User login
Dr. Whitcomb is chief medical officer of Remedy Partners. He is co-founder and past president of SHM. E-mail him at [email protected].
Female physicians, lower mortality, lower readmissions: A case study
Week in, week out for the past 25 years, I have had a front-row seat to the medical practice of a certain female physician: my wife, Heather. We met when we worked together on the wards during residency in 1991; spent a year in rural Montana working together in clinics, ERs, and hospitals; shared the care of one another’s patients as our practices grew in parallel – hers in skilled nursing facilities, mine in the hospital; and reunited in recent years to work together as part of the same practice.
When I saw the paper by Yusuke Tsugawa, MD, MPH, PhD, and his associates showing lower mortality and readmission rates for female physicians versus their male counterparts, I began to wonder if the case of Heather’s practice style, and my observations of it, could help to interpret the findings of the study (JAMA Intern Med. 2016 Dec 19. doi: 10.1001/jamainternmed.2016.7875). The authors suggested that female physicians may produce better outcomes than male physicians.
The study in question, which analyzed more than 1.5 million hospitalizations, looked at Medicare beneficiaries hospitalized with a medical condition treated by general internists between 2011 and 2014. The authors found that patients treated by female physicians had lower 30-day mortality (adjusted rate, 11.07% vs. 11.49%, P<.001) and readmissions (adjusted rate, 15.02% vs. 15.57%, P<.001) than those treated by male physicians within the same hospital. The differences were “modest but important,” coauthor Ashish K. Jha, MD, MPH, wrote in his blog. Numbers needed to treat to prevent one death and one readmission were 233 and 182, respectively.

My observations of Heather’s practice approach, compared with my own, center around three main themes:
She spends more time considering her approach to a challenging case.
She has less urgency in deciding on a definitive course of action and more patience in sorting things out before proceeding with a diagnostic and therapeutic plan. She is more likely to leave open the possibility of changing her mind; she has less of a tendency to anchor on a particular diagnosis and treatment. Put another way, she is more willing to continue with ambiguous findings without lateralizing to one particular approach.
She brings more work-life balance to her professional responsibilities.
Despite being highly productive at work (and at home), she has worked less than full time throughout her career. This means that, during any given patient encounter, she is more likely to be unburdened by overwork and its negative consequences. It is my sense that many full-time physicians would be happier (and more effective) if they simply worked less. Heather has had the self-knowledge to take on a more manageable workload; the result is that she has remained joyous in practice for more than two decades.
She is less dogmatic and more willing to customize care based on the needs of the individual patient.
Although a good fund of knowledge is essential, if such knowledge obscures the physician’s ability to read the patient, then it is best abandoned, at least temporarily. Heather refers to the body of scientific evidence frequently, but she reserves an equal or greater portion of her cognitive bandwidth for the patient she is caring for at a particular moment.
How might the observations of this case study help to derive meaning from the study by Dr. Tsugawa and his associates, so that all patients may benefit from whatever it is that female physicians do to achieve better outcomes?
First, if physicians – regardless of gender – simply have an awareness of anchoring bias or rushing to land on a diagnosis or treatment, they will be less likely to do so in the future.
Next, we can learn that avoiding overwork can make for more joy in work, and if this is so, our patients may fare better. When I say “avoiding overwork,” that might mean rethinking our assumptions underlying the amount of work we take on.
Finally, while amassing a large fund of knowledge is a good thing, balancing medical knowledge with knowledge of the individual patient is crucial to good medical practice.
Dr. Whitcomb is Chief Medical Officer at Remedy Partners in Darien, CT. He is a cofounder and past president of SHM. Email him at [email protected].
Week in, week out for the past 25 years, I have had a front-row seat to the medical practice of a certain female physician: my wife, Heather. We met when we worked together on the wards during residency in 1991; spent a year in rural Montana working together in clinics, ERs, and hospitals; shared the care of one another’s patients as our practices grew in parallel – hers in skilled nursing facilities, mine in the hospital; and reunited in recent years to work together as part of the same practice.
When I saw the paper by Yusuke Tsugawa, MD, MPH, PhD, and his associates showing lower mortality and readmission rates for female physicians versus their male counterparts, I began to wonder if the case of Heather’s practice style, and my observations of it, could help to interpret the findings of the study (JAMA Intern Med. 2016 Dec 19. doi: 10.1001/jamainternmed.2016.7875). The authors suggested that female physicians may produce better outcomes than male physicians.
The study in question, which analyzed more than 1.5 million hospitalizations, looked at Medicare beneficiaries hospitalized with a medical condition treated by general internists between 2011 and 2014. The authors found that patients treated by female physicians had lower 30-day mortality (adjusted rate, 11.07% vs. 11.49%, P<.001) and readmissions (adjusted rate, 15.02% vs. 15.57%, P<.001) than those treated by male physicians within the same hospital. The differences were “modest but important,” coauthor Ashish K. Jha, MD, MPH, wrote in his blog. Numbers needed to treat to prevent one death and one readmission were 233 and 182, respectively.

My observations of Heather’s practice approach, compared with my own, center around three main themes:
She spends more time considering her approach to a challenging case.
She has less urgency in deciding on a definitive course of action and more patience in sorting things out before proceeding with a diagnostic and therapeutic plan. She is more likely to leave open the possibility of changing her mind; she has less of a tendency to anchor on a particular diagnosis and treatment. Put another way, she is more willing to continue with ambiguous findings without lateralizing to one particular approach.
She brings more work-life balance to her professional responsibilities.
Despite being highly productive at work (and at home), she has worked less than full time throughout her career. This means that, during any given patient encounter, she is more likely to be unburdened by overwork and its negative consequences. It is my sense that many full-time physicians would be happier (and more effective) if they simply worked less. Heather has had the self-knowledge to take on a more manageable workload; the result is that she has remained joyous in practice for more than two decades.
She is less dogmatic and more willing to customize care based on the needs of the individual patient.
Although a good fund of knowledge is essential, if such knowledge obscures the physician’s ability to read the patient, then it is best abandoned, at least temporarily. Heather refers to the body of scientific evidence frequently, but she reserves an equal or greater portion of her cognitive bandwidth for the patient she is caring for at a particular moment.
How might the observations of this case study help to derive meaning from the study by Dr. Tsugawa and his associates, so that all patients may benefit from whatever it is that female physicians do to achieve better outcomes?
First, if physicians – regardless of gender – simply have an awareness of anchoring bias or rushing to land on a diagnosis or treatment, they will be less likely to do so in the future.
Next, we can learn that avoiding overwork can make for more joy in work, and if this is so, our patients may fare better. When I say “avoiding overwork,” that might mean rethinking our assumptions underlying the amount of work we take on.
Finally, while amassing a large fund of knowledge is a good thing, balancing medical knowledge with knowledge of the individual patient is crucial to good medical practice.
Dr. Whitcomb is Chief Medical Officer at Remedy Partners in Darien, CT. He is a cofounder and past president of SHM. Email him at [email protected].
Week in, week out for the past 25 years, I have had a front-row seat to the medical practice of a certain female physician: my wife, Heather. We met when we worked together on the wards during residency in 1991; spent a year in rural Montana working together in clinics, ERs, and hospitals; shared the care of one another’s patients as our practices grew in parallel – hers in skilled nursing facilities, mine in the hospital; and reunited in recent years to work together as part of the same practice.
When I saw the paper by Yusuke Tsugawa, MD, MPH, PhD, and his associates showing lower mortality and readmission rates for female physicians versus their male counterparts, I began to wonder if the case of Heather’s practice style, and my observations of it, could help to interpret the findings of the study (JAMA Intern Med. 2016 Dec 19. doi: 10.1001/jamainternmed.2016.7875). The authors suggested that female physicians may produce better outcomes than male physicians.
The study in question, which analyzed more than 1.5 million hospitalizations, looked at Medicare beneficiaries hospitalized with a medical condition treated by general internists between 2011 and 2014. The authors found that patients treated by female physicians had lower 30-day mortality (adjusted rate, 11.07% vs. 11.49%, P<.001) and readmissions (adjusted rate, 15.02% vs. 15.57%, P<.001) than those treated by male physicians within the same hospital. The differences were “modest but important,” coauthor Ashish K. Jha, MD, MPH, wrote in his blog. Numbers needed to treat to prevent one death and one readmission were 233 and 182, respectively.

My observations of Heather’s practice approach, compared with my own, center around three main themes:
She spends more time considering her approach to a challenging case.
She has less urgency in deciding on a definitive course of action and more patience in sorting things out before proceeding with a diagnostic and therapeutic plan. She is more likely to leave open the possibility of changing her mind; she has less of a tendency to anchor on a particular diagnosis and treatment. Put another way, she is more willing to continue with ambiguous findings without lateralizing to one particular approach.
She brings more work-life balance to her professional responsibilities.
Despite being highly productive at work (and at home), she has worked less than full time throughout her career. This means that, during any given patient encounter, she is more likely to be unburdened by overwork and its negative consequences. It is my sense that many full-time physicians would be happier (and more effective) if they simply worked less. Heather has had the self-knowledge to take on a more manageable workload; the result is that she has remained joyous in practice for more than two decades.
She is less dogmatic and more willing to customize care based on the needs of the individual patient.
Although a good fund of knowledge is essential, if such knowledge obscures the physician’s ability to read the patient, then it is best abandoned, at least temporarily. Heather refers to the body of scientific evidence frequently, but she reserves an equal or greater portion of her cognitive bandwidth for the patient she is caring for at a particular moment.
How might the observations of this case study help to derive meaning from the study by Dr. Tsugawa and his associates, so that all patients may benefit from whatever it is that female physicians do to achieve better outcomes?
First, if physicians – regardless of gender – simply have an awareness of anchoring bias or rushing to land on a diagnosis or treatment, they will be less likely to do so in the future.
Next, we can learn that avoiding overwork can make for more joy in work, and if this is so, our patients may fare better. When I say “avoiding overwork,” that might mean rethinking our assumptions underlying the amount of work we take on.
Finally, while amassing a large fund of knowledge is a good thing, balancing medical knowledge with knowledge of the individual patient is crucial to good medical practice.
Dr. Whitcomb is Chief Medical Officer at Remedy Partners in Darien, CT. He is a cofounder and past president of SHM. Email him at [email protected].
Thinking Outside the DRG Box
When choosing quality improvement activities, hospitalists have no shortage of choices. In this column, I offer a strategic guide for hospitalists as they assess where best to spend their energy as the shift to value-based care progresses. This includes the introduction of MACRA, the landmark new payment program for doctors and other clinicians (aka the Medicare Access and CHIP Reauthorization Act of 2015), with its incentives for participation in alternative payment models.
Since 1983, Medicare has reimbursed hospitals using a lump-sum payment known as a diagnosis-related group, or DRG. Since then, hospitals have focused a good deal of their energy on removing needless expenses from the hospitalization to improve their bottom line, recognizing the DRG payment they receive is relatively fixed. To this end, a major strategy has been to use hospitalists to decrease length of stay and “right size” the utilization of in-hospital tests and treatments.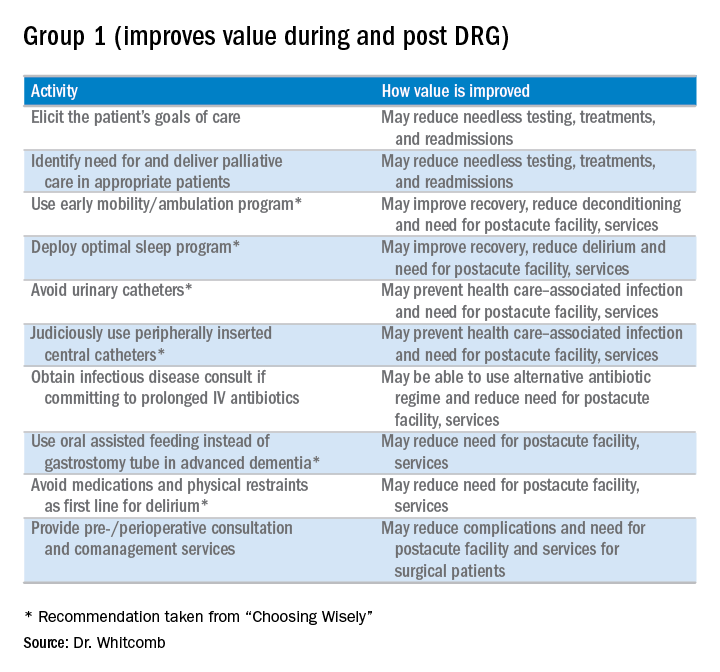
However, things are changing as we enter the era of alternative payment models such as accountable care organizations (ACOs) and bundled payments. The lens Medicare (and, to a great extent, commercial payors) peers through to assess inpatient hospital costs is the DRG payment amount. Beyond that, Medicare has little visibility into the actual costs hospitals incur. Since hospital spending equates to the payment amount for a DRG, it becomes apparent that the incremental opportunity for hospitalists to improve value (quality divided by cost) in alternative payment models stems from payments outside the DRG. Such payments include those related to the post-acute period such as nursing and rehabilitation facilities, readmissions, and part B activity (e.g., consultants and outpatient tests).
What does this mean for hospitalists? MACRA begins in 2019, but initial payments will be based on 2017 performance. The associated advantage of participating in an “advanced alternative payment model” where there is accountability for care beyond the hospitalization is that hospitalists will be rewarded for taking costs out of the post-acute time period.
To be clear, hospitalists should remain agents of in-hospital efficiency and quality. After all, that is how we add value to the hospitals in which we practice. All things being equal, however, hospitalists should focus on practices that will improve value beyond the four walls of the hospital.
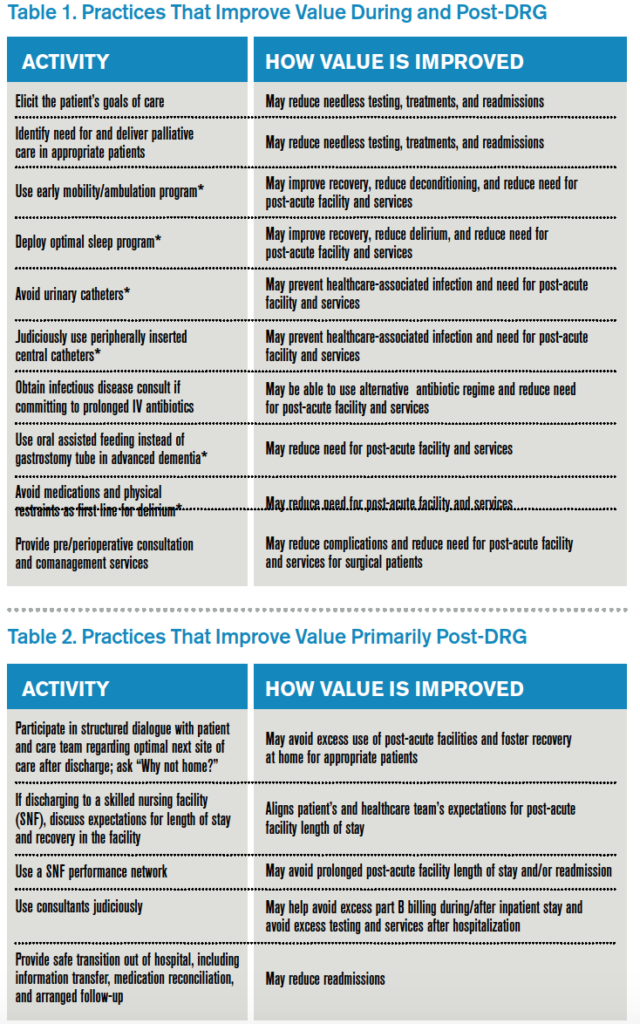
Here is my shortlist of these practices. While there is crossover between the categories, I divide the practices into those that improve value during the DRG period and also post-DRG and those that improve value primarily post-DRG (thanks to Choosing Wisely for contributing to the recommendations with an asterisk1):
Thinking outside the DRG box will require an adjustment to the approach taken by hospitalists because the current demands are often more than enough for a day’s work. Hospitalists will be called upon to innovate and fashion better approaches to care. This will require support by other members of the healthcare team so hospitalists can work smarter, not harder, to meet the requirements of a changing healthcare system. A prerequisite is better payment models that align financial incentives so that providing higher-value care is sustainable and appropriately rewarded.

