User login
- Though all non-narcotic analgesics have equivalent efficacy against tension-type headache, ibuprofen’s generally favorable side-effect profile makes it a reasonable first choice.
Whereas quantitative and qualitative analyses of 41 randomized controlled trials (RCTs) strongly suggests that all types of NSAIDs are more effective than placebo (>50% pain relief) against an acute episode of tension-type headache (TTH), the evidence also shows that no single nonsteroidal anti-inflammatory drug (NSAID) is more effective than another in this setting.
How, then, to choose an NSAID? Many of the 41 articles we reviewed reported on the side effects of NSAIDs. No clear differences were reported in the number of side effects between the NSAIDs and placebo. However, differences were found among the types of NSAIDs. Our results agree with those found by Henry et al,1 who concluded from their meta-analysis that ibuprofen, compared with other NSAIDs, had the lowest relative risk of serious gastrointestinal complications. Given the lack of important differences in efficacy among NSAIDs for relieving an acute episode of TTH, using the most effective dose of a drug that is well tolerated by a patient is a reasonable basis for selection. Ibuprofen, therefore, generally may be advocated.
When acetaminophen is preferred. Our results suggest NSAIDs might be more effective than acetaminophen for TTH. However, because NSAIDs are allergenic for some people, and they must not be used in association with anticoagulants,2 acetaminophen might be an alternative in these situations. When giving acetaminophen, the dose of the medication might be important due to a possible dose-response relationship.
Why this review was needed
Tension-type headache, also known as tension headache or muscle contraction headache, is the most commonly experienced type of headache (see Episodic tension-type headache). Population-based studies suggest prevalence rates of 35% to 40% in adults.3-5
Persons experiencing an acute episode of TTH most often self-treat with mild, non-narcotic analgesics for initial pain relief. Studies have suggested that acetaminophen and NSAIDs like aspirin, ibuprofen, naproxen, and ketoprofen are effective in reducing headache symptoms. But a variety of drugs, dosages, and combinations have been described. No systematic review has, until now, described the efficacy and tolerability of analgesics for the treatment of acute episodes of TTH. Good quality-controlled trials and a systematic review form the basis for evidence-based treatment guidelines, which provide a basis for the individual patient.
Episodic TTH has been defined in the classification of the International Headache Society (IHS) as headache frequency of greater than 10 lifetime episodes, but fewer than 15 episodes per month; an average episode duration of 30 minutes to 7 days; and with at least 2 quality of pain features (ie, mild or moderate pain intensity, bilateral, pressing or tightening [nonpulsating] feeling, and no exacerbation by exercise).7 In addition, the headache does not have the IHS-defining features of migraine (ie, nausea, vomiting, or photophobia and phonophobia). The definition of chronic TTH is identical to those for episodic TTH, except that the episode frequency is 15 or more episodes per month for at least 6 months, and 1 associated symptom of nausea, photophobia, or phonophobia is permitted.
We aimed to describe and assess the data from RCTs concerning the efficacy and tolerability of analgesics for the treatment of acute episodes of TTH in adult patients. Details of our Methods and Results follow.
Methods
Search strategy
Medline and EMBASE were searched from inception to January 2005 using the terms tension-type headache, tension headache, stress headache, or muscle contraction headache together with the search strategy for identifying RCTs described by Robinson and Dickerson.6 The Cochrane Controlled Trials Register was searched using the words tension headache or tension-type headache or muscle contraction headache. Additional strategies for identifying trials included searching the reference lists of review articles and included studies.
Study selection
Only RCTs including analgesic medicine used in the treatment or management of TTH conducted among adult patients (aged 18 years or older), with reasonable criteria designed to distinguish TTH from migraine, were selected for our review. The use of a specific set of diagnostic criteria (eg, IHS 1988 and Ad Hoc 1962)7,8 was not required, but TTH diagnoses had to be based on at least some of the distinctive features of TTH—eg, bilateral in location, no nausea or vomiting, mild or moderate intensity, or no exacerbation by exercise.
Main outcome measures were pain relief or recovery over 2 to 6 hours.
Two authors (LD, AV) independently screened titles and abstracts of identified studies for eligibility. All potentially relevant studies were retrieved as full papers and then again independently reviewed by 2 authors (LD, AV). Disagreements were resolved through consensus where possible, or by arbitration with a third author (MB). Crossover designs often presented data from treatment groups, as if the trial was a parallel group trial. The results from these studies were excluded from data-analysis if no results from both arms were presented or a binary correlation coefficient was available.9
Methodological quality and data extraction
Two authors (LD with MB, BK, or AV) independently rated the methodological quality of the included trials using the Delphi list.10 The Delphi list is a generic criteria list developed by international consensus and consists of the following 9 items: 1) randomization; 2) adequate allocation concealment; 3) groups similar at baseline; 4) specification of eligibility criteria; 5) blinding of outcome assessor; 6) blinding of care provider; 7) blinding of patient; 8) presentation of point estimates and measures of variability; 9) intention-to-treat-analysis. One extra item was added: 10) withdrawal or dropout rate unlikely to cause bias. All selected methodological criteria were scored as yes (=1), no (=0) or don’t know (=0). A quality score of a trial was computed by counting the number of positive scores, with equal weights applied on all items. In case of a disagreement between the 2 authors, consensus was used to resolve disagreement. When consensus could not be reached, a third author made the final decision (MB or AV).
Extraction of data from the original reports was performed by 1 author (LD) and checked by a second (AV). Disagreements were resolved by consensus. Extracted information included (if available) demographic data, detailed description of the intervention and control (ie, dose given, study duration, rescue medication), data on pain relief or recovery, and information on adverse effects measured during a treatment period of 2 to 6 hours. When a trial protocol permitted the use of rescue medication prior to the outcome time (2 to 6 hours), then the latest outcome assessment not confounded by the use of rescue medication was extracted
Data analysis
A quantitative analysis was limited to clinically homogenous studies for which the study populations, interventions and outcomes were considered to be similar. For each study, the number of patients who were recovered (often defined as more than 50% pain relief) was used to calculate relative risk (RR) with 95% confidence interval (CI). RRs and 95% CI were presented using the random effects model. Data are presented as treatment success, indicating that an RR >1 represents a better outcome for the first mentioned medication group.
In parallel studies, when more than 1 comparison from the same study (ie, aspirin 650 mg vs placebo and ibuprofen 400 mg vs placebo) was used for the statistical pooling of NSAIDs vs placebo, the results from the placebo group were evenly spread out over the 2 comparisons and the number of patients in the placebo group was divided by 2 in order to prevent double counting (personal communication RJPM Scholten, Dutch Cochrane Centre).
Because only a subset of available trials provides sufficient data for inclusion in the quantitative analysis, also a qualitative analysis was performed. We summarized findings by strength of evidence, nature of intervention and control treatments. The evidence was judged to be strong when multiple high-quality trials produced generally consistent findings.11 Results were considered consistent if over 75% of the studies reported similar results on the same outcome measure. It was judged to be moderate when multiple low-quality trials or one high-quality and 1 or more low-quality trials produced generally consistent findings. Evidence was considered to be limited when only 1 low-quality RCT existed and conflicting when the findings of existing trials were inconsistent. We arbitrarily regarded trials with methodological quality scores of 6 or more as of high quality.11
Relation between funding source of the RCTs and conclusions
We extracted the sources of funding of the RCTs from the text, statements of sources of support, authors’ affiliations, and acknowledgements. Funding sources were classified as nonprofit organizations, not reported, both nonprofit and for-profit organizations, or for-profit organizations.12 For-profit organizations were defined as companies that might acquire financial gain or loss depending on the outcome of the trial.12 Funding included provision of grants, study material (drug, placebo), or manpower (authorship, statistical analysis, or other assistance).12 We used the effect sizes between medication(s) and placebo to evaluate whether funding source affected outcome.
Results
Search results
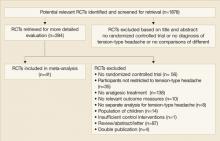
A total of 1878 publications were identified by our search strategy. Finally, 41 RCTs met our inclusion criteria and 4 papers concerned double publications (FIGURE 1),13-16 leaving a total of 41 trials which were included in this review. Thirteen of these RCTs used a crossover design.15,7-27
FIGURE 1
How the 41 trials made our cut for the review
Description of studies
Full details of the included studies are presented in TABLE W1. The number of participants included in each trial ranged from 12 to 900 (mean=252.7 patients), with a total of 10,363 patients included. The mean percentage of participants who dropped out from the trials was 15.2% (range=0%–61.9%). Age of participants (for studies reporting this information) ranged from 18 to 87 years. Overall, the percentage of women was generally higher than men (mean=69.3%; range=36%–97%). Fifteen trials used the criteria of the International Headache Society to classify TTH,14,17,19-21,24,28-36 12 trials used the Ad Hoc Committee’s criteria,13,23,26,37,45 while the remaining studies did not use a formal classification.
Twenty-five studies compared 1 or more types of NSAIDs with placebo,13-17,22-24,26-36,38,41-43,45-47 17 studies compared 1 or more doses of acetaminophen with placebo,17-21,25,30-34,41,44-46,48,49 7 studies compared different types of NSAIDs,15,26,28,29,35-37 9 studies compared 1 or more types of NSAIDs with acetaminophen,17,30-34,41,45,46 and 13 studies compared other analgesics with placebo.15,18,25,27,39,40,44,49,50-53
The quality score (with positive items in parenthesis) is presented in the “Notes” section of TABLE W1. The interobserver reliability of the methodological quality assessment was high (κ=0.85). There was disagreement between the 2 authors in 7.5% of the criteria, but after consensus no disagreement persisted. The median quality score was 5 (range 1–9). Using a cutoff point of 6 out of 10 criteria, 15 studies (36.6%) were considered to be of high quality.15,17,19,21,22,24,25,28-30,32-34,36
Only 1 study reported a concealed randomization method.34 Other methodological flaws, which often scored “negative” or “unclear,” were blinding of the care provider (unclear 88%) and an intention-to-treat analysis (unclear 30% and negative 60%).
Effectiveness of analgesics
TABLE 1 gives the quantitative analysis for high-quality studies, low-quality studies, and for all studies for the different comparisons of NSAIDs, acetaminophen, and placebo.
TABLE 1
Quantitative analysis for the different studies for the comparisons of NSAIDs, acetaminophen and placebo
| HIGH-QUALITY TRIALS | LOW-QUALITY TRIALS | ALL TRIALS | |||||
|---|---|---|---|---|---|---|---|
| N/n | RR (95% CI) | N/n | RR (95% CI) | N/n | RR (95% CI) | ||
| 1. NSAIDs vs placebo | 7/13 | 1.5 (1.3–1.8)* | 8/15 | 2.0 (1.4–2.7)* | 15/28 | 1.6 (1.4–2.0)* | |
| 2. Acetaminophen vs placebo | 5/6 | 1.4 (1.04–1.8)* | 3/3 | 1.6 (0.9–2.7) | 8/9 | 1.4 (1.1–1.8)* | |
| 500 mg vs placebo | 1/1 | 1.1 (0.8–1.5) | 1/1 | 1.1 (0.8–1.5) | |||
| 1000 mg vs placebo | 4/5 | 1.4 (0.97–2.0) | 3/3 | 1.6 (0.9–2.7) | 7/8 | 1.5 (1.1–2.0)8 | |
| 4. NSAIDs vs acetaminophen | 5/7 | 1.1 (0.96–1.4) | 2/2 | 2.2 (1.4–3.4)* | 7/9 | 1.3 (1.04–1.5)* | |
| 3. NSAIDs vs NSAIDs | |||||||
| Ibuprofen 400/800 mg vs aspirin 650 mg37 | 1/2 | 1.2 (0.6–2.2) | |||||
| Ketoprofen 12.5/25/50 mg vs ibuprofen 200 mg29,36 | 1/2 | 1.1 (0.8–1.5) | 1/2 | 1.5 (0.8–2.7) | 2/4 | 1.2 (0.9–1.6) | |
| Ketoprofen 12.5/25 mg vs naproxen 275 mg29 | 1/2 | 0.96 (0.7–1.3) | |||||
| Naproxen 275 mg vs ibuprofen 200 mg29 | 1/1 | 0.9 (0.7–1.2) | |||||
| Metamizol 500/1000 mg vs aspirin 1000 mg30 | 1/2 | 1.2 (0.9–1.7) | |||||
| Diclofenac 12.5/25 mg vs ibuprofen 400 mg55 | 1/2 | 1.1 (0.8–1.5) | |||||
| N/n=number of trials/total number of comparisons; RR: relative risk; CI: confidence interval. *P<.05. | |||||||
1. NSAIDs vs placebo
Twenty-five studies compared one or more types of NSAIDs with placebo, of which 10 are of high quality.15,17,22,24,29,30,32-34,36,45
Quantitative analysis. Sufficient data were available in 15 studies,13,14,29-38,41,45,47 of which 6 were of high quality.29,30,32-34,36,45 Because some trials included 3 or more treatment groups, data were available for 28 comparisons. We found a significant effect in favor of NSAIDs compared with placebo on short-term pain relief (see TABLE 1 and FIGURE W1).
