User login
SHM has gotten behind the Choosing Wisely campaign in a big way. Earlier this year, SHM announced lists of suggested practices for adult and pediatric hospital medicine (see Table 1). To keep it on the front burner, hospitalists John Bulger and Ian Jenkins held a pre-course at HM13 devoted entirely to quality-improvement (QI) approaches to implementing and sustaining the practices outlined in the campaign. During the main meeting, they did an encore presentation, with Doug Carlson and Ricardo Quinonez presenting the elements of Choosing Wisely for pediatric hospital medicine.
The widely publicized campaign arose from an American Board of Internal Medicine (ABIM) Foundation grant program to “facilitate the development of innovative, emerging strategies to advance appropriate health-care decision-making and stewardship of health-care resources.” (For more information, visit www.abimfoundation.org.)
Adoption of many of the suggested Choosing Wisely practices will require a change in deeply ingrained, habitual behaviors. We assert that rational, reflective, cognitive processes might not be enough to overturn these behaviors, and that we must look to other mental systems to achieve the consistent adoption of the campaign’s suggested practices. An analogy exists in economics, where theories behind classical economics are challenged by behavioral economics.
What is behavioral economics? Classical economics asserts the individual as “homo economicus”: a person making rational, predictable decisions to advance their interests. However, due to social or professional influence, behavior often does not comport to expected ends. We succumb, sympathize, or follow the pack, diverging from the rulebook. Behavioral economics attempts to understand and compensate for these deviations.
In medicine, we often yield to cognitive biases. To simplify decision-making, we generalize our observations to arrive at decisions quickly. Daniel Kahneman, winner of the Nobel Memorial Prize in Economic Sciences, describes Type I thinking as fast and automatic, and Type II thinking as slow and effortful. Using Kahneman’s framework, we attempt to understand where reasoning may stray and, in turn, introduce environmental changes to achieve better outcomes.
How does this relate to Choosing Wisely? Embracing and embedding the practices of the Choosing Wisely campaign in day-to-day practice will require change in how we approach the clinical decisions we make each day. How can we create the conditions so as not to yield to the status quo?
The MINDSPACE framework
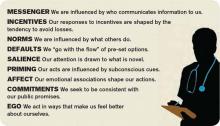
King et al in a recent Health Affairs article describe the MINDSPACE framework (see Table 2), which captures nine effects on behavior—messenger, incentives, norms, defaults, salience, priming, affect, commitments, and ego—that mostly involve automatic systems (Kahneman’s Type I), and how we can leverage them to minimize ineffective health care.1 Below, we describe Choosing Wisely’s HM components and how MINDSPACE can help promote better practice.
Messenger refers to the importance we place on the source of information conveyed to us. In the campaign, the ABIM Foundation engaged professional societies to come up with a list of specialty-specific practices. We know physicians pay more attention to messages from professional societies than, for example, insurance companies. Having the chair of medicine, the chief of hospital medicine, or the vice president of quality officially sanction the campaign’s practices at your organization leverages messengers.
Incentives, while widely used in health care, have had mixed results in terms of their utility in improving outcomes. People are loss-averse, and behavioral economics leverages that finding, which means incentives structured as penalties seem to have more powerful effects than bonuses. While the familiar pay-for-performance programs might not yield desired results, the evidence base continues to grow, and we have lots to learn. Does a 2% bonus change culture? What would really facilitate modifications in your test ordering patterns?
Norms, or what we perceive as the views of the majority, shape our behavior. How do we establish new ones? We all know the axiom “culture eats strategy for breakfast,” and, like patterned antibiotic administration, redirecting behavior requires examination of why we order items. Often, we order not because the drug combination conforms to standards, but because our training programs imbue us with less-than-ideal habits. These habits become standards, and their root causes require layered examination.
