User login
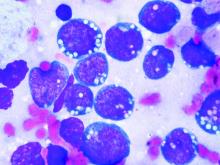
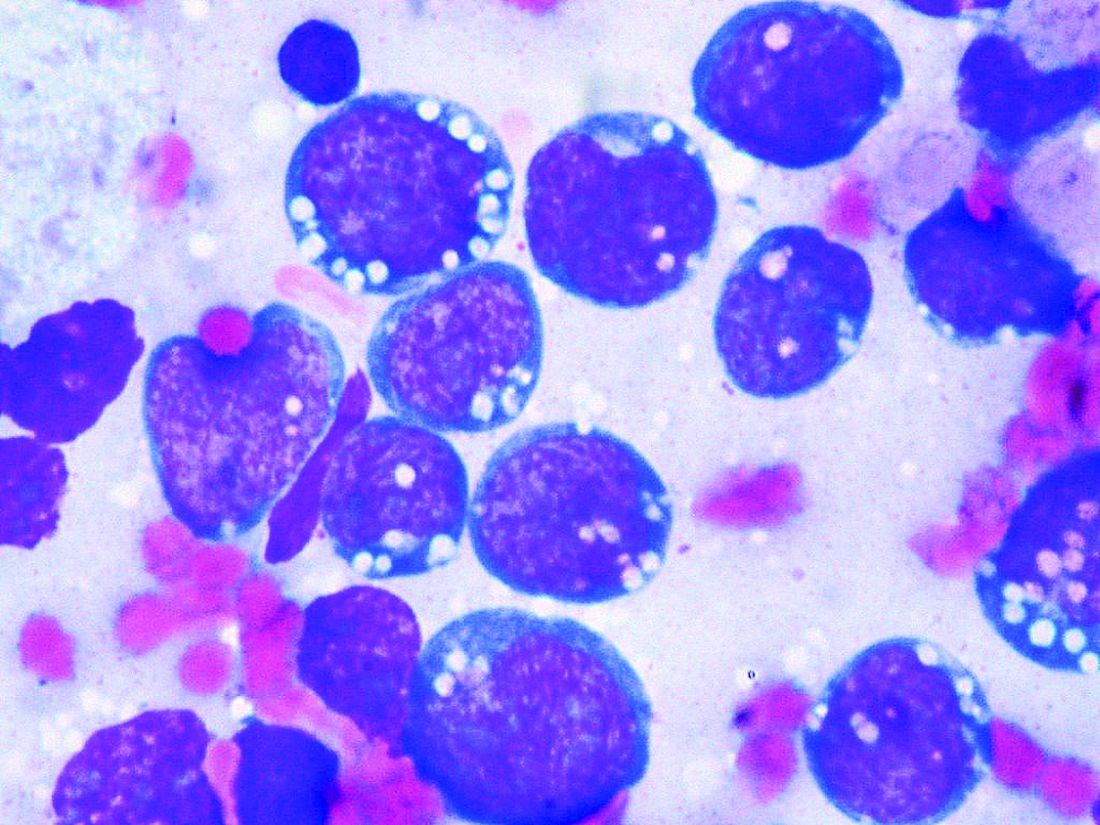
The addition of rituximab to standard chemotherapy was a more effective therapy in children and adolescents with high-risk, high-grade,mature B-cell non-Hodgkin lymphoma than the use of chemotherapy alone, according to a study published in the New England Journal of Medicine. The addition of rituximab resulted in long-term complete remission in the vast majority of patients, reported Veronique Minard-Colin, MD, of the Gustave Roussy Institute, Villejuif Cedex, France, and her colleagues on behalf of the European Intergroup for Childhood Non-Hodgkin Lymphoma and the Children’s Oncology Group.
The researchers performed an open-label, randomized, phase 3 trial of 328 patients younger than 18 years of age with high-risk, mature B-cell non-Hodgkin’s lymphoma (stage III with an elevated lactate dehydrogenase level or stage IV) or acute leukemia to compare the addition of six doses of rituximab to standard lymphomes malins B (LMB) chemotherapy with standard LMB chemotherapy alone. There were 164 patients assigned to each group. The primary end point of the study was event-free survival; overall survival and toxic effects were also followed.
The majority of patients had Burkitt’s lymphoma: 139 (84.8%) in the rituximab-chemotherapy group and 142 (86.6%) in the chemotherapy-alone group, with diffuse large B-cell lymphoma being the second most common cancer: 19 (11.6%) vs. 12 (7.3%), respectively.