Qualitative analysis. The 10 high-quality studies reported 30 comparisons, of which in 26 (86.6%) NSAIDs were significantly more effective compared with placebo for short-term pain relief (strong evidence).
Adverse events. Twenty studies reported during a 2 to 6 hours treatment period data on adverse events. For the NSAID group (n=2061) frequently mentioned side effects were nausea (4.6%), photophobia (3.1%), vomiting (2.7%), phonophobia (1.7%), aching limbs (1.2%), dizziness (1.1%), and drowsiness (1.0%). For the placebo group (n=1323), these were nausea (7.0%), photophobia (4.8%), vomiting (3.9%), phonophobia (3.4%), aching limbs (2.0%), drowsiness (1.7%), and dizziness (1.0%). The pooled RR for the number of patients reporting side effects for 14 studies with sufficient data was 0.96 (95% CI, 0.7–1.3), indicating no significant difference.
2. Acetaminophen vs placebo
Seventeen studies compared 1 or more doses of acetaminophen with placebo; 9 were high-quality studies.17,19,21,25,30-34,45
Quantitative analysis. The pooled analysis of 5 high-quality trials30,32-34,45 and 3 low-quality trials31,41,44 showed that acetaminophen was significantly more effective compared with placebo for patients on short-term pain relief (TABLE 1 and FIGURE W2). This result was due to the studies comparing acetaminophen with placebo. The only high-quality trial34 with acetaminophen 500 mg failed to show a difference in short-term pain relief compared with placebo (TABLE 1).
Qualitative analysis. The 9 high-quality studies reported 16 comparisons, of which 10 (62.5%) mentioned that acetaminophen showed significantly more pain relief than placebo (conflicting evidence). In 2 high-quality studies,17,34 we found no significant differences between acetaminophen 500 mg and placebo (strong evidence), but in the 9 high-quality studies, in 10 out of 14 comparisons (71.4%) acetaminophen 1000 mg showed significantly more pain relief compared with placebo (conflicting evidence).
Adverse events. Twelve studies reported data on adverse events. For the acetaminophen group (n=3715), frequently mentioned side effects were stomach discomfort (3.9%), dizziness (1.6%), nervousness (0.7%), nausea (0.4%), and drowsiness (0.3%). For the placebo group (n=3700), these were stomach discomfort (3.7%), nervousness (0.7%), nausea (0.6%), dizziness (0.5%), and drowsiness (0.3%). The pooled RR for the number of patients reporting side effects was 1.3 (95% CI, 0.9–1.7), indicating no significant difference.
3. NSAIDs vs acetaminophen
Nine studies compared 1 or more types of NSAIDs with acetaminophen, of which 6 are of high-quality.17,30-34,45
Quantitative analysis. The pooled analysis of 5 high-quality studies30-34,45 and 2 low-quality studies31,41 showed a significant difference in short-term pain relief in favor of NSAIDs (TABLE 1).
Qualitative analysis. Six high-quality studies showed that in 9 out of 13 comparisons (69%) NSAIDs were not significantly more effective than acetaminophen for short-term pain relief in patients with acute episodes of TTH (conflicting evidence).
Adverse events. Seven studies reported data on adverse events. The pooled RR for number of patients reporting side effects was 1.3 (95% CI, 0.97–1.6), indicating no significant difference.
4. Comparison between different NSAIDs
Seven studies compared different types of NSAIDs,15,26,28,29,35-37 of which 4 provided data.
Quantitative and qualitative analysis. The analysis the between different types of NSAIDs no differences in short-term pain relief can be found; RR vary between 0.9 and 1.5 (TABLE 1).
Adverse events. The adverse effects were reported involving the central nervous system (ie, dizziness, drowsiness, vertigo), gastrointestinal system (ie, nausea, vomiting, gastrointestinal upset or discomfort), and the body as a whole (ie, light-headed, fatigue, cramps, asthenia, chills).
Naproxen and zomepirac gave more adverse events involving the central nervous system than aspirin, ibuprofen, and ketoprofen. Naproxen and zomepirac were also more often associated with gastrointestinal side effects than ibuprofen and ketoprofen.
Furthermore, aspirin was more associated with gastrointestinal complaints than ibuprofen. Side effects such as fatigue and cramps (body as whole) occurred significantly more often with ketoprofen compared with aspirin and ibuprofen, naproxen compared with ketoprofen, and zomepirac compared with aspirin.
5. Other analgesics vs placebo
Qualitative analysis. There is insufficient evidence to either support or refute the effectiveness of all other analgesics compared with placebo, due to the fact that most analgesics were a unique combination of analgesics with caffeine or peppermint oil. Also, the low methodological quality of nearly all these studies and the low number of studies per comparison made drawing conclusions difficult.
Optalidon and Tonopan were compared with placebo in 3 substudies of 1 high-quality study, and we found significant more pain relief using these analgesics than placebo.15 No adverse events were stated in these studies.
The combination of acetaminophen and caffeine was compared with placebo in 2 studies of high quality25,49 showed that the combination of acetaminophen with caffeine is more effective than placebo (moderate evidence).
The combination of acetaminophen, aspirin, and caffeine was compared with placebo in 4 substudies of the same high-quality study.25 Data from these studies suggest that this combination is significantly more effective than placebo. All groups reported low numbers of side effects as stomach discomfort, nervousness, and dizziness.
Relation between funding source and effect estimates
The pooled effect estimates in placebo-controlled trials stratified by funding are shown in TABLE 2. No major differences in effect sizes were found between the different funding sources.
TABLE 2
Relation between funding source and effect estimate, intervention vs placebo only
| NUMBER OF COMPARISONS (TRIALS) | NUMBER OF COMPARISONS IN HIGH QUALITY STUDIES (TRIALS) | EFFECT ESTIMATE ALLSTUDIES: RR (95% CI) | EFFECT ESTIMATE HIGH QUALITY STUDIES: RR (95% CI) | |
|---|---|---|---|---|
| Non-profit organizations | 0 | 0 | — | — |
| Not reported | 4 (2) | 0 | 1.4 (0.8–2.6) | — |
| Non-profit and for-profit organizations | 26 (11) | 11 (4) | 1.7 (1.4–2.1) | 1.4 (1.1–1.7) |
| For-profit organizations | 14 (7) | 8 (3) | 1.4 (1.2–1.6) | 1.2 (1.06–1.4) |
| All studies | 44 (20) | 19 (7) | 1.5 (1.3–1.8) | 1.4 (1.1–1.7) |
| *P=.006 using χ2 test | ||||
Methodological quality of included studies
This review shows that many RCTs on the efficacy of analgesics in TTH have methodological shortcomings. Using a cut-off point of 6 out of 10 criteria, only 35% of the included studies were found to be of high quality. Most authors failed to explicitly specify the method of treatment allocation and blinding procedure. In many studies authors stated that the trial had a double-blind procedure, however, when the blinding procedure was not explicitly reported (ie, identical looking tablets) we did not score 1 or more blinding items positive. These flaws can be prevented in future trials.
We are unaware of any prior systematic reviews or meta-analyses that have assessed the efficacy and tolerability of analgesics in the treatment of acute episodes of tension-type headache in adults. We conducted the review according to the high Cochrane standard, resulting in a review of high validity. Our review succeeded in identifying a large number of only randomized trials. Also the methodological quality did not explain the possible association between funding and effect estimates.
Although systematic reviews offer the least biased method of summarizing research literature, our review should be considered with the following limitations in mind. First, we decided not to contact the authors for additional information, because most trials were published before 1995. Second, some of the medications have only been evaluated in 1 or 2 studies, which may limit the generalizability of the findings. We do not think these factors have influences our conclusions.
CORRESPONDENCE
Arianne P. Verhagen, PhD, Department of General Practice, Erasmus Medical Centre, PO Box 1738, 3000 DR Rotterdam, The Netherlands. E-mail: [email protected]
1. Henry D, Lim LLY, Garcia Rodriguez LA, et al. Variability in risk of gastrointestinal complications with individual nonsteroidal anti-inflammatory drugs: results of a collaborative meta-analysis. BMJ 1996;312:1563-1566.
2. D’Amico D, Grazzi L, Leone M, Moschiano F, Bussone G. A review of the treatment of primary headaches. Part II: Tension-type headache. Ital J Neurol Sci 1998;19:2-9.
3. Schwartz BS, Stewart WF, Simon D, Lipton RB. Epidemiology of tension-type headache. JAMA 1998;279:381-383.
4. Rasmussen BK. Epidemiology of headache. Cephalalgia 1995;15:45-68.
5. Pryse-Philips W, Findlay H, Tugwell P, Edmeads J, Murray TJ, Nelson RF. Canadian population survey on the clinical, epidemiologic and societal impact of migraine and tension-type headache. Can J Neurol Sci 1992;19:333-339.
6. Robinson KA, Dickerson K. Development of a highly sensitive search strategy for the retrieval of reports of controlled trials using PubMed. Int J Epidemiol 2002;31:150-153.
7. Headache Classification Committee of the International Headache Society. Classification and diagnostic criteria for headache disorders, cranial neuralgias and facial pain. Cephalalgia 1988;8(Suppl 7):1-96;Headache Classification Committee of the International Headache Society. The International Classification of headache disorders.Cephalalgia 2004; 24(Suppl 1): 1-152.
8. Ad Hoc Committee on the Classification of Headache of the National Institute of Neurological Diseases and Blindness. Classification of headache. JAMA 1962;179:717-718.
9. Elbourne DR, Altman DG, Higgins JP, Curtin F, Worthington HV, Vail A. Meta-analyses involving crossover trials: methodological issues. Int J Epidemiol 2002;31:140-149.
10. Verhagen AP, de Vet HCW, de Bie RA, et al. The art of quality assessment of RCTs included in systematic reviews. J Clin Epidemiol 2001;54:651-654.
11. Van Tulder MW, Furlan A, Bombarbier C, Bouter L. Editorial Board of the Cochrane Collabaration Back Review Group. Updated method guidelines for systematic reviews in the Cochrane Collaboration Back review Group. Spine 2003;28:1290-1299.
12. Als-Nielsen B, Chen W, Gluud C, Kjaergard LL. Association of funding and conclusions in randomized drug trials. A reflection of treatment effect or adverse events? JAMA 2003;290:921-928.
13. Diamond S. Zomepirac in the symptomatic treatment of muscle contraction headache. J Clin Pharmacol 1980;20:298-302;Diamond S, Medina JL. A double-blind study of zomepirac sodium and placebo in the treatment of muscle contraction headache. Headache 1981; 21:45-48.