Reference
Clinician lists. Choosing Wisely website. Accessed October 25, 2016.
When choosing quality improvement activities, hospitalists have no shortage of choices. In this column, I offer a strategic guide for hospitalists as they assess where best to spend their energy as the shift to value-based care progresses. This includes the introduction of MACRA, the landmark new payment program for doctors and other clinicians (aka the Medicare Access and CHIP Reauthorization Act of 2015), with its incentives for participation in alternative payment models.
Since 1983, Medicare has reimbursed hospitals using a lump-sum payment known as a diagnosis-related group, or DRG. Since then, hospitals have focused a good deal of their energy on removing needless expenses from the hospitalization to improve their bottom line, recognizing the DRG payment they receive is relatively fixed. To this end, a major strategy has been to use hospitalists to decrease length of stay and “right size” the utilization of in-hospital tests and treatments.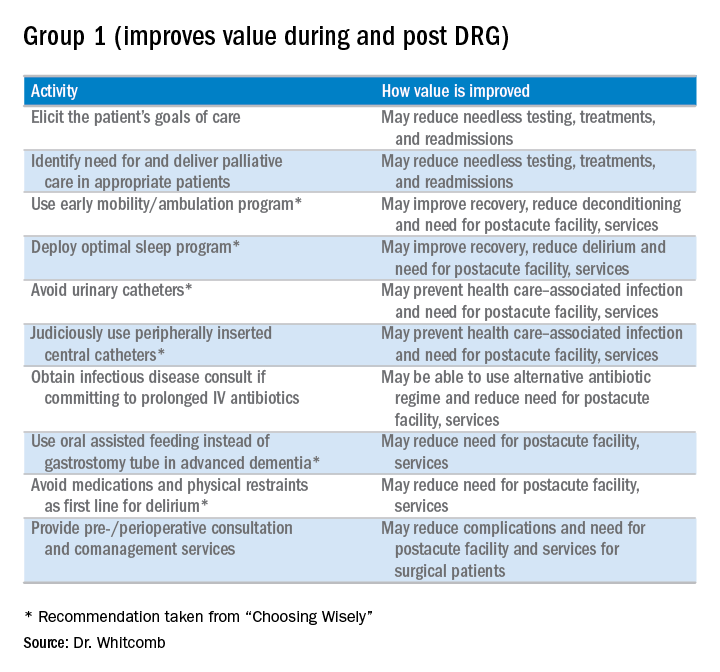
However, things are changing as we enter the era of alternative payment models such as accountable care organizations (ACOs) and bundled payments. The lens Medicare (and, to a great extent, commercial payors) peers through to assess inpatient hospital costs is the DRG payment amount. Beyond that, Medicare has little visibility into the actual costs hospitals incur. Since hospital spending equates to the payment amount for a DRG, it becomes apparent that the incremental opportunity for hospitalists to improve value (quality divided by cost) in alternative payment models stems from payments outside the DRG. Such payments include those related to the post-acute period such as nursing and rehabilitation facilities, readmissions, and part B activity (e.g., consultants and outpatient tests).
What does this mean for hospitalists? MACRA begins in 2019, but initial payments will be based on 2017 performance. The associated advantage of participating in an “advanced alternative payment model” where there is accountability for care beyond the hospitalization is that hospitalists will be rewarded for taking costs out of the post-acute time period.
To be clear, hospitalists should remain agents of in-hospital efficiency and quality. After all, that is how we add value to the hospitals in which we practice. All things being equal, however, hospitalists should focus on practices that will improve value beyond the four walls of the hospital.
Here is my shortlist of these practices. While there is crossover between the categories, I divide the practices into those that improve value during the DRG period and also post-DRG and those that improve value primarily post-DRG (thanks to Choosing Wisely for contributing to the recommendations with an asterisk1):
Thinking outside the DRG box will require an adjustment to the approach taken by hospitalists because the current demands are often more than enough for a day’s work. Hospitalists will be called upon to innovate and fashion better approaches to care. This will require support by other members of the healthcare team so hospitalists can work smarter, not harder, to meet the requirements of a changing healthcare system. A prerequisite is better payment models that align financial incentives so that providing higher-value care is sustainable and appropriately rewarded.

Reference
Clinician lists. Choosing Wisely website. Accessed October 25, 2016.
When choosing quality improvement activities, hospitalists have no shortage of choices. In this column, I offer a strategic guide for hospitalists as they assess where best to spend their energy as the shift to value-based care progresses. This includes the introduction of MACRA, the landmark new payment program for doctors and other clinicians (aka the Medicare Access and CHIP Reauthorization Act of 2015), with its incentives for participation in alternative payment models.
Since 1983, Medicare has reimbursed hospitals using a lump-sum payment known as a diagnosis-related group, or DRG. Since then, hospitals have focused a good deal of their energy on removing needless expenses from the hospitalization to improve their bottom line, recognizing the DRG payment they receive is relatively fixed. To this end, a major strategy has been to use hospitalists to decrease length of stay and “right size” the utilization of in-hospital tests and treatments.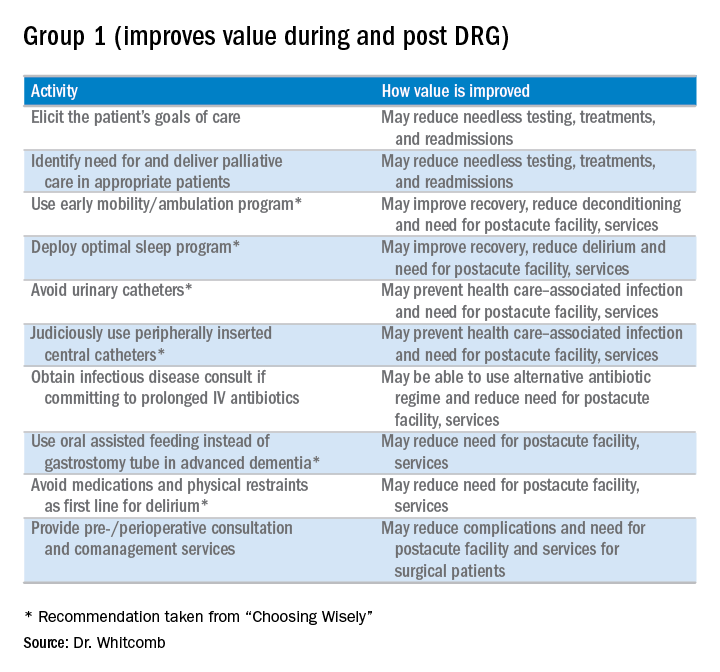
However, things are changing as we enter the era of alternative payment models such as accountable care organizations (ACOs) and bundled payments. The lens Medicare (and, to a great extent, commercial payors) peers through to assess inpatient hospital costs is the DRG payment amount. Beyond that, Medicare has little visibility into the actual costs hospitals incur. Since hospital spending equates to the payment amount for a DRG, it becomes apparent that the incremental opportunity for hospitalists to improve value (quality divided by cost) in alternative payment models stems from payments outside the DRG. Such payments include those related to the post-acute period such as nursing and rehabilitation facilities, readmissions, and part B activity (e.g., consultants and outpatient tests).
What does this mean for hospitalists? MACRA begins in 2019, but initial payments will be based on 2017 performance. The associated advantage of participating in an “advanced alternative payment model” where there is accountability for care beyond the hospitalization is that hospitalists will be rewarded for taking costs out of the post-acute time period.
To be clear, hospitalists should remain agents of in-hospital efficiency and quality. After all, that is how we add value to the hospitals in which we practice. All things being equal, however, hospitalists should focus on practices that will improve value beyond the four walls of the hospital.
Here is my shortlist of these practices. While there is crossover between the categories, I divide the practices into those that improve value during the DRG period and also post-DRG and those that improve value primarily post-DRG (thanks to Choosing Wisely for contributing to the recommendations with an asterisk1):
Thinking outside the DRG box will require an adjustment to the approach taken by hospitalists because the current demands are often more than enough for a day’s work. Hospitalists will be called upon to innovate and fashion better approaches to care. This will require support by other members of the healthcare team so hospitalists can work smarter, not harder, to meet the requirements of a changing healthcare system. A prerequisite is better payment models that align financial incentives so that providing higher-value care is sustainable and appropriately rewarded.

