User login
A 60-year-old African American woman who had congestive heart failure (CHF) with reduced ejection fraction, untreated hepatitis C virus infection, and chronic kidney disease presented to the emergency department (ED) with a 6-month history of bilateral lower extremity edema. Use of diuretics and antibiotic therapy for suspected CHF exacerbation and cellulitis, directed by her primary care physician, had no effect. In the month prior to presenting to the ED, the patient took 2 different antibiotics, each for 10 days: clindamycin 300 mg every 6 hours and doxycycline 100 mg every 12 hours. Additionally, she was taking furosemide 40 mg/d with good urine output, but no appreciable improvement in lower extremity edema.
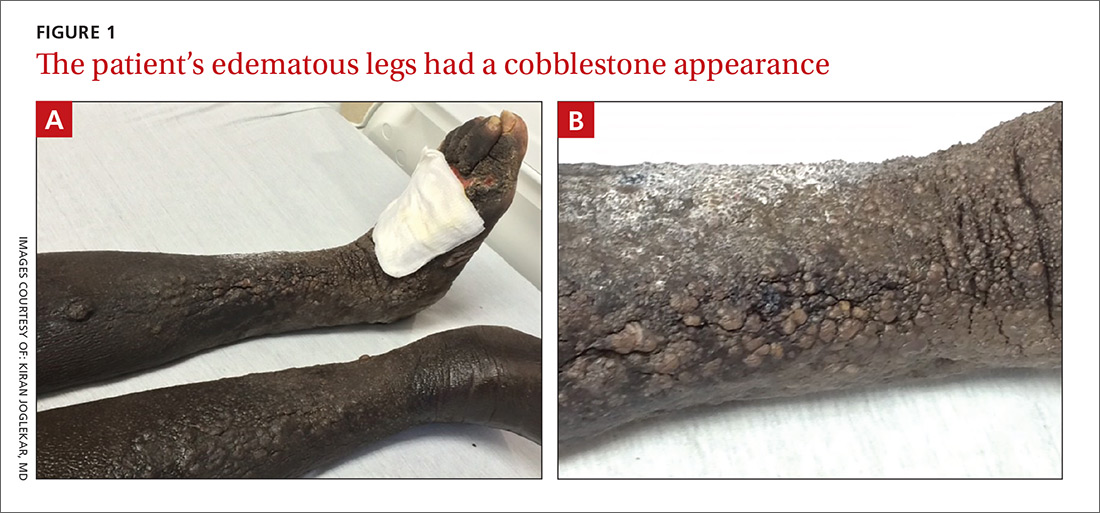
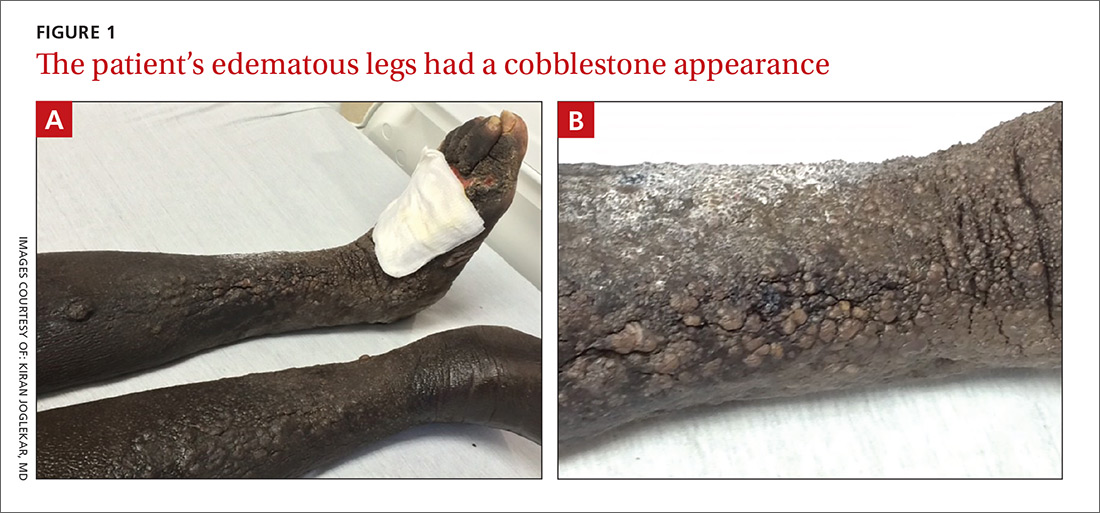
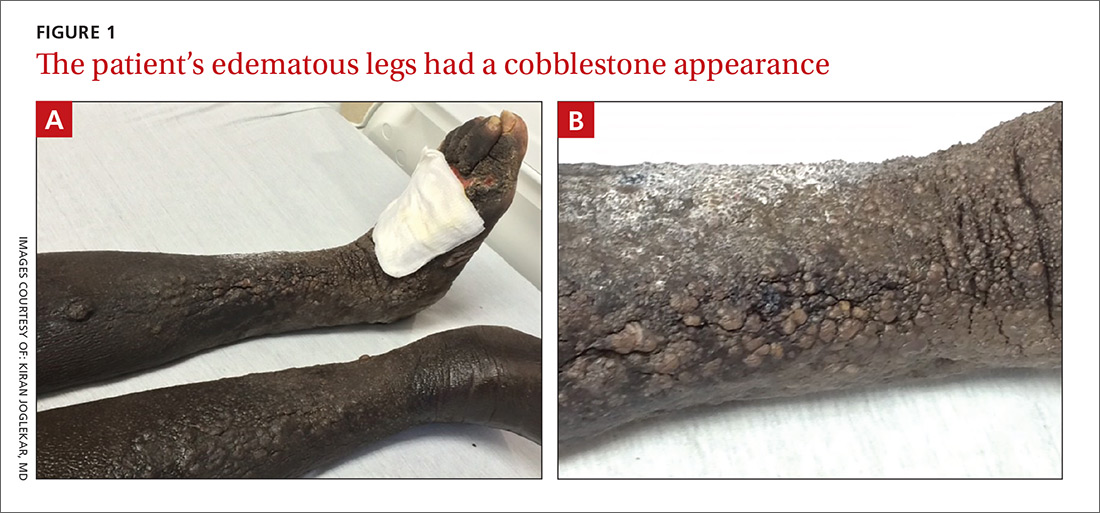
The physical examination revealed bilateral nonpitting edema. Weeping pearly papules, xerotic skin, and a cobblestone appearance extended from the dorsa of the patient’s feet to her knees (FIGURES 1A and 1B). The patient underwent Doppler ultrasound of the lower extremities and a skin biopsy.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Elephantiasis nostras verrucosa
The Doppler ultrasound was negative, and the biopsy ruled out malignancy and infection; however, the pathology report was histologically consistent with a diagnosis of elephantiasis nostras verrucosa (ENV).