Defaults suggest that we are more likely to embrace a certain behavior if we otherwise need to “opt out” to avoid the behavior. We know that, for example, automatic enrollment in retirement savings plans has dramatically increased participation in such programs. For the Choosing Wisely campaign, the suggested practices should be set up as the default option. Examples include appropriate auto-stop orders for urinary catheters, telemetry, oximetry, or the requirement for added clicks to order daily CBCs. Think about ED orders and how they become substitute defaults once patients arrive on the wards. How do you disrupt the inertia?
Salience is when an individual makes a decision based on what is novel or what their attention is drawn to. Anticipating what subspecialists might expect, what your CMO demands, or what trainees envisage in their supervising attendings all may subconsciously override best judgment and deter best practice.
Priming describes how simple cues—often detected by our subconscious—influence decisions we make. When a physician, perhaps out of concern but often due to poorly reasoned or cavalier messaging, scribes “consider test X,” we involuntarily complete the act. We assume, because of the prime, that we need to act accordingly.
Affect is when we rely on gut feelings to make decisions. Emotions guide our ordering a urinary catheter for incontinence or transfusing to a HGB of 10, even when evidence contradicts what we might know as correct. Countering these actions requires credible stops to convert our emotions to reason (think clinical decision support with teeth).
Commitments are made in advance of an undertaking, behavioral economics suggests, as a way to combat the moment when willpower fails and desired behaviors go by the wayside. By publically signing a contract, in front of your group, chair, or medical director, and going on record as having pledged something, chances of success increase.
Ego, which underpins the need for a positive self-image, can drive the kind of automatic behavior that enables one to compare favorably to others. This effect has driven much of the motivation to perform well on public reporting of hospital quality measures. But ideal reporting of results must be valid; otherwise, attribution of subpar outcomes justifies the usual refrains of “not my responsibility” or the “system needs fixing, not me.”
Conclusions
Choosing Wisely is an ambitious undertaking made up of more than 90 suggested best practices put forth by 25 medical societies. In their book “Nudge,” authors Richard Thaler and Cass Sunstein describe how automatic behaviors arise from the environment or context in which choices to engage in such behaviors are presented.2 For the Choosing Wisely campaign to have staying power, we submit that institutional leaders and front-line clinicians will need to create a context where the safest, most cost-effective choices are the automatic, or nearly automatic, ones.
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is co-founder and past president of SHM. Email him at [email protected]. Dr. Flansbaum is director of hospitalist services at Lenox Hill Hospital in New York City and an SHM Public Policy Committee member.
References
- King D, Greaves F, Vlaev I, Darzi A. Approaches based on behavioral economics could help nudge patients and providers toward lower health spending growth. Health Aff (Millwood). 2013;32(4):661-668.
- Thaler RH, Sunstein CR. Nudge: improving decisions about health, wealth and happiness. New Haven, Conn: Yale University Press; 2008.
SHM has gotten behind the Choosing Wisely campaign in a big way. Earlier this year, SHM announced lists of suggested practices for adult and pediatric hospital medicine (see Table 1). To keep it on the front burner, hospitalists John Bulger and Ian Jenkins held a pre-course at HM13 devoted entirely to quality-improvement (QI) approaches to implementing and sustaining the practices outlined in the campaign. During the main meeting, they did an encore presentation, with Doug Carlson and Ricardo Quinonez presenting the elements of Choosing Wisely for pediatric hospital medicine.
The widely publicized campaign arose from an American Board of Internal Medicine (ABIM) Foundation grant program to “facilitate the development of innovative, emerging strategies to advance appropriate health-care decision-making and stewardship of health-care resources.” (For more information, visit www.abimfoundation.org.)
Adoption of many of the suggested Choosing Wisely practices will require a change in deeply ingrained, habitual behaviors. We assert that rational, reflective, cognitive processes might not be enough to overturn these behaviors, and that we must look to other mental systems to achieve the consistent adoption of the campaign’s suggested practices. An analogy exists in economics, where theories behind classical economics are challenged by behavioral economics.