Reference
Clinician lists. Choosing Wisely website. Accessed October 25, 2016.
Providing Effective Palliative Care in the Era of Value
Although effective palliative care has always been a must-have for patients and caregivers facing serious illness, it hasn’t always been readily available. With the emergence of value-based healthcare models—and their potent incentives to reduce avoidable readmissions—there is renewed hope that such care will be accessible to those who need it.
Palliative and end-of-life care have long been promoted as core skills for hospitalists. The topic has regularly been included at SHM annual meetings and other prominent hospital medicine conferences, in the American Board of Internal Medicine blueprint for recognition of focused practice in hospital medicine, and in a number of influential references for hospitalists. Still, as I look at hospitalist programs around the country, there is a clear need to improve hospitalists’ delivery of palliative and end-of-life care.
Care of patients with chronic illness in their last two years of life accounts for a third of all Medicare spending.1 As hospitalists, we encounter many of these patients as they are hospitalized—and often re-hospitalized. Palliative care, which can improve quality of life and decrease costs for patients while leading to increased satisfaction and better outcomes for caregivers, can help alleviate unneeded and unwanted aggressive interventions like hospitalization.2,3
In its 2014 report, Dying in America, the Institute of Medicine (IOM) identified several areas for improvement, including better advance care planning and payment systems supporting high quality end-of-life care.4 As I write this column in mid 2016, there are two notable achievements since the IOM report: two E&M codes for advance care planning and a substantial and growing number of hospitalist patients in alternative payment models like bundled payments or ACOs.5 I believe we are entering a time when the availability of good palliative care will be accelerated due to broader forces in healthcare that for the first time align incentives between patients’ wishes and how care is paid for.
Palliative Care Skills for Hospitalists
The following are key actions for physicians in addressing palliative care for the hospitalized patient. At the risk of oversimplifying the discipline, I offer a few key actions for hospitalists to keep in mind.
Identify patients who would benefit from palliative care. The surprise question—“Would I be surprised if this patient died in the next year?”—has the ability to predict which patients would benefit from palliative care. In one observation from a group of patients with cancer, a “no” answer identified 60% of patients who died within a year.6 The surprise question has previously been shown to be predictive in other cancer and non-cancer populations.7,8
Weisman and Meier suggest using the following in a checklist at the time of hospital admission as “primary criteria to screen for unmet palliative care needs”:9
- The surprise question
- Frequent admissions
- Admission prompted by difficult-to-control physical or psychological symptoms
- Complex care requirements
- Decline in function, feeding intolerance, or unintended decline in weight
Hold a “goals of care” meeting. A notable step forward for supporting conversations between physicians and patients occurred on Jan. 1, when the Centers for Medicare & Medicaid Services (CMS) announced the Advance Care Planning E&M codes. These are CPT codes 99497 and 99498. They can be used on the same day as other E&M codes and cover discussions regarding advance care planning issues including discussing advance directives, appointing a healthcare proxy or durable power of attorney, discussing a living will, or addressing orders for life-sustaining treatment like the role of hydration or future hospitalizations. (For more information on how to use them, visit the CMS website and search for the FAQ.)
What should hospitalists concentrate on when having “goals of care” conversations with patients and caregivers? Ariadne Labs, a Harvard-affiliated health innovation group, offers the following as elements of a serious illness conversation:10
- Patients’ understanding of their illness
- Patients’ preferences for information and for family involvement
- Personal life goals, fears, and anxieties
- Trade-offs they are willing to accept
For hospitalists, an important area to pay particular attention to is the role of future hospitalizations in patients’ wishes for care, as some patients, if offered appropriate symptom control, would prefer to remain at home.
Two other crucial elements of inpatient palliative care—offer psychosocial support and symptom relief and hand off patient to effective post-hospital palliative care—are outside the scope of this article. However, they should be kept in mind and, of course, applied.
Understand the role of the palliative care consultation. Busy hospitalists might reasonably think, “I simply don’t have time to address palliative care in patients who aren’t likely to die during this hospitalization or soon after.” The palliative care consult service, if available, should be accessed when patients are identified as palliative care candidates but the primary hospitalist does not have the time or resources—including specialized knowledge in some cases—to deliver adequate palliative care. Palliative care specialists can also help bridge the gap between inpatient and outpatient palliative care resources.
In sum, the move to value-based payment models and the new advance care planning E&M codes provide a renewed focus—with more aligned incentives—and the opportunity to provide good palliative care to all who need it.
For hospitalists, identifying those who would benefit from palliative care and working with the healthcare team to ensure the care is delivered are at the heart of our professional mission. TH
References
- End-of-life care. The Darmouth Atlas of Health Care website. Accessed June 23, 2016.
- Gade G, Venohr I, Conner D, et al. Impact of an inpatient palliative care team: a randomized control trial. J Palliat Med. 2008;11(2):180-190.
- Morrison RS, Penrod JD, Cassel JB, et al. Cost savings associated with US hospital palliative care consultation programs. Arch Int Med. 2008;168(16):1783-1790.
- Institute of Medicine. Dying in America: Improving Quality and Honoring Individual Preferences near the End of Life. 2014.
- BPCI Model 2: Retrospective acute & post acute care episode. Centers for Medicare & Medicaid Services website. Accessed June 24, 2016.
- Vick JB, Pertsch N, Hutchings M, et al. The utility of the surprise question in identifying patients most at risk of death. J Clin Oncol. 2015;33(suppl):8.
- Moss AH, Ganjoo J, Sharma S, et al. Utility of the “surprise” question to identify dialysis patients with high mortality. Clin J Am Soc Nephrol. 2008;3:1379-1384.
- Moss AH, Lunney JR, Culp S, et al. Prognostic significance of the “surprise” question in cancer patients. J Palliat Med. 2010;13(7):837-840.
- Weissman D, Meier C. Identifying patients in need of a palliative care assessment in the hospital setting: a consensus report from the Center to Advance Palliative Care. J Palliat Med. 2011;14(1):17-23.
- Serious illness care resources. Ariadne Labs website. Accessed June 24, 2016.
Although effective palliative care has always been a must-have for patients and caregivers facing serious illness, it hasn’t always been readily available. With the emergence of value-based healthcare models—and their potent incentives to reduce avoidable readmissions—there is renewed hope that such care will be accessible to those who need it.
Palliative and end-of-life care have long been promoted as core skills for hospitalists. The topic has regularly been included at SHM annual meetings and other prominent hospital medicine conferences, in the American Board of Internal Medicine blueprint for recognition of focused practice in hospital medicine, and in a number of influential references for hospitalists. Still, as I look at hospitalist programs around the country, there is a clear need to improve hospitalists’ delivery of palliative and end-of-life care.
Care of patients with chronic illness in their last two years of life accounts for a third of all Medicare spending.1 As hospitalists, we encounter many of these patients as they are hospitalized—and often re-hospitalized. Palliative care, which can improve quality of life and decrease costs for patients while leading to increased satisfaction and better outcomes for caregivers, can help alleviate unneeded and unwanted aggressive interventions like hospitalization.2,3
In its 2014 report, Dying in America, the Institute of Medicine (IOM) identified several areas for improvement, including better advance care planning and payment systems supporting high quality end-of-life care.4 As I write this column in mid 2016, there are two notable achievements since the IOM report: two E&M codes for advance care planning and a substantial and growing number of hospitalist patients in alternative payment models like bundled payments or ACOs.5 I believe we are entering a time when the availability of good palliative care will be accelerated due to broader forces in healthcare that for the first time align incentives between patients’ wishes and how care is paid for.
Palliative Care Skills for Hospitalists
The following are key actions for physicians in addressing palliative care for the hospitalized patient. At the risk of oversimplifying the discipline, I offer a few key actions for hospitalists to keep in mind.
Identify patients who would benefit from palliative care. The surprise question—“Would I be surprised if this patient died in the next year?”—has the ability to predict which patients would benefit from palliative care. In one observation from a group of patients with cancer, a “no” answer identified 60% of patients who died within a year.6 The surprise question has previously been shown to be predictive in other cancer and non-cancer populations.7,8
Weisman and Meier suggest using the following in a checklist at the time of hospital admission as “primary criteria to screen for unmet palliative care needs”:9
- The surprise question
- Frequent admissions
- Admission prompted by difficult-to-control physical or psychological symptoms
- Complex care requirements
- Decline in function, feeding intolerance, or unintended decline in weight
Hold a “goals of care” meeting. A notable step forward for supporting conversations between physicians and patients occurred on Jan. 1, when the Centers for Medicare & Medicaid Services (CMS) announced the Advance Care Planning E&M codes. These are CPT codes 99497 and 99498. They can be used on the same day as other E&M codes and cover discussions regarding advance care planning issues including discussing advance directives, appointing a healthcare proxy or durable power of attorney, discussing a living will, or addressing orders for life-sustaining treatment like the role of hydration or future hospitalizations. (For more information on how to use them, visit the CMS website and search for the FAQ.)
What should hospitalists concentrate on when having “goals of care” conversations with patients and caregivers? Ariadne Labs, a Harvard-affiliated health innovation group, offers the following as elements of a serious illness conversation:10
- Patients’ understanding of their illness
- Patients’ preferences for information and for family involvement
- Personal life goals, fears, and anxieties
- Trade-offs they are willing to accept
For hospitalists, an important area to pay particular attention to is the role of future hospitalizations in patients’ wishes for care, as some patients, if offered appropriate symptom control, would prefer to remain at home.
Two other crucial elements of inpatient palliative care—offer psychosocial support and symptom relief and hand off patient to effective post-hospital palliative care—are outside the scope of this article. However, they should be kept in mind and, of course, applied.
Understand the role of the palliative care consultation. Busy hospitalists might reasonably think, “I simply don’t have time to address palliative care in patients who aren’t likely to die during this hospitalization or soon after.” The palliative care consult service, if available, should be accessed when patients are identified as palliative care candidates but the primary hospitalist does not have the time or resources—including specialized knowledge in some cases—to deliver adequate palliative care. Palliative care specialists can also help bridge the gap between inpatient and outpatient palliative care resources.
In sum, the move to value-based payment models and the new advance care planning E&M codes provide a renewed focus—with more aligned incentives—and the opportunity to provide good palliative care to all who need it.
For hospitalists, identifying those who would benefit from palliative care and working with the healthcare team to ensure the care is delivered are at the heart of our professional mission. TH
References
- End-of-life care. The Darmouth Atlas of Health Care website. Accessed June 23, 2016.
- Gade G, Venohr I, Conner D, et al. Impact of an inpatient palliative care team: a randomized control trial. J Palliat Med. 2008;11(2):180-190.
- Morrison RS, Penrod JD, Cassel JB, et al. Cost savings associated with US hospital palliative care consultation programs. Arch Int Med. 2008;168(16):1783-1790.
- Institute of Medicine. Dying in America: Improving Quality and Honoring Individual Preferences near the End of Life. 2014.
- BPCI Model 2: Retrospective acute & post acute care episode. Centers for Medicare & Medicaid Services website. Accessed June 24, 2016.
- Vick JB, Pertsch N, Hutchings M, et al. The utility of the surprise question in identifying patients most at risk of death. J Clin Oncol. 2015;33(suppl):8.
- Moss AH, Ganjoo J, Sharma S, et al. Utility of the “surprise” question to identify dialysis patients with high mortality. Clin J Am Soc Nephrol. 2008;3:1379-1384.
- Moss AH, Lunney JR, Culp S, et al. Prognostic significance of the “surprise” question in cancer patients. J Palliat Med. 2010;13(7):837-840.
- Weissman D, Meier C. Identifying patients in need of a palliative care assessment in the hospital setting: a consensus report from the Center to Advance Palliative Care. J Palliat Med. 2011;14(1):17-23.
- Serious illness care resources. Ariadne Labs website. Accessed June 24, 2016.
Although effective palliative care has always been a must-have for patients and caregivers facing serious illness, it hasn’t always been readily available. With the emergence of value-based healthcare models—and their potent incentives to reduce avoidable readmissions—there is renewed hope that such care will be accessible to those who need it.
Palliative and end-of-life care have long been promoted as core skills for hospitalists. The topic has regularly been included at SHM annual meetings and other prominent hospital medicine conferences, in the American Board of Internal Medicine blueprint for recognition of focused practice in hospital medicine, and in a number of influential references for hospitalists. Still, as I look at hospitalist programs around the country, there is a clear need to improve hospitalists’ delivery of palliative and end-of-life care.
Care of patients with chronic illness in their last two years of life accounts for a third of all Medicare spending.1 As hospitalists, we encounter many of these patients as they are hospitalized—and often re-hospitalized. Palliative care, which can improve quality of life and decrease costs for patients while leading to increased satisfaction and better outcomes for caregivers, can help alleviate unneeded and unwanted aggressive interventions like hospitalization.2,3
In its 2014 report, Dying in America, the Institute of Medicine (IOM) identified several areas for improvement, including better advance care planning and payment systems supporting high quality end-of-life care.4 As I write this column in mid 2016, there are two notable achievements since the IOM report: two E&M codes for advance care planning and a substantial and growing number of hospitalist patients in alternative payment models like bundled payments or ACOs.5 I believe we are entering a time when the availability of good palliative care will be accelerated due to broader forces in healthcare that for the first time align incentives between patients’ wishes and how care is paid for.
Palliative Care Skills for Hospitalists
The following are key actions for physicians in addressing palliative care for the hospitalized patient. At the risk of oversimplifying the discipline, I offer a few key actions for hospitalists to keep in mind.
Identify patients who would benefit from palliative care. The surprise question—“Would I be surprised if this patient died in the next year?”—has the ability to predict which patients would benefit from palliative care. In one observation from a group of patients with cancer, a “no” answer identified 60% of patients who died within a year.6 The surprise question has previously been shown to be predictive in other cancer and non-cancer populations.7,8
Weisman and Meier suggest using the following in a checklist at the time of hospital admission as “primary criteria to screen for unmet palliative care needs”:9
- The surprise question
- Frequent admissions
- Admission prompted by difficult-to-control physical or psychological symptoms
- Complex care requirements
- Decline in function, feeding intolerance, or unintended decline in weight
Hold a “goals of care” meeting. A notable step forward for supporting conversations between physicians and patients occurred on Jan. 1, when the Centers for Medicare & Medicaid Services (CMS) announced the Advance Care Planning E&M codes. These are CPT codes 99497 and 99498. They can be used on the same day as other E&M codes and cover discussions regarding advance care planning issues including discussing advance directives, appointing a healthcare proxy or durable power of attorney, discussing a living will, or addressing orders for life-sustaining treatment like the role of hydration or future hospitalizations. (For more information on how to use them, visit the CMS website and search for the FAQ.)
What should hospitalists concentrate on when having “goals of care” conversations with patients and caregivers? Ariadne Labs, a Harvard-affiliated health innovation group, offers the following as elements of a serious illness conversation:10
- Patients’ understanding of their illness
- Patients’ preferences for information and for family involvement
- Personal life goals, fears, and anxieties
- Trade-offs they are willing to accept
For hospitalists, an important area to pay particular attention to is the role of future hospitalizations in patients’ wishes for care, as some patients, if offered appropriate symptom control, would prefer to remain at home.
Two other crucial elements of inpatient palliative care—offer psychosocial support and symptom relief and hand off patient to effective post-hospital palliative care—are outside the scope of this article. However, they should be kept in mind and, of course, applied.
Understand the role of the palliative care consultation. Busy hospitalists might reasonably think, “I simply don’t have time to address palliative care in patients who aren’t likely to die during this hospitalization or soon after.” The palliative care consult service, if available, should be accessed when patients are identified as palliative care candidates but the primary hospitalist does not have the time or resources—including specialized knowledge in some cases—to deliver adequate palliative care. Palliative care specialists can also help bridge the gap between inpatient and outpatient palliative care resources.
In sum, the move to value-based payment models and the new advance care planning E&M codes provide a renewed focus—with more aligned incentives—and the opportunity to provide good palliative care to all who need it.
For hospitalists, identifying those who would benefit from palliative care and working with the healthcare team to ensure the care is delivered are at the heart of our professional mission. TH
References
- End-of-life care. The Darmouth Atlas of Health Care website. Accessed June 23, 2016.
- Gade G, Venohr I, Conner D, et al. Impact of an inpatient palliative care team: a randomized control trial. J Palliat Med. 2008;11(2):180-190.
- Morrison RS, Penrod JD, Cassel JB, et al. Cost savings associated with US hospital palliative care consultation programs. Arch Int Med. 2008;168(16):1783-1790.
- Institute of Medicine. Dying in America: Improving Quality and Honoring Individual Preferences near the End of Life. 2014.
- BPCI Model 2: Retrospective acute & post acute care episode. Centers for Medicare & Medicaid Services website. Accessed June 24, 2016.
- Vick JB, Pertsch N, Hutchings M, et al. The utility of the surprise question in identifying patients most at risk of death. J Clin Oncol. 2015;33(suppl):8.
- Moss AH, Ganjoo J, Sharma S, et al. Utility of the “surprise” question to identify dialysis patients with high mortality. Clin J Am Soc Nephrol. 2008;3:1379-1384.
- Moss AH, Lunney JR, Culp S, et al. Prognostic significance of the “surprise” question in cancer patients. J Palliat Med. 2010;13(7):837-840.
- Weissman D, Meier C. Identifying patients in need of a palliative care assessment in the hospital setting: a consensus report from the Center to Advance Palliative Care. J Palliat Med. 2011;14(1):17-23.
- Serious illness care resources. Ariadne Labs website. Accessed June 24, 2016.
8 Lessons for Hospitalists Turned Entrepreneurs
If you are a hospitalist, you are an entrepreneur almost by definition. All hospitalists are continuously engaged in improving the hospital experience for our patients. For some of us, the inner entrepreneur may grow to a point where we seriously consider a part-time or full-time commitment to an entrepreneurial dream. Combining our years of immersion in hospital patient care with an inventive streak can be a potent recipe for an innovative product or service idea.
It may be that the burgeoning startup scene in healthcare has inspired your dream. From coast to coast, there are startup incubators such as Rock Health, Healthbox, Blueprint Health, StartUp Health, Health Wildcatters, The Iron Yard, and TechSpring. These outfits support entrepreneurs with mentorship, funding, workspace, and/or information, such as how to deal with HIPAA or the FDA. Most of us have had at least a passing fascination with Steve Jobs–type characters, individuals who changed the world through their vision and force of will or who just seemed to enjoy a freedom that those who work for “The Man” will never know.
A few years ago, I caught the entrepreneurial bug. Initially, I continued with my day job and worked nights and weekends on my side project. Eventually, I made the leap to work full-time at an early-stage healthcare company. Since then, I’ve spent a lot of time trying to improve my new practice as a full-time entrepreneur, working as hard as ever, trying to be an effective innovator. Every day seems to bring new lessons—some more hard-earned than others—and there’s a lifetime of them still ahead. I’d like to share some of the insights I have learned on this journey. By the way, I still make time for patient care since that remains a priority for me.
Patience Is a Virtue, but Persistence and Positivity Count Even More
As Henry David Thoreau wrote, “Go confidently in the direction of your dreams.” Don’t postpone action indefinitely just because there are obstacles. Stop making excuses, make a start, and build momentum every day. Commit.
Becoming an entrepreneur is a long-term effort fueled by dedication and optimism, but first you have to make a start. You can’t win if you don’t play.
Action and Learning Matter More than Ideation
Start with your idea and a rough plan, but above all, believe in yourself, especially your ability to problem-solve. Many of the qualities that have fueled our success as physicians—precision, thoughtfulness, error aversion, and compulsiveness—might be constraints in a startup environment. Startups are hostile places for perfectionists and those who require complete information before proceeding. Have a bias for action and become comfortable with ambiguity. Entrepreneurs turn little things into big things by making progress every day.
Perhaps contrary to what we learn as physicians, entrepreneurs understand progress is measured more by authentic learning than by getting particular results. Entrepreneurs must quickly learn how to fail. In fact, progress often resembles multiple experiments that allow you to fail (and learn) faster. For entrepreneurs, perfection truly is the enemy of the good.
Learn, make adjustments, and progress will follow.
Guidance Is More Valuable than Money
Commercializing an idea is a challenging proposition. First-timers need advice, support, and help. For advice, find a mentor who has successfully launched a startup. Most of the successful people I know have had the wisdom or good fortune to have a mentor to provide guidance.
Startup incubators can be another source of support. Nearly all large cities and many medium and small cities now have business incubators or accelerators. Attend an event and get involved. They will provide many of the tools you will need to get started.
There are lots of opportunities for innovation in healthcare. But commercializing an idea will be one of the most challenging things you’ll ever do. Surround yourself with people who have skills that complement yours. Physician entrepreneurs need to be part of a viable team.
Sell, Sell, Sell
In business, as in life, “we’re all in sales.” We sell our ideas, our work product, ourselves. Even as physicians we have to sell patients and colleagues on our thought processes to be successful. Successful entrepreneurs are comfortable selling and put their best foot forward when trying to recruit a resource or persuade a potential customer.
Conflicts of Interest
“There is no interest without conflict.” If you look hard enough, you’ll see that we all have conflicts of interest. The key is to recognize them and disclose them. Of course, there are certain conflicts that are deal breakers. They must be avoided. If you remain employed, most of them are spelled out in your employer’s conflict of interest and intellectual property policies.
HIPAA Is an Innovation Killer
If your idea involves technology or services that address protected health information, become a HIPAA savant as soon as possible. The good news is that if you can effectively navigate the HIPAA challenge, you will have an advantage over your competitors.
Pure ‘Tech’ Plays Are Difficult
If you want to try to build the next killer app for healthcare and hope it will go viral, good luck. Based on my experience, it is difficult to get market traction with a pure technology offering. The strategy with a higher likelihood of success is to provide services with a technology platform that supports those services. As a provider of a service, you can provide immediate value to the customer and become “sticky” as you build your business (and software).
Enjoy the Journey, No Matter What
At first, you will be propelled by irrational exuberance and a passion for the greatness of your idea. That’s not only a good thing, it’s a requirement. But becoming a successful entrepreneur is a heavy haul down a long road of hard work and execution. Enjoying the journey is crucial since, beyond that, there are no guarantees. But life is short, so maybe you also value a career with no regrets. Take a chance and enjoy the ride.
Being a physician entrepreneur is not for everyone. But for those who take the plunge, it can be one of the most fulfilling, exciting, and meaningful journeys one could imagine. TH
Author note: I’d like to thank Dr. Jason Stein and Joe Miller for their helpful comments on this column.

If you are a hospitalist, you are an entrepreneur almost by definition. All hospitalists are continuously engaged in improving the hospital experience for our patients. For some of us, the inner entrepreneur may grow to a point where we seriously consider a part-time or full-time commitment to an entrepreneurial dream. Combining our years of immersion in hospital patient care with an inventive streak can be a potent recipe for an innovative product or service idea.
It may be that the burgeoning startup scene in healthcare has inspired your dream. From coast to coast, there are startup incubators such as Rock Health, Healthbox, Blueprint Health, StartUp Health, Health Wildcatters, The Iron Yard, and TechSpring. These outfits support entrepreneurs with mentorship, funding, workspace, and/or information, such as how to deal with HIPAA or the FDA. Most of us have had at least a passing fascination with Steve Jobs–type characters, individuals who changed the world through their vision and force of will or who just seemed to enjoy a freedom that those who work for “The Man” will never know.
A few years ago, I caught the entrepreneurial bug. Initially, I continued with my day job and worked nights and weekends on my side project. Eventually, I made the leap to work full-time at an early-stage healthcare company. Since then, I’ve spent a lot of time trying to improve my new practice as a full-time entrepreneur, working as hard as ever, trying to be an effective innovator. Every day seems to bring new lessons—some more hard-earned than others—and there’s a lifetime of them still ahead. I’d like to share some of the insights I have learned on this journey. By the way, I still make time for patient care since that remains a priority for me.
Patience Is a Virtue, but Persistence and Positivity Count Even More
As Henry David Thoreau wrote, “Go confidently in the direction of your dreams.” Don’t postpone action indefinitely just because there are obstacles. Stop making excuses, make a start, and build momentum every day. Commit.
Becoming an entrepreneur is a long-term effort fueled by dedication and optimism, but first you have to make a start. You can’t win if you don’t play.
Action and Learning Matter More than Ideation
Start with your idea and a rough plan, but above all, believe in yourself, especially your ability to problem-solve. Many of the qualities that have fueled our success as physicians—precision, thoughtfulness, error aversion, and compulsiveness—might be constraints in a startup environment. Startups are hostile places for perfectionists and those who require complete information before proceeding. Have a bias for action and become comfortable with ambiguity. Entrepreneurs turn little things into big things by making progress every day.
Perhaps contrary to what we learn as physicians, entrepreneurs understand progress is measured more by authentic learning than by getting particular results. Entrepreneurs must quickly learn how to fail. In fact, progress often resembles multiple experiments that allow you to fail (and learn) faster. For entrepreneurs, perfection truly is the enemy of the good.
Learn, make adjustments, and progress will follow.
Guidance Is More Valuable than Money
Commercializing an idea is a challenging proposition. First-timers need advice, support, and help. For advice, find a mentor who has successfully launched a startup. Most of the successful people I know have had the wisdom or good fortune to have a mentor to provide guidance.
Startup incubators can be another source of support. Nearly all large cities and many medium and small cities now have business incubators or accelerators. Attend an event and get involved. They will provide many of the tools you will need to get started.
There are lots of opportunities for innovation in healthcare. But commercializing an idea will be one of the most challenging things you’ll ever do. Surround yourself with people who have skills that complement yours. Physician entrepreneurs need to be part of a viable team.
Sell, Sell, Sell
In business, as in life, “we’re all in sales.” We sell our ideas, our work product, ourselves. Even as physicians we have to sell patients and colleagues on our thought processes to be successful. Successful entrepreneurs are comfortable selling and put their best foot forward when trying to recruit a resource or persuade a potential customer.
Conflicts of Interest
“There is no interest without conflict.” If you look hard enough, you’ll see that we all have conflicts of interest. The key is to recognize them and disclose them. Of course, there are certain conflicts that are deal breakers. They must be avoided. If you remain employed, most of them are spelled out in your employer’s conflict of interest and intellectual property policies.
HIPAA Is an Innovation Killer
If your idea involves technology or services that address protected health information, become a HIPAA savant as soon as possible. The good news is that if you can effectively navigate the HIPAA challenge, you will have an advantage over your competitors.
Pure ‘Tech’ Plays Are Difficult
If you want to try to build the next killer app for healthcare and hope it will go viral, good luck. Based on my experience, it is difficult to get market traction with a pure technology offering. The strategy with a higher likelihood of success is to provide services with a technology platform that supports those services. As a provider of a service, you can provide immediate value to the customer and become “sticky” as you build your business (and software).
Enjoy the Journey, No Matter What
At first, you will be propelled by irrational exuberance and a passion for the greatness of your idea. That’s not only a good thing, it’s a requirement. But becoming a successful entrepreneur is a heavy haul down a long road of hard work and execution. Enjoying the journey is crucial since, beyond that, there are no guarantees. But life is short, so maybe you also value a career with no regrets. Take a chance and enjoy the ride.
Being a physician entrepreneur is not for everyone. But for those who take the plunge, it can be one of the most fulfilling, exciting, and meaningful journeys one could imagine. TH
Author note: I’d like to thank Dr. Jason Stein and Joe Miller for their helpful comments on this column.

