User login
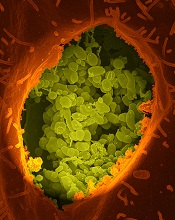
Coxiella burnetii
Image courtesy of NIAID
The bacterium that causes Q fever may confer an increased risk of diffuse large B-cell lymphoma (DLBCL) and follicular lymphoma (FL), according to a study published in Blood.
Q fever is an infectious disease caused by Coxiella burnetii, a bacterium primarily transmitted through the excrements of cattle, sheep, and goats.
Because some patients with Q fever develop lymphoma, researchers believed the malignancy could be a risk factor for Q fever.
However, the experience of 1 patient prompted a group of researchers in France to consider the opposite—that the infection might cause the lymphoma.
“During a follow-up scan in a patient we had successfully treated for Q fever, we observed a tumor close to the location of the previous infection,” said study author Didier Raoult, MD, PhD, of Aix-Marseille University in Marseille, France.
“The discovery that it was a lymphoma tumor containing C burnetii encouraged us to consider that the infection might have contributed to the development of the cancer.”
To better understand the association between C burnetii and lymphoma, Dr Raoult and his colleagues screened 1468 patients treated at the French National Referral Center for Q Fever from 2004 to 2014.
The researchers imaged patient tissue samples and identified 7 people, including the initial patient, who developed lymphoma after C burnetii infection. Six patients were diagnosed with DLBCL and 1 with FL.
To determine if patients with Q fever have a higher risk of lymphoma than the general population, the researchers compared the incidence of lymphoma in the Q fever registry to the incidence reported in France’s general population.
This revealed an excess risk of DLBCL and FL in the Q fever population, with standardized incidence ratios of 25.4 for DLBCL and 6.7 for FL.
In addition, the odds of developing lymphoma were higher in patients with persistent, concentrated infections than in those with other forms of Q fever. The hazard ratio for patients with persistent, concentrated infection was 9.35.
Finally, the researchers observed interleukin-10 overproduction in Q fever patients with lymphoma. The team said this suggests that suppression of the immune system may have allowed the lymphoma cells to evade immune detection and multiply.
“As we continue to learn more about the association between C burnetii and lymphoma, these results should encourage clinicians to survey high-risk patients as early as possible for potential cancer,” Dr Raoult said.
“Ultimately, this early diagnosis and treatment would improve outcomes for Q fever patients who subsequently develop lymphoma, particularly those with B-cell non-Hodgkin lymphoma.” ![]()
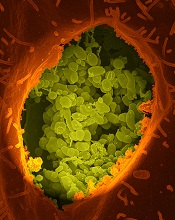
Coxiella burnetii
Image courtesy of NIAID
The bacterium that causes Q fever may confer an increased risk of diffuse large B-cell lymphoma (DLBCL) and follicular lymphoma (FL), according to a study published in Blood.
Q fever is an infectious disease caused by Coxiella burnetii, a bacterium primarily transmitted through the excrements of cattle, sheep, and goats.
Because some patients with Q fever develop lymphoma, researchers believed the malignancy could be a risk factor for Q fever.
However, the experience of 1 patient prompted a group of researchers in France to consider the opposite—that the infection might cause the lymphoma.
“During a follow-up scan in a patient we had successfully treated for Q fever, we observed a tumor close to the location of the previous infection,” said study author Didier Raoult, MD, PhD, of Aix-Marseille University in Marseille, France.
“The discovery that it was a lymphoma tumor containing C burnetii encouraged us to consider that the infection might have contributed to the development of the cancer.”
To better understand the association between C burnetii and lymphoma, Dr Raoult and his colleagues screened 1468 patients treated at the French National Referral Center for Q Fever from 2004 to 2014.
The researchers imaged patient tissue samples and identified 7 people, including the initial patient, who developed lymphoma after C burnetii infection. Six patients were diagnosed with DLBCL and 1 with FL.
To determine if patients with Q fever have a higher risk of lymphoma than the general population, the researchers compared the incidence of lymphoma in the Q fever registry to the incidence reported in France’s general population.
This revealed an excess risk of DLBCL and FL in the Q fever population, with standardized incidence ratios of 25.4 for DLBCL and 6.7 for FL.
In addition, the odds of developing lymphoma were higher in patients with persistent, concentrated infections than in those with other forms of Q fever. The hazard ratio for patients with persistent, concentrated infection was 9.35.
Finally, the researchers observed interleukin-10 overproduction in Q fever patients with lymphoma. The team said this suggests that suppression of the immune system may have allowed the lymphoma cells to evade immune detection and multiply.
“As we continue to learn more about the association between C burnetii and lymphoma, these results should encourage clinicians to survey high-risk patients as early as possible for potential cancer,” Dr Raoult said.
“Ultimately, this early diagnosis and treatment would improve outcomes for Q fever patients who subsequently develop lymphoma, particularly those with B-cell non-Hodgkin lymphoma.” ![]()
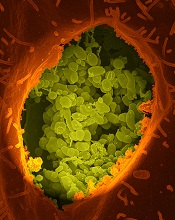
Coxiella burnetii
Image courtesy of NIAID
The bacterium that causes Q fever may confer an increased risk of diffuse large B-cell lymphoma (DLBCL) and follicular lymphoma (FL), according to a study published in Blood.
Q fever is an infectious disease caused by Coxiella burnetii, a bacterium primarily transmitted through the excrements of cattle, sheep, and goats.
Because some patients with Q fever develop lymphoma, researchers believed the malignancy could be a risk factor for Q fever.
However, the experience of 1 patient prompted a group of researchers in France to consider the opposite—that the infection might cause the lymphoma.
“During a follow-up scan in a patient we had successfully treated for Q fever, we observed a tumor close to the location of the previous infection,” said study author Didier Raoult, MD, PhD, of Aix-Marseille University in Marseille, France.
“The discovery that it was a lymphoma tumor containing C burnetii encouraged us to consider that the infection might have contributed to the development of the cancer.”
To better understand the association between C burnetii and lymphoma, Dr Raoult and his colleagues screened 1468 patients treated at the French National Referral Center for Q Fever from 2004 to 2014.
The researchers imaged patient tissue samples and identified 7 people, including the initial patient, who developed lymphoma after C burnetii infection. Six patients were diagnosed with DLBCL and 1 with FL.
To determine if patients with Q fever have a higher risk of lymphoma than the general population, the researchers compared the incidence of lymphoma in the Q fever registry to the incidence reported in France’s general population.
This revealed an excess risk of DLBCL and FL in the Q fever population, with standardized incidence ratios of 25.4 for DLBCL and 6.7 for FL.
In addition, the odds of developing lymphoma were higher in patients with persistent, concentrated infections than in those with other forms of Q fever. The hazard ratio for patients with persistent, concentrated infection was 9.35.
Finally, the researchers observed interleukin-10 overproduction in Q fever patients with lymphoma. The team said this suggests that suppression of the immune system may have allowed the lymphoma cells to evade immune detection and multiply.
“As we continue to learn more about the association between C burnetii and lymphoma, these results should encourage clinicians to survey high-risk patients as early as possible for potential cancer,” Dr Raoult said.
“Ultimately, this early diagnosis and treatment would improve outcomes for Q fever patients who subsequently develop lymphoma, particularly those with B-cell non-Hodgkin lymphoma.” ![]()