What is behavioral economics? Classical economics asserts the individual as “homo economicus”: a person making rational, predictable decisions to advance their interests. However, due to social or professional influence, behavior often does not comport to expected ends. We succumb, sympathize, or follow the pack, diverging from the rulebook. Behavioral economics attempts to understand and compensate for these deviations.
In medicine, we often yield to cognitive biases. To simplify decision-making, we generalize our observations to arrive at decisions quickly. Daniel Kahneman, winner of the Nobel Memorial Prize in Economic Sciences, describes Type I thinking as fast and automatic, and Type II thinking as slow and effortful. Using Kahneman’s framework, we attempt to understand where reasoning may stray and, in turn, introduce environmental changes to achieve better outcomes.
How does this relate to Choosing Wisely? Embracing and embedding the practices of the Choosing Wisely campaign in day-to-day practice will require change in how we approach the clinical decisions we make each day. How can we create the conditions so as not to yield to the status quo?
The MINDSPACE framework
King et al in a recent Health Affairs article describe the MINDSPACE framework (see Table 2), which captures nine effects on behavior—messenger, incentives, norms, defaults, salience, priming, affect, commitments, and ego—that mostly involve automatic systems (Kahneman’s Type I), and how we can leverage them to minimize ineffective health care.1 Below, we describe Choosing Wisely’s HM components and how MINDSPACE can help promote better practice.
Messenger refers to the importance we place on the source of information conveyed to us. In the campaign, the ABIM Foundation engaged professional societies to come up with a list of specialty-specific practices. We know physicians pay more attention to messages from professional societies than, for example, insurance companies. Having the chair of medicine, the chief of hospital medicine, or the vice president of quality officially sanction the campaign’s practices at your organization leverages messengers.
Incentives, while widely used in health care, have had mixed results in terms of their utility in improving outcomes. People are loss-averse, and behavioral economics leverages that finding, which means incentives structured as penalties seem to have more powerful effects than bonuses. While the familiar pay-for-performance programs might not yield desired results, the evidence base continues to grow, and we have lots to learn. Does a 2% bonus change culture? What would really facilitate modifications in your test ordering patterns?
Norms, or what we perceive as the views of the majority, shape our behavior. How do we establish new ones? We all know the axiom “culture eats strategy for breakfast,” and, like patterned antibiotic administration, redirecting behavior requires examination of why we order items. Often, we order not because the drug combination conforms to standards, but because our training programs imbue us with less-than-ideal habits. These habits become standards, and their root causes require layered examination.
Defaults suggest that we are more likely to embrace a certain behavior if we otherwise need to “opt out” to avoid the behavior. We know that, for example, automatic enrollment in retirement savings plans has dramatically increased participation in such programs. For the Choosing Wisely campaign, the suggested practices should be set up as the default option. Examples include appropriate auto-stop orders for urinary catheters, telemetry, oximetry, or the requirement for added clicks to order daily CBCs. Think about ED orders and how they become substitute defaults once patients arrive on the wards. How do you disrupt the inertia?
Salience is when an individual makes a decision based on what is novel or what their attention is drawn to. Anticipating what subspecialists might expect, what your CMO demands, or what trainees envisage in their supervising attendings all may subconsciously override best judgment and deter best practice.
Priming describes how simple cues—often detected by our subconscious—influence decisions we make. When a physician, perhaps out of concern but often due to poorly reasoned or cavalier messaging, scribes “consider test X,” we involuntarily complete the act. We assume, because of the prime, that we need to act accordingly.
Affect is when we rely on gut feelings to make decisions. Emotions guide our ordering a urinary catheter for incontinence or transfusing to a HGB of 10, even when evidence contradicts what we might know as correct. Countering these actions requires credible stops to convert our emotions to reason (think clinical decision support with teeth).
Commitments are made in advance of an undertaking, behavioral economics suggests, as a way to combat the moment when willpower fails and desired behaviors go by the wayside. By publically signing a contract, in front of your group, chair, or medical director, and going on record as having pledged something, chances of success increase.