If you are a hospitalist, you are an entrepreneur almost by definition. All hospitalists are continuously engaged in improving the hospital experience for our patients. For some of us, the inner entrepreneur may grow to a point where we seriously consider a part-time or full-time commitment to an entrepreneurial dream. Combining our years of immersion in hospital patient care with an inventive streak can be a potent recipe for an innovative product or service idea.
It may be that the burgeoning startup scene in healthcare has inspired your dream. From coast to coast, there are startup incubators such as Rock Health, Healthbox, Blueprint Health, StartUp Health, Health Wildcatters, The Iron Yard, and TechSpring. These outfits support entrepreneurs with mentorship, funding, workspace, and/or information, such as how to deal with HIPAA or the FDA. Most of us have had at least a passing fascination with Steve Jobs–type characters, individuals who changed the world through their vision and force of will or who just seemed to enjoy a freedom that those who work for “The Man” will never know.
A few years ago, I caught the entrepreneurial bug. Initially, I continued with my day job and worked nights and weekends on my side project. Eventually, I made the leap to work full-time at an early-stage healthcare company. Since then, I’ve spent a lot of time trying to improve my new practice as a full-time entrepreneur, working as hard as ever, trying to be an effective innovator. Every day seems to bring new lessons—some more hard-earned than others—and there’s a lifetime of them still ahead. I’d like to share some of the insights I have learned on this journey. By the way, I still make time for patient care since that remains a priority for me.
Patience Is a Virtue, but Persistence and Positivity Count Even More
As Henry David Thoreau wrote, “Go confidently in the direction of your dreams.” Don’t postpone action indefinitely just because there are obstacles. Stop making excuses, make a start, and build momentum every day. Commit.
Becoming an entrepreneur is a long-term effort fueled by dedication and optimism, but first you have to make a start. You can’t win if you don’t play.
Action and Learning Matter More than Ideation
Start with your idea and a rough plan, but above all, believe in yourself, especially your ability to problem-solve. Many of the qualities that have fueled our success as physicians—precision, thoughtfulness, error aversion, and compulsiveness—might be constraints in a startup environment. Startups are hostile places for perfectionists and those who require complete information before proceeding. Have a bias for action and become comfortable with ambiguity. Entrepreneurs turn little things into big things by making progress every day.
Perhaps contrary to what we learn as physicians, entrepreneurs understand progress is measured more by authentic learning than by getting particular results. Entrepreneurs must quickly learn how to fail. In fact, progress often resembles multiple experiments that allow you to fail (and learn) faster. For entrepreneurs, perfection truly is the enemy of the good.
Learn, make adjustments, and progress will follow.
Guidance Is More Valuable than Money
Commercializing an idea is a challenging proposition. First-timers need advice, support, and help. For advice, find a mentor who has successfully launched a startup. Most of the successful people I know have had the wisdom or good fortune to have a mentor to provide guidance.
Startup incubators can be another source of support. Nearly all large cities and many medium and small cities now have business incubators or accelerators. Attend an event and get involved. They will provide many of the tools you will need to get started.
There are lots of opportunities for innovation in healthcare. But commercializing an idea will be one of the most challenging things you’ll ever do. Surround yourself with people who have skills that complement yours. Physician entrepreneurs need to be part of a viable team.
Sell, Sell, Sell
In business, as in life, “we’re all in sales.” We sell our ideas, our work product, ourselves. Even as physicians we have to sell patients and colleagues on our thought processes to be successful. Successful entrepreneurs are comfortable selling and put their best foot forward when trying to recruit a resource or persuade a potential customer.
Conflicts of Interest
“There is no interest without conflict.” If you look hard enough, you’ll see that we all have conflicts of interest. The key is to recognize them and disclose them. Of course, there are certain conflicts that are deal breakers. They must be avoided. If you remain employed, most of them are spelled out in your employer’s conflict of interest and intellectual property policies.
HIPAA Is an Innovation Killer
If your idea involves technology or services that address protected health information, become a HIPAA savant as soon as possible. The good news is that if you can effectively navigate the HIPAA challenge, you will have an advantage over your competitors.
Pure ‘Tech’ Plays Are Difficult
If you want to try to build the next killer app for healthcare and hope it will go viral, good luck. Based on my experience, it is difficult to get market traction with a pure technology offering. The strategy with a higher likelihood of success is to provide services with a technology platform that supports those services. As a provider of a service, you can provide immediate value to the customer and become “sticky” as you build your business (and software).
Enjoy the Journey, No Matter What
At first, you will be propelled by irrational exuberance and a passion for the greatness of your idea. That’s not only a good thing, it’s a requirement. But becoming a successful entrepreneur is a heavy haul down a long road of hard work and execution. Enjoying the journey is crucial since, beyond that, there are no guarantees. But life is short, so maybe you also value a career with no regrets. Take a chance and enjoy the ride.
Being a physician entrepreneur is not for everyone. But for those who take the plunge, it can be one of the most fulfilling, exciting, and meaningful journeys one could imagine. TH
Author note: I’d like to thank Dr. Jason Stein and Joe Miller for their helpful comments on this column.

Revisiting the ‘Key Principles and Characteristics of an Effective Hospital Medicine Group'
It has been two years since the “Key Characteristics” was published in the Journal of Hospital Medicine.1 The SHM board of directors envisions the Key Characteristics as a tool to improve the performance of hospital medicine groups (HMGs) and “raise the bar” for the specialty.
At SHM’s annual meeting (www.hospitalmedicine2016.org) next month in San Diego, the Key Characteristics will provide the framework for the Practice Management Pre-Course (Sunday, March 6). The pre-course faculty, of which I am a member, will address all 10 principles of the Key Characteristics (see Table 1), including case studies and practical ideas for performance improvement. As a preview, I will cover Principle 6 and provide a few practical tips that you can implement in your practice.
For a more comprehensive discussion of all the Key Characteristics and how to use them, visit the SHM website (visit www.hospitalmedicine.org, then click on the “Practice Management” icon at the top of the landing page).
Characteristic 6.1
The HMG has systems in place to ensure effective and reliable communication with the patient’s primary care physician and/or other provider(s) involved in the patient’s care in the non-acute-care setting.
Practical tip: Your practice probably has administrative procedures in place to notify PCPs that their patient has been admitted to the hospital, using the electronic health record or secure email, if available, or messaging by fax/phone. But are you receiving vital information from the PCP’s office or from the nursing facility? Establish a protocol for obtaining key history, medication, and diagnostic testing information from these sources. One approach is to request this information when notifying the PCP of the patient’s admission.
Practical tip: Use the “grocery store test” to determine when to contact the PCP during the hospital stay. For example, if the PCP were to run into a family member of the patient in the grocery store, would the PCP want to have learned of a change in the patient’s condition in advance of the family member encounter?
Practical tip: Because reaching skilling nursing facility (SNF) physicians/providers (SNFists) can be challenging, hold an annual social event so that they can meet the hospitalists in your practice face-to-face. At the event, exchange cellphone or beeper numbers with the SNFists, and establish an explicit understanding of how handoffs will occur, especially for high-risk patients.
Characteristic 6.2
The HMG contributes in meaningful ways to the hospital’s efforts to improve care transitions.
Because of readmissions penalties, every hospital in the country is concerned with care transitions and avoiding readmissions. But HMGs want to know which interventions reliably decrease readmissions. The Commonwealth Fund recently released the results of a study of 428 hospitals that participated in national efforts to reduce readmissions, including the State Action on Avoidable Rehospitalizations (STAAR) and Hospital to Home (H2H) initiatives. The study’s primary conclusions were as follows:
- The only strategy consistently associated with reduced risk-standardized readmissions was discharging patients with their appointments already made.2 No other single strategy was reliably associated with a reduction.
- Hospitals that implemented three or more readmission reduction strategies showed a significant decrease in risk-standardized readmissions versus those implementing fewer than three.
Practical tip: Ensure patients leave the hospital with a PCP follow-up appointment made and in hand.
Practical tip: Work with your hospital on at least three definitive strategies to reduce readmissions.
Implement to Improve Your HMG
The basic and updated 2015 versions of the “Key Principles and Characteristics of an Effective Hospital Medicine Group” can be downloaded from the SHM website (visit www.hospitalmedicine.org, then click on the “Practice Management” icon at the top of the landing page). The updated 2015 version provides definitions and requirements and suggested approaches to demonstrating the characteristic that enables the HMG to conduct a comprehensive self-assessment.
In addition, there is a new tool intended for use by hospitalist practice administrators that cross-references the Key Characteristics with another tool, The Core Competencies for a Hospitalist Practice Administrator. TH

References
- Cawley P, Deitelzweig S, Flores L, et al. The key principles and characteristics of an effective hospital medicine group: an assessment guide for hospitals and hospitalists. J Hosp Med. 2014;9(2):123-128.
- Bradley EH, Brewster A, Curry L. National campaigns to reduce readmissions: what have we learned? The Commonwealth Fund website. Available at: commonwealthfund.org/publications/blog/2015/oct/national-campaigns-to-reduce-readmissions. Accessed December 28, 2015.
It has been two years since the “Key Characteristics” was published in the Journal of Hospital Medicine.1 The SHM board of directors envisions the Key Characteristics as a tool to improve the performance of hospital medicine groups (HMGs) and “raise the bar” for the specialty.
At SHM’s annual meeting (www.hospitalmedicine2016.org) next month in San Diego, the Key Characteristics will provide the framework for the Practice Management Pre-Course (Sunday, March 6). The pre-course faculty, of which I am a member, will address all 10 principles of the Key Characteristics (see Table 1), including case studies and practical ideas for performance improvement. As a preview, I will cover Principle 6 and provide a few practical tips that you can implement in your practice.
For a more comprehensive discussion of all the Key Characteristics and how to use them, visit the SHM website (visit www.hospitalmedicine.org, then click on the “Practice Management” icon at the top of the landing page).
Characteristic 6.1
The HMG has systems in place to ensure effective and reliable communication with the patient’s primary care physician and/or other provider(s) involved in the patient’s care in the non-acute-care setting.
Practical tip: Your practice probably has administrative procedures in place to notify PCPs that their patient has been admitted to the hospital, using the electronic health record or secure email, if available, or messaging by fax/phone. But are you receiving vital information from the PCP’s office or from the nursing facility? Establish a protocol for obtaining key history, medication, and diagnostic testing information from these sources. One approach is to request this information when notifying the PCP of the patient’s admission.
Practical tip: Use the “grocery store test” to determine when to contact the PCP during the hospital stay. For example, if the PCP were to run into a family member of the patient in the grocery store, would the PCP want to have learned of a change in the patient’s condition in advance of the family member encounter?
Practical tip: Because reaching skilling nursing facility (SNF) physicians/providers (SNFists) can be challenging, hold an annual social event so that they can meet the hospitalists in your practice face-to-face. At the event, exchange cellphone or beeper numbers with the SNFists, and establish an explicit understanding of how handoffs will occur, especially for high-risk patients.
Characteristic 6.2
The HMG contributes in meaningful ways to the hospital’s efforts to improve care transitions.
Because of readmissions penalties, every hospital in the country is concerned with care transitions and avoiding readmissions. But HMGs want to know which interventions reliably decrease readmissions. The Commonwealth Fund recently released the results of a study of 428 hospitals that participated in national efforts to reduce readmissions, including the State Action on Avoidable Rehospitalizations (STAAR) and Hospital to Home (H2H) initiatives. The study’s primary conclusions were as follows:
- The only strategy consistently associated with reduced risk-standardized readmissions was discharging patients with their appointments already made.2 No other single strategy was reliably associated with a reduction.
- Hospitals that implemented three or more readmission reduction strategies showed a significant decrease in risk-standardized readmissions versus those implementing fewer than three.
Practical tip: Ensure patients leave the hospital with a PCP follow-up appointment made and in hand.
Practical tip: Work with your hospital on at least three definitive strategies to reduce readmissions.
Implement to Improve Your HMG
The basic and updated 2015 versions of the “Key Principles and Characteristics of an Effective Hospital Medicine Group” can be downloaded from the SHM website (visit www.hospitalmedicine.org, then click on the “Practice Management” icon at the top of the landing page). The updated 2015 version provides definitions and requirements and suggested approaches to demonstrating the characteristic that enables the HMG to conduct a comprehensive self-assessment.
In addition, there is a new tool intended for use by hospitalist practice administrators that cross-references the Key Characteristics with another tool, The Core Competencies for a Hospitalist Practice Administrator. TH

References
- Cawley P, Deitelzweig S, Flores L, et al. The key principles and characteristics of an effective hospital medicine group: an assessment guide for hospitals and hospitalists. J Hosp Med. 2014;9(2):123-128.
- Bradley EH, Brewster A, Curry L. National campaigns to reduce readmissions: what have we learned? The Commonwealth Fund website. Available at: commonwealthfund.org/publications/blog/2015/oct/national-campaigns-to-reduce-readmissions. Accessed December 28, 2015.
It has been two years since the “Key Characteristics” was published in the Journal of Hospital Medicine.1 The SHM board of directors envisions the Key Characteristics as a tool to improve the performance of hospital medicine groups (HMGs) and “raise the bar” for the specialty.
At SHM’s annual meeting (www.hospitalmedicine2016.org) next month in San Diego, the Key Characteristics will provide the framework for the Practice Management Pre-Course (Sunday, March 6). The pre-course faculty, of which I am a member, will address all 10 principles of the Key Characteristics (see Table 1), including case studies and practical ideas for performance improvement. As a preview, I will cover Principle 6 and provide a few practical tips that you can implement in your practice.
For a more comprehensive discussion of all the Key Characteristics and how to use them, visit the SHM website (visit www.hospitalmedicine.org, then click on the “Practice Management” icon at the top of the landing page).
Characteristic 6.1
The HMG has systems in place to ensure effective and reliable communication with the patient’s primary care physician and/or other provider(s) involved in the patient’s care in the non-acute-care setting.
Practical tip: Your practice probably has administrative procedures in place to notify PCPs that their patient has been admitted to the hospital, using the electronic health record or secure email, if available, or messaging by fax/phone. But are you receiving vital information from the PCP’s office or from the nursing facility? Establish a protocol for obtaining key history, medication, and diagnostic testing information from these sources. One approach is to request this information when notifying the PCP of the patient’s admission.
Practical tip: Use the “grocery store test” to determine when to contact the PCP during the hospital stay. For example, if the PCP were to run into a family member of the patient in the grocery store, would the PCP want to have learned of a change in the patient’s condition in advance of the family member encounter?
Practical tip: Because reaching skilling nursing facility (SNF) physicians/providers (SNFists) can be challenging, hold an annual social event so that they can meet the hospitalists in your practice face-to-face. At the event, exchange cellphone or beeper numbers with the SNFists, and establish an explicit understanding of how handoffs will occur, especially for high-risk patients.
Characteristic 6.2
The HMG contributes in meaningful ways to the hospital’s efforts to improve care transitions.
Because of readmissions penalties, every hospital in the country is concerned with care transitions and avoiding readmissions. But HMGs want to know which interventions reliably decrease readmissions. The Commonwealth Fund recently released the results of a study of 428 hospitals that participated in national efforts to reduce readmissions, including the State Action on Avoidable Rehospitalizations (STAAR) and Hospital to Home (H2H) initiatives. The study’s primary conclusions were as follows:
- The only strategy consistently associated with reduced risk-standardized readmissions was discharging patients with their appointments already made.2 No other single strategy was reliably associated with a reduction.
- Hospitals that implemented three or more readmission reduction strategies showed a significant decrease in risk-standardized readmissions versus those implementing fewer than three.
Practical tip: Ensure patients leave the hospital with a PCP follow-up appointment made and in hand.
Practical tip: Work with your hospital on at least three definitive strategies to reduce readmissions.
Implement to Improve Your HMG
The basic and updated 2015 versions of the “Key Principles and Characteristics of an Effective Hospital Medicine Group” can be downloaded from the SHM website (visit www.hospitalmedicine.org, then click on the “Practice Management” icon at the top of the landing page). The updated 2015 version provides definitions and requirements and suggested approaches to demonstrating the characteristic that enables the HMG to conduct a comprehensive self-assessment.
In addition, there is a new tool intended for use by hospitalist practice administrators that cross-references the Key Characteristics with another tool, The Core Competencies for a Hospitalist Practice Administrator. TH