ENV is a disfiguring, nonfilarial lymphedema that affects the lower extremities and is characterized by progressive cobblestoning and verrucous distortion of gravity-dependent areas.1 The skin changes are caused by lymphatic damage and obstruction from an accumulation of protein-rich fluid in the dermis and subcutaneous tissues.1,2
The term ENV was first coined by Aldo Castellani in 1934 to differentiate the condition from elephantiasis tropica (filariasis), which is caused by parasitic Wuchereria worms.3 ENV is also known as lymphangitis recurrens elephantogenica, elephantiasis verrucosa, elephantiasis nostra, mossy leg, and elephantiasis of the temperate zone.1
ENV is notably uncommon; its exact incidence is unknown. The etiology is multifactorial but can include obesity, chronic lymphedema, CHF, and recurrent cellulitis (the latter 2 were noted in our patient’s history).1
Although the diagnosis can be made based on patient history and physical examination alone, skin biopsy is warranted to rule out underlying malignancy or fungal infection.1,4 Histologic findings suggestive of ENV include pseudoepitheliomatous hyperplasia, lymph channel dilation, widened tissue spaces, and loss of dermal papillae.1 In our patient’s case, the pathology report revealed dermal fibrosis, dilated lymph channels, and a mixed inflammatory infiltrate. Her lab work, which included a complete blood count and basic metabolic panel, was significant for neutrophilic leukocytosis (white blood cell count, 30,000 cells/mcL), chronic kidney disease, and elevated inflammatory markers.
