User login
, according to a new study involving registry data for more than 11,000 individuals.
These new findings “raise a different perspective from the conventional view that AA does not differ by race/ethnicity,” said Hemin Lee, MD, MPH, of the division of pharmacoepidemiology and pharmacoeconomics at Brigham and Women’s Hospital, Boston, and associates.
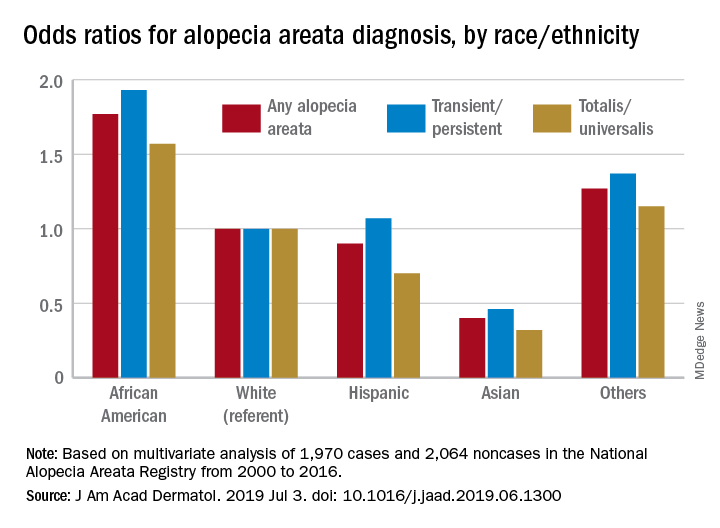
Multivariate-adjusted odds ratios for ever-diagnosis of AA were 1.77 for African Americans and 0.4 for Asians when whites were the referent group. Hispanics/Latinos were similar to whites, with an odds ratio of 0.9, and the group of other races/ethnicities (including American Indians and Pacific Islanders) was higher at 1.27, the investigators noted. The report is in the Journal of the American Academy of Dermatology.
The odds played out in a similar fashion when broken down by AA subtype. With whites as the referent at 1.0, blacks were most likely to have been diagnosed with AA transient/persistent at 1.93 and Asians were lowest at 0.46. For AA totalis/universalis, odds ratios were 1.57 for blacks and 0.32 for Asians, they said, based on 2000-2016 data from the National Alopecia Areata Registry.
“An intricate interplay between genetic and environmental factors may account for the racial differences. Pathogenesis of AA is at times linked with autoimmunity by its strong association with HLA class II alleles,” Dr. Lee and associates wrote.
The study involved 11,404 participants from the registry: 9,340 had reported at least one episode of AA and 2,064 had no history of lifetime alopecia. The multivariate analysis was based on the same group of noncases but a subgroup of 1,970 AA patients who had been enrolled in the registry “through academic institutions after dermatologist-confirmed diagnosis,” they said.
There was no funding source to report. One of Dr. Lee’s associates has received honoraria from Abbvie, Amgen, the Centers for Disease Control and Prevention, Janssen, Merck, Novartis, Pfizer, and Amgen, which have been donated to charity, and is an investigator for Sanofi/Regeneron with no financial compensation. All other authors have no conflicts of interest.
SOURCE: Lee H et al. J Am Acad Dermatol. 2019 Jul 3. doi: 10.1016/j.jaad.2019.06.1300.
, according to a new study involving registry data for more than 11,000 individuals.
These new findings “raise a different perspective from the conventional view that AA does not differ by race/ethnicity,” said Hemin Lee, MD, MPH, of the division of pharmacoepidemiology and pharmacoeconomics at Brigham and Women’s Hospital, Boston, and associates.
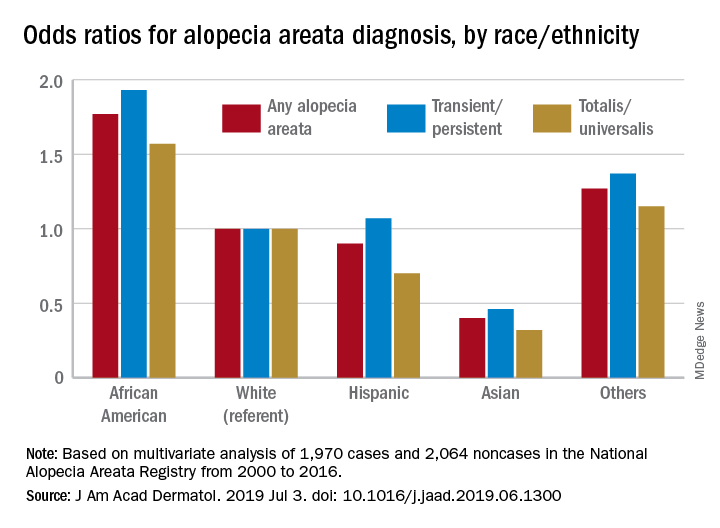
Multivariate-adjusted odds ratios for ever-diagnosis of AA were 1.77 for African Americans and 0.4 for Asians when whites were the referent group. Hispanics/Latinos were similar to whites, with an odds ratio of 0.9, and the group of other races/ethnicities (including American Indians and Pacific Islanders) was higher at 1.27, the investigators noted. The report is in the Journal of the American Academy of Dermatology.
