User login
Images courtesy Dr. Michael Davidson
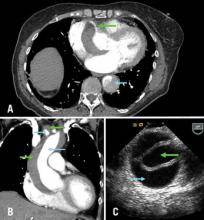
A) Axial CT chest at level of aortic root: green arrow = right coronary artery filling from true lumen, traversing false lumen; blue arrow = dissection in descending thoracic aorta; B) CT chest coronal reconstruction; blue arrows = true lumen in ascending aorta and innominate artery opacified with intravenous contrast; green arrows = false lumen; C) Transesophageal echocardiography of ascending aorta; green arrow= true lumen, blue arrow = false lumen.
BTX
A 71-year-old female with known ascending aortic aneurysm previously 4.5 cm presents to the emergency room with sharp chest pain of acute onset radiating to her back. She has diminished right radial and left femoral pulses. Chest x-ray shows a moderately widened mediastinum. Representative images are shown from the computed tomography of chest with contrast and a transesophageal echo with views of the ascending aorta.
Directed questions:
1. What is the diagnosis?
2. What are the two most common classification systems of this disease process?
3. What is the mortality associated with this diagnosis?
4. What is the best method of diagnosis in a stable patient? In an unstable patient?
5. What is the recommended treatment strategy?
6. What options are available for arterial cannulation?
Answers to the Clinical Challenge
1) Acute Aortic dissection of the ascending aorta, aortic arch and descending aorta
2) Stanford system (A=ascending arch, B=descending arch), Debakey system (I=ascending, arch and descending aorta, II - ascending aorta only, III - descending aorta only)
3) An acute type A dissection has been classically described as having a mortality of 1% per hour. Common causes of death are aortic free rupture, pericardial tamponade, acute aortic regurgitation, acute myocardial ischemia from coronary malperfusion.
4) In a stable patient, computed tomography with intravenous contrast is best due its ease and a sensitivity and a specificity nearing 90-100%. In unstable patients transesophageal echocardiography in the operating room is an excellent strategy for diagnosis to avoid delay in definitive surgical repair.
5) Initial medical management is aimed at control of blood pressure and pain. Esmolol and nitroprusside are good options. Unstable patients belong in the operating room and all delays should be avoided. Surgical repair is indicated in nearly all type A acute aortic dissections except maybe in the highest risk patients. At surgery, the ascending aorta, the aortic root, aortic valve, coronary arteries, aortic arch and arch vessels must all be assessed and repaired or replaced as necessary. As dissections frequently will extend into the arch, a short period of deep hypothermic circulatory arrest is common.
6) Most commonly, peripheral arterial cannulation is performed via the femoral or axillary artery. Care must be taken if dissection into the peripheral vessels is suspected. The ascending aorta may be cannulated but one must ensure perfusion through the true lumen. Transapical cannulation has been described as well. Transesophageal echocardiography can be used to guide cannulation placement into the ascending aorta.
Selected References and Additional Resources:
Bolman, R. Acute Type A Aortic Dissection. Operative Techniques in Thoracic and Cardiovascular Surgery. 14(2):124, 2009.
Coady MA, et al. Natural history, pathogenesis, and etiology of thoracic aortic aneurysms and dissections. Cardiology Clinics. 17:615, 1999.
Sabik JF, et al: Long-term effectiveness of operations for ascending aortic dissections. J Thorac Cardiovasc Surg. 119:946, 2000.
Safi HJ, Miller CC 3rd, Reardon MJ, et al: Operation for acute and chronic aortic dissection: Recent outcome with regard to neurologic deficit and early death. Ann Thorac Surg 1998; 66:402
TSDAWeekly Curriculum - "Acute Aortic Dissection" http://tsda.org/documents/PDF/Weekly%20Curricula/E-mail%20Archive/03.11.10.pdf
Images courtesy Dr. Michael Davidson
A) Axial CT chest at level of aortic root: green arrow = right coronary artery filling from true lumen, traversing false lumen; blue arrow = dissection in descending thoracic aorta; B) CT chest coronal reconstruction; blue arrows = true lumen in ascending aorta and innominate artery opacified with intravenous contrast; green arrows = false lumen; C) Transesophageal echocardiography of ascending aorta; green arrow= true lumen, blue arrow = false lumen.
BTX
A 71-year-old female with known ascending aortic aneurysm previously 4.5 cm presents to the emergency room with sharp chest pain of acute onset radiating to her back. She has diminished right radial and left femoral pulses. Chest x-ray shows a moderately widened mediastinum. Representative images are shown from the computed tomography of chest with contrast and a transesophageal echo with views of the ascending aorta.
Directed questions:
1. What is the diagnosis?
2. What are the two most common classification systems of this disease process?
3. What is the mortality associated with this diagnosis?
4. What is the best method of diagnosis in a stable patient? In an unstable patient?
5. What is the recommended treatment strategy?
6. What options are available for arterial cannulation?
Answers to the Clinical Challenge
1) Acute Aortic dissection of the ascending aorta, aortic arch and descending aorta
2) Stanford system (A=ascending arch, B=descending arch), Debakey system (I=ascending, arch and descending aorta, II - ascending aorta only, III - descending aorta only)
3) An acute type A dissection has been classically described as having a mortality of 1% per hour. Common causes of death are aortic free rupture, pericardial tamponade, acute aortic regurgitation, acute myocardial ischemia from coronary malperfusion.
4) In a stable patient, computed tomography with intravenous contrast is best due its ease and a sensitivity and a specificity nearing 90-100%. In unstable patients transesophageal echocardiography in the operating room is an excellent strategy for diagnosis to avoid delay in definitive surgical repair.
5) Initial medical management is aimed at control of blood pressure and pain. Esmolol and nitroprusside are good options. Unstable patients belong in the operating room and all delays should be avoided. Surgical repair is indicated in nearly all type A acute aortic dissections except maybe in the highest risk patients. At surgery, the ascending aorta, the aortic root, aortic valve, coronary arteries, aortic arch and arch vessels must all be assessed and repaired or replaced as necessary. As dissections frequently will extend into the arch, a short period of deep hypothermic circulatory arrest is common.
6) Most commonly, peripheral arterial cannulation is performed via the femoral or axillary artery. Care must be taken if dissection into the peripheral vessels is suspected. The ascending aorta may be cannulated but one must ensure perfusion through the true lumen. Transapical cannulation has been described as well. Transesophageal echocardiography can be used to guide cannulation placement into the ascending aorta.
Selected References and Additional Resources:
Bolman, R. Acute Type A Aortic Dissection. Operative Techniques in Thoracic and Cardiovascular Surgery. 14(2):124, 2009.
Coady MA, et al. Natural history, pathogenesis, and etiology of thoracic aortic aneurysms and dissections. Cardiology Clinics. 17:615, 1999.
Sabik JF, et al: Long-term effectiveness of operations for ascending aortic dissections. J Thorac