User login
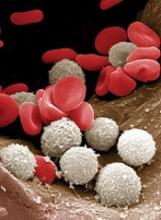
New research suggests that bacterial infection activates hematopoietic stem cells (HSCs) and significantly reduces their ability to produce blood by forcibly inducing proliferation.
These findings indicate that bacterial infections might cause dysregulated hematopoiesis like that which occurs in patients with anemias and leukemias.
Hitoshi Takizawa, PhD, of Kumamoto University’s International Research Center for Medical Sciences in Kumamoto, Japan, and his colleagues reported these findings in Cell Stem Cell.
The researchers gave lipopolysaccharide to mice to generate a bacterial infection model and analyzed the role of Toll-like receptors (TLRs) in HSCs.
The team found that lipopolysaccharides spread throughout the body, with some eventually reaching the bone marrow. This stimulated TLR4 and induced HSCs to proliferate.
However, the stimulus also induced stress on the HSCs.
So although HSCs proliferate temporarily upon TLR4 stimulation, their ability to successfully self-replicate decreases, resulting in diminished blood production.
The researchers observed similar results after infecting mice with Salmonella Typhimurium.
“Fortunately, we were able to confirm that this molecular reaction can be inhibited by drugs,” Dr Takizawa said.
Specifically, the researchers found that activation of reactive oxygen species and p38 through TLR4 ligation is key to HSC dysfunction.
And small-molecule inhibitors of reactive oxygen species and p38 were able to prevent HSC dysfunction.
“The medication maintains the production of blood and immune cells without weakening the immune reaction against pathogenic bacteria,” Dr Takizawa said. “It might be possible to simultaneously prevent blood diseases and many bacterial infections in the future.” ![]()
New research suggests that bacterial infection activates hematopoietic stem cells (HSCs) and significantly reduces their ability to produce blood by forcibly inducing proliferation.
These findings indicate that bacterial infections might cause dysregulated hematopoiesis like that which occurs in patients with anemias and leukemias.
Hitoshi Takizawa, PhD, of Kumamoto University’s International Research Center for Medical Sciences in Kumamoto, Japan, and his colleagues reported these findings in Cell Stem Cell.
The researchers gave lipopolysaccharide to mice to generate a bacterial infection model and analyzed the role of Toll-like receptors (TLRs) in HSCs.
The team found that lipopolysaccharides spread throughout the body, with some eventually reaching the bone marrow. This stimulated TLR4 and induced HSCs to proliferate.
However, the stimulus also induced stress on the HSCs.
So although HSCs proliferate temporarily upon TLR4 stimulation, their ability to successfully self-replicate decreases, resulting in diminished blood production.
The researchers observed similar results after infecting mice with Salmonella Typhimurium.
“Fortunately, we were able to confirm that this molecular reaction can be inhibited by drugs,” Dr Takizawa said.
Specifically, the researchers found that activation of reactive oxygen species and p38 through TLR4 ligation is key to HSC dysfunction.
And small-molecule inhibitors of reactive oxygen species and p38 were able to prevent HSC dysfunction.
“The medication maintains the production of blood and immune cells without weakening the immune reaction against pathogenic bacteria,” Dr Takizawa said. “It might be possible to simultaneously prevent blood diseases and many bacterial infections in the future.” ![]()
New research suggests that bacterial infection activates hematopoietic stem cells (HSCs) and significantly reduces their ability to produce blood by forcibly inducing proliferation.
These findings indicate that bacterial infections might cause dysregulated hematopoiesis like that which occurs in patients with anemias and leukemias.
Hitoshi Takizawa, PhD, of Kumamoto University’s International Research Center for Medical Sciences in Kumamoto, Japan, and his colleagues reported these findings in Cell Stem Cell.
The researchers gave lipopolysaccharide to mice to generate a bacterial infection model and analyzed the role of Toll-like receptors (TLRs) in HSCs.
The team found that lipopolysaccharides spread throughout the body, with some eventually reaching the bone marrow. This stimulated TLR4 and induced HSCs to proliferate.
However, the stimulus also induced stress on the HSCs.
So although HSCs proliferate temporarily upon TLR4 stimulation, their ability to successfully self-replicate decreases, resulting in diminished blood production.
The researchers observed similar results after infecting mice with Salmonella Typhimurium.
“Fortunately, we were able to confirm that this molecular reaction can be inhibited by drugs,” Dr Takizawa said.
Specifically, the researchers found that activation of reactive oxygen species and p38 through TLR4 ligation is key to HSC dysfunction.
And small-molecule inhibitors of reactive oxygen species and p38 were able to prevent HSC dysfunction.
“The medication maintains the production of blood and immune cells without weakening the immune reaction against pathogenic bacteria,” Dr Takizawa said. “It might be possible to simultaneously prevent blood diseases and many bacterial infections in the future.” ![]()