Event-free survival at 3 years was 93.9% (95% confidence interval, 89.1-96.7) in the rituximab-chemotherapy group and 82.3% (95% CI, 75.7-87.5) in the chemotherapy group.
Higher 3-year overall survival was also observed (95.1% in the rituximab-chemotherapy group vs. 87.3% in the chemotherapy group; hazard ratio for death, 0.36; 95% CI, 0.16 -0.82).
Eight patients in the rituximab-chemotherapy group died (4 deaths were disease related, 3 were treatment related, and 1 was from a second cancer), as did 20 in the chemotherapy group (17 deaths disease related, and 3 treatment related); HR, 0.36; 95% CI, 0.16-0.82.
The incidence of acute adverse events of grade 4 or higher after prephase treatment was 33.3% in the rituximab-chemotherapy group and 24.2% in the chemotherapy group, a nonsignificant difference (P = .07). However, around twice as many patients in the rituximab-chemotherapy group had a low IgG level at 1 year after trial inclusion, compared with the chemotherapy-alone group, which could indicate the potential for more frequent infections in the long term, the researchers stated.
“An assessment of the long-term effects of combining rituximab with this chemotherapy regimen in children with non-Hodgkin lymphoma, including data on immune status, will be useful,” they added.
The study was funded by the French Ministry of Health, Cancer Research UK, the National Institute for Health Research Clinical Research Network, the Children’s Cancer Foundation Hong Kong, the U.S. National Cancer Institute, and F. Hoffmann–La Roche–Genentech. Several of the authors reported consulting for and institutional and grant funding from F. Hoffmann-LaRoche, which markets rituximab, as well as relationships with other pharmaceutical companies.
SOURCE: Minard-Colin V et al. N Engl J Med. 2020;382:2207-19.
The addition of rituximab to standard chemotherapy was a more effective therapy in children and adolescents with high-risk, high-grade,mature B-cell non-Hodgkin lymphoma than the use of chemotherapy alone, according to a study published in the New England Journal of Medicine. The addition of rituximab resulted in long-term complete remission in the vast majority of patients, reported Veronique Minard-Colin, MD, of the Gustave Roussy Institute, Villejuif Cedex, France, and her colleagues on behalf of the European Intergroup for Childhood Non-Hodgkin Lymphoma and the Children’s Oncology Group.
The researchers performed an open-label, randomized, phase 3 trial of 328 patients younger than 18 years of age with high-risk, mature B-cell non-Hodgkin’s lymphoma (stage III with an elevated lactate dehydrogenase level or stage IV) or acute leukemia to compare the addition of six doses of rituximab to standard lymphomes malins B (LMB) chemotherapy with standard LMB chemotherapy alone. There were 164 patients assigned to each group. The primary end point of the study was event-free survival; overall survival and toxic effects were also followed.
The majority of patients had Burkitt’s lymphoma: 139 (84.8%) in the rituximab-chemotherapy group and 142 (86.6%) in the chemotherapy-alone group, with diffuse large B-cell lymphoma being the second most common cancer: 19 (11.6%) vs. 12 (7.3%), respectively.
Event-free survival at 3 years was 93.9% (95% confidence interval, 89.1-96.7) in the rituximab-chemotherapy group and 82.3% (95% CI, 75.7-87.5) in the chemotherapy group.
Higher 3-year overall survival was also observed (95.1% in the rituximab-chemotherapy group vs. 87.3% in the chemotherapy group; hazard ratio for death, 0.36; 95% CI, 0.16 -0.82).
Eight patients in the rituximab-chemotherapy group died (4 deaths were disease related, 3 were treatment related, and 1 was from a second cancer), as did 20 in the chemotherapy group (17 deaths disease related, and 3 treatment related); HR, 0.36; 95% CI, 0.16-0.82.
The incidence of acute adverse events of grade 4 or higher after prephase treatment was 33.3% in the rituximab-chemotherapy group and 24.2% in the chemotherapy group, a nonsignificant difference (P = .07). However, around twice as many patients in the rituximab-chemotherapy group had a low IgG level at 1 year after trial inclusion, compared with the chemotherapy-alone group, which could indicate the potential for more frequent infections in the long term, the researchers stated.
“An assessment of the long-term effects of combining rituximab with this chemotherapy regimen in children with non-Hodgkin lymphoma, including data on immune status, will be useful,” they added.