Ego, which underpins the need for a positive self-image, can drive the kind of automatic behavior that enables one to compare favorably to others. This effect has driven much of the motivation to perform well on public reporting of hospital quality measures. But ideal reporting of results must be valid; otherwise, attribution of subpar outcomes justifies the usual refrains of “not my responsibility” or the “system needs fixing, not me.”
Conclusions
Choosing Wisely is an ambitious undertaking made up of more than 90 suggested best practices put forth by 25 medical societies. In their book “Nudge,” authors Richard Thaler and Cass Sunstein describe how automatic behaviors arise from the environment or context in which choices to engage in such behaviors are presented.2 For the Choosing Wisely campaign to have staying power, we submit that institutional leaders and front-line clinicians will need to create a context where the safest, most cost-effective choices are the automatic, or nearly automatic, ones.
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is co-founder and past president of SHM. Email him at [email protected]. Dr. Flansbaum is director of hospitalist services at Lenox Hill Hospital in New York City and an SHM Public Policy Committee member.
References
- King D, Greaves F, Vlaev I, Darzi A. Approaches based on behavioral economics could help nudge patients and providers toward lower health spending growth. Health Aff (Millwood). 2013;32(4):661-668.
- Thaler RH, Sunstein CR. Nudge: improving decisions about health, wealth and happiness. New Haven, Conn: Yale University Press; 2008.
SHM has gotten behind the Choosing Wisely campaign in a big way. Earlier this year, SHM announced lists of suggested practices for adult and pediatric hospital medicine (see Table 1). To keep it on the front burner, hospitalists John Bulger and Ian Jenkins held a pre-course at HM13 devoted entirely to quality-improvement (QI) approaches to implementing and sustaining the practices outlined in the campaign. During the main meeting, they did an encore presentation, with Doug Carlson and Ricardo Quinonez presenting the elements of Choosing Wisely for pediatric hospital medicine.
The widely publicized campaign arose from an American Board of Internal Medicine (ABIM) Foundation grant program to “facilitate the development of innovative, emerging strategies to advance appropriate health-care decision-making and stewardship of health-care resources.” (For more information, visit www.abimfoundation.org.)
Adoption of many of the suggested Choosing Wisely practices will require a change in deeply ingrained, habitual behaviors. We assert that rational, reflective, cognitive processes might not be enough to overturn these behaviors, and that we must look to other mental systems to achieve the consistent adoption of the campaign’s suggested practices. An analogy exists in economics, where theories behind classical economics are challenged by behavioral economics.
What is behavioral economics? Classical economics asserts the individual as “homo economicus”: a person making rational, predictable decisions to advance their interests. However, due to social or professional influence, behavior often does not comport to expected ends. We succumb, sympathize, or follow the pack, diverging from the rulebook. Behavioral economics attempts to understand and compensate for these deviations.
In medicine, we often yield to cognitive biases. To simplify decision-making, we generalize our observations to arrive at decisions quickly. Daniel Kahneman, winner of the Nobel Memorial Prize in Economic Sciences, describes Type I thinking as fast and automatic, and Type II thinking as slow and effortful. Using Kahneman’s framework, we attempt to understand where reasoning may stray and, in turn, introduce environmental changes to achieve better outcomes.
How does this relate to Choosing Wisely? Embracing and embedding the practices of the Choosing Wisely campaign in day-to-day practice will require change in how we approach the clinical decisions we make each day. How can we create the conditions so as not to yield to the status quo?
The MINDSPACE framework
King et al in a recent Health Affairs article describe the MINDSPACE framework (see Table 2), which captures nine effects on behavior—messenger, incentives, norms, defaults, salience, priming, affect, commitments, and ego—that mostly involve automatic systems (Kahneman’s Type I), and how we can leverage them to minimize ineffective health care.1 Below, we describe Choosing Wisely’s HM components and how MINDSPACE can help promote better practice.