The differential includes other types of edema and infections
Several other diseases must be differentiated from ENV, including:
Venous stasis dermatitis. Unlike ENV, this condition involves pitting edema with erythema and does not have a verrucous appearance.2,4
Lipedema. Histologically, lipedema shows no changes. It typically spares the feet, has an early age of onset, and is associated with a positive family history.1,2,4
Lipodermatosclerosis. This condition is caused by venous stasis with swelling of the proximal lower extremity and fibrosis of the distal parts. The affected leg develops an “inverted wine bottle” appearance.2,4
Pretibial myxedema. Patients with pretibial myxedema will have thyroid function test abnormalities and exhibit other signs of hyperthyroidism. If suspected, the laboratory evaluation should include thyroid-stimulating hormone levels.2,4
Filariasis. Endemic to tropical regions, filariasis is a parasitic infection. A travel history helps to differentiate this from ENV. If suspected, include a Giemsa blood smear in the laboratory evaluation.2
Chromoblastomycosis. This chronic fungal infection is typically contracted in rural tropical or subtropical regions. The causative fungi, which are present in soil, enter the skin through minor wounds (eg, thorns or splinters). The wounds are typically forgotten by the time the patient seeks medical attention. Biopsy can effectively rule out this condition.1,2,5
Treatment centers on preserving function, preventing complications
Currently, no standard treatment exists for ENV.1,4 Therapies are aimed at treating the underlying cause, preserving function in the affected limb, and preventing complications. Conservative therapy includes elevation of the affected limb and use of compression devices for edema. Antibiotics can be administered for associated cellulitis. There have been few case reports of successful treatment with oral retinoids. If medical therapy fails, surgical debridement serves as a last resort.1,4,6
Our patient improved after a week with antibiotic therapy (IV piperacillin/tazobactam 3.375 g every 6 hours) and other conservative measures, such as leg elevation.
CORRESPONDENCE
Kavita Natrajan, MBBS, George Washington University/Medical Faculty Associates, Division of Hematology and Oncology, 2150 Pennsylvania Avenue NW, DC 20037; [email protected].
1. Sisto K, Khachemoune A. Elephantiasis nostras verrucosa: a review. Am J Clin Dermatol. 2008;9:141-146.
2. Liaw FY, Huang CF, Wu YC, et al. Elephantiasis nostras verrucosa: swelling with verrucose appearance of lower limbs. Can Fam Physician. 2012;58:e551-e553.
3. Castellani A. Researches on elephantiasis nostras and elephantiasis tropica with special regard to their initial stage of recurring lymphangitis (lymphangitis recurrens elephantogenica). J Trop Med Hyg. 1969;72:89-97.
4. Baird D, Bode D, Akers T, et al. Elephantiasis nostras verrucosa (ENV): a complication of congestive heart failure and obesity. J Am Board Fam Med. 2010;23:413-417.
5. Queiroz-Telles F, Fahal AH, Falci R, et. al. Neglected endemic mycoses. Lancet Inf Dis. 2017;17:e367-e377.
6. Han HH, Lim SY, Oh DY. Successful surgical treatment for elephantiasis nostras verrucosa using a new designed column flap. Int J Low Extrem Wounds. 2015;14:299-302.