14. Diamond S, Balm TK, Freitag FG. Ibuprofen plus caffeine in the treatment of tension-type headache. Clin Pharmacol Ther 2000;68:312-319;Diamond S, Freitag FG. The use of ibuprofen plus caffeine to treat tension-type headache. Curr Pain Headache Rep 2001; 5:472-478.
15. von Graffenried B, Hill RC, Nüesch E. Headache as a model for assessing mild analgesic drugs. J Clin Pharmacol 1980;20:131-144;von Graffenried B, Nüesch B. Non-migrainous headache for the evaluation of oral analgesics. Br J Clin Pharmacol 1980; 10(suppl2):225S-231S.
16. Friedman AP, Boyles WF, Elkind AH, et al. Fiorinal with codeine in the treatment of tension headache-the contribution of components to the combination drug. Clin Ther 1988;10:303-315;Hwang DS, Mietlowski MJ, Friedman AP. Fiorinal with Codeine in the management of tension headache: impact of placebo response. Clin Ther 1987; 9:201-222.
17. Dahlöf CG, Jacobs LD. Ketoprofen, paracetamol and placebo in the treatment of episodic tension-type headache. Cephalalgia 1996;16:117-123.
18. Gilbert MM, De Sola Pool N, Schecter C. Analgesic/calmative effects of acetaminophen and phenyltoloxamine in treatment of simple nervous tension accompanied by headache. Curr Ther Res Clin Exp 1976;20:53-58.
19. Göbel H, Fresenius J, Heinze A, Dworschak M, Soyka D. Effectiveness of peppermint oil and paracetamol in the treatment of tension headache [German]. Nervenarzt 1996;67:672-681.
20. Göbel H, Heinze A, Lurch A, Dworschak M. Essential oils in the therapy of tension headache [German]. Z Allg Med 1998;74:223-228.
21. Göbel H, Heinze A, Dworschak M, Heinze-Kuhn Stolze H. Analgesic efficacy and tolerability of locally applied oleum menthae piperitae preparation LI 170 in patients with migraine or tension-type headache [German]. Z Allg Med 2001;77:287-295.
22. Guidotti M, Zanasi S, Garagiola U. Pirprofen in the treatment of migraine and episodic headache attacks: a placebo-controlled crossover clinical trial. J Int Med Res 1989;17:48-54.
23. Langemark M, Olesen J. Effervescent ASA versus solid ASA in the treatment of tension headache. A double-blind, placebo controlled study. Headache 1987;27:90-95.
24. Laveneziana D, Speranza R, Raulli P, Paredi G. Comparative efficacy of ibuprofen arginine and beta-cyclodextrin piroxicam as treatment for tension-type headache. Clin Drug Invest 1996;11(Suppl 1):22-26.
25. Migliardi JR, Armellino JJ, Friedman M, Gillings DB, Beaver WT. Caffeine as an analgesic adjuvant in tension headache. Clin Pharmacol Ther 1994;56:576-586.
26. Ryan RE, Sr. Motrin- A new agent for the symptomatic treatment of muscle contraction headache. Headache 1977;16:280-283.
27. Wood A, von Graffenried B. Fluproquazone: Analgesic activity in outpatients with non-migrainous headache. Arzneim-Forsch/Drug Res 1981;31:914-917.
28. Lange R, Lentz R. Comparison ketoprofen, ibuprofen and naproxen sodium in the treatment of tension-type headache. Drugs Exp Clin Res 1995;21:89-96.
29. Martinez-Martin P, Raffaelli E, Jr, Titus F, et al. Efficacy and safety of metamizol vs. acetylsalicylic acid in patients with moderate episodic tension-type headache: a randomized, double-blind, placebo- and active-controlled, multicentre study. Cephalalgia 2001;21:604-610.
30. Mehlisch DR, Weaver M, Fladung B. Ketoprofen, acetaminophen, and placebo in the treatment of tension headache. Headache 1998;38:579-589.
31. Packman B, Packman E, Doyle G, et al. Solubilized ibuprofen: evaluation of onset, relief, and safety of a novel formulation in the treatment of episodic tension-type headache. Headache 2000;40:561-567.
32. Prior MJ, Cooper KM, May LG, Bowen DL. Efficacy and safety of acetaminophen and naproxen in the treatment of tension-type headache. A randomized, double-blind, placebo-controlled trial. Cephalalgia 2002;22:740-748.
33. Steiner TJ, Lange R. Ketoprofen (25 mg) in the symptomatic treatment of episodic tension-type headache: double-blind placebo-controlled comparison with acetaminophen (1000 mg). Cephalalgia 1998;18:38-43.
34. Steiner T, Lange R, Voelker M. Aspirin in episodic tension-type headache: placebo-controlled dose-ranging comparison with paracetamol. Cephalalgia 2003;23:59-66.
35. van Gerven JM, Schoemaker RC, Jacobs LD, et al. Self-medication of a single headache episode with ketoprofen, ibuprofen or placebo, home-monitored with an electronic patient diary. Br J Clin Pharmacol 1996;42:475-481.
36. Kubitzek F, Ziegler G, Gold MS, Liu JMH, Ionescu E. Low-dose diclofenac potassium in the treatment of episodic tension-type headache. European J Pain 2003;7:155-162.
37. Diamond S. Ibuprofen versus aspirin and placebo in the treatment of muscle contraction headache. Headache 1983;23:206-210.
38. DiSerio FJ, Friedman AP, Parno J, Singer JM. Proquazone for tension headache-a multicenter trial. Headache 1985;25:127-133.
39. Friedman AP. Assessment of Fiorinal with Codeine in the treatment of tension headache. Clin Ther 1986;8:703-721.
40. Friedman AP, DiSerio FJ. Symptomatic treatment of chronically recurring tension headache: a placebo-controlled, multicenter investigation of Fioricet and acetaminophen with codeine. Clin Ther 1987;10:69-81.
41. Miller DS, Talbot CA, Simpson W, Korey A. A comparison of naproxen sodium, acetaminophen and placebo in the treatment of muscle contraction headache. Headache 1987;27:392-396.
42. Sargent JD, Peters K, Goldstein J, Madison DS, Solbach P. Naproxen sodium for muscle contraction headache treatment. Headache 1988;28:180-182.
43. Schachtel BP, Thoden WR. Onset of action of ibuprofen in the treatment of muscle-contraction headache. Headache 1988;28:471-474.
44. Schachtel BP, Thoden WR, Konerman JP, Brown A, Chaing DS. Headache pain model for assessing and comparing the efficacy of over-the-counter analgesic agents. Clin Pharmacol Ther 1991;50:322-329.
45. Schachtel BP, Furey SA, Thoden WR. Nonprescription ibuprofen and acetaminophen in the treatment of tension-type headache. J Clin Pharmacol 1996;36:1120-1125.
46. Peters BH, Fraim CJ, Masel BE. Comparison of 650 mg aspirin and 1,000 mg acetaminophen with each other, and with placebo in moderately severe headache. Am J Med 1983;74:36-42.
47. Ryan RE, Sr, Ryan RE, Jr. Symptomatic treatment of tension headache. Ear Nose Throat J 1979;58:423-426.
48. Schattner P, Randerson D. Tiger Balm as a treatment of tension headache. A clinical trial in general practice. Aust Fam Physician 1996;25:216, 218,220passim
49. Ward N, Whitney C, Avery D, Dunner D. The analgesic effects of caffeine in headache. Pain 1991;44:151-155.
50. Borges J, Zavaleta C. Study of a new analgesic compound in the treatment of tension headache. J Int Med Res 1976;4:74-78.
51. Thorpe P. Controlled and uncontrolled studies on “Fiorinal-PA” for symptomatic relief in tension headache. Med J Aust 1970;2:180-181.
52. Kagan G, Masheter HC. A controlled study of short-term treatment of tension headache. Curr Med Res Opin 1978;5:709-713.
53. Scheepers F. Syndol in the treatment of tension headache. Med Proc 1971;359-368.
- Though all non-narcotic analgesics have equivalent efficacy against tension-type headache, ibuprofen’s generally favorable side-effect profile makes it a reasonable first choice.
Whereas quantitative and qualitative analyses of 41 randomized controlled trials (RCTs) strongly suggests that all types of NSAIDs are more effective than placebo (>50% pain relief) against an acute episode of tension-type headache (TTH), the evidence also shows that no single nonsteroidal anti-inflammatory drug (NSAID) is more effective than another in this setting.
How, then, to choose an NSAID? Many of the 41 articles we reviewed reported on the side effects of NSAIDs. No clear differences were reported in the number of side effects between the NSAIDs and placebo. However, differences were found among the types of NSAIDs. Our results agree with those found by Henry et al,1 who concluded from their meta-analysis that ibuprofen, compared with other NSAIDs, had the lowest relative risk of serious gastrointestinal complications. Given the lack of important differences in efficacy among NSAIDs for relieving an acute episode of TTH, using the most effective dose of a drug that is well tolerated by a patient is a reasonable basis for selection. Ibuprofen, therefore, generally may be advocated.
When acetaminophen is preferred. Our results suggest NSAIDs might be more effective than acetaminophen for TTH. However, because NSAIDs are allergenic for some people, and they must not be used in association with anticoagulants,2 acetaminophen might be an alternative in these situations. When giving acetaminophen, the dose of the medication might be important due to a possible dose-response relationship.
Why this review was needed
Tension-type headache, also known as tension headache or muscle contraction headache, is the most commonly experienced type of headache (see Episodic tension-type headache). Population-based studies suggest prevalence rates of 35% to 40% in adults.3-5
Persons experiencing an acute episode of TTH most often self-treat with mild, non-narcotic analgesics for initial pain relief. Studies have suggested that acetaminophen and NSAIDs like aspirin, ibuprofen, naproxen, and ketoprofen are effective in reducing headache symptoms. But a variety of drugs, dosages, and combinations have been described. No systematic review has, until now, described the efficacy and tolerability of analgesics for the treatment of acute episodes of TTH. Good quality-controlled trials and a systematic review form the basis for evidence-based treatment guidelines, which provide a basis for the individual patient.
Episodic TTH has been defined in the classification of the International Headache Society (IHS) as headache frequency of greater than 10 lifetime episodes, but fewer than 15 episodes per month; an average episode duration of 30 minutes to 7 days; and with at least 2 quality of pain features (ie, mild or moderate pain intensity, bilateral, pressing or tightening [nonpulsating] feeling, and no exacerbation by exercise).7 In addition, the headache does not have the IHS-defining features of migraine (ie, nausea, vomiting, or photophobia and phonophobia). The definition of chronic TTH is identical to those for episodic TTH, except that the episode frequency is 15 or more episodes per month for at least 6 months, and 1 associated symptom of nausea, photophobia, or phonophobia is permitted.
We aimed to describe and assess the data from RCTs concerning the efficacy and tolerability of analgesics for the treatment of acute episodes of TTH in adult patients. Details of our Methods and Results follow.
Methods
Search strategy
Medline and EMBASE were searched from inception to January 2005 using the terms tension-type headache, tension headache, stress headache, or muscle contraction headache together with the search strategy for identifying RCTs described by Robinson and Dickerson.6 The Cochrane Controlled Trials Register was searched using the words tension headache or tension-type headache or muscle contraction headache. Additional strategies for identifying trials included searching the reference lists of review articles and included studies.
Study selection
Only RCTs including analgesic medicine used in the treatment or management of TTH conducted among adult patients (aged 18 years or older), with reasonable criteria designed to distinguish TTH from migraine, were selected for our review. The use of a specific set of diagnostic criteria (eg, IHS 1988 and Ad Hoc 1962)7,8 was not required, but TTH diagnoses had to be based on at least some of the distinctive features of TTH—eg, bilateral in location, no nausea or vomiting, mild or moderate intensity, or no exacerbation by exercise.