References
- Cawley P, Deitelzweig S, Flores L, et al. The key principles and characteristics of an effective hospital medicine group: an assessment guide for hospitals and hospitalists. J Hosp Med. 2014;9(2):123-128.
- Bradley EH, Brewster A, Curry L. National campaigns to reduce readmissions: what have we learned? The Commonwealth Fund website. Available at: commonwealthfund.org/publications/blog/2015/oct/national-campaigns-to-reduce-readmissions. Accessed December 28, 2015.
Early Mobility Program
“I didn’t get out of bed for 10 days”
—Anonymous patient admitted to a skilled nursing facility post-hospitalization for a COPD exacerbation
Readmission penalties, “Medicare spending per beneficiary” under value-based purchasing, and the move to accountable care are propelling hospitalists to do more to ensure our patients recover well in the least restrictive setting, without returning to the hospital. As we build systems to support patient recovery, we are focused on a medical model, paying attention to managing diseases and reconciling medications. At the same time, there is a growing awareness that functional status and mobility are critical pieces of patient care during and post-hospitalization.
Regardless of principal diagnosis and comorbidities, patients’ functional mobility ultimately determines their trajectory during recovery. To illustrate the importance of functional status and outcomes, one study showed that models predicting readmission based on functional measures outperformed those based on comorbidities.1
The negative effects of hospitalization on patient mobility, and in turn, on recovery, have been recognized for a long time. Immobility is associated with functional decline, which contributes to falls, increased length of stay, delirium, loss of ability to perform activities of daily living, and loss of ambulatory independence. A number of studies have reported successful early mobility programs in critical care and surgical patients.2 Fewer have been reported in general medical patients.3 Taken together, they suggest that a program for mobilizing patients, using a team approach, is an important part of recovery during and after hospitalization.
The purpose of this column is to report the components of one healthcare system’s mobility program for general medical-surgical patients.
Early Mobility: A Case Study
St Luke’s University Health Network (SLUHN) in northeastern Pennsylvania has implemented an early mobility program as part of its broader strategy to reduce readmissions and discharge as many patients home as possible. Although the SLUHN early mobility program depends on nursing, nursing assistants, and the judicious use of therapists, physician leadership during implementation and maintenance of the program has been essential. Moreover, because the program represents a culture shift, especially for nursing, leadership and change management are crucial ingredients for success. Below are the key steps in the SLUHN early mobility program.
Establish baseline functional status. Recording baseline function is an essential first step. For patients admitted through the ED, nurses collect ambulatory status, patient needs for assistance, ambulatory aids/special equipment, and history of falls. They populate an SBAR (situation, background, assessment, recommendation) form with this information and, as part of the handoff, ensure that it is transmitted to the inpatient nurse receiving the patient.
Obtain and document Barthel Index score. SLUHN uses the Barthel Index (see Figure 1) to establish a patient’s degree of independence and need for supervision. The index is scored on a 0-100 scale, with a higher score corresponding to a greater degree of independence. SLUHN created three categories: 0-59, stage 1; 60-84, stage 2; 85-100, stage 3.
Patient mobility plan. Based on the Barthel-derived stage, a patient is assigned a mobility plan.
The role of nursing. The patient’s registered nurse is responsible for implementing the “patient mobility plan.” The nurse initiates an “interdisciplinary plan of care,” in which the mobility stage is written on the SBAR handoff report tool. The report is discussed at change of shift and at multidisciplinary rounds. Nursing also communicates the mobility plan to the nursing assistants and assigns responsibilities for the mobility plan (activities of daily living, out of bed, ambulation, and so on), including verifying documentation of daily activities and assessing the patient’s response to the activity level of the assigned stage.
Further, nursing maintains and revises the mobility status on the SBAR, updates progress toward outcomes on the care plan, consults with the physician and team regarding the discharge plan, and discusses progress with the patient and family.
The role of the nursing/patient care assistant. The nursing assistant is responsible for implementing elements of the plan, such as activities of daily living, getting out of bed, and ambulation, under the guidance of the nurse. The nursing assistant reports patient responses to activity level and reflects mobility goals back to the patient verbally and through white board messaging.
Patient progress in mobility. When a patient sustains progress at one stage for 24 hours, the nurse aims to move the patient to the next stage by reevaluating the Barthel Index and going through the same steps as those followed during the initial scoring. The process moves the patient to higher activity levels, unless there are intervening problems affecting mobility.
In such cases, according to the Barthel Index, the patient may remain at the same—or be moved to a lower—activity level. In practice, patients are assessed each shift, and those with higher function (stage 3) are progressed to unsupervised ambulation.
The role of physical and occupational therapy. Although the role of physical and occupational therapists in the SLUHN mobility program is well codified, it is reserved for patients with complex rehabilitation needs due to the number of patients requiring rehabilitation.
In sum, this patient mobility program–for non-ICU hospitalized patients–relies on:
- Documentation of baseline function;
- Independent scoring using the Barthel Index;
- Creation of clear roles for nursing, nursing assistants, and therapists; and
- Reevaluation of patients at regular intervals based on the Barthel Index, so that they may progress to greater activity levels (or to lower levels in the case of a setback).
A key subsequent step, an evaluation of the program’s performance in terms of readmissions, transfer rates to a skilled nursing facility, and skilled facility length of stay, has shown positive results in all three domains.


References
- Shi SL, Girrard P, Goldstein R, et al. Functional status outperforms comorbidities in predicting acute care readmissions in medically complex patients. J Gen Intern Med. 2015;30(11):1688-1695.
- Dammeyer JA, Baldwin N, Packard D, et al. Mobilizing outcomes: implementation of a nurse-led multidisciplinary mobility program. Crit Care Nurs Q. 2013;36(1):109-119.
- Wood W, Tschannen D, Trotsky A, et al. A mobility program for an inpatient acute care medical unit. Am J Nurs. 2014;114(10):34-40.
- Mahoney FI, Barthel DW. Functional evaluation: the Barthel Index. Md State Med J. 1965;14:61-65.
“I didn’t get out of bed for 10 days”
—Anonymous patient admitted to a skilled nursing facility post-hospitalization for a COPD exacerbation
Readmission penalties, “Medicare spending per beneficiary” under value-based purchasing, and the move to accountable care are propelling hospitalists to do more to ensure our patients recover well in the least restrictive setting, without returning to the hospital. As we build systems to support patient recovery, we are focused on a medical model, paying attention to managing diseases and reconciling medications. At the same time, there is a growing awareness that functional status and mobility are critical pieces of patient care during and post-hospitalization.
Regardless of principal diagnosis and comorbidities, patients’ functional mobility ultimately determines their trajectory during recovery. To illustrate the importance of functional status and outcomes, one study showed that models predicting readmission based on functional measures outperformed those based on comorbidities.1
The negative effects of hospitalization on patient mobility, and in turn, on recovery, have been recognized for a long time. Immobility is associated with functional decline, which contributes to falls, increased length of stay, delirium, loss of ability to perform activities of daily living, and loss of ambulatory independence. A number of studies have reported successful early mobility programs in critical care and surgical patients.2 Fewer have been reported in general medical patients.3 Taken together, they suggest that a program for mobilizing patients, using a team approach, is an important part of recovery during and after hospitalization.
The purpose of this column is to report the components of one healthcare system’s mobility program for general medical-surgical patients.
Early Mobility: A Case Study
St Luke’s University Health Network (SLUHN) in northeastern Pennsylvania has implemented an early mobility program as part of its broader strategy to reduce readmissions and discharge as many patients home as possible. Although the SLUHN early mobility program depends on nursing, nursing assistants, and the judicious use of therapists, physician leadership during implementation and maintenance of the program has been essential. Moreover, because the program represents a culture shift, especially for nursing, leadership and change management are crucial ingredients for success. Below are the key steps in the SLUHN early mobility program.
Establish baseline functional status. Recording baseline function is an essential first step. For patients admitted through the ED, nurses collect ambulatory status, patient needs for assistance, ambulatory aids/special equipment, and history of falls. They populate an SBAR (situation, background, assessment, recommendation) form with this information and, as part of the handoff, ensure that it is transmitted to the inpatient nurse receiving the patient.
Obtain and document Barthel Index score. SLUHN uses the Barthel Index (see Figure 1) to establish a patient’s degree of independence and need for supervision. The index is scored on a 0-100 scale, with a higher score corresponding to a greater degree of independence. SLUHN created three categories: 0-59, stage 1; 60-84, stage 2; 85-100, stage 3.
Patient mobility plan. Based on the Barthel-derived stage, a patient is assigned a mobility plan.
The role of nursing. The patient’s registered nurse is responsible for implementing the “patient mobility plan.” The nurse initiates an “interdisciplinary plan of care,” in which the mobility stage is written on the SBAR handoff report tool. The report is discussed at change of shift and at multidisciplinary rounds. Nursing also communicates the mobility plan to the nursing assistants and assigns responsibilities for the mobility plan (activities of daily living, out of bed, ambulation, and so on), including verifying documentation of daily activities and assessing the patient’s response to the activity level of the assigned stage.
Further, nursing maintains and revises the mobility status on the SBAR, updates progress toward outcomes on the care plan, consults with the physician and team regarding the discharge plan, and discusses progress with the patient and family.
The role of the nursing/patient care assistant. The nursing assistant is responsible for implementing elements of the plan, such as activities of daily living, getting out of bed, and ambulation, under the guidance of the nurse. The nursing assistant reports patient responses to activity level and reflects mobility goals back to the patient verbally and through white board messaging.
Patient progress in mobility. When a patient sustains progress at one stage for 24 hours, the nurse aims to move the patient to the next stage by reevaluating the Barthel Index and going through the same steps as those followed during the initial scoring. The process moves the patient to higher activity levels, unless there are intervening problems affecting mobility.
In such cases, according to the Barthel Index, the patient may remain at the same—or be moved to a lower—activity level. In practice, patients are assessed each shift, and those with higher function (stage 3) are progressed to unsupervised ambulation.
The role of physical and occupational therapy. Although the role of physical and occupational therapists in the SLUHN mobility program is well codified, it is reserved for patients with complex rehabilitation needs due to the number of patients requiring rehabilitation.
In sum, this patient mobility program–for non-ICU hospitalized patients–relies on:
- Documentation of baseline function;
- Independent scoring using the Barthel Index;
- Creation of clear roles for nursing, nursing assistants, and therapists; and
- Reevaluation of patients at regular intervals based on the Barthel Index, so that they may progress to greater activity levels (or to lower levels in the case of a setback).
A key subsequent step, an evaluation of the program’s performance in terms of readmissions, transfer rates to a skilled nursing facility, and skilled facility length of stay, has shown positive results in all three domains.


References
- Shi SL, Girrard P, Goldstein R, et al. Functional status outperforms comorbidities in predicting acute care readmissions in medically complex patients. J Gen Intern Med. 2015;30(11):1688-1695.
- Dammeyer JA, Baldwin N, Packard D, et al. Mobilizing outcomes: implementation of a nurse-led multidisciplinary mobility program. Crit Care Nurs Q. 2013;36(1):109-119.
- Wood W, Tschannen D, Trotsky A, et al. A mobility program for an inpatient acute care medical unit. Am J Nurs. 2014;114(10):34-40.
- Mahoney FI, Barthel DW. Functional evaluation: the Barthel Index. Md State Med J. 1965;14:61-65.
“I didn’t get out of bed for 10 days”
—Anonymous patient admitted to a skilled nursing facility post-hospitalization for a COPD exacerbation
Readmission penalties, “Medicare spending per beneficiary” under value-based purchasing, and the move to accountable care are propelling hospitalists to do more to ensure our patients recover well in the least restrictive setting, without returning to the hospital. As we build systems to support patient recovery, we are focused on a medical model, paying attention to managing diseases and reconciling medications. At the same time, there is a growing awareness that functional status and mobility are critical pieces of patient care during and post-hospitalization.
Regardless of principal diagnosis and comorbidities, patients’ functional mobility ultimately determines their trajectory during recovery. To illustrate the importance of functional status and outcomes, one study showed that models predicting readmission based on functional measures outperformed those based on comorbidities.1
The negative effects of hospitalization on patient mobility, and in turn, on recovery, have been recognized for a long time. Immobility is associated with functional decline, which contributes to falls, increased length of stay, delirium, loss of ability to perform activities of daily living, and loss of ambulatory independence. A number of studies have reported successful early mobility programs in critical care and surgical patients.2 Fewer have been reported in general medical patients.3 Taken together, they suggest that a program for mobilizing patients, using a team approach, is an important part of recovery during and after hospitalization.
The purpose of this column is to report the components of one healthcare system’s mobility program for general medical-surgical patients.
Early Mobility: A Case Study
St Luke’s University Health Network (SLUHN) in northeastern Pennsylvania has implemented an early mobility program as part of its broader strategy to reduce readmissions and discharge as many patients home as possible. Although the SLUHN early mobility program depends on nursing, nursing assistants, and the judicious use of therapists, physician leadership during implementation and maintenance of the program has been essential. Moreover, because the program represents a culture shift, especially for nursing, leadership and change management are crucial ingredients for success. Below are the key steps in the SLUHN early mobility program.
Establish baseline functional status. Recording baseline function is an essential first step. For patients admitted through the ED, nurses collect ambulatory status, patient needs for assistance, ambulatory aids/special equipment, and history of falls. They populate an SBAR (situation, background, assessment, recommendation) form with this information and, as part of the handoff, ensure that it is transmitted to the inpatient nurse receiving the patient.
Obtain and document Barthel Index score. SLUHN uses the Barthel Index (see Figure 1) to establish a patient’s degree of independence and need for supervision. The index is scored on a 0-100 scale, with a higher score corresponding to a greater degree of independence. SLUHN created three categories: 0-59, stage 1; 60-84, stage 2; 85-100, stage 3.
Patient mobility plan. Based on the Barthel-derived stage, a patient is assigned a mobility plan.
The role of nursing. The patient’s registered nurse is responsible for implementing the “patient mobility plan.” The nurse initiates an “interdisciplinary plan of care,” in which the mobility stage is written on the SBAR handoff report tool. The report is discussed at change of shift and at multidisciplinary rounds. Nursing also communicates the mobility plan to the nursing assistants and assigns responsibilities for the mobility plan (activities of daily living, out of bed, ambulation, and so on), including verifying documentation of daily activities and assessing the patient’s response to the activity level of the assigned stage.
Further, nursing maintains and revises the mobility status on the SBAR, updates progress toward outcomes on the care plan, consults with the physician and team regarding the discharge plan, and discusses progress with the patient and family.
The role of the nursing/patient care assistant. The nursing assistant is responsible for implementing elements of the plan, such as activities of daily living, getting out of bed, and ambulation, under the guidance of the nurse. The nursing assistant reports patient responses to activity level and reflects mobility goals back to the patient verbally and through white board messaging.
Patient progress in mobility. When a patient sustains progress at one stage for 24 hours, the nurse aims to move the patient to the next stage by reevaluating the Barthel Index and going through the same steps as those followed during the initial scoring. The process moves the patient to higher activity levels, unless there are intervening problems affecting mobility.
In such cases, according to the Barthel Index, the patient may remain at the same—or be moved to a lower—activity level. In practice, patients are assessed each shift, and those with higher function (stage 3) are progressed to unsupervised ambulation.
The role of physical and occupational therapy. Although the role of physical and occupational therapists in the SLUHN mobility program is well codified, it is reserved for patients with complex rehabilitation needs due to the number of patients requiring rehabilitation.
In sum, this patient mobility program–for non-ICU hospitalized patients–relies on:
- Documentation of baseline function;
- Independent scoring using the Barthel Index;
- Creation of clear roles for nursing, nursing assistants, and therapists; and
- Reevaluation of patients at regular intervals based on the Barthel Index, so that they may progress to greater activity levels (or to lower levels in the case of a setback).
A key subsequent step, an evaluation of the program’s performance in terms of readmissions, transfer rates to a skilled nursing facility, and skilled facility length of stay, has shown positive results in all three domains.