A 60-year-old African American woman who had congestive heart failure (CHF) with reduced ejection fraction, untreated hepatitis C virus infection, and chronic kidney disease presented to the emergency department (ED) with a 6-month history of bilateral lower extremity edema. Use of diuretics and antibiotic therapy for suspected CHF exacerbation and cellulitis, directed by her primary care physician, had no effect. In the month prior to presenting to the ED, the patient took 2 different antibiotics, each for 10 days: clindamycin 300 mg every 6 hours and doxycycline 100 mg every 12 hours. Additionally, she was taking furosemide 40 mg/d with good urine output, but no appreciable improvement in lower extremity edema.
The physical examination revealed bilateral nonpitting edema. Weeping pearly papules, xerotic skin, and a cobblestone appearance extended from the dorsa of the patient’s feet to her knees (FIGURES 1A and 1B). The patient underwent Doppler ultrasound of the lower extremities and a skin biopsy.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Elephantiasis nostras verrucosa
The Doppler ultrasound was negative, and the biopsy ruled out malignancy and infection; however, the pathology report was histologically consistent with a diagnosis of elephantiasis nostras verrucosa (ENV).
ENV is a disfiguring, nonfilarial lymphedema that affects the lower extremities and is characterized by progressive cobblestoning and verrucous distortion of gravity-dependent areas.1 The skin changes are caused by lymphatic damage and obstruction from an accumulation of protein-rich fluid in the dermis and subcutaneous tissues.1,2
The term ENV was first coined by Aldo Castellani in 1934 to differentiate the condition from elephantiasis tropica (filariasis), which is caused by parasitic Wuchereria worms.3 ENV is also known as lymphangitis recurrens elephantogenica, elephantiasis verrucosa, elephantiasis nostra, mossy leg, and elephantiasis of the temperate zone.1
ENV is notably uncommon; its exact incidence is unknown. The etiology is multifactorial but can include obesity, chronic lymphedema, CHF, and recurrent cellulitis (the latter 2 were noted in our patient’s history).1
Although the diagnosis can be made based on patient history and physical examination alone, skin biopsy is warranted to rule out underlying malignancy or fungal infection.1,4 Histologic findings suggestive of ENV include pseudoepitheliomatous hyperplasia, lymph channel dilation, widened tissue spaces, and loss of dermal papillae.1 In our patient’s case, the pathology report revealed dermal fibrosis, dilated lymph channels, and a mixed inflammatory infiltrate. Her lab work, which included a complete blood count and basic metabolic panel, was significant for neutrophilic leukocytosis (white blood cell count, 30,000 cells/mcL), chronic kidney disease, and elevated inflammatory markers.
The differential includes other types of edema and infections
Several other diseases must be differentiated from ENV, including:
Venous stasis dermatitis. Unlike ENV, this condition involves pitting edema with erythema and does not have a verrucous appearance.2,4
Lipedema. Histologically, lipedema shows no changes. It typically spares the feet, has an early age of onset, and is associated with a positive family history.1,2,4
Lipodermatosclerosis. This condition is caused by venous stasis with swelling of the proximal lower extremity and fibrosis of the distal parts. The affected leg develops an “inverted wine bottle” appearance.2,4
Pretibial myxedema. Patients with pretibial myxedema will have thyroid function test abnormalities and exhibit other signs of hyperthyroidism. If suspected, the laboratory evaluation should include thyroid-stimulating hormone levels.2,4
Filariasis. Endemic to tropical regions, filariasis is a parasitic infection. A travel history helps to differentiate this from ENV. If suspected, include a Giemsa blood smear in the laboratory evaluation.2
Chromoblastomycosis. This chronic fungal infection is typically contracted in rural tropical or subtropical regions. The causative fungi, which are present in soil, enter the skin through minor wounds (eg, thorns or splinters). The wounds are typically forgotten by the time the patient seeks medical attention. Biopsy can effectively rule out this condition.1,2,5
Treatment centers on preserving function, preventing complications
Currently, no standard treatment exists for ENV.1,4 Therapies are aimed at treating the underlying cause, preserving function in the affected limb, and preventing complications. Conservative therapy includes elevation of the affected limb and use of compression devices for edema. Antibiotics can be administered for associated cellulitis. There have been few case reports of successful treatment with oral retinoids. If medical therapy fails, surgical debridement serves as a last resort.1,4,6
Our patient improved after a week with antibiotic therapy (IV piperacillin/tazobactam 3.375 g every 6 hours) and other conservative measures, such as leg elevation.