Main outcome measures were pain relief or recovery over 2 to 6 hours.
Two authors (LD, AV) independently screened titles and abstracts of identified studies for eligibility. All potentially relevant studies were retrieved as full papers and then again independently reviewed by 2 authors (LD, AV). Disagreements were resolved through consensus where possible, or by arbitration with a third author (MB). Crossover designs often presented data from treatment groups, as if the trial was a parallel group trial. The results from these studies were excluded from data-analysis if no results from both arms were presented or a binary correlation coefficient was available.9
Methodological quality and data extraction
Two authors (LD with MB, BK, or AV) independently rated the methodological quality of the included trials using the Delphi list.10 The Delphi list is a generic criteria list developed by international consensus and consists of the following 9 items: 1) randomization; 2) adequate allocation concealment; 3) groups similar at baseline; 4) specification of eligibility criteria; 5) blinding of outcome assessor; 6) blinding of care provider; 7) blinding of patient; 8) presentation of point estimates and measures of variability; 9) intention-to-treat-analysis. One extra item was added: 10) withdrawal or dropout rate unlikely to cause bias. All selected methodological criteria were scored as yes (=1), no (=0) or don’t know (=0). A quality score of a trial was computed by counting the number of positive scores, with equal weights applied on all items. In case of a disagreement between the 2 authors, consensus was used to resolve disagreement. When consensus could not be reached, a third author made the final decision (MB or AV).
Extraction of data from the original reports was performed by 1 author (LD) and checked by a second (AV). Disagreements were resolved by consensus. Extracted information included (if available) demographic data, detailed description of the intervention and control (ie, dose given, study duration, rescue medication), data on pain relief or recovery, and information on adverse effects measured during a treatment period of 2 to 6 hours. When a trial protocol permitted the use of rescue medication prior to the outcome time (2 to 6 hours), then the latest outcome assessment not confounded by the use of rescue medication was extracted
Data analysis
A quantitative analysis was limited to clinically homogenous studies for which the study populations, interventions and outcomes were considered to be similar. For each study, the number of patients who were recovered (often defined as more than 50% pain relief) was used to calculate relative risk (RR) with 95% confidence interval (CI). RRs and 95% CI were presented using the random effects model. Data are presented as treatment success, indicating that an RR >1 represents a better outcome for the first mentioned medication group.
In parallel studies, when more than 1 comparison from the same study (ie, aspirin 650 mg vs placebo and ibuprofen 400 mg vs placebo) was used for the statistical pooling of NSAIDs vs placebo, the results from the placebo group were evenly spread out over the 2 comparisons and the number of patients in the placebo group was divided by 2 in order to prevent double counting (personal communication RJPM Scholten, Dutch Cochrane Centre).
Because only a subset of available trials provides sufficient data for inclusion in the quantitative analysis, also a qualitative analysis was performed. We summarized findings by strength of evidence, nature of intervention and control treatments. The evidence was judged to be strong when multiple high-quality trials produced generally consistent findings.11 Results were considered consistent if over 75% of the studies reported similar results on the same outcome measure. It was judged to be moderate when multiple low-quality trials or one high-quality and 1 or more low-quality trials produced generally consistent findings. Evidence was considered to be limited when only 1 low-quality RCT existed and conflicting when the findings of existing trials were inconsistent. We arbitrarily regarded trials with methodological quality scores of 6 or more as of high quality.11
Relation between funding source of the RCTs and conclusions
We extracted the sources of funding of the RCTs from the text, statements of sources of support, authors’ affiliations, and acknowledgements. Funding sources were classified as nonprofit organizations, not reported, both nonprofit and for-profit organizations, or for-profit organizations.12 For-profit organizations were defined as companies that might acquire financial gain or loss depending on the outcome of the trial.12 Funding included provision of grants, study material (drug, placebo), or manpower (authorship, statistical analysis, or other assistance).12 We used the effect sizes between medication(s) and placebo to evaluate whether funding source affected outcome.
Results
Search results
A total of 1878 publications were identified by our search strategy. Finally, 41 RCTs met our inclusion criteria and 4 papers concerned double publications (FIGURE 1),13-16 leaving a total of 41 trials which were included in this review. Thirteen of these RCTs used a crossover design.15,7-27
FIGURE 1
How the 41 trials made our cut for the review
Description of studies
Full details of the included studies are presented in TABLE W1. The number of participants included in each trial ranged from 12 to 900 (mean=252.7 patients), with a total of 10,363 patients included. The mean percentage of participants who dropped out from the trials was 15.2% (range=0%–61.9%). Age of participants (for studies reporting this information) ranged from 18 to 87 years. Overall, the percentage of women was generally higher than men (mean=69.3%; range=36%–97%). Fifteen trials used the criteria of the International Headache Society to classify TTH,14,17,19-21,24,28-36 12 trials used the Ad Hoc Committee’s criteria,13,23,26,37,45 while the remaining studies did not use a formal classification.
Twenty-five studies compared 1 or more types of NSAIDs with placebo,13-17,22-24,26-36,38,41-43,45-47 17 studies compared 1 or more doses of acetaminophen with placebo,17-21,25,30-34,41,44-46,48,49 7 studies compared different types of NSAIDs,15,26,28,29,35-37 9 studies compared 1 or more types of NSAIDs with acetaminophen,17,30-34,41,45,46 and 13 studies compared other analgesics with placebo.15,18,25,27,39,40,44,49,50-53
The quality score (with positive items in parenthesis) is presented in the “Notes” section of TABLE W1. The interobserver reliability of the methodological quality assessment was high (κ=0.85). There was disagreement between the 2 authors in 7.5% of the criteria, but after consensus no disagreement persisted. The median quality score was 5 (range 1–9). Using a cutoff point of 6 out of 10 criteria, 15 studies (36.6%) were considered to be of high quality.15,17,19,21,22,24,25,28-30,32-34,36
Only 1 study reported a concealed randomization method.34 Other methodological flaws, which often scored “negative” or “unclear,” were blinding of the care provider (unclear 88%) and an intention-to-treat analysis (unclear 30% and negative 60%).
Effectiveness of analgesics
TABLE 1 gives the quantitative analysis for high-quality studies, low-quality studies, and for all studies for the different comparisons of NSAIDs, acetaminophen, and placebo.
TABLE 1
Quantitative analysis for the different studies for the comparisons of NSAIDs, acetaminophen and placebo
| HIGH-QUALITY TRIALS | LOW-QUALITY TRIALS | ALL TRIALS | |||||
|---|---|---|---|---|---|---|---|
| N/n | RR (95% CI) | N/n | RR (95% CI) | N/n | RR (95% CI) | ||
| 1. NSAIDs vs placebo | 7/13 | 1.5 (1.3–1.8)* | 8/15 | 2.0 (1.4–2.7)* | 15/28 | 1.6 (1.4–2.0)* | |
| 2. Acetaminophen vs placebo | 5/6 | 1.4 (1.04–1.8)* | 3/3 | 1.6 (0.9–2.7) | 8/9 | 1.4 (1.1–1.8)* | |
| 500 mg vs placebo | 1/1 | 1.1 (0.8–1.5) | 1/1 | 1.1 (0.8–1.5) | |||
| 1000 mg vs placebo | 4/5 | 1.4 (0.97–2.0) | 3/3 | 1.6 (0.9–2.7) | 7/8 | 1.5 (1.1–2.0)8 | |
| 4. NSAIDs vs acetaminophen | 5/7 | 1.1 (0.96–1.4) | 2/2 | 2.2 (1.4–3.4)* | 7/9 | 1.3 (1.04–1.5)* | |
| 3. NSAIDs vs NSAIDs | |||||||
| Ibuprofen 400/800 mg vs aspirin 650 mg37 | 1/2 | 1.2 (0.6–2.2) | |||||
| Ketoprofen 12.5/25/50 mg vs ibuprofen 200 mg29,36 | 1/2 | 1.1 (0.8–1.5) | 1/2 | 1.5 (0.8–2.7) | 2/4 | 1.2 (0.9–1.6) | |
| Ketoprofen 12.5/25 mg vs naproxen 275 mg29 | 1/2 | 0.96 (0.7–1.3) | |||||
| Naproxen 275 mg vs ibuprofen 200 mg29 | 1/1 | 0.9 (0.7–1.2) | |||||
| Metamizol 500/1000 mg vs aspirin 1000 mg30 | 1/2 | 1.2 (0.9–1.7) | |||||
| Diclofenac 12.5/25 mg vs ibuprofen 400 mg55 | 1/2 | 1.1 (0.8–1.5) | |||||
| N/n=number of trials/total number of comparisons; RR: relative risk; CI: confidence interval. *P<.05. | |||||||
1. NSAIDs vs placebo
Twenty-five studies compared one or more types of NSAIDs with placebo, of which 10 are of high quality.15,17,22,24,29,30,32-34,36,45
Quantitative analysis. Sufficient data were available in 15 studies,13,14,29-38,41,45,47 of which 6 were of high quality.29,30,32-34,36,45 Because some trials included 3 or more treatment groups, data were available for 28 comparisons. We found a significant effect in favor of NSAIDs compared with placebo on short-term pain relief (see TABLE 1 and FIGURE W1).
Qualitative analysis. The 10 high-quality studies reported 30 comparisons, of which in 26 (86.6%) NSAIDs were significantly more effective compared with placebo for short-term pain relief (strong evidence).
Adverse events. Twenty studies reported during a 2 to 6 hours treatment period data on adverse events. For the NSAID group (n=2061) frequently mentioned side effects were nausea (4.6%), photophobia (3.1%), vomiting (2.7%), phonophobia (1.7%), aching limbs (1.2%), dizziness (1.1%), and drowsiness (1.0%). For the placebo group (n=1323), these were nausea (7.0%), photophobia (4.8%), vomiting (3.9%), phonophobia (3.4%), aching limbs (2.0%), drowsiness (1.7%), and dizziness (1.0%). The pooled RR for the number of patients reporting side effects for 14 studies with sufficient data was 0.96 (95% CI, 0.7–1.3), indicating no significant difference.
2. Acetaminophen vs placebo
Seventeen studies compared 1 or more doses of acetaminophen with placebo; 9 were high-quality studies.17,19,21,25,30-34,45
Quantitative analysis. The pooled analysis of 5 high-quality trials30,32-34,45 and 3 low-quality trials31,41,44 showed that acetaminophen was significantly more effective compared with placebo for patients on short-term pain relief (TABLE 1 and FIGURE W2). This result was due to the studies comparing acetaminophen with placebo. The only high-quality trial34 with acetaminophen 500 mg failed to show a difference in short-term pain relief compared with placebo (TABLE 1).
Qualitative analysis. The 9 high-quality studies reported 16 comparisons, of which 10 (62.5%) mentioned that acetaminophen showed significantly more pain relief than placebo (conflicting evidence). In 2 high-quality studies,17,34 we found no significant differences between acetaminophen 500 mg and placebo (strong evidence), but in the 9 high-quality studies, in 10 out of 14 comparisons (71.4%) acetaminophen 1000 mg showed significantly more pain relief compared with placebo (conflicting evidence).
Adverse events. Twelve studies reported data on adverse events. For the acetaminophen group (n=3715), frequently mentioned side effects were stomach discomfort (3.9%), dizziness (1.6%), nervousness (0.7%), nausea (0.4%), and drowsiness (0.3%). For the placebo group (n=3700), these were stomach discomfort (3.7%), nervousness (0.7%), nausea (0.6%), dizziness (0.5%), and drowsiness (0.3%). The pooled RR for the number of patients reporting side effects was 1.3 (95% CI, 0.9–1.7), indicating no significant difference.