References
- Shi SL, Girrard P, Goldstein R, et al. Functional status outperforms comorbidities in predicting acute care readmissions in medically complex patients. J Gen Intern Med. 2015;30(11):1688-1695.
- Dammeyer JA, Baldwin N, Packard D, et al. Mobilizing outcomes: implementation of a nurse-led multidisciplinary mobility program. Crit Care Nurs Q. 2013;36(1):109-119.
- Wood W, Tschannen D, Trotsky A, et al. A mobility program for an inpatient acute care medical unit. Am J Nurs. 2014;114(10):34-40.
- Mahoney FI, Barthel DW. Functional evaluation: the Barthel Index. Md State Med J. 1965;14:61-65.
Empathy, Patients, and Caregivers
Empathy—the feeling that you understand and share another person’s experiences and emotions: the ability to share someone else’s feelings.
—Merriam-Webster
By the time I became a third-year medical resident, I had mastered the repertoire of “don’t tread on me” behaviors that seemed essential to survive as a senior level trainee. I emulated my supervisors, mostly residents, as they advocated for themselves in the face of an onslaught of demand from other departments and from patients. I remember one occasion when, in front of my intern, I firmly “told off” a patient who was obviously poor and possibly homeless and who I thought was faking pain in order to get admitted to the hospital and receive analgesics. I was pleased with myself when I informed the ED staff that I would not accept the patient onto the medical service.
In retrospect, I wonder how and why I had become a “tough guy”? What had happened to my desire to “be there” for patients in their hour of need? Had I lost my aspiration to care for others, fueled by role models like my father, an internist and pillar in the community?
Does Empathy Decrease over Time?
A number of studies support my personal observation that physician empathy decreases during the training years and later persists at lower levels.1
Yet, perhaps ironically, increased empathy is associated with fewer medical errors, increased patient satisfaction, fewer malpractice claims, and improved clinical outcomes.1
Can We Increase Empathy?
In a 2012 study, Helen Reiss and colleagues randomized residents from several specialties into two groups, one receiving standard post-graduate education and a second whose education included three 60-minute empathy training modules. The empathy training consisted of the following elements:
- Neurobiology of empathy;
- Approaches to increase awareness of the physiology of emotions during patient encounters;
- Skills involved in interpreting the meaning of facial expressions; and
- Breathing exercises and mindfulness practices to enhance empathic responses to patients.
Using a validated instrument to measure empathy as rated by patients, the study reported increased empathy scores for the residents who participated in the empathy training program. An important skill the residents learned in the training was the ability to read/decode the facial expressions of patients and use that information to alter their behavior, thereby increasing patient-reported empathy.1
The authors point to the need for more studies to learn if, and to what extent, empathy training can improve performance in key areas like patient outcomes, malpractice claims, physician well-being, and patient satisfaction. Furthermore, they concluded that “long-lasting improvements in empathic clinical care cannot be sustained without organizational changes at all levels of healthcare. Such cultural changes require a commitment from clinical and administrative leaders to place empathic care at the forefront of institutional missions.”
Committing to Enhancing Physician Empathy
The Cleveland Clinic has addressed empathy as an important element of its institutional mission. Consider the following initiatives and interventions:
- The health system’s CEO publicly prioritizes empathy as a path to better patient experience and caregiver well-being.
- There is a chief experience officer position.
- All employees receive specialized H.E.A.R.T. (Hear, Empathize, Apologize, Respond, Thank) training; embedded approaches and practices support ongoing prioritization of empathy.
- All employees are trained to see themselves as caregivers.
- Physicians and trainees receive training in communication with patients.
- The health system holds an annual national summit on empathy and patient experience.
If you haven’t seen the Cleveland Clinic video that has gone viral, Google “Empathy: The Human Connection to Patient Care.” The video takes advantage of a universal human trait: When we truly know what another person is experiencing and feeling, we can experience and feel the same thing.
Can Hospitalists Retain an Empathic Approach over the Long Term?
I believe hospitalists can retain or regain the empathy that led to our choice of medicine as a career. To do this, we should consider a few critical practices, some of which occur at work and some at home. These include the following strategies:
- Find ways to be fully present in your human encounters with patients and co-workers. This includes minimizing interruptions whenever possible, sitting with people, making eye contact, and putting your phone away.
- Reward yourself for hard work. Make rewards, which needn’t always be expensive, a regular part of your life.
- Take measures to avoid overwork. Know when to say “no” to added responsibilities. Find time to add a wellness practice to your life, such as exercise, art, literature, spending time with your spouse/children, or community service.
- Express the gratitude you are feeling to those you work and live with.
Resources for Empathy Training
Empathetics.com offers CME and nursing continuing education credits for training in “how to detect and manage the emotional states of patients and how to respond with empathy and compassion, even in difficult interactions.”
PaulEkman.com has a series of training modules geared to detecting the “unspoken feelings” of others by recognizing the meaning of facial expressions.

Reference
- Reiss H, Kelley JM, Bailey RW, Dunn EJ, Phillips M. Empathy training for resident physicians: a randomized controlled trial of a neuroscience-informed curriculum. J Gen Intern Med. 2012;27(10):1280-1286.
Empathy—the feeling that you understand and share another person’s experiences and emotions: the ability to share someone else’s feelings.
—Merriam-Webster
By the time I became a third-year medical resident, I had mastered the repertoire of “don’t tread on me” behaviors that seemed essential to survive as a senior level trainee. I emulated my supervisors, mostly residents, as they advocated for themselves in the face of an onslaught of demand from other departments and from patients. I remember one occasion when, in front of my intern, I firmly “told off” a patient who was obviously poor and possibly homeless and who I thought was faking pain in order to get admitted to the hospital and receive analgesics. I was pleased with myself when I informed the ED staff that I would not accept the patient onto the medical service.
In retrospect, I wonder how and why I had become a “tough guy”? What had happened to my desire to “be there” for patients in their hour of need? Had I lost my aspiration to care for others, fueled by role models like my father, an internist and pillar in the community?
Does Empathy Decrease over Time?
A number of studies support my personal observation that physician empathy decreases during the training years and later persists at lower levels.1
Yet, perhaps ironically, increased empathy is associated with fewer medical errors, increased patient satisfaction, fewer malpractice claims, and improved clinical outcomes.1
Can We Increase Empathy?
In a 2012 study, Helen Reiss and colleagues randomized residents from several specialties into two groups, one receiving standard post-graduate education and a second whose education included three 60-minute empathy training modules. The empathy training consisted of the following elements:
- Neurobiology of empathy;
- Approaches to increase awareness of the physiology of emotions during patient encounters;
- Skills involved in interpreting the meaning of facial expressions; and
- Breathing exercises and mindfulness practices to enhance empathic responses to patients.
Using a validated instrument to measure empathy as rated by patients, the study reported increased empathy scores for the residents who participated in the empathy training program. An important skill the residents learned in the training was the ability to read/decode the facial expressions of patients and use that information to alter their behavior, thereby increasing patient-reported empathy.1
The authors point to the need for more studies to learn if, and to what extent, empathy training can improve performance in key areas like patient outcomes, malpractice claims, physician well-being, and patient satisfaction. Furthermore, they concluded that “long-lasting improvements in empathic clinical care cannot be sustained without organizational changes at all levels of healthcare. Such cultural changes require a commitment from clinical and administrative leaders to place empathic care at the forefront of institutional missions.”
Committing to Enhancing Physician Empathy
The Cleveland Clinic has addressed empathy as an important element of its institutional mission. Consider the following initiatives and interventions:
- The health system’s CEO publicly prioritizes empathy as a path to better patient experience and caregiver well-being.
- There is a chief experience officer position.
- All employees receive specialized H.E.A.R.T. (Hear, Empathize, Apologize, Respond, Thank) training; embedded approaches and practices support ongoing prioritization of empathy.
- All employees are trained to see themselves as caregivers.
- Physicians and trainees receive training in communication with patients.
- The health system holds an annual national summit on empathy and patient experience.
If you haven’t seen the Cleveland Clinic video that has gone viral, Google “Empathy: The Human Connection to Patient Care.” The video takes advantage of a universal human trait: When we truly know what another person is experiencing and feeling, we can experience and feel the same thing.
Can Hospitalists Retain an Empathic Approach over the Long Term?
I believe hospitalists can retain or regain the empathy that led to our choice of medicine as a career. To do this, we should consider a few critical practices, some of which occur at work and some at home. These include the following strategies:
- Find ways to be fully present in your human encounters with patients and co-workers. This includes minimizing interruptions whenever possible, sitting with people, making eye contact, and putting your phone away.
- Reward yourself for hard work. Make rewards, which needn’t always be expensive, a regular part of your life.
- Take measures to avoid overwork. Know when to say “no” to added responsibilities. Find time to add a wellness practice to your life, such as exercise, art, literature, spending time with your spouse/children, or community service.
- Express the gratitude you are feeling to those you work and live with.
Resources for Empathy Training
Empathetics.com offers CME and nursing continuing education credits for training in “how to detect and manage the emotional states of patients and how to respond with empathy and compassion, even in difficult interactions.”
PaulEkman.com has a series of training modules geared to detecting the “unspoken feelings” of others by recognizing the meaning of facial expressions.

Reference
- Reiss H, Kelley JM, Bailey RW, Dunn EJ, Phillips M. Empathy training for resident physicians: a randomized controlled trial of a neuroscience-informed curriculum. J Gen Intern Med. 2012;27(10):1280-1286.
Empathy—the feeling that you understand and share another person’s experiences and emotions: the ability to share someone else’s feelings.
—Merriam-Webster
By the time I became a third-year medical resident, I had mastered the repertoire of “don’t tread on me” behaviors that seemed essential to survive as a senior level trainee. I emulated my supervisors, mostly residents, as they advocated for themselves in the face of an onslaught of demand from other departments and from patients. I remember one occasion when, in front of my intern, I firmly “told off” a patient who was obviously poor and possibly homeless and who I thought was faking pain in order to get admitted to the hospital and receive analgesics. I was pleased with myself when I informed the ED staff that I would not accept the patient onto the medical service.
In retrospect, I wonder how and why I had become a “tough guy”? What had happened to my desire to “be there” for patients in their hour of need? Had I lost my aspiration to care for others, fueled by role models like my father, an internist and pillar in the community?
Does Empathy Decrease over Time?
A number of studies support my personal observation that physician empathy decreases during the training years and later persists at lower levels.1
Yet, perhaps ironically, increased empathy is associated with fewer medical errors, increased patient satisfaction, fewer malpractice claims, and improved clinical outcomes.1
Can We Increase Empathy?
In a 2012 study, Helen Reiss and colleagues randomized residents from several specialties into two groups, one receiving standard post-graduate education and a second whose education included three 60-minute empathy training modules. The empathy training consisted of the following elements:
- Neurobiology of empathy;
- Approaches to increase awareness of the physiology of emotions during patient encounters;
- Skills involved in interpreting the meaning of facial expressions; and
- Breathing exercises and mindfulness practices to enhance empathic responses to patients.
Using a validated instrument to measure empathy as rated by patients, the study reported increased empathy scores for the residents who participated in the empathy training program. An important skill the residents learned in the training was the ability to read/decode the facial expressions of patients and use that information to alter their behavior, thereby increasing patient-reported empathy.1
The authors point to the need for more studies to learn if, and to what extent, empathy training can improve performance in key areas like patient outcomes, malpractice claims, physician well-being, and patient satisfaction. Furthermore, they concluded that “long-lasting improvements in empathic clinical care cannot be sustained without organizational changes at all levels of healthcare. Such cultural changes require a commitment from clinical and administrative leaders to place empathic care at the forefront of institutional missions.”
Committing to Enhancing Physician Empathy
The Cleveland Clinic has addressed empathy as an important element of its institutional mission. Consider the following initiatives and interventions:
- The health system’s CEO publicly prioritizes empathy as a path to better patient experience and caregiver well-being.
- There is a chief experience officer position.
- All employees receive specialized H.E.A.R.T. (Hear, Empathize, Apologize, Respond, Thank) training; embedded approaches and practices support ongoing prioritization of empathy.
- All employees are trained to see themselves as caregivers.
- Physicians and trainees receive training in communication with patients.
- The health system holds an annual national summit on empathy and patient experience.
If you haven’t seen the Cleveland Clinic video that has gone viral, Google “Empathy: The Human Connection to Patient Care.” The video takes advantage of a universal human trait: When we truly know what another person is experiencing and feeling, we can experience and feel the same thing.
Can Hospitalists Retain an Empathic Approach over the Long Term?
I believe hospitalists can retain or regain the empathy that led to our choice of medicine as a career. To do this, we should consider a few critical practices, some of which occur at work and some at home. These include the following strategies:
- Find ways to be fully present in your human encounters with patients and co-workers. This includes minimizing interruptions whenever possible, sitting with people, making eye contact, and putting your phone away.
- Reward yourself for hard work. Make rewards, which needn’t always be expensive, a regular part of your life.
- Take measures to avoid overwork. Know when to say “no” to added responsibilities. Find time to add a wellness practice to your life, such as exercise, art, literature, spending time with your spouse/children, or community service.
- Express the gratitude you are feeling to those you work and live with.
Resources for Empathy Training
Empathetics.com offers CME and nursing continuing education credits for training in “how to detect and manage the emotional states of patients and how to respond with empathy and compassion, even in difficult interactions.”
PaulEkman.com has a series of training modules geared to detecting the “unspoken feelings” of others by recognizing the meaning of facial expressions.

Reference
- Reiss H, Kelley JM, Bailey RW, Dunn EJ, Phillips M. Empathy training for resident physicians: a randomized controlled trial of a neuroscience-informed curriculum. J Gen Intern Med. 2012;27(10):1280-1286.
The Three-Year Plan
Although 2019 may seem like a long way away, it isn’t too soon to start thinking about and preparing for the Merit-based Incentive Payment System (MIPS) or its (seemingly preferable) alternative, participation in an alternative payment model (APM) such as an ACO, a medical home, or a bundled payment program.
In April, Congress permanently repealed Medicare’s sustainable growth rate (SGR) formula for controlling physician payment. In yet another sign that we are in the midst of the biggest healthcare transformation in a generation, the 18-year-old SGR formula will be replaced by a far-reaching package of payment reforms. Here we will focus on the MIPS and its alternative, an APM, which involves assuming risk for financial loss or gain and measuring and reporting on quality.
The MIPS replaces three existing quality measurement programs that, to greater and lesser degrees, physicians have struggled with:
- Physician Quality Reporting System (PQRS);
- Value-based payment modifier; and
- Meaningful use of electronic health records.
MIPS will not totally eliminate these programs but will instead incorporate yet-to-be-defined elements of them and, presumably, though it is yet unclear, add new elements. For 2015-2018, the current payment system will remain intact. For 2019, physicians will have a choice. Either they must participate in MIPS, which will likely be complex and involve some administrative burden, or derive at least 25% of their practice revenue from an APM.
For those participating in MIPS, physician payment rates will be subject to an up or down adjustment based on performance in four categories: quality, meaningful use of EHRs, resource use, and clinical practice improvement.
There is an opportunity to avoid MIPS altogether, however. One of the most notable elements of the SGR fix is its push for physicians to participate in APMs such as ACOs, medical homes, bundled payment arrangements, and other payment models now being evaluated by the CMS Innovation Center. Physicians who gain a substantial portion—this means 25% in 2019 and 2020, and likely more thereafter—of their revenue through APMs like these will have the dual benefit of being exempt from MIPS participation and receiving a 5% annual bonus through 2024. After that, physicians in APMs will receive annual fee increases of 0.75%, while all other physicians will receive only a 0.25% increase.1
Strategic Thinking for Hospitalists: Enter an APM
If you’re asking yourself where you want your hospitalist practice to be in three years, I would suggest the answer is “in an alternative payment model of one kind or another.”
If you are an employed practice, strategic planning will involve assessing the APMs your hospital or health system is participating in and planning how your hospitalist practice can become a formal member of the arrangement.
If you are a freestanding practice, you should become a student of the APM policy coming from the CMS Innovation Center, and determine the best “insertion point” for your practice, such that you gain at least a quarter of your revenue through an APM within three years.

