User login
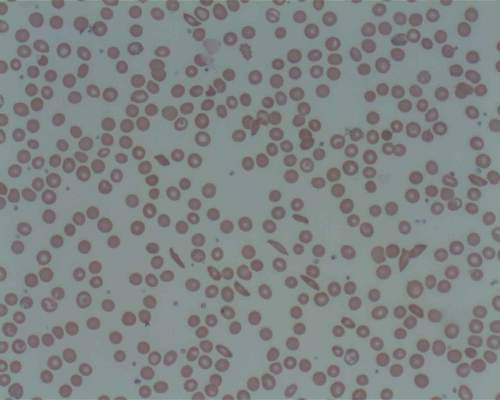
The human body’s microbiota regulates the aging of circulating neutrophils, and aged neutrophils, which are excessively active and adherent, promote tissue injury in inflammatory diseases. These two discoveries appear to point the way toward a simple, effective antibiotic treatment for sickle-cell disease, and may eventually lead to similar therapies for other disorders that induce inflammation-related organ damage, such as septic shock, according to a Research Letter published online Sept. 16 in Nature.
“To our knowledge, this is the first therapy shown to alleviate the chronic tissue damage induced by sickle-cell disease,” said Dachuan Zhang of the Gottesman Institute for Stem Cell and Regenerative Medicine Research and the department of cell biology, Albert Einstein College of Medicine, New York, and his associates. “Our results raise the possibility that manipulation of the microbiome may have sustained implications in disease outcome that should be further studied in clinical trials.”
In a series of in vitro and in vivo studies, the researchers demonstrated that aging neutrophils differ from others in that they are overactive and extra-adherent. Adherent neutrophils are already known to precipitate the acute vaso-occlusion that characterizes sickle-cell disease. Aging neutrophils also displayed other traits suggesting that exogenous inflammatory mediators may contribute to their excessive activity and adherence.
Dr. Zhang and his colleagues suspected that molecules in the microbiota – the ecologic community of all microorganisms residing in the body – may be involved, as they are known to cross the intestinal barrier to affect multiple systemic immune-cell populations, and a recent study suggested that the microbiota may regulate neutrophil production and function. To test this hypothesis they treated mice with broad-spectrum antibiotics, which caused dramatic depletion of microbiota volume and composition in the gut. This in turn significantly reduced aged neutrophils in the circulation, which immediately rebounded when the antibiotics were counteracted.
Further mouse studies revealed that neutrophil aging is delayed in a bacterially depleted environment, and that microbiota-derived molecules actually induce neutrophil aging. In a subsequent study of an in vivo model of septic shock, mice that were given antibiotics were protected from neutrophil-mediated damage in the vasculature and showed markedly prolonged survival, compared with untreated mice, the investigators noted (Nature. 2015 Sep 24;525[7570]. doi: 10.1038/nature15367 ).
In an in vivo model of sickle-cell disease, untreated mice with the disease showed markedly increased neutrophil activity and adhesion while affected mice given antibiotics showed marked microbiota depletion; enhanced blood flow; significantly reduced splenomegaly; and marked alleviation of liver necrosis, fibrosis, and inflammation. Survival was significantly improved in the treated mice. Finally, a laboratory-induced replenishment of aging neutrophils in the circulation resulted in acute vaso-occlusive crises and death within 10-30 hours in all affected mice.
“Together, these data suggest that the microbiota regulates aged neutrophil numbers, thereby affecting both acute vaso-occlusive crisis and the ensuing chronic tissue damage in sickle-cell disease,” Dr. Zhang and his associates said.
To assess how their findings applied to human beings, the investigators next studied 23 patients with sickle-cell disease who were not taking antibiotics, 11 patients with sickle-cell disease who were taking penicillin to prevent life-threatening infections, and 9 healthy control subjects. Compared with controls, only the patients who weren’t taking antibiotics showed a dramatic increase in circulating aged neutrophils. This protective effect of antibiotics was consistent across all ages, both genders, and regardless of hydroxyurea intake. Now, a prospective study involving age-matched participants is needed to confirm that antibiotics, by reducing the gut microbiota, decrease aged neutrophils in the circulation and thereby improve vaso-occlusive disease, the researchers said.