3. NSAIDs vs acetaminophen
Nine studies compared 1 or more types of NSAIDs with acetaminophen, of which 6 are of high-quality.17,30-34,45
Quantitative analysis. The pooled analysis of 5 high-quality studies30-34,45 and 2 low-quality studies31,41 showed a significant difference in short-term pain relief in favor of NSAIDs (TABLE 1).
Qualitative analysis. Six high-quality studies showed that in 9 out of 13 comparisons (69%) NSAIDs were not significantly more effective than acetaminophen for short-term pain relief in patients with acute episodes of TTH (conflicting evidence).
Adverse events. Seven studies reported data on adverse events. The pooled RR for number of patients reporting side effects was 1.3 (95% CI, 0.97–1.6), indicating no significant difference.
4. Comparison between different NSAIDs
Seven studies compared different types of NSAIDs,15,26,28,29,35-37 of which 4 provided data.
Quantitative and qualitative analysis. The analysis the between different types of NSAIDs no differences in short-term pain relief can be found; RR vary between 0.9 and 1.5 (TABLE 1).
Adverse events. The adverse effects were reported involving the central nervous system (ie, dizziness, drowsiness, vertigo), gastrointestinal system (ie, nausea, vomiting, gastrointestinal upset or discomfort), and the body as a whole (ie, light-headed, fatigue, cramps, asthenia, chills).
Naproxen and zomepirac gave more adverse events involving the central nervous system than aspirin, ibuprofen, and ketoprofen. Naproxen and zomepirac were also more often associated with gastrointestinal side effects than ibuprofen and ketoprofen.
Furthermore, aspirin was more associated with gastrointestinal complaints than ibuprofen. Side effects such as fatigue and cramps (body as whole) occurred significantly more often with ketoprofen compared with aspirin and ibuprofen, naproxen compared with ketoprofen, and zomepirac compared with aspirin.
5. Other analgesics vs placebo
Qualitative analysis. There is insufficient evidence to either support or refute the effectiveness of all other analgesics compared with placebo, due to the fact that most analgesics were a unique combination of analgesics with caffeine or peppermint oil. Also, the low methodological quality of nearly all these studies and the low number of studies per comparison made drawing conclusions difficult.
Optalidon and Tonopan were compared with placebo in 3 substudies of 1 high-quality study, and we found significant more pain relief using these analgesics than placebo.15 No adverse events were stated in these studies.
The combination of acetaminophen and caffeine was compared with placebo in 2 studies of high quality25,49 showed that the combination of acetaminophen with caffeine is more effective than placebo (moderate evidence).
The combination of acetaminophen, aspirin, and caffeine was compared with placebo in 4 substudies of the same high-quality study.25 Data from these studies suggest that this combination is significantly more effective than placebo. All groups reported low numbers of side effects as stomach discomfort, nervousness, and dizziness.
Relation between funding source and effect estimates
The pooled effect estimates in placebo-controlled trials stratified by funding are shown in TABLE 2. No major differences in effect sizes were found between the different funding sources.
TABLE 2
Relation between funding source and effect estimate, intervention vs placebo only
| NUMBER OF COMPARISONS (TRIALS) | NUMBER OF COMPARISONS IN HIGH QUALITY STUDIES (TRIALS) | EFFECT ESTIMATE ALLSTUDIES: RR (95% CI) | EFFECT ESTIMATE HIGH QUALITY STUDIES: RR (95% CI) | |
|---|---|---|---|---|
| Non-profit organizations | 0 | 0 | — | — |
| Not reported | 4 (2) | 0 | 1.4 (0.8–2.6) | — |
| Non-profit and for-profit organizations | 26 (11) | 11 (4) | 1.7 (1.4–2.1) | 1.4 (1.1–1.7) |
| For-profit organizations | 14 (7) | 8 (3) | 1.4 (1.2–1.6) | 1.2 (1.06–1.4) |
| All studies | 44 (20) | 19 (7) | 1.5 (1.3–1.8) | 1.4 (1.1–1.7) |
| *P=.006 using χ2 test | ||||
Methodological quality of included studies
This review shows that many RCTs on the efficacy of analgesics in TTH have methodological shortcomings. Using a cut-off point of 6 out of 10 criteria, only 35% of the included studies were found to be of high quality. Most authors failed to explicitly specify the method of treatment allocation and blinding procedure. In many studies authors stated that the trial had a double-blind procedure, however, when the blinding procedure was not explicitly reported (ie, identical looking tablets) we did not score 1 or more blinding items positive. These flaws can be prevented in future trials.
We are unaware of any prior systematic reviews or meta-analyses that have assessed the efficacy and tolerability of analgesics in the treatment of acute episodes of tension-type headache in adults. We conducted the review according to the high Cochrane standard, resulting in a review of high validity. Our review succeeded in identifying a large number of only randomized trials. Also the methodological quality did not explain the possible association between funding and effect estimates.
Although systematic reviews offer the least biased method of summarizing research literature, our review should be considered with the following limitations in mind. First, we decided not to contact the authors for additional information, because most trials were published before 1995. Second, some of the medications have only been evaluated in 1 or 2 studies, which may limit the generalizability of the findings. We do not think these factors have influences our conclusions.
CORRESPONDENCE
Arianne P. Verhagen, PhD, Department of General Practice, Erasmus Medical Centre, PO Box 1738, 3000 DR Rotterdam, The Netherlands. E-mail: [email protected]
- Though all non-narcotic analgesics have equivalent efficacy against tension-type headache, ibuprofen’s generally favorable side-effect profile makes it a reasonable first choice.
Whereas quantitative and qualitative analyses of 41 randomized controlled trials (RCTs) strongly suggests that all types of NSAIDs are more effective than placebo (>50% pain relief) against an acute episode of tension-type headache (TTH), the evidence also shows that no single nonsteroidal anti-inflammatory drug (NSAID) is more effective than another in this setting.
How, then, to choose an NSAID? Many of the 41 articles we reviewed reported on the side effects of NSAIDs. No clear differences were reported in the number of side effects between the NSAIDs and placebo. However, differences were found among the types of NSAIDs. Our results agree with those found by Henry et al,1 who concluded from their meta-analysis that ibuprofen, compared with other NSAIDs, had the lowest relative risk of serious gastrointestinal complications. Given the lack of important differences in efficacy among NSAIDs for relieving an acute episode of TTH, using the most effective dose of a drug that is well tolerated by a patient is a reasonable basis for selection. Ibuprofen, therefore, generally may be advocated.
When acetaminophen is preferred. Our results suggest NSAIDs might be more effective than acetaminophen for TTH. However, because NSAIDs are allergenic for some people, and they must not be used in association with anticoagulants,2 acetaminophen might be an alternative in these situations. When giving acetaminophen, the dose of the medication might be important due to a possible dose-response relationship.
Why this review was needed
Tension-type headache, also known as tension headache or muscle contraction headache, is the most commonly experienced type of headache (see Episodic tension-type headache). Population-based studies suggest prevalence rates of 35% to 40% in adults.3-5
Persons experiencing an acute episode of TTH most often self-treat with mild, non-narcotic analgesics for initial pain relief. Studies have suggested that acetaminophen and NSAIDs like aspirin, ibuprofen, naproxen, and ketoprofen are effective in reducing headache symptoms. But a variety of drugs, dosages, and combinations have been described. No systematic review has, until now, described the efficacy and tolerability of analgesics for the treatment of acute episodes of TTH. Good quality-controlled trials and a systematic review form the basis for evidence-based treatment guidelines, which provide a basis for the individual patient.
Episodic TTH has been defined in the classification of the International Headache Society (IHS) as headache frequency of greater than 10 lifetime episodes, but fewer than 15 episodes per month; an average episode duration of 30 minutes to 7 days; and with at least 2 quality of pain features (ie, mild or moderate pain intensity, bilateral, pressing or tightening [nonpulsating] feeling, and no exacerbation by exercise).7 In addition, the headache does not have the IHS-defining features of migraine (ie, nausea, vomiting, or photophobia and phonophobia). The definition of chronic TTH is identical to those for episodic TTH, except that the episode frequency is 15 or more episodes per month for at least 6 months, and 1 associated symptom of nausea, photophobia, or phonophobia is permitted.
We aimed to describe and assess the data from RCTs concerning the efficacy and tolerability of analgesics for the treatment of acute episodes of TTH in adult patients. Details of our Methods and Results follow.
Methods
Search strategy
Medline and EMBASE were searched from inception to January 2005 using the terms tension-type headache, tension headache, stress headache, or muscle contraction headache together with the search strategy for identifying RCTs described by Robinson and Dickerson.6 The Cochrane Controlled Trials Register was searched using the words tension headache or tension-type headache or muscle contraction headache. Additional strategies for identifying trials included searching the reference lists of review articles and included studies.
Study selection
Only RCTs including analgesic medicine used in the treatment or management of TTH conducted among adult patients (aged 18 years or older), with reasonable criteria designed to distinguish TTH from migraine, were selected for our review. The use of a specific set of diagnostic criteria (eg, IHS 1988 and Ad Hoc 1962)7,8 was not required, but TTH diagnoses had to be based on at least some of the distinctive features of TTH—eg, bilateral in location, no nausea or vomiting, mild or moderate intensity, or no exacerbation by exercise.
Main outcome measures were pain relief or recovery over 2 to 6 hours.
Two authors (LD, AV) independently screened titles and abstracts of identified studies for eligibility. All potentially relevant studies were retrieved as full papers and then again independently reviewed by 2 authors (LD, AV). Disagreements were resolved through consensus where possible, or by arbitration with a third author (MB). Crossover designs often presented data from treatment groups, as if the trial was a parallel group trial. The results from these studies were excluded from data-analysis if no results from both arms were presented or a binary correlation coefficient was available.9
Methodological quality and data extraction
Two authors (LD with MB, BK, or AV) independently rated the methodological quality of the included trials using the Delphi list.10 The Delphi list is a generic criteria list developed by international consensus and consists of the following 9 items: 1) randomization; 2) adequate allocation concealment; 3) groups similar at baseline; 4) specification of eligibility criteria; 5) blinding of outcome assessor; 6) blinding of care provider; 7) blinding of patient; 8) presentation of point estimates and measures of variability; 9) intention-to-treat-analysis. One extra item was added: 10) withdrawal or dropout rate unlikely to cause bias. All selected methodological criteria were scored as yes (=1), no (=0) or don’t know (=0). A quality score of a trial was computed by counting the number of positive scores, with equal weights applied on all items. In case of a disagreement between the 2 authors, consensus was used to resolve disagreement. When consensus could not be reached, a third author made the final decision (MB or AV).
Extraction of data from the original reports was performed by 1 author (LD) and checked by a second (AV). Disagreements were resolved by consensus. Extracted information included (if available) demographic data, detailed description of the intervention and control (ie, dose given, study duration, rescue medication), data on pain relief or recovery, and information on adverse effects measured during a treatment period of 2 to 6 hours. When a trial protocol permitted the use of rescue medication prior to the outcome time (2 to 6 hours), then the latest outcome assessment not confounded by the use of rescue medication was extracted
Data analysis
A quantitative analysis was limited to clinically homogenous studies for which the study populations, interventions and outcomes were considered to be similar. For each study, the number of patients who were recovered (often defined as more than 50% pain relief) was used to calculate relative risk (RR) with 95% confidence interval (CI). RRs and 95% CI were presented using the random effects model. Data are presented as treatment success, indicating that an RR >1 represents a better outcome for the first mentioned medication group.
In parallel studies, when more than 1 comparison from the same study (ie, aspirin 650 mg vs placebo and ibuprofen 400 mg vs placebo) was used for the statistical pooling of NSAIDs vs placebo, the results from the placebo group were evenly spread out over the 2 comparisons and the number of patients in the placebo group was divided by 2 in order to prevent double counting (personal communication RJPM Scholten, Dutch Cochrane Centre).