The odds played out in a similar fashion when broken down by AA subtype. With whites as the referent at 1.0, blacks were most likely to have been diagnosed with AA transient/persistent at 1.93 and Asians were lowest at 0.46. For AA totalis/universalis, odds ratios were 1.57 for blacks and 0.32 for Asians, they said, based on 2000-2016 data from the National Alopecia Areata Registry.
“An intricate interplay between genetic and environmental factors may account for the racial differences. Pathogenesis of AA is at times linked with autoimmunity by its strong association with HLA class II alleles,” Dr. Lee and associates wrote.
The study involved 11,404 participants from the registry: 9,340 had reported at least one episode of AA and 2,064 had no history of lifetime alopecia. The multivariate analysis was based on the same group of noncases but a subgroup of 1,970 AA patients who had been enrolled in the registry “through academic institutions after dermatologist-confirmed diagnosis,” they said.
There was no funding source to report. One of Dr. Lee’s associates has received honoraria from Abbvie, Amgen, the Centers for Disease Control and Prevention, Janssen, Merck, Novartis, Pfizer, and Amgen, which have been donated to charity, and is an investigator for Sanofi/Regeneron with no financial compensation. All other authors have no conflicts of interest.
SOURCE: Lee H et al. J Am Acad Dermatol. 2019 Jul 3. doi: 10.1016/j.jaad.2019.06.1300.
, according to a new study involving registry data for more than 11,000 individuals.
These new findings “raise a different perspective from the conventional view that AA does not differ by race/ethnicity,” said Hemin Lee, MD, MPH, of the division of pharmacoepidemiology and pharmacoeconomics at Brigham and Women’s Hospital, Boston, and associates.
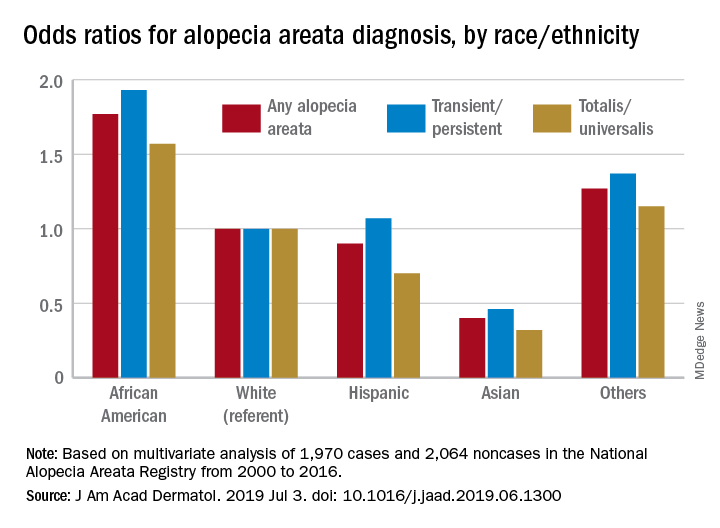
Multivariate-adjusted odds ratios for ever-diagnosis of AA were 1.77 for African Americans and 0.4 for Asians when whites were the referent group. Hispanics/Latinos were similar to whites, with an odds ratio of 0.9, and the group of other races/ethnicities (including American Indians and Pacific Islanders) was higher at 1.27, the investigators noted. The report is in the Journal of the American Academy of Dermatology.
The odds played out in a similar fashion when broken down by AA subtype. With whites as the referent at 1.0, blacks were most likely to have been diagnosed with AA transient/persistent at 1.93 and Asians were lowest at 0.46. For AA totalis/universalis, odds ratios were 1.57 for blacks and 0.32 for Asians, they said, based on 2000-2016 data from the National Alopecia Areata Registry.
“An intricate interplay between genetic and environmental factors may account for the racial differences. Pathogenesis of AA is at times linked with autoimmunity by its strong association with HLA class II alleles,” Dr. Lee and associates wrote.
The study involved 11,404 participants from the registry: 9,340 had reported at least one episode of AA and 2,064 had no history of lifetime alopecia. The multivariate analysis was based on the same group of noncases but a subgroup of 1,970 AA patients who had been enrolled in the registry “through academic institutions after dermatologist-confirmed diagnosis,” they said.
There was no funding source to report. One of Dr. Lee’s associates has received honoraria from Abbvie, Amgen, the Centers for Disease Control and Prevention, Janssen, Merck, Novartis, Pfizer, and Amgen, which have been donated to charity, and is an investigator for Sanofi/Regeneron with no financial compensation. All other authors have no conflicts of interest.
SOURCE: Lee H et al. J Am Acad Dermatol. 2019 Jul 3. doi: 10.1016/j.jaad.2019.06.1300.
FROM THE JOURNAL OF THE AMERICAN ACADEMY OF DERMATOLOGY