The American Heart Association, the National Institutes of Health, and the New York State Stem Cell Science Program funded the study. Dr. Zhang and his associates reported having no relevant disclosures.
The human body’s microbiota regulates the aging of circulating neutrophils, and aged neutrophils, which are excessively active and adherent, promote tissue injury in inflammatory diseases. These two discoveries appear to point the way toward a simple, effective antibiotic treatment for sickle-cell disease, and may eventually lead to similar therapies for other disorders that induce inflammation-related organ damage, such as septic shock, according to a Research Letter published online Sept. 16 in Nature.
“To our knowledge, this is the first therapy shown to alleviate the chronic tissue damage induced by sickle-cell disease,” said Dachuan Zhang of the Gottesman Institute for Stem Cell and Regenerative Medicine Research and the department of cell biology, Albert Einstein College of Medicine, New York, and his associates. “Our results raise the possibility that manipulation of the microbiome may have sustained implications in disease outcome that should be further studied in clinical trials.”
In a series of in vitro and in vivo studies, the researchers demonstrated that aging neutrophils differ from others in that they are overactive and extra-adherent. Adherent neutrophils are already known to precipitate the acute vaso-occlusion that characterizes sickle-cell disease. Aging neutrophils also displayed other traits suggesting that exogenous inflammatory mediators may contribute to their excessive activity and adherence.
Dr. Zhang and his colleagues suspected that molecules in the microbiota – the ecologic community of all microorganisms residing in the body – may be involved, as they are known to cross the intestinal barrier to affect multiple systemic immune-cell populations, and a recent study suggested that the microbiota may regulate neutrophil production and function. To test this hypothesis they treated mice with broad-spectrum antibiotics, which caused dramatic depletion of microbiota volume and composition in the gut. This in turn significantly reduced aged neutrophils in the circulation, which immediately rebounded when the antibiotics were counteracted.
Further mouse studies revealed that neutrophil aging is delayed in a bacterially depleted environment, and that microbiota-derived molecules actually induce neutrophil aging. In a subsequent study of an in vivo model of septic shock, mice that were given antibiotics were protected from neutrophil-mediated damage in the vasculature and showed markedly prolonged survival, compared with untreated mice, the investigators noted (Nature. 2015 Sep 24;525[7570]. doi: 10.1038/nature15367 ).
In an in vivo model of sickle-cell disease, untreated mice with the disease showed markedly increased neutrophil activity and adhesion while affected mice given antibiotics showed marked microbiota depletion; enhanced blood flow; significantly reduced splenomegaly; and marked alleviation of liver necrosis, fibrosis, and inflammation. Survival was significantly improved in the treated mice. Finally, a laboratory-induced replenishment of aging neutrophils in the circulation resulted in acute vaso-occlusive crises and death within 10-30 hours in all affected mice.
“Together, these data suggest that the microbiota regulates aged neutrophil numbers, thereby affecting both acute vaso-occlusive crisis and the ensuing chronic tissue damage in sickle-cell disease,” Dr. Zhang and his associates said.
To assess how their findings applied to human beings, the investigators next studied 23 patients with sickle-cell disease who were not taking antibiotics, 11 patients with sickle-cell disease who were taking penicillin to prevent life-threatening infections, and 9 healthy control subjects. Compared with controls, only the patients who weren’t taking antibiotics showed a dramatic increase in circulating aged neutrophils. This protective effect of antibiotics was consistent across all ages, both genders, and regardless of hydroxyurea intake. Now, a prospective study involving age-matched participants is needed to confirm that antibiotics, by reducing the gut microbiota, decrease aged neutrophils in the circulation and thereby improve vaso-occlusive disease, the researchers said.
The American Heart Association, the National Institutes of Health, and the New York State Stem Cell Science Program funded the study. Dr. Zhang and his associates reported having no relevant disclosures.
The human body’s microbiota regulates the aging of circulating neutrophils, and aged neutrophils, which are excessively active and adherent, promote tissue injury in inflammatory diseases. These two discoveries appear to point the way toward a simple, effective antibiotic treatment for sickle-cell disease, and may eventually lead to similar therapies for other disorders that induce inflammation-related organ damage, such as septic shock, according to a Research Letter published online Sept. 16 in Nature.