Because only a subset of available trials provides sufficient data for inclusion in the quantitative analysis, also a qualitative analysis was performed. We summarized findings by strength of evidence, nature of intervention and control treatments. The evidence was judged to be strong when multiple high-quality trials produced generally consistent findings.11 Results were considered consistent if over 75% of the studies reported similar results on the same outcome measure. It was judged to be moderate when multiple low-quality trials or one high-quality and 1 or more low-quality trials produced generally consistent findings. Evidence was considered to be limited when only 1 low-quality RCT existed and conflicting when the findings of existing trials were inconsistent. We arbitrarily regarded trials with methodological quality scores of 6 or more as of high quality.11
Relation between funding source of the RCTs and conclusions
We extracted the sources of funding of the RCTs from the text, statements of sources of support, authors’ affiliations, and acknowledgements. Funding sources were classified as nonprofit organizations, not reported, both nonprofit and for-profit organizations, or for-profit organizations.12 For-profit organizations were defined as companies that might acquire financial gain or loss depending on the outcome of the trial.12 Funding included provision of grants, study material (drug, placebo), or manpower (authorship, statistical analysis, or other assistance).12 We used the effect sizes between medication(s) and placebo to evaluate whether funding source affected outcome.
Results
Search results
A total of 1878 publications were identified by our search strategy. Finally, 41 RCTs met our inclusion criteria and 4 papers concerned double publications (FIGURE 1),13-16 leaving a total of 41 trials which were included in this review. Thirteen of these RCTs used a crossover design.15,7-27
FIGURE 1
How the 41 trials made our cut for the review
Description of studies
Full details of the included studies are presented in TABLE W1. The number of participants included in each trial ranged from 12 to 900 (mean=252.7 patients), with a total of 10,363 patients included. The mean percentage of participants who dropped out from the trials was 15.2% (range=0%–61.9%). Age of participants (for studies reporting this information) ranged from 18 to 87 years. Overall, the percentage of women was generally higher than men (mean=69.3%; range=36%–97%). Fifteen trials used the criteria of the International Headache Society to classify TTH,14,17,19-21,24,28-36 12 trials used the Ad Hoc Committee’s criteria,13,23,26,37,45 while the remaining studies did not use a formal classification.
Twenty-five studies compared 1 or more types of NSAIDs with placebo,13-17,22-24,26-36,38,41-43,45-47 17 studies compared 1 or more doses of acetaminophen with placebo,17-21,25,30-34,41,44-46,48,49 7 studies compared different types of NSAIDs,15,26,28,29,35-37 9 studies compared 1 or more types of NSAIDs with acetaminophen,17,30-34,41,45,46 and 13 studies compared other analgesics with placebo.15,18,25,27,39,40,44,49,50-53
The quality score (with positive items in parenthesis) is presented in the “Notes” section of TABLE W1. The interobserver reliability of the methodological quality assessment was high (κ=0.85). There was disagreement between the 2 authors in 7.5% of the criteria, but after consensus no disagreement persisted. The median quality score was 5 (range 1–9). Using a cutoff point of 6 out of 10 criteria, 15 studies (36.6%) were considered to be of high quality.15,17,19,21,22,24,25,28-30,32-34,36
Only 1 study reported a concealed randomization method.34 Other methodological flaws, which often scored “negative” or “unclear,” were blinding of the care provider (unclear 88%) and an intention-to-treat analysis (unclear 30% and negative 60%).
Effectiveness of analgesics
TABLE 1 gives the quantitative analysis for high-quality studies, low-quality studies, and for all studies for the different comparisons of NSAIDs, acetaminophen, and placebo.
TABLE 1
Quantitative analysis for the different studies for the comparisons of NSAIDs, acetaminophen and placebo
| HIGH-QUALITY TRIALS | LOW-QUALITY TRIALS | ALL TRIALS | |||||
|---|---|---|---|---|---|---|---|
| N/n | RR (95% CI) | N/n | RR (95% CI) | N/n | RR (95% CI) | ||
| 1. NSAIDs vs placebo | 7/13 | 1.5 (1.3–1.8)* | 8/15 | 2.0 (1.4–2.7)* | 15/28 | 1.6 (1.4–2.0)* | |
| 2. Acetaminophen vs placebo | 5/6 | 1.4 (1.04–1.8)* | 3/3 | 1.6 (0.9–2.7) | 8/9 | 1.4 (1.1–1.8)* | |
| 500 mg vs placebo | 1/1 | 1.1 (0.8–1.5) | 1/1 | 1.1 (0.8–1.5) | |||
| 1000 mg vs placebo | 4/5 | 1.4 (0.97–2.0) | 3/3 | 1.6 (0.9–2.7) | 7/8 | 1.5 (1.1–2.0)8 | |
| 4. NSAIDs vs acetaminophen | 5/7 | 1.1 (0.96–1.4) | 2/2 | 2.2 (1.4–3.4)* | 7/9 | 1.3 (1.04–1.5)* | |
| 3. NSAIDs vs NSAIDs | |||||||
| Ibuprofen 400/800 mg vs aspirin 650 mg37 | 1/2 | 1.2 (0.6–2.2) | |||||
| Ketoprofen 12.5/25/50 mg vs ibuprofen 200 mg29,36 | 1/2 | 1.1 (0.8–1.5) | 1/2 | 1.5 (0.8–2.7) | 2/4 | 1.2 (0.9–1.6) | |
| Ketoprofen 12.5/25 mg vs naproxen 275 mg29 | 1/2 | 0.96 (0.7–1.3) | |||||
| Naproxen 275 mg vs ibuprofen 200 mg29 | 1/1 | 0.9 (0.7–1.2) | |||||
| Metamizol 500/1000 mg vs aspirin 1000 mg30 | 1/2 | 1.2 (0.9–1.7) | |||||
| Diclofenac 12.5/25 mg vs ibuprofen 400 mg55 | 1/2 | 1.1 (0.8–1.5) | |||||
| N/n=number of trials/total number of comparisons; RR: relative risk; CI: confidence interval. *P<.05. | |||||||
1. NSAIDs vs placebo
Twenty-five studies compared one or more types of NSAIDs with placebo, of which 10 are of high quality.15,17,22,24,29,30,32-34,36,45
Quantitative analysis. Sufficient data were available in 15 studies,13,14,29-38,41,45,47 of which 6 were of high quality.29,30,32-34,36,45 Because some trials included 3 or more treatment groups, data were available for 28 comparisons. We found a significant effect in favor of NSAIDs compared with placebo on short-term pain relief (see TABLE 1 and FIGURE W1).
Qualitative analysis. The 10 high-quality studies reported 30 comparisons, of which in 26 (86.6%) NSAIDs were significantly more effective compared with placebo for short-term pain relief (strong evidence).
Adverse events. Twenty studies reported during a 2 to 6 hours treatment period data on adverse events. For the NSAID group (n=2061) frequently mentioned side effects were nausea (4.6%), photophobia (3.1%), vomiting (2.7%), phonophobia (1.7%), aching limbs (1.2%), dizziness (1.1%), and drowsiness (1.0%). For the placebo group (n=1323), these were nausea (7.0%), photophobia (4.8%), vomiting (3.9%), phonophobia (3.4%), aching limbs (2.0%), drowsiness (1.7%), and dizziness (1.0%). The pooled RR for the number of patients reporting side effects for 14 studies with sufficient data was 0.96 (95% CI, 0.7–1.3), indicating no significant difference.
2. Acetaminophen vs placebo
Seventeen studies compared 1 or more doses of acetaminophen with placebo; 9 were high-quality studies.17,19,21,25,30-34,45
Quantitative analysis. The pooled analysis of 5 high-quality trials30,32-34,45 and 3 low-quality trials31,41,44 showed that acetaminophen was significantly more effective compared with placebo for patients on short-term pain relief (TABLE 1 and FIGURE W2). This result was due to the studies comparing acetaminophen with placebo. The only high-quality trial34 with acetaminophen 500 mg failed to show a difference in short-term pain relief compared with placebo (TABLE 1).
Qualitative analysis. The 9 high-quality studies reported 16 comparisons, of which 10 (62.5%) mentioned that acetaminophen showed significantly more pain relief than placebo (conflicting evidence). In 2 high-quality studies,17,34 we found no significant differences between acetaminophen 500 mg and placebo (strong evidence), but in the 9 high-quality studies, in 10 out of 14 comparisons (71.4%) acetaminophen 1000 mg showed significantly more pain relief compared with placebo (conflicting evidence).
Adverse events. Twelve studies reported data on adverse events. For the acetaminophen group (n=3715), frequently mentioned side effects were stomach discomfort (3.9%), dizziness (1.6%), nervousness (0.7%), nausea (0.4%), and drowsiness (0.3%). For the placebo group (n=3700), these were stomach discomfort (3.7%), nervousness (0.7%), nausea (0.6%), dizziness (0.5%), and drowsiness (0.3%). The pooled RR for the number of patients reporting side effects was 1.3 (95% CI, 0.9–1.7), indicating no significant difference.
3. NSAIDs vs acetaminophen
Nine studies compared 1 or more types of NSAIDs with acetaminophen, of which 6 are of high-quality.17,30-34,45
Quantitative analysis. The pooled analysis of 5 high-quality studies30-34,45 and 2 low-quality studies31,41 showed a significant difference in short-term pain relief in favor of NSAIDs (TABLE 1).
Qualitative analysis. Six high-quality studies showed that in 9 out of 13 comparisons (69%) NSAIDs were not significantly more effective than acetaminophen for short-term pain relief in patients with acute episodes of TTH (conflicting evidence).
Adverse events. Seven studies reported data on adverse events. The pooled RR for number of patients reporting side effects was 1.3 (95% CI, 0.97–1.6), indicating no significant difference.
4. Comparison between different NSAIDs
Seven studies compared different types of NSAIDs,15,26,28,29,35-37 of which 4 provided data.
Quantitative and qualitative analysis. The analysis the between different types of NSAIDs no differences in short-term pain relief can be found; RR vary between 0.9 and 1.5 (TABLE 1).
Adverse events. The adverse effects were reported involving the central nervous system (ie, dizziness, drowsiness, vertigo), gastrointestinal system (ie, nausea, vomiting, gastrointestinal upset or discomfort), and the body as a whole (ie, light-headed, fatigue, cramps, asthenia, chills).
Naproxen and zomepirac gave more adverse events involving the central nervous system than aspirin, ibuprofen, and ketoprofen. Naproxen and zomepirac were also more often associated with gastrointestinal side effects than ibuprofen and ketoprofen.
Furthermore, aspirin was more associated with gastrointestinal complaints than ibuprofen. Side effects such as fatigue and cramps (body as whole) occurred significantly more often with ketoprofen compared with aspirin and ibuprofen, naproxen compared with ketoprofen, and zomepirac compared with aspirin.
5. Other analgesics vs placebo
Qualitative analysis. There is insufficient evidence to either support or refute the effectiveness of all other analgesics compared with placebo, due to the fact that most analgesics were a unique combination of analgesics with caffeine or peppermint oil. Also, the low methodological quality of nearly all these studies and the low number of studies per comparison made drawing conclusions difficult.
Optalidon and Tonopan were compared with placebo in 3 substudies of 1 high-quality study, and we found significant more pain relief using these analgesics than placebo.15 No adverse events were stated in these studies.
The combination of acetaminophen and caffeine was compared with placebo in 2 studies of high quality25,49 showed that the combination of acetaminophen with caffeine is more effective than placebo (moderate evidence).
The combination of acetaminophen, aspirin, and caffeine was compared with placebo in 4 substudies of the same high-quality study.25 Data from these studies suggest that this combination is significantly more effective than placebo. All groups reported low numbers of side effects as stomach discomfort, nervousness, and dizziness.
Relation between funding source and effect estimates
The pooled effect estimates in placebo-controlled trials stratified by funding are shown in TABLE 2. No major differences in effect sizes were found between the different funding sources.