CORRESPONDENCE
Kavita Natrajan, MBBS, George Washington University/Medical Faculty Associates, Division of Hematology and Oncology, 2150 Pennsylvania Avenue NW, DC 20037; [email protected].
A 60-year-old African American woman who had congestive heart failure (CHF) with reduced ejection fraction, untreated hepatitis C virus infection, and chronic kidney disease presented to the emergency department (ED) with a 6-month history of bilateral lower extremity edema. Use of diuretics and antibiotic therapy for suspected CHF exacerbation and cellulitis, directed by her primary care physician, had no effect. In the month prior to presenting to the ED, the patient took 2 different antibiotics, each for 10 days: clindamycin 300 mg every 6 hours and doxycycline 100 mg every 12 hours. Additionally, she was taking furosemide 40 mg/d with good urine output, but no appreciable improvement in lower extremity edema.
The physical examination revealed bilateral nonpitting edema. Weeping pearly papules, xerotic skin, and a cobblestone appearance extended from the dorsa of the patient’s feet to her knees (FIGURES 1A and 1B). The patient underwent Doppler ultrasound of the lower extremities and a skin biopsy.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Elephantiasis nostras verrucosa
The Doppler ultrasound was negative, and the biopsy ruled out malignancy and infection; however, the pathology report was histologically consistent with a diagnosis of elephantiasis nostras verrucosa (ENV).
ENV is a disfiguring, nonfilarial lymphedema that affects the lower extremities and is characterized by progressive cobblestoning and verrucous distortion of gravity-dependent areas.1 The skin changes are caused by lymphatic damage and obstruction from an accumulation of protein-rich fluid in the dermis and subcutaneous tissues.1,2
The term ENV was first coined by Aldo Castellani in 1934 to differentiate the condition from elephantiasis tropica (filariasis), which is caused by parasitic Wuchereria worms.3 ENV is also known as lymphangitis recurrens elephantogenica, elephantiasis verrucosa, elephantiasis nostra, mossy leg, and elephantiasis of the temperate zone.1
ENV is notably uncommon; its exact incidence is unknown. The etiology is multifactorial but can include obesity, chronic lymphedema, CHF, and recurrent cellulitis (the latter 2 were noted in our patient’s history).1
Although the diagnosis can be made based on patient history and physical examination alone, skin biopsy is warranted to rule out underlying malignancy or fungal infection.1,4 Histologic findings suggestive of ENV include pseudoepitheliomatous hyperplasia, lymph channel dilation, widened tissue spaces, and loss of dermal papillae.1 In our patient’s case, the pathology report revealed dermal fibrosis, dilated lymph channels, and a mixed inflammatory infiltrate. Her lab work, which included a complete blood count and basic metabolic panel, was significant for neutrophilic leukocytosis (white blood cell count, 30,000 cells/mcL), chronic kidney disease, and elevated inflammatory markers.