Reference
- Steinbrook R. The repeal of Medicare’s sustainable growth rate for physician payment. JAMA. 2015;313(20):2025-2026.
Although 2019 may seem like a long way away, it isn’t too soon to start thinking about and preparing for the Merit-based Incentive Payment System (MIPS) or its (seemingly preferable) alternative, participation in an alternative payment model (APM) such as an ACO, a medical home, or a bundled payment program.
In April, Congress permanently repealed Medicare’s sustainable growth rate (SGR) formula for controlling physician payment. In yet another sign that we are in the midst of the biggest healthcare transformation in a generation, the 18-year-old SGR formula will be replaced by a far-reaching package of payment reforms. Here we will focus on the MIPS and its alternative, an APM, which involves assuming risk for financial loss or gain and measuring and reporting on quality.
The MIPS replaces three existing quality measurement programs that, to greater and lesser degrees, physicians have struggled with:
- Physician Quality Reporting System (PQRS);
- Value-based payment modifier; and
- Meaningful use of electronic health records.
MIPS will not totally eliminate these programs but will instead incorporate yet-to-be-defined elements of them and, presumably, though it is yet unclear, add new elements. For 2015-2018, the current payment system will remain intact. For 2019, physicians will have a choice. Either they must participate in MIPS, which will likely be complex and involve some administrative burden, or derive at least 25% of their practice revenue from an APM.
For those participating in MIPS, physician payment rates will be subject to an up or down adjustment based on performance in four categories: quality, meaningful use of EHRs, resource use, and clinical practice improvement.
There is an opportunity to avoid MIPS altogether, however. One of the most notable elements of the SGR fix is its push for physicians to participate in APMs such as ACOs, medical homes, bundled payment arrangements, and other payment models now being evaluated by the CMS Innovation Center. Physicians who gain a substantial portion—this means 25% in 2019 and 2020, and likely more thereafter—of their revenue through APMs like these will have the dual benefit of being exempt from MIPS participation and receiving a 5% annual bonus through 2024. After that, physicians in APMs will receive annual fee increases of 0.75%, while all other physicians will receive only a 0.25% increase.1
Strategic Thinking for Hospitalists: Enter an APM
If you’re asking yourself where you want your hospitalist practice to be in three years, I would suggest the answer is “in an alternative payment model of one kind or another.”
If you are an employed practice, strategic planning will involve assessing the APMs your hospital or health system is participating in and planning how your hospitalist practice can become a formal member of the arrangement.
If you are a freestanding practice, you should become a student of the APM policy coming from the CMS Innovation Center, and determine the best “insertion point” for your practice, such that you gain at least a quarter of your revenue through an APM within three years.

Reference
- Steinbrook R. The repeal of Medicare’s sustainable growth rate for physician payment. JAMA. 2015;313(20):2025-2026.
Although 2019 may seem like a long way away, it isn’t too soon to start thinking about and preparing for the Merit-based Incentive Payment System (MIPS) or its (seemingly preferable) alternative, participation in an alternative payment model (APM) such as an ACO, a medical home, or a bundled payment program.
In April, Congress permanently repealed Medicare’s sustainable growth rate (SGR) formula for controlling physician payment. In yet another sign that we are in the midst of the biggest healthcare transformation in a generation, the 18-year-old SGR formula will be replaced by a far-reaching package of payment reforms. Here we will focus on the MIPS and its alternative, an APM, which involves assuming risk for financial loss or gain and measuring and reporting on quality.
The MIPS replaces three existing quality measurement programs that, to greater and lesser degrees, physicians have struggled with:
- Physician Quality Reporting System (PQRS);
- Value-based payment modifier; and
- Meaningful use of electronic health records.
MIPS will not totally eliminate these programs but will instead incorporate yet-to-be-defined elements of them and, presumably, though it is yet unclear, add new elements. For 2015-2018, the current payment system will remain intact. For 2019, physicians will have a choice. Either they must participate in MIPS, which will likely be complex and involve some administrative burden, or derive at least 25% of their practice revenue from an APM.
For those participating in MIPS, physician payment rates will be subject to an up or down adjustment based on performance in four categories: quality, meaningful use of EHRs, resource use, and clinical practice improvement.
There is an opportunity to avoid MIPS altogether, however. One of the most notable elements of the SGR fix is its push for physicians to participate in APMs such as ACOs, medical homes, bundled payment arrangements, and other payment models now being evaluated by the CMS Innovation Center. Physicians who gain a substantial portion—this means 25% in 2019 and 2020, and likely more thereafter—of their revenue through APMs like these will have the dual benefit of being exempt from MIPS participation and receiving a 5% annual bonus through 2024. After that, physicians in APMs will receive annual fee increases of 0.75%, while all other physicians will receive only a 0.25% increase.1
Strategic Thinking for Hospitalists: Enter an APM
If you’re asking yourself where you want your hospitalist practice to be in three years, I would suggest the answer is “in an alternative payment model of one kind or another.”
If you are an employed practice, strategic planning will involve assessing the APMs your hospital or health system is participating in and planning how your hospitalist practice can become a formal member of the arrangement.
If you are a freestanding practice, you should become a student of the APM policy coming from the CMS Innovation Center, and determine the best “insertion point” for your practice, such that you gain at least a quarter of your revenue through an APM within three years.

Reference
- Steinbrook R. The repeal of Medicare’s sustainable growth rate for physician payment. JAMA. 2015;313(20):2025-2026.
Bundled Payment and Hospital Medicine, Pt. 2
Editor’s note: Second in a two-part series examining bundled payments and hospital medicine. In full disclosure, Dr. Whitcomb works for a company that is an Awardee Convener in the CMS Bundled Payments for Care Improvement (BPCI) Initiative.
In part one of this series, we discussed the basics of the BPCI program. Now we will delve into specific roles and opportunities for hospitalists in bundled payment programs in general, and the BPCI program in particular.
The bundled payment model can be hard to explain. One example that might make it clearer is that of LASIK vision correction surgery, where a single bundled payment covers the fees of the ophthalmologist, the operating facility, and any other services (like optometry) and medications (like eye drops). Another example is the diagnosis-related group (DRG) payment for hospital care, in which all facility costs are bundled together into a single payment.
A simplistic way to differentiate bundled payment from accountable care organization (ACOs) is that the former is typically initiated by an acute medical or surgical event and concludes after a recovery period—often 30, 60, or 90 days. Conversely, the latter generally covers the care of individuals within a population over time, often focusing on the management of chronic conditions.
The Opportunity
Two major opportunities for hospitalists to improve value (quality/cost) present themselves through the BPCI initiative. One is in post-acute facility utilization, and the other is in reducing readmissions. Figure 1 shows that for 30-day episodes starting with a hospitalization for five common conditions, payments for post-acute care are surprisingly close in amount to those for the preceding hospitalization.1
Much of the cost of post-acute care comes from skilled nursing facilities (SNFs) and, to a lesser degree, inpatient rehabilitation facilities. A broad range of research studies has demonstrated that inpatient care managed by hospitalists—compared with the traditional model—is associated with a decrease in inpatient costs; however, recent research indicates that the hospital cost savings generated by hospitalists are offset by more spending in the 30 days post discharge, specifically on more SNF care and increased readmissions.2 As another indicator that post-acute care needs a closer look, a 2013 Institute of Medicine report concluded that spending on post-acute care was responsible for the majority of Medicare’s overall regional variation in spending.1,3
Of course, success in a bundled payment model will also be derived from reducing costs in the hospital setting, such as those stemming from unnecessary or duplicative testing and imaging, injudicious use of consultants, and practices identified in programs such as Choosing Wisely.
How Your Practice Can Drive Bundled Payment Success
The aforementioned observations point to the need to improve the value of post-acute care by optimizing post-acute spending—driven mostly by SNF costs—and minimizing avoidable readmissions. I offer the following inpatient interventions to achieve these goals:
- Speak with patients early and often regarding expectations for recovery post discharge. When possible, set a goal of home discharge with the needed support.
- Write orders for early ambulation. Develop an early ambulation program with nursing and physical therapy.
- Address goals of care during the patient/family meeting. For appropriate patients with life-limiting illness, involve the palliative care service or equivalent and discuss the role of future aggressive interventions, including hospitalization, so that the course set is consistent with the patients’ goals and wishes.
- Lead the in-hospital team, instead of defaulting to others, like case management, in making an informed decision about ideal post-discharge location by factoring in caregiver availability, independence, and SNF needs. Marshal resources to enable a home recovery (i.e., home health evaluation), whether or not there is an intervening SNF stay. If patients go to a SNF, set expectations for length of stay in the facility.
- Adhere to best practices for care transitions, such as those in Project BOOST, including thorough medication reconciliation.
Beyond the Four Walls
As you aim for a high-value (high quality and affordable) discharge, your hospital medicine practice may consider new approaches to filling longstanding gaps in post-acute care. Forward-looking hospitalist groups have implemented the following approaches:
- Establish a post-discharge clinic where patients are seen after discharge, in the interim before they have an opportunity for primary care follow-up;
- Send teams to work in SNFs;
- Call patients after discharge to ensure they are following their plan of care;
- Leverage newer current procedural terminology (CPT) codes, like the Transitional Care Management or Chronic Care Management codes, to support your transitional care services;
- Provide home visits for high-risk patients; and
- Access waivers for G-codes for home visits and/or telemedicine outside of rural areas. These waivers exist under the BPCI initiative.
Shift from ‘Traditional’ Hospitalist to ‘Value’ Hospitalist
If some of the changes in practice needed to succeed in a bundled payment world seem daunting to you, it may be helpful to realize that with the challenge comes an opportunity. This opportunity for hospitalists parallels that of the early days of the specialty, when reducing length of stay created substantial support from hospital leaders and was a factor leading to the rapid growth in the number of hospitalists. In January, the U.S. Secretary of Health and Human Services set a goal to tie 50% of Medicare payments to ‘alternative payment models’ like bundled payments by 2018. In April, as part of the sustainable growth rate fix, Medicare announced it would create substantial new bonuses for physicians who have at least 25% of their revenue in such models.1
As healthcare policy aligns behind ‘alternative payment models,’ bundled payment programs are likely to be a potent driver of an evolving hospitalist specialty. Next-generation hospitalists will be asked to take a leadership role in addressing ‘value’ with responsibility for improving care coordination and affordability over an episode of illness.
Now may be the time to take to heart the words of computer scientist Alan Kay: “The best way to predict the future is to invent it.”

References
- Mechanic R. Post-acute care–the next frontier for controlling Medicare spending. N Engl J Med. 2014;370(8):692-694.
- Kuo YF, Goodwin JS. Association of hospitalist care with medical utilization after discharge: evidence of cost shift from a cohort study. Ann Intern Med. 2011;155(3):152-159.
- Newhouse JP, Garber AM. Geographic variation in Medicare services. N Engl J Med. 2013;368(16):1465-1468.
Editor’s note: Second in a two-part series examining bundled payments and hospital medicine. In full disclosure, Dr. Whitcomb works for a company that is an Awardee Convener in the CMS Bundled Payments for Care Improvement (BPCI) Initiative.
In part one of this series, we discussed the basics of the BPCI program. Now we will delve into specific roles and opportunities for hospitalists in bundled payment programs in general, and the BPCI program in particular.
The bundled payment model can be hard to explain. One example that might make it clearer is that of LASIK vision correction surgery, where a single bundled payment covers the fees of the ophthalmologist, the operating facility, and any other services (like optometry) and medications (like eye drops). Another example is the diagnosis-related group (DRG) payment for hospital care, in which all facility costs are bundled together into a single payment.
A simplistic way to differentiate bundled payment from accountable care organization (ACOs) is that the former is typically initiated by an acute medical or surgical event and concludes after a recovery period—often 30, 60, or 90 days. Conversely, the latter generally covers the care of individuals within a population over time, often focusing on the management of chronic conditions.
The Opportunity
Two major opportunities for hospitalists to improve value (quality/cost) present themselves through the BPCI initiative. One is in post-acute facility utilization, and the other is in reducing readmissions. Figure 1 shows that for 30-day episodes starting with a hospitalization for five common conditions, payments for post-acute care are surprisingly close in amount to those for the preceding hospitalization.1
Much of the cost of post-acute care comes from skilled nursing facilities (SNFs) and, to a lesser degree, inpatient rehabilitation facilities. A broad range of research studies has demonstrated that inpatient care managed by hospitalists—compared with the traditional model—is associated with a decrease in inpatient costs; however, recent research indicates that the hospital cost savings generated by hospitalists are offset by more spending in the 30 days post discharge, specifically on more SNF care and increased readmissions.2 As another indicator that post-acute care needs a closer look, a 2013 Institute of Medicine report concluded that spending on post-acute care was responsible for the majority of Medicare’s overall regional variation in spending.1,3
Of course, success in a bundled payment model will also be derived from reducing costs in the hospital setting, such as those stemming from unnecessary or duplicative testing and imaging, injudicious use of consultants, and practices identified in programs such as Choosing Wisely.
How Your Practice Can Drive Bundled Payment Success
The aforementioned observations point to the need to improve the value of post-acute care by optimizing post-acute spending—driven mostly by SNF costs—and minimizing avoidable readmissions. I offer the following inpatient interventions to achieve these goals:
- Speak with patients early and often regarding expectations for recovery post discharge. When possible, set a goal of home discharge with the needed support.
- Write orders for early ambulation. Develop an early ambulation program with nursing and physical therapy.
- Address goals of care during the patient/family meeting. For appropriate patients with life-limiting illness, involve the palliative care service or equivalent and discuss the role of future aggressive interventions, including hospitalization, so that the course set is consistent with the patients’ goals and wishes.
- Lead the in-hospital team, instead of defaulting to others, like case management, in making an informed decision about ideal post-discharge location by factoring in caregiver availability, independence, and SNF needs. Marshal resources to enable a home recovery (i.e., home health evaluation), whether or not there is an intervening SNF stay. If patients go to a SNF, set expectations for length of stay in the facility.
- Adhere to best practices for care transitions, such as those in Project BOOST, including thorough medication reconciliation.
Beyond the Four Walls
As you aim for a high-value (high quality and affordable) discharge, your hospital medicine practice may consider new approaches to filling longstanding gaps in post-acute care. Forward-looking hospitalist groups have implemented the following approaches:
- Establish a post-discharge clinic where patients are seen after discharge, in the interim before they have an opportunity for primary care follow-up;
- Send teams to work in SNFs;
- Call patients after discharge to ensure they are following their plan of care;
- Leverage newer current procedural terminology (CPT) codes, like the Transitional Care Management or Chronic Care Management codes, to support your transitional care services;
- Provide home visits for high-risk patients; and
- Access waivers for G-codes for home visits and/or telemedicine outside of rural areas. These waivers exist under the BPCI initiative.
Shift from ‘Traditional’ Hospitalist to ‘Value’ Hospitalist
If some of the changes in practice needed to succeed in a bundled payment world seem daunting to you, it may be helpful to realize that with the challenge comes an opportunity. This opportunity for hospitalists parallels that of the early days of the specialty, when reducing length of stay created substantial support from hospital leaders and was a factor leading to the rapid growth in the number of hospitalists. In January, the U.S. Secretary of Health and Human Services set a goal to tie 50% of Medicare payments to ‘alternative payment models’ like bundled payments by 2018. In April, as part of the sustainable growth rate fix, Medicare announced it would create substantial new bonuses for physicians who have at least 25% of their revenue in such models.1
As healthcare policy aligns behind ‘alternative payment models,’ bundled payment programs are likely to be a potent driver of an evolving hospitalist specialty. Next-generation hospitalists will be asked to take a leadership role in addressing ‘value’ with responsibility for improving care coordination and affordability over an episode of illness.
Now may be the time to take to heart the words of computer scientist Alan Kay: “The best way to predict the future is to invent it.”