TABLE 2
Relation between funding source and effect estimate, intervention vs placebo only
| NUMBER OF COMPARISONS (TRIALS) | NUMBER OF COMPARISONS IN HIGH QUALITY STUDIES (TRIALS) | EFFECT ESTIMATE ALLSTUDIES: RR (95% CI) | EFFECT ESTIMATE HIGH QUALITY STUDIES: RR (95% CI) | |
|---|---|---|---|---|
| Non-profit organizations | 0 | 0 | — | — |
| Not reported | 4 (2) | 0 | 1.4 (0.8–2.6) | — |
| Non-profit and for-profit organizations | 26 (11) | 11 (4) | 1.7 (1.4–2.1) | 1.4 (1.1–1.7) |
| For-profit organizations | 14 (7) | 8 (3) | 1.4 (1.2–1.6) | 1.2 (1.06–1.4) |
| All studies | 44 (20) | 19 (7) | 1.5 (1.3–1.8) | 1.4 (1.1–1.7) |
| *P=.006 using χ2 test | ||||
Methodological quality of included studies
This review shows that many RCTs on the efficacy of analgesics in TTH have methodological shortcomings. Using a cut-off point of 6 out of 10 criteria, only 35% of the included studies were found to be of high quality. Most authors failed to explicitly specify the method of treatment allocation and blinding procedure. In many studies authors stated that the trial had a double-blind procedure, however, when the blinding procedure was not explicitly reported (ie, identical looking tablets) we did not score 1 or more blinding items positive. These flaws can be prevented in future trials.
We are unaware of any prior systematic reviews or meta-analyses that have assessed the efficacy and tolerability of analgesics in the treatment of acute episodes of tension-type headache in adults. We conducted the review according to the high Cochrane standard, resulting in a review of high validity. Our review succeeded in identifying a large number of only randomized trials. Also the methodological quality did not explain the possible association between funding and effect estimates.
Although systematic reviews offer the least biased method of summarizing research literature, our review should be considered with the following limitations in mind. First, we decided not to contact the authors for additional information, because most trials were published before 1995. Second, some of the medications have only been evaluated in 1 or 2 studies, which may limit the generalizability of the findings. We do not think these factors have influences our conclusions.
CORRESPONDENCE
Arianne P. Verhagen, PhD, Department of General Practice, Erasmus Medical Centre, PO Box 1738, 3000 DR Rotterdam, The Netherlands. E-mail: [email protected]
1. Henry D, Lim LLY, Garcia Rodriguez LA, et al. Variability in risk of gastrointestinal complications with individual nonsteroidal anti-inflammatory drugs: results of a collaborative meta-analysis. BMJ 1996;312:1563-1566.
2. D’Amico D, Grazzi L, Leone M, Moschiano F, Bussone G. A review of the treatment of primary headaches. Part II: Tension-type headache. Ital J Neurol Sci 1998;19:2-9.
3. Schwartz BS, Stewart WF, Simon D, Lipton RB. Epidemiology of tension-type headache. JAMA 1998;279:381-383.
4. Rasmussen BK. Epidemiology of headache. Cephalalgia 1995;15:45-68.
5. Pryse-Philips W, Findlay H, Tugwell P, Edmeads J, Murray TJ, Nelson RF. Canadian population survey on the clinical, epidemiologic and societal impact of migraine and tension-type headache. Can J Neurol Sci 1992;19:333-339.
6. Robinson KA, Dickerson K. Development of a highly sensitive search strategy for the retrieval of reports of controlled trials using PubMed. Int J Epidemiol 2002;31:150-153.
7. Headache Classification Committee of the International Headache Society. Classification and diagnostic criteria for headache disorders, cranial neuralgias and facial pain. Cephalalgia 1988;8(Suppl 7):1-96;Headache Classification Committee of the International Headache Society. The International Classification of headache disorders.Cephalalgia 2004; 24(Suppl 1): 1-152.
8. Ad Hoc Committee on the Classification of Headache of the National Institute of Neurological Diseases and Blindness. Classification of headache. JAMA 1962;179:717-718.
9. Elbourne DR, Altman DG, Higgins JP, Curtin F, Worthington HV, Vail A. Meta-analyses involving crossover trials: methodological issues. Int J Epidemiol 2002;31:140-149.
10. Verhagen AP, de Vet HCW, de Bie RA, et al. The art of quality assessment of RCTs included in systematic reviews. J Clin Epidemiol 2001;54:651-654.
11. Van Tulder MW, Furlan A, Bombarbier C, Bouter L. Editorial Board of the Cochrane Collabaration Back Review Group. Updated method guidelines for systematic reviews in the Cochrane Collaboration Back review Group. Spine 2003;28:1290-1299.
12. Als-Nielsen B, Chen W, Gluud C, Kjaergard LL. Association of funding and conclusions in randomized drug trials. A reflection of treatment effect or adverse events? JAMA 2003;290:921-928.
13. Diamond S. Zomepirac in the symptomatic treatment of muscle contraction headache. J Clin Pharmacol 1980;20:298-302;Diamond S, Medina JL. A double-blind study of zomepirac sodium and placebo in the treatment of muscle contraction headache. Headache 1981; 21:45-48.
14. Diamond S, Balm TK, Freitag FG. Ibuprofen plus caffeine in the treatment of tension-type headache. Clin Pharmacol Ther 2000;68:312-319;Diamond S, Freitag FG. The use of ibuprofen plus caffeine to treat tension-type headache. Curr Pain Headache Rep 2001; 5:472-478.
15. von Graffenried B, Hill RC, Nüesch E. Headache as a model for assessing mild analgesic drugs. J Clin Pharmacol 1980;20:131-144;von Graffenried B, Nüesch B. Non-migrainous headache for the evaluation of oral analgesics. Br J Clin Pharmacol 1980; 10(suppl2):225S-231S.
16. Friedman AP, Boyles WF, Elkind AH, et al. Fiorinal with codeine in the treatment of tension headache-the contribution of components to the combination drug. Clin Ther 1988;10:303-315;Hwang DS, Mietlowski MJ, Friedman AP. Fiorinal with Codeine in the management of tension headache: impact of placebo response. Clin Ther 1987; 9:201-222.
17. Dahlöf CG, Jacobs LD. Ketoprofen, paracetamol and placebo in the treatment of episodic tension-type headache. Cephalalgia 1996;16:117-123.
18. Gilbert MM, De Sola Pool N, Schecter C. Analgesic/calmative effects of acetaminophen and phenyltoloxamine in treatment of simple nervous tension accompanied by headache. Curr Ther Res Clin Exp 1976;20:53-58.
19. Göbel H, Fresenius J, Heinze A, Dworschak M, Soyka D. Effectiveness of peppermint oil and paracetamol in the treatment of tension headache [German]. Nervenarzt 1996;67:672-681.
20. Göbel H, Heinze A, Lurch A, Dworschak M. Essential oils in the therapy of tension headache [German]. Z Allg Med 1998;74:223-228.
21. Göbel H, Heinze A, Dworschak M, Heinze-Kuhn Stolze H. Analgesic efficacy and tolerability of locally applied oleum menthae piperitae preparation LI 170 in patients with migraine or tension-type headache [German]. Z Allg Med 2001;77:287-295.
22. Guidotti M, Zanasi S, Garagiola U. Pirprofen in the treatment of migraine and episodic headache attacks: a placebo-controlled crossover clinical trial. J Int Med Res 1989;17:48-54.
23. Langemark M, Olesen J. Effervescent ASA versus solid ASA in the treatment of tension headache. A double-blind, placebo controlled study. Headache 1987;27:90-95.
24. Laveneziana D, Speranza R, Raulli P, Paredi G. Comparative efficacy of ibuprofen arginine and beta-cyclodextrin piroxicam as treatment for tension-type headache. Clin Drug Invest 1996;11(Suppl 1):22-26.
25. Migliardi JR, Armellino JJ, Friedman M, Gillings DB, Beaver WT. Caffeine as an analgesic adjuvant in tension headache. Clin Pharmacol Ther 1994;56:576-586.
26. Ryan RE, Sr. Motrin- A new agent for the symptomatic treatment of muscle contraction headache. Headache 1977;16:280-283.
27. Wood A, von Graffenried B. Fluproquazone: Analgesic activity in outpatients with non-migrainous headache. Arzneim-Forsch/Drug Res 1981;31:914-917.
28. Lange R, Lentz R. Comparison ketoprofen, ibuprofen and naproxen sodium in the treatment of tension-type headache. Drugs Exp Clin Res 1995;21:89-96.
29. Martinez-Martin P, Raffaelli E, Jr, Titus F, et al. Efficacy and safety of metamizol vs. acetylsalicylic acid in patients with moderate episodic tension-type headache: a randomized, double-blind, placebo- and active-controlled, multicentre study. Cephalalgia 2001;21:604-610.
30. Mehlisch DR, Weaver M, Fladung B. Ketoprofen, acetaminophen, and placebo in the treatment of tension headache. Headache 1998;38:579-589.
31. Packman B, Packman E, Doyle G, et al. Solubilized ibuprofen: evaluation of onset, relief, and safety of a novel formulation in the treatment of episodic tension-type headache. Headache 2000;40:561-567.
32. Prior MJ, Cooper KM, May LG, Bowen DL. Efficacy and safety of acetaminophen and naproxen in the treatment of tension-type headache. A randomized, double-blind, placebo-controlled trial. Cephalalgia 2002;22:740-748.
33. Steiner TJ, Lange R. Ketoprofen (25 mg) in the symptomatic treatment of episodic tension-type headache: double-blind placebo-controlled comparison with acetaminophen (1000 mg). Cephalalgia 1998;18:38-43.
34. Steiner T, Lange R, Voelker M. Aspirin in episodic tension-type headache: placebo-controlled dose-ranging comparison with paracetamol. Cephalalgia 2003;23:59-66.
35. van Gerven JM, Schoemaker RC, Jacobs LD, et al. Self-medication of a single headache episode with ketoprofen, ibuprofen or placebo, home-monitored with an electronic patient diary. Br J Clin Pharmacol 1996;42:475-481.
36. Kubitzek F, Ziegler G, Gold MS, Liu JMH, Ionescu E. Low-dose diclofenac potassium in the treatment of episodic tension-type headache. European J Pain 2003;7:155-162.
37. Diamond S. Ibuprofen versus aspirin and placebo in the treatment of muscle contraction headache. Headache 1983;23:206-210.
38. DiSerio FJ, Friedman AP, Parno J, Singer JM. Proquazone for tension headache-a multicenter trial. Headache 1985;25:127-133.
39. Friedman AP. Assessment of Fiorinal with Codeine in the treatment of tension headache. Clin Ther 1986;8:703-721.
40. Friedman AP, DiSerio FJ. Symptomatic treatment of chronically recurring tension headache: a placebo-controlled, multicenter investigation of Fioricet and acetaminophen with codeine. Clin Ther 1987;10:69-81.
41. Miller DS, Talbot CA, Simpson W, Korey A. A comparison of naproxen sodium, acetaminophen and placebo in the treatment of muscle contraction headache. Headache 1987;27:392-396.
42. Sargent JD, Peters K, Goldstein J, Madison DS, Solbach P. Naproxen sodium for muscle contraction headache treatment. Headache 1988;28:180-182.
43. Schachtel BP, Thoden WR. Onset of action of ibuprofen in the treatment of muscle-contraction headache. Headache 1988;28:471-474.
44. Schachtel BP, Thoden WR, Konerman JP, Brown A, Chaing DS. Headache pain model for assessing and comparing the efficacy of over-the-counter analgesic agents. Clin Pharmacol Ther 1991;50:322-329.
45. Schachtel BP, Furey SA, Thoden WR. Nonprescription ibuprofen and acetaminophen in the treatment of tension-type headache. J Clin Pharmacol 1996;36:1120-1125.
