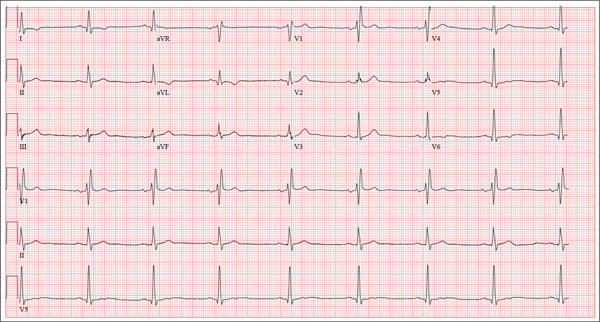
The correct interpretation includes marked sinus bradycardia, a right bundle branch block, and T-wave abnormalities in the lateral leads.
Sinus bradycardia is evidenced by a sinus rate less than 60 beats/min and may be considered “marked” if the rate is less than 50 beats/min.
A right bundle branch block is indicated by a QRS duration ≥ 120 ms, a terminal broad S wave in lead I, and the presence of an RSR’ pattern in lead V1.
Small or nonexistent T waves in leads V5 and V6 are suggestive of lateral ischemia but are not diagnostic in this individual.
His marked bradycardia was attributed to his exceptional athleticism and the fact that the ECG was taken “at rest.” It was not of concern, nor did it require treatment.
ANSWER
The correct interpretation includes marked sinus bradycardia, a right bundle branch block, and T-wave abnormalities in the lateral leads.
Sinus bradycardia is evidenced by a sinus rate less than 60 beats/min and may be considered “marked” if the rate is less than 50 beats/min.
A right bundle branch block is indicated by a QRS duration ≥ 120 ms, a terminal broad S wave in lead I, and the presence of an RSR’ pattern in lead V1.
Small or nonexistent T waves in leads V5 and V6 are suggestive of lateral ischemia but are not diagnostic in this individual.
His marked bradycardia was attributed to his exceptional athleticism and the fact that the ECG was taken “at rest.” It was not of concern, nor did it require treatment.
A 62-year-old man presents for a preoperative history and physical exam prior to surgical repair of an injury to his right anterior cruciate ligament (ACL). He reports that he has been healthy all his life and has never had an injury or illness requiring hospitalization. He is an accountant at a local financial institution and has a very active lifestyle, which includes competitive cycling, running, and skiing. He recently completed his fourth triathlon and was training for his sixth marathon until his injury occurred. One week ago, he was skiing moguls on a black diamond course when he fell and tumbled about 20 feet before stopping. His right ski binding did not release from the boot. He felt his right knee “pop” and knew immediately that he had sustained a serious injury. When he tried to stand, he was unable to bear weight on his right leg. The ski patrol transported him off the slope via basket. He was then taken to a local hospital by a colleague. Physical exam and MRI confirmed an avulsion of the ACL. He has been convalescing at home (having delayed his surgery in order to catch up on paper-work for work) and is scheduled for surgery in two days’ time. Medical history is unremarkable. Aside from the usual childhood illnesses (eg, ear infections, chicken pox, mumps), he has been very healthy and attributes this to a strict diet and rigorous exercise. Social history reveals that he is married to an attorney and has no children. He has never smoked or taken recreational drugs, and he consumes approximately one bottle of wine per week. His current medications include naproxen as needed for pain, a daily aspirin, fish oil, a multivitamin, and omeprazole on rare occasions. The review of systems is remarkable only for occasional gastroesophageal re-flux, which is exacerbated by spicy dishes containing curry. Physical exam reveals a thin, athletic male in no acute distress. His weight is 168 lb, and his height is 74”. Vital signs include a blood pressure of 104/62 mm Hg; pulse, 50 beats/min; respiratory rate, 14 breaths/min-1; and temperature, 98°F. Examination of the head, neck, lungs, heart, abdomen, skin, and nervous system yields normal findings. Lachman, pivot shift, and anterior drawer maneuvers of the right knee are all positive. A routine ECG is performed that reveals the following: a ventricular rate of 49 beats/min; PR interval, 176 ms; QRS dura-tion, 120 ms; QT/QTc interval, 430/388 ms; P axis, 14°; R axis, 38°; and T axis, 103°. What is your interpretation of this ECG?