References
- Mechanic R. Post-acute care–the next frontier for controlling Medicare spending. N Engl J Med. 2014;370(8):692-694.
- Kuo YF, Goodwin JS. Association of hospitalist care with medical utilization after discharge: evidence of cost shift from a cohort study. Ann Intern Med. 2011;155(3):152-159.
- Newhouse JP, Garber AM. Geographic variation in Medicare services. N Engl J Med. 2013;368(16):1465-1468.
Editor’s note: Second in a two-part series examining bundled payments and hospital medicine. In full disclosure, Dr. Whitcomb works for a company that is an Awardee Convener in the CMS Bundled Payments for Care Improvement (BPCI) Initiative.
In part one of this series, we discussed the basics of the BPCI program. Now we will delve into specific roles and opportunities for hospitalists in bundled payment programs in general, and the BPCI program in particular.
The bundled payment model can be hard to explain. One example that might make it clearer is that of LASIK vision correction surgery, where a single bundled payment covers the fees of the ophthalmologist, the operating facility, and any other services (like optometry) and medications (like eye drops). Another example is the diagnosis-related group (DRG) payment for hospital care, in which all facility costs are bundled together into a single payment.
A simplistic way to differentiate bundled payment from accountable care organization (ACOs) is that the former is typically initiated by an acute medical or surgical event and concludes after a recovery period—often 30, 60, or 90 days. Conversely, the latter generally covers the care of individuals within a population over time, often focusing on the management of chronic conditions.
The Opportunity
Two major opportunities for hospitalists to improve value (quality/cost) present themselves through the BPCI initiative. One is in post-acute facility utilization, and the other is in reducing readmissions. Figure 1 shows that for 30-day episodes starting with a hospitalization for five common conditions, payments for post-acute care are surprisingly close in amount to those for the preceding hospitalization.1
Much of the cost of post-acute care comes from skilled nursing facilities (SNFs) and, to a lesser degree, inpatient rehabilitation facilities. A broad range of research studies has demonstrated that inpatient care managed by hospitalists—compared with the traditional model—is associated with a decrease in inpatient costs; however, recent research indicates that the hospital cost savings generated by hospitalists are offset by more spending in the 30 days post discharge, specifically on more SNF care and increased readmissions.2 As another indicator that post-acute care needs a closer look, a 2013 Institute of Medicine report concluded that spending on post-acute care was responsible for the majority of Medicare’s overall regional variation in spending.1,3
Of course, success in a bundled payment model will also be derived from reducing costs in the hospital setting, such as those stemming from unnecessary or duplicative testing and imaging, injudicious use of consultants, and practices identified in programs such as Choosing Wisely.
How Your Practice Can Drive Bundled Payment Success
The aforementioned observations point to the need to improve the value of post-acute care by optimizing post-acute spending—driven mostly by SNF costs—and minimizing avoidable readmissions. I offer the following inpatient interventions to achieve these goals:
- Speak with patients early and often regarding expectations for recovery post discharge. When possible, set a goal of home discharge with the needed support.
- Write orders for early ambulation. Develop an early ambulation program with nursing and physical therapy.
- Address goals of care during the patient/family meeting. For appropriate patients with life-limiting illness, involve the palliative care service or equivalent and discuss the role of future aggressive interventions, including hospitalization, so that the course set is consistent with the patients’ goals and wishes.
- Lead the in-hospital team, instead of defaulting to others, like case management, in making an informed decision about ideal post-discharge location by factoring in caregiver availability, independence, and SNF needs. Marshal resources to enable a home recovery (i.e., home health evaluation), whether or not there is an intervening SNF stay. If patients go to a SNF, set expectations for length of stay in the facility.
- Adhere to best practices for care transitions, such as those in Project BOOST, including thorough medication reconciliation.
Beyond the Four Walls
As you aim for a high-value (high quality and affordable) discharge, your hospital medicine practice may consider new approaches to filling longstanding gaps in post-acute care. Forward-looking hospitalist groups have implemented the following approaches:
- Establish a post-discharge clinic where patients are seen after discharge, in the interim before they have an opportunity for primary care follow-up;
- Send teams to work in SNFs;
- Call patients after discharge to ensure they are following their plan of care;
- Leverage newer current procedural terminology (CPT) codes, like the Transitional Care Management or Chronic Care Management codes, to support your transitional care services;
- Provide home visits for high-risk patients; and
- Access waivers for G-codes for home visits and/or telemedicine outside of rural areas. These waivers exist under the BPCI initiative.
Shift from ‘Traditional’ Hospitalist to ‘Value’ Hospitalist
If some of the changes in practice needed to succeed in a bundled payment world seem daunting to you, it may be helpful to realize that with the challenge comes an opportunity. This opportunity for hospitalists parallels that of the early days of the specialty, when reducing length of stay created substantial support from hospital leaders and was a factor leading to the rapid growth in the number of hospitalists. In January, the U.S. Secretary of Health and Human Services set a goal to tie 50% of Medicare payments to ‘alternative payment models’ like bundled payments by 2018. In April, as part of the sustainable growth rate fix, Medicare announced it would create substantial new bonuses for physicians who have at least 25% of their revenue in such models.1
As healthcare policy aligns behind ‘alternative payment models,’ bundled payment programs are likely to be a potent driver of an evolving hospitalist specialty. Next-generation hospitalists will be asked to take a leadership role in addressing ‘value’ with responsibility for improving care coordination and affordability over an episode of illness.
Now may be the time to take to heart the words of computer scientist Alan Kay: “The best way to predict the future is to invent it.”

References
- Mechanic R. Post-acute care–the next frontier for controlling Medicare spending. N Engl J Med. 2014;370(8):692-694.
- Kuo YF, Goodwin JS. Association of hospitalist care with medical utilization after discharge: evidence of cost shift from a cohort study. Ann Intern Med. 2011;155(3):152-159.
- Newhouse JP, Garber AM. Geographic variation in Medicare services. N Engl J Med. 2013;368(16):1465-1468.
The Biggest Thing in Hospital Medicine Since Patient Safety?
Editor’s note: First of a two-part series examining bundled payments and hospital medicine. Additionally, Dr. Whitcomb works for a company that is an Awardee Convener in the CMS Bundled Payments for Care Improvement (BPCI) Initiative.
The Centers for Medicare and Medicaid Services’ (CMS) bundled payment initiative was announced in August 2011 and has been “live” since October 2013, when a handful of healthcare systems launched bundled payment programs. In 2014, the CMS initiative grew substantially as a result of large-scale interest on the part of hospitals, physician groups, skilled nursing facilities (SNFs), and others in testing the model, which can be described as a single payment for an episode of care.
The BPCI initiative will be a large-scale program by July 1; it starts with an April 1 cohort launch and will result in the program’s presence in all 50 states, with hundreds of physician practices and hospitals participating. The 2015 cohort will involve a large number of hospitalist practices, participating as “episode initiators” that bear clinical and economic responsibility for the bundle, or as “gainsharers” who are eligible to receive incentive payments if they can reduce costs while maintaining measurable quality for an episode of care.
How Does Bundled Payment Work?
The BPCI initiative is a large-scale, three- to five-year demonstration to test bundled payment in patients with fee-for-service Medicare. The most common model, referred to as Model 2, involves an inpatient hospitalization for one of 48 defined episodes, which include both medical and surgical conditions, followed by a recovery period lasting 30, 60, or 90 days.
Each hospital or physician practice that is considering entering the BPCI program receives prices for all 48 episodes based on a 2009-2012 historical average of Medicare part A and B claims associated with that hospital or physician group. After analyzing those prices, the hospital or physician practice may elect to choose the bundles that have a good chance of being successful—where actual spending comes in under the historical target price—based on care improvement expectations in their local system. In Model 2, CMS takes 2% off the target price for 90-day episodes and 3% off the target price for 30- and 60-day episodes, making it all the more important to choose bundles that demonstrate a high likelihood of success.
The revenue cycle for hospitals and physicians in the program does not change. They submit claims for their services and receive reimbursement as they always have; however, after the end of each quarter, when the majority of part A and B claims have been processed, a “look back” at actual spending for all participating episodes is reconciled against the baseline price derived from 2009-2012. If there is a net savings compared to the baseline, monies can be distributed to the participating providers—the hospital or physician practice—and those providers may further share some of the savings with other physicians/providers who have signed a gainsharing contract.
Hospitalists and BPCI
Hospitalist practices participate in the CMS program either as episode initiators or gainsharers. As episode initiators, they “own” the bundle, which means they bear economic risk for the program. In this capacity, overall savings will mean the hospitalist practice has a new revenue stream, which could be substantial; however, the practice is also responsible for any losses.
Other hospitalist practices have become gainsharers in the program, which means they have signed an agreement enabling them to receive payments in addition to professional fee revenues for activities that reduce costs while maintaining or improving quality. Such activities are referred to as “care redesign” in the program. Gainsharers do not bear financial risk.
Where Will Savings Come From?
Perhaps ironically for hospitalists, the main source of savings in the BPCI program comes from post-acute care and readmissions. For example, for common conditions like heart failure, COPD, and pneumonia, Medicare spends almost as much on post-acute care and readmissions in the first 30 days after discharge as it does on the index hospitalization.1 As a result, the BPCI program adds further emphasis on preventing readmissions when added to existing pressures, and there is a new premium placed on “right-sizing” the usage of SNF and other post-acute facilities, such as inpatient rehabilitation and long-term acute care hospitals. For hospitalists, this means that new rigor is needed to connect to the post-acute setting, such as determining why a patient is being discharged to a skilled facility.
Another savings pool, called “internal cost savings,” is available to reward decreasing inpatient utilization from, for example, testing, imaging, and implantable devices.
Conclusion
Bundled payment might be the biggest thing to come along for hospitalists since the patient safety movement launched some 16 years ago. Why? Although accountable care organizations have largely focused on ambulatory practice, bundled payment has a major focus on hospital care and on the post-acute care decisions that are made during the hospitalization. If bundled payment proves to be an effective way to pay for—and organize—care, hospitalists will play a central role in the success of this innovation.
In part two of this series, I will explore specific roles hospitalists play in successful bundled payment programs.

Reference
Editor’s note: First of a two-part series examining bundled payments and hospital medicine. Additionally, Dr. Whitcomb works for a company that is an Awardee Convener in the CMS Bundled Payments for Care Improvement (BPCI) Initiative.
The Centers for Medicare and Medicaid Services’ (CMS) bundled payment initiative was announced in August 2011 and has been “live” since October 2013, when a handful of healthcare systems launched bundled payment programs. In 2014, the CMS initiative grew substantially as a result of large-scale interest on the part of hospitals, physician groups, skilled nursing facilities (SNFs), and others in testing the model, which can be described as a single payment for an episode of care.
The BPCI initiative will be a large-scale program by July 1; it starts with an April 1 cohort launch and will result in the program’s presence in all 50 states, with hundreds of physician practices and hospitals participating. The 2015 cohort will involve a large number of hospitalist practices, participating as “episode initiators” that bear clinical and economic responsibility for the bundle, or as “gainsharers” who are eligible to receive incentive payments if they can reduce costs while maintaining measurable quality for an episode of care.
How Does Bundled Payment Work?
The BPCI initiative is a large-scale, three- to five-year demonstration to test bundled payment in patients with fee-for-service Medicare. The most common model, referred to as Model 2, involves an inpatient hospitalization for one of 48 defined episodes, which include both medical and surgical conditions, followed by a recovery period lasting 30, 60, or 90 days.
Each hospital or physician practice that is considering entering the BPCI program receives prices for all 48 episodes based on a 2009-2012 historical average of Medicare part A and B claims associated with that hospital or physician group. After analyzing those prices, the hospital or physician practice may elect to choose the bundles that have a good chance of being successful—where actual spending comes in under the historical target price—based on care improvement expectations in their local system. In Model 2, CMS takes 2% off the target price for 90-day episodes and 3% off the target price for 30- and 60-day episodes, making it all the more important to choose bundles that demonstrate a high likelihood of success.
The revenue cycle for hospitals and physicians in the program does not change. They submit claims for their services and receive reimbursement as they always have; however, after the end of each quarter, when the majority of part A and B claims have been processed, a “look back” at actual spending for all participating episodes is reconciled against the baseline price derived from 2009-2012. If there is a net savings compared to the baseline, monies can be distributed to the participating providers—the hospital or physician practice—and those providers may further share some of the savings with other physicians/providers who have signed a gainsharing contract.
Hospitalists and BPCI
Hospitalist practices participate in the CMS program either as episode initiators or gainsharers. As episode initiators, they “own” the bundle, which means they bear economic risk for the program. In this capacity, overall savings will mean the hospitalist practice has a new revenue stream, which could be substantial; however, the practice is also responsible for any losses.
Other hospitalist practices have become gainsharers in the program, which means they have signed an agreement enabling them to receive payments in addition to professional fee revenues for activities that reduce costs while maintaining or improving quality. Such activities are referred to as “care redesign” in the program. Gainsharers do not bear financial risk.
Where Will Savings Come From?
Perhaps ironically for hospitalists, the main source of savings in the BPCI program comes from post-acute care and readmissions. For example, for common conditions like heart failure, COPD, and pneumonia, Medicare spends almost as much on post-acute care and readmissions in the first 30 days after discharge as it does on the index hospitalization.1 As a result, the BPCI program adds further emphasis on preventing readmissions when added to existing pressures, and there is a new premium placed on “right-sizing” the usage of SNF and other post-acute facilities, such as inpatient rehabilitation and long-term acute care hospitals. For hospitalists, this means that new rigor is needed to connect to the post-acute setting, such as determining why a patient is being discharged to a skilled facility.
Another savings pool, called “internal cost savings,” is available to reward decreasing inpatient utilization from, for example, testing, imaging, and implantable devices.
Conclusion
Bundled payment might be the biggest thing to come along for hospitalists since the patient safety movement launched some 16 years ago. Why? Although accountable care organizations have largely focused on ambulatory practice, bundled payment has a major focus on hospital care and on the post-acute care decisions that are made during the hospitalization. If bundled payment proves to be an effective way to pay for—and organize—care, hospitalists will play a central role in the success of this innovation.
In part two of this series, I will explore specific roles hospitalists play in successful bundled payment programs.

Reference
Editor’s note: First of a two-part series examining bundled payments and hospital medicine. Additionally, Dr. Whitcomb works for a company that is an Awardee Convener in the CMS Bundled Payments for Care Improvement (BPCI) Initiative.
The Centers for Medicare and Medicaid Services’ (CMS) bundled payment initiative was announced in August 2011 and has been “live” since October 2013, when a handful of healthcare systems launched bundled payment programs. In 2014, the CMS initiative grew substantially as a result of large-scale interest on the part of hospitals, physician groups, skilled nursing facilities (SNFs), and others in testing the model, which can be described as a single payment for an episode of care.
The BPCI initiative will be a large-scale program by July 1; it starts with an April 1 cohort launch and will result in the program’s presence in all 50 states, with hundreds of physician practices and hospitals participating. The 2015 cohort will involve a large number of hospitalist practices, participating as “episode initiators” that bear clinical and economic responsibility for the bundle, or as “gainsharers” who are eligible to receive incentive payments if they can reduce costs while maintaining measurable quality for an episode of care.
How Does Bundled Payment Work?
The BPCI initiative is a large-scale, three- to five-year demonstration to test bundled payment in patients with fee-for-service Medicare. The most common model, referred to as Model 2, involves an inpatient hospitalization for one of 48 defined episodes, which include both medical and surgical conditions, followed by a recovery period lasting 30, 60, or 90 days.
Each hospital or physician practice that is considering entering the BPCI program receives prices for all 48 episodes based on a 2009-2012 historical average of Medicare part A and B claims associated with that hospital or physician group. After analyzing those prices, the hospital or physician practice may elect to choose the bundles that have a good chance of being successful—where actual spending comes in under the historical target price—based on care improvement expectations in their local system. In Model 2, CMS takes 2% off the target price for 90-day episodes and 3% off the target price for 30- and 60-day episodes, making it all the more important to choose bundles that demonstrate a high likelihood of success.
The revenue cycle for hospitals and physicians in the program does not change. They submit claims for their services and receive reimbursement as they always have; however, after the end of each quarter, when the majority of part A and B claims have been processed, a “look back” at actual spending for all participating episodes is reconciled against the baseline price derived from 2009-2012. If there is a net savings compared to the baseline, monies can be distributed to the participating providers—the hospital or physician practice—and those providers may further share some of the savings with other physicians/providers who have signed a gainsharing contract.
Hospitalists and BPCI
Hospitalist practices participate in the CMS program either as episode initiators or gainsharers. As episode initiators, they “own” the bundle, which means they bear economic risk for the program. In this capacity, overall savings will mean the hospitalist practice has a new revenue stream, which could be substantial; however, the practice is also responsible for any losses.
Other hospitalist practices have become gainsharers in the program, which means they have signed an agreement enabling them to receive payments in addition to professional fee revenues for activities that reduce costs while maintaining or improving quality. Such activities are referred to as “care redesign” in the program. Gainsharers do not bear financial risk.
Where Will Savings Come From?
Perhaps ironically for hospitalists, the main source of savings in the BPCI program comes from post-acute care and readmissions. For example, for common conditions like heart failure, COPD, and pneumonia, Medicare spends almost as much on post-acute care and readmissions in the first 30 days after discharge as it does on the index hospitalization.1 As a result, the BPCI program adds further emphasis on preventing readmissions when added to existing pressures, and there is a new premium placed on “right-sizing” the usage of SNF and other post-acute facilities, such as inpatient rehabilitation and long-term acute care hospitals. For hospitalists, this means that new rigor is needed to connect to the post-acute setting, such as determining why a patient is being discharged to a skilled facility.
Another savings pool, called “internal cost savings,” is available to reward decreasing inpatient utilization from, for example, testing, imaging, and implantable devices.
Conclusion
Bundled payment might be the biggest thing to come along for hospitalists since the patient safety movement launched some 16 years ago. Why? Although accountable care organizations have largely focused on ambulatory practice, bundled payment has a major focus on hospital care and on the post-acute care decisions that are made during the hospitalization. If bundled payment proves to be an effective way to pay for—and organize—care, hospitalists will play a central role in the success of this innovation.
In part two of this series, I will explore specific roles hospitalists play in successful bundled payment programs.