“To our knowledge, this is the first therapy shown to alleviate the chronic tissue damage induced by sickle-cell disease,” said Dachuan Zhang of the Gottesman Institute for Stem Cell and Regenerative Medicine Research and the department of cell biology, Albert Einstein College of Medicine, New York, and his associates. “Our results raise the possibility that manipulation of the microbiome may have sustained implications in disease outcome that should be further studied in clinical trials.”
In a series of in vitro and in vivo studies, the researchers demonstrated that aging neutrophils differ from others in that they are overactive and extra-adherent. Adherent neutrophils are already known to precipitate the acute vaso-occlusion that characterizes sickle-cell disease. Aging neutrophils also displayed other traits suggesting that exogenous inflammatory mediators may contribute to their excessive activity and adherence.
Dr. Zhang and his colleagues suspected that molecules in the microbiota – the ecologic community of all microorganisms residing in the body – may be involved, as they are known to cross the intestinal barrier to affect multiple systemic immune-cell populations, and a recent study suggested that the microbiota may regulate neutrophil production and function. To test this hypothesis they treated mice with broad-spectrum antibiotics, which caused dramatic depletion of microbiota volume and composition in the gut. This in turn significantly reduced aged neutrophils in the circulation, which immediately rebounded when the antibiotics were counteracted.
Further mouse studies revealed that neutrophil aging is delayed in a bacterially depleted environment, and that microbiota-derived molecules actually induce neutrophil aging. In a subsequent study of an in vivo model of septic shock, mice that were given antibiotics were protected from neutrophil-mediated damage in the vasculature and showed markedly prolonged survival, compared with untreated mice, the investigators noted (Nature. 2015 Sep 24;525[7570]. doi: 10.1038/nature15367 ).
In an in vivo model of sickle-cell disease, untreated mice with the disease showed markedly increased neutrophil activity and adhesion while affected mice given antibiotics showed marked microbiota depletion; enhanced blood flow; significantly reduced splenomegaly; and marked alleviation of liver necrosis, fibrosis, and inflammation. Survival was significantly improved in the treated mice. Finally, a laboratory-induced replenishment of aging neutrophils in the circulation resulted in acute vaso-occlusive crises and death within 10-30 hours in all affected mice.
“Together, these data suggest that the microbiota regulates aged neutrophil numbers, thereby affecting both acute vaso-occlusive crisis and the ensuing chronic tissue damage in sickle-cell disease,” Dr. Zhang and his associates said.
To assess how their findings applied to human beings, the investigators next studied 23 patients with sickle-cell disease who were not taking antibiotics, 11 patients with sickle-cell disease who were taking penicillin to prevent life-threatening infections, and 9 healthy control subjects. Compared with controls, only the patients who weren’t taking antibiotics showed a dramatic increase in circulating aged neutrophils. This protective effect of antibiotics was consistent across all ages, both genders, and regardless of hydroxyurea intake. Now, a prospective study involving age-matched participants is needed to confirm that antibiotics, by reducing the gut microbiota, decrease aged neutrophils in the circulation and thereby improve vaso-occlusive disease, the researchers said.
The American Heart Association, the National Institutes of Health, and the New York State Stem Cell Science Program funded the study. Dr. Zhang and his associates reported having no relevant disclosures.
FROM NATURE
Key clinical point: The body’s microbiota was found to regulate the aging of circulating neutrophils, a discovery that points the way to easily and markedly improve the chronic tissue damage induced by sickle-cell and perhaps other diseases.
Major finding: In an in vivo mouse model of sickle-cell disease, mice given antibiotics showed marked microbiota depletion; enhanced blood flow; significantly reduced splenomegaly; marked alleviation of liver necrosis, fibrosis, and inflammation; and significantly improved survival.
Data source: A series of in vitro, in vivo, and human studies, the latter involving 23 patients with SCD, 11 with SCD taking prophylactic antibiotics, and 9 healthy control subjects.
Disclosures: The American Heart Association, the National Institutes of Health, and the New York State Stem Cell Science Program funded the study. Dr. Zhang and his associates reported having no relevant disclosures.