46. Peters BH, Fraim CJ, Masel BE. Comparison of 650 mg aspirin and 1,000 mg acetaminophen with each other, and with placebo in moderately severe headache. Am J Med 1983;74:36-42.
47. Ryan RE, Sr, Ryan RE, Jr. Symptomatic treatment of tension headache. Ear Nose Throat J 1979;58:423-426.
48. Schattner P, Randerson D. Tiger Balm as a treatment of tension headache. A clinical trial in general practice. Aust Fam Physician 1996;25:216, 218,220passim
49. Ward N, Whitney C, Avery D, Dunner D. The analgesic effects of caffeine in headache. Pain 1991;44:151-155.
50. Borges J, Zavaleta C. Study of a new analgesic compound in the treatment of tension headache. J Int Med Res 1976;4:74-78.
51. Thorpe P. Controlled and uncontrolled studies on “Fiorinal-PA” for symptomatic relief in tension headache. Med J Aust 1970;2:180-181.
52. Kagan G, Masheter HC. A controlled study of short-term treatment of tension headache. Curr Med Res Opin 1978;5:709-713.
53. Scheepers F. Syndol in the treatment of tension headache. Med Proc 1971;359-368.
1. Henry D, Lim LLY, Garcia Rodriguez LA, et al. Variability in risk of gastrointestinal complications with individual nonsteroidal anti-inflammatory drugs: results of a collaborative meta-analysis. BMJ 1996;312:1563-1566.
2. D’Amico D, Grazzi L, Leone M, Moschiano F, Bussone G. A review of the treatment of primary headaches. Part II: Tension-type headache. Ital J Neurol Sci 1998;19:2-9.
3. Schwartz BS, Stewart WF, Simon D, Lipton RB. Epidemiology of tension-type headache. JAMA 1998;279:381-383.
4. Rasmussen BK. Epidemiology of headache. Cephalalgia 1995;15:45-68.
5. Pryse-Philips W, Findlay H, Tugwell P, Edmeads J, Murray TJ, Nelson RF. Canadian population survey on the clinical, epidemiologic and societal impact of migraine and tension-type headache. Can J Neurol Sci 1992;19:333-339.
6. Robinson KA, Dickerson K. Development of a highly sensitive search strategy for the retrieval of reports of controlled trials using PubMed. Int J Epidemiol 2002;31:150-153.
7. Headache Classification Committee of the International Headache Society. Classification and diagnostic criteria for headache disorders, cranial neuralgias and facial pain. Cephalalgia 1988;8(Suppl 7):1-96;Headache Classification Committee of the International Headache Society. The International Classification of headache disorders.Cephalalgia 2004; 24(Suppl 1): 1-152.
8. Ad Hoc Committee on the Classification of Headache of the National Institute of Neurological Diseases and Blindness. Classification of headache. JAMA 1962;179:717-718.
9. Elbourne DR, Altman DG, Higgins JP, Curtin F, Worthington HV, Vail A. Meta-analyses involving crossover trials: methodological issues. Int J Epidemiol 2002;31:140-149.
10. Verhagen AP, de Vet HCW, de Bie RA, et al. The art of quality assessment of RCTs included in systematic reviews. J Clin Epidemiol 2001;54:651-654.
11. Van Tulder MW, Furlan A, Bombarbier C, Bouter L. Editorial Board of the Cochrane Collabaration Back Review Group. Updated method guidelines for systematic reviews in the Cochrane Collaboration Back review Group. Spine 2003;28:1290-1299.
12. Als-Nielsen B, Chen W, Gluud C, Kjaergard LL. Association of funding and conclusions in randomized drug trials. A reflection of treatment effect or adverse events? JAMA 2003;290:921-928.
13. Diamond S. Zomepirac in the symptomatic treatment of muscle contraction headache. J Clin Pharmacol 1980;20:298-302;Diamond S, Medina JL. A double-blind study of zomepirac sodium and placebo in the treatment of muscle contraction headache. Headache 1981; 21:45-48.
14. Diamond S, Balm TK, Freitag FG. Ibuprofen plus caffeine in the treatment of tension-type headache. Clin Pharmacol Ther 2000;68:312-319;Diamond S, Freitag FG. The use of ibuprofen plus caffeine to treat tension-type headache. Curr Pain Headache Rep 2001; 5:472-478.
15. von Graffenried B, Hill RC, Nüesch E. Headache as a model for assessing mild analgesic drugs. J Clin Pharmacol 1980;20:131-144;von Graffenried B, Nüesch B. Non-migrainous headache for the evaluation of oral analgesics. Br J Clin Pharmacol 1980; 10(suppl2):225S-231S.
16. Friedman AP, Boyles WF, Elkind AH, et al. Fiorinal with codeine in the treatment of tension headache-the contribution of components to the combination drug. Clin Ther 1988;10:303-315;Hwang DS, Mietlowski MJ, Friedman AP. Fiorinal with Codeine in the management of tension headache: impact of placebo response. Clin Ther 1987; 9:201-222.
17. Dahlöf CG, Jacobs LD. Ketoprofen, paracetamol and placebo in the treatment of episodic tension-type headache. Cephalalgia 1996;16:117-123.
18. Gilbert MM, De Sola Pool N, Schecter C. Analgesic/calmative effects of acetaminophen and phenyltoloxamine in treatment of simple nervous tension accompanied by headache. Curr Ther Res Clin Exp 1976;20:53-58.
19. Göbel H, Fresenius J, Heinze A, Dworschak M, Soyka D. Effectiveness of peppermint oil and paracetamol in the treatment of tension headache [German]. Nervenarzt 1996;67:672-681.
20. Göbel H, Heinze A, Lurch A, Dworschak M. Essential oils in the therapy of tension headache [German]. Z Allg Med 1998;74:223-228.
21. Göbel H, Heinze A, Dworschak M, Heinze-Kuhn Stolze H. Analgesic efficacy and tolerability of locally applied oleum menthae piperitae preparation LI 170 in patients with migraine or tension-type headache [German]. Z Allg Med 2001;77:287-295.
22. Guidotti M, Zanasi S, Garagiola U. Pirprofen in the treatment of migraine and episodic headache attacks: a placebo-controlled crossover clinical trial. J Int Med Res 1989;17:48-54.
23. Langemark M, Olesen J. Effervescent ASA versus solid ASA in the treatment of tension headache. A double-blind, placebo controlled study. Headache 1987;27:90-95.
24. Laveneziana D, Speranza R, Raulli P, Paredi G. Comparative efficacy of ibuprofen arginine and beta-cyclodextrin piroxicam as treatment for tension-type headache. Clin Drug Invest 1996;11(Suppl 1):22-26.
25. Migliardi JR, Armellino JJ, Friedman M, Gillings DB, Beaver WT. Caffeine as an analgesic adjuvant in tension headache. Clin Pharmacol Ther 1994;56:576-586.
26. Ryan RE, Sr. Motrin- A new agent for the symptomatic treatment of muscle contraction headache. Headache 1977;16:280-283.
27. Wood A, von Graffenried B. Fluproquazone: Analgesic activity in outpatients with non-migrainous headache. Arzneim-Forsch/Drug Res 1981;31:914-917.
28. Lange R, Lentz R. Comparison ketoprofen, ibuprofen and naproxen sodium in the treatment of tension-type headache. Drugs Exp Clin Res 1995;21:89-96.
29. Martinez-Martin P, Raffaelli E, Jr, Titus F, et al. Efficacy and safety of metamizol vs. acetylsalicylic acid in patients with moderate episodic tension-type headache: a randomized, double-blind, placebo- and active-controlled, multicentre study. Cephalalgia 2001;21:604-610.
30. Mehlisch DR, Weaver M, Fladung B. Ketoprofen, acetaminophen, and placebo in the treatment of tension headache. Headache 1998;38:579-589.
31. Packman B, Packman E, Doyle G, et al. Solubilized ibuprofen: evaluation of onset, relief, and safety of a novel formulation in the treatment of episodic tension-type headache. Headache 2000;40:561-567.
32. Prior MJ, Cooper KM, May LG, Bowen DL. Efficacy and safety of acetaminophen and naproxen in the treatment of tension-type headache. A randomized, double-blind, placebo-controlled trial. Cephalalgia 2002;22:740-748.
33. Steiner TJ, Lange R. Ketoprofen (25 mg) in the symptomatic treatment of episodic tension-type headache: double-blind placebo-controlled comparison with acetaminophen (1000 mg). Cephalalgia 1998;18:38-43.
34. Steiner T, Lange R, Voelker M. Aspirin in episodic tension-type headache: placebo-controlled dose-ranging comparison with paracetamol. Cephalalgia 2003;23:59-66.
35. van Gerven JM, Schoemaker RC, Jacobs LD, et al. Self-medication of a single headache episode with ketoprofen, ibuprofen or placebo, home-monitored with an electronic patient diary. Br J Clin Pharmacol 1996;42:475-481.
36. Kubitzek F, Ziegler G, Gold MS, Liu JMH, Ionescu E. Low-dose diclofenac potassium in the treatment of episodic tension-type headache. European J Pain 2003;7:155-162.
37. Diamond S. Ibuprofen versus aspirin and placebo in the treatment of muscle contraction headache. Headache 1983;23:206-210.
38. DiSerio FJ, Friedman AP, Parno J, Singer JM. Proquazone for tension headache-a multicenter trial. Headache 1985;25:127-133.
39. Friedman AP. Assessment of Fiorinal with Codeine in the treatment of tension headache. Clin Ther 1986;8:703-721.
40. Friedman AP, DiSerio FJ. Symptomatic treatment of chronically recurring tension headache: a placebo-controlled, multicenter investigation of Fioricet and acetaminophen with codeine. Clin Ther 1987;10:69-81.
41. Miller DS, Talbot CA, Simpson W, Korey A. A comparison of naproxen sodium, acetaminophen and placebo in the treatment of muscle contraction headache. Headache 1987;27:392-396.
42. Sargent JD, Peters K, Goldstein J, Madison DS, Solbach P. Naproxen sodium for muscle contraction headache treatment. Headache 1988;28:180-182.
43. Schachtel BP, Thoden WR. Onset of action of ibuprofen in the treatment of muscle-contraction headache. Headache 1988;28:471-474.
44. Schachtel BP, Thoden WR, Konerman JP, Brown A, Chaing DS. Headache pain model for assessing and comparing the efficacy of over-the-counter analgesic agents. Clin Pharmacol Ther 1991;50:322-329.
45. Schachtel BP, Furey SA, Thoden WR. Nonprescription ibuprofen and acetaminophen in the treatment of tension-type headache. J Clin Pharmacol 1996;36:1120-1125.
46. Peters BH, Fraim CJ, Masel BE. Comparison of 650 mg aspirin and 1,000 mg acetaminophen with each other, and with placebo in moderately severe headache. Am J Med 1983;74:36-42.
47. Ryan RE, Sr, Ryan RE, Jr. Symptomatic treatment of tension headache. Ear Nose Throat J 1979;58:423-426.
48. Schattner P, Randerson D. Tiger Balm as a treatment of tension headache. A clinical trial in general practice. Aust Fam Physician 1996;25:216, 218,220passim
49. Ward N, Whitney C, Avery D, Dunner D. The analgesic effects of caffeine in headache. Pain 1991;44:151-155.
50. Borges J, Zavaleta C. Study of a new analgesic compound in the treatment of tension headache. J Int Med Res 1976;4:74-78.
51. Thorpe P. Controlled and uncontrolled studies on “Fiorinal-PA” for symptomatic relief in tension headache. Med J Aust 1970;2:180-181.
52. Kagan G, Masheter HC. A controlled study of short-term treatment of tension headache. Curr Med Res Opin 1978;5:709-713.
53. Scheepers F. Syndol in the treatment of tension headache. Med Proc 1971;359-368.