The study was funded by the French Ministry of Health, Cancer Research UK, the National Institute for Health Research Clinical Research Network, the Children’s Cancer Foundation Hong Kong, the U.S. National Cancer Institute, and F. Hoffmann–La Roche–Genentech. Several of the authors reported consulting for and institutional and grant funding from F. Hoffmann-LaRoche, which markets rituximab, as well as relationships with other pharmaceutical companies.
SOURCE: Minard-Colin V et al. N Engl J Med. 2020;382:2207-19.
The addition of rituximab to standard chemotherapy was a more effective therapy in children and adolescents with high-risk, high-grade,mature B-cell non-Hodgkin lymphoma than the use of chemotherapy alone, according to a study published in the New England Journal of Medicine. The addition of rituximab resulted in long-term complete remission in the vast majority of patients, reported Veronique Minard-Colin, MD, of the Gustave Roussy Institute, Villejuif Cedex, France, and her colleagues on behalf of the European Intergroup for Childhood Non-Hodgkin Lymphoma and the Children’s Oncology Group.
The researchers performed an open-label, randomized, phase 3 trial of 328 patients younger than 18 years of age with high-risk, mature B-cell non-Hodgkin’s lymphoma (stage III with an elevated lactate dehydrogenase level or stage IV) or acute leukemia to compare the addition of six doses of rituximab to standard lymphomes malins B (LMB) chemotherapy with standard LMB chemotherapy alone. There were 164 patients assigned to each group. The primary end point of the study was event-free survival; overall survival and toxic effects were also followed.
The majority of patients had Burkitt’s lymphoma: 139 (84.8%) in the rituximab-chemotherapy group and 142 (86.6%) in the chemotherapy-alone group, with diffuse large B-cell lymphoma being the second most common cancer: 19 (11.6%) vs. 12 (7.3%), respectively.
Event-free survival at 3 years was 93.9% (95% confidence interval, 89.1-96.7) in the rituximab-chemotherapy group and 82.3% (95% CI, 75.7-87.5) in the chemotherapy group.
Higher 3-year overall survival was also observed (95.1% in the rituximab-chemotherapy group vs. 87.3% in the chemotherapy group; hazard ratio for death, 0.36; 95% CI, 0.16 -0.82).
Eight patients in the rituximab-chemotherapy group died (4 deaths were disease related, 3 were treatment related, and 1 was from a second cancer), as did 20 in the chemotherapy group (17 deaths disease related, and 3 treatment related); HR, 0.36; 95% CI, 0.16-0.82.
The incidence of acute adverse events of grade 4 or higher after prephase treatment was 33.3% in the rituximab-chemotherapy group and 24.2% in the chemotherapy group, a nonsignificant difference (P = .07). However, around twice as many patients in the rituximab-chemotherapy group had a low IgG level at 1 year after trial inclusion, compared with the chemotherapy-alone group, which could indicate the potential for more frequent infections in the long term, the researchers stated.
“An assessment of the long-term effects of combining rituximab with this chemotherapy regimen in children with non-Hodgkin lymphoma, including data on immune status, will be useful,” they added.
The study was funded by the French Ministry of Health, Cancer Research UK, the National Institute for Health Research Clinical Research Network, the Children’s Cancer Foundation Hong Kong, the U.S. National Cancer Institute, and F. Hoffmann–La Roche–Genentech. Several of the authors reported consulting for and institutional and grant funding from F. Hoffmann-LaRoche, which markets rituximab, as well as relationships with other pharmaceutical companies.
SOURCE: Minard-Colin V et al. N Engl J Med. 2020;382:2207-19.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Adding rituximab to chemotherapy was effective in children and adolescents with high-risk, high-grade, mature B-cell non-Hodgkin lymphoma.
Major finding: Higher 3-year overall survival was observed (95.1% in the rituximab-chemotherapy group vs. 87.3% in the chemotherapy group).
Study details: Analysis of 328 patients who underwent randomization to standard chemotherapy vs. chemo plus rituximab (164 patients per group).
Disclosures: The study was funded by the French Ministry of Health, Cancer Research UK, the National Institute for Health Research Clinical Research Network, the Children’s Cancer Foundation Hong Kong, the U.S. National Cancer Institute, and F. Hoffmann–La Roche–Genentech. Several of the authors reported consulting for and institutional and grant funding from F. Hoffmann-LaRoche, which markets rituximab, as well as relationships with other pharmaceutical companies.
Source: Minard-Colin V et al. N Engl J Med. 2020; 382:2207-19.