The differential includes other types of edema and infections
Several other diseases must be differentiated from ENV, including:
Venous stasis dermatitis. Unlike ENV, this condition involves pitting edema with erythema and does not have a verrucous appearance.2,4
Lipedema. Histologically, lipedema shows no changes. It typically spares the feet, has an early age of onset, and is associated with a positive family history.1,2,4
Lipodermatosclerosis. This condition is caused by venous stasis with swelling of the proximal lower extremity and fibrosis of the distal parts. The affected leg develops an “inverted wine bottle” appearance.2,4
Pretibial myxedema. Patients with pretibial myxedema will have thyroid function test abnormalities and exhibit other signs of hyperthyroidism. If suspected, the laboratory evaluation should include thyroid-stimulating hormone levels.2,4
Filariasis. Endemic to tropical regions, filariasis is a parasitic infection. A travel history helps to differentiate this from ENV. If suspected, include a Giemsa blood smear in the laboratory evaluation.2
Chromoblastomycosis. This chronic fungal infection is typically contracted in rural tropical or subtropical regions. The causative fungi, which are present in soil, enter the skin through minor wounds (eg, thorns or splinters). The wounds are typically forgotten by the time the patient seeks medical attention. Biopsy can effectively rule out this condition.1,2,5
Treatment centers on preserving function, preventing complications
Currently, no standard treatment exists for ENV.1,4 Therapies are aimed at treating the underlying cause, preserving function in the affected limb, and preventing complications. Conservative therapy includes elevation of the affected limb and use of compression devices for edema. Antibiotics can be administered for associated cellulitis. There have been few case reports of successful treatment with oral retinoids. If medical therapy fails, surgical debridement serves as a last resort.1,4,6
Our patient improved after a week with antibiotic therapy (IV piperacillin/tazobactam 3.375 g every 6 hours) and other conservative measures, such as leg elevation.
CORRESPONDENCE
Kavita Natrajan, MBBS, George Washington University/Medical Faculty Associates, Division of Hematology and Oncology, 2150 Pennsylvania Avenue NW, DC 20037; [email protected].
1. Sisto K, Khachemoune A. Elephantiasis nostras verrucosa: a review. Am J Clin Dermatol. 2008;9:141-146.
2. Liaw FY, Huang CF, Wu YC, et al. Elephantiasis nostras verrucosa: swelling with verrucose appearance of lower limbs. Can Fam Physician. 2012;58:e551-e553.
3. Castellani A. Researches on elephantiasis nostras and elephantiasis tropica with special regard to their initial stage of recurring lymphangitis (lymphangitis recurrens elephantogenica). J Trop Med Hyg. 1969;72:89-97.
4. Baird D, Bode D, Akers T, et al. Elephantiasis nostras verrucosa (ENV): a complication of congestive heart failure and obesity. J Am Board Fam Med. 2010;23:413-417.
5. Queiroz-Telles F, Fahal AH, Falci R, et. al. Neglected endemic mycoses. Lancet Inf Dis. 2017;17:e367-e377.
6. Han HH, Lim SY, Oh DY. Successful surgical treatment for elephantiasis nostras verrucosa using a new designed column flap. Int J Low Extrem Wounds. 2015;14:299-302.
1. Sisto K, Khachemoune A. Elephantiasis nostras verrucosa: a review. Am J Clin Dermatol. 2008;9:141-146.
2. Liaw FY, Huang CF, Wu YC, et al. Elephantiasis nostras verrucosa: swelling with verrucose appearance of lower limbs. Can Fam Physician. 2012;58:e551-e553.
3. Castellani A. Researches on elephantiasis nostras and elephantiasis tropica with special regard to their initial stage of recurring lymphangitis (lymphangitis recurrens elephantogenica). J Trop Med Hyg. 1969;72:89-97.
4. Baird D, Bode D, Akers T, et al. Elephantiasis nostras verrucosa (ENV): a complication of congestive heart failure and obesity. J Am Board Fam Med. 2010;23:413-417.
5. Queiroz-Telles F, Fahal AH, Falci R, et. al. Neglected endemic mycoses. Lancet Inf Dis. 2017;17:e367-e377.
6. Han HH, Lim SY, Oh DY. Successful surgical treatment for elephantiasis nostras verrucosa using a new designed column flap. Int J Low Extrem Wounds. 2015;14:299-302.