Messenger refers to the importance we place on the source of information conveyed to us. In the campaign, the ABIM Foundation engaged professional societies to come up with a list of specialty-specific practices. We know physicians pay more attention to messages from professional societies than, for example, insurance companies. Having the chair of medicine, the chief of hospital medicine, or the vice president of quality officially sanction the campaign’s practices at your organization leverages messengers.
Incentives, while widely used in health care, have had mixed results in terms of their utility in improving outcomes. People are loss-averse, and behavioral economics leverages that finding, which means incentives structured as penalties seem to have more powerful effects than bonuses. While the familiar pay-for-performance programs might not yield desired results, the evidence base continues to grow, and we have lots to learn. Does a 2% bonus change culture? What would really facilitate modifications in your test ordering patterns?
Norms, or what we perceive as the views of the majority, shape our behavior. How do we establish new ones? We all know the axiom “culture eats strategy for breakfast,” and, like patterned antibiotic administration, redirecting behavior requires examination of why we order items. Often, we order not because the drug combination conforms to standards, but because our training programs imbue us with less-than-ideal habits. These habits become standards, and their root causes require layered examination.
Defaults suggest that we are more likely to embrace a certain behavior if we otherwise need to “opt out” to avoid the behavior. We know that, for example, automatic enrollment in retirement savings plans has dramatically increased participation in such programs. For the Choosing Wisely campaign, the suggested practices should be set up as the default option. Examples include appropriate auto-stop orders for urinary catheters, telemetry, oximetry, or the requirement for added clicks to order daily CBCs. Think about ED orders and how they become substitute defaults once patients arrive on the wards. How do you disrupt the inertia?
Salience is when an individual makes a decision based on what is novel or what their attention is drawn to. Anticipating what subspecialists might expect, what your CMO demands, or what trainees envisage in their supervising attendings all may subconsciously override best judgment and deter best practice.
Priming describes how simple cues—often detected by our subconscious—influence decisions we make. When a physician, perhaps out of concern but often due to poorly reasoned or cavalier messaging, scribes “consider test X,” we involuntarily complete the act. We assume, because of the prime, that we need to act accordingly.
Affect is when we rely on gut feelings to make decisions. Emotions guide our ordering a urinary catheter for incontinence or transfusing to a HGB of 10, even when evidence contradicts what we might know as correct. Countering these actions requires credible stops to convert our emotions to reason (think clinical decision support with teeth).
Commitments are made in advance of an undertaking, behavioral economics suggests, as a way to combat the moment when willpower fails and desired behaviors go by the wayside. By publically signing a contract, in front of your group, chair, or medical director, and going on record as having pledged something, chances of success increase.
Ego, which underpins the need for a positive self-image, can drive the kind of automatic behavior that enables one to compare favorably to others. This effect has driven much of the motivation to perform well on public reporting of hospital quality measures. But ideal reporting of results must be valid; otherwise, attribution of subpar outcomes justifies the usual refrains of “not my responsibility” or the “system needs fixing, not me.”
Conclusions
Choosing Wisely is an ambitious undertaking made up of more than 90 suggested best practices put forth by 25 medical societies. In their book “Nudge,” authors Richard Thaler and Cass Sunstein describe how automatic behaviors arise from the environment or context in which choices to engage in such behaviors are presented.2 For the Choosing Wisely campaign to have staying power, we submit that institutional leaders and front-line clinicians will need to create a context where the safest, most cost-effective choices are the automatic, or nearly automatic, ones.
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is co-founder and past president of SHM. Email him at [email protected]. Dr. Flansbaum is director of hospitalist services at Lenox Hill Hospital in New York City and an SHM Public Policy Committee member.
References
- King D, Greaves F, Vlaev I, Darzi A. Approaches based on behavioral economics could help nudge patients and providers toward lower health spending growth. Health Aff (Millwood). 2013;32(4):661-668.
- Thaler RH, Sunstein CR. Nudge: improving decisions about health, wealth and happiness. New Haven, Conn: Yale University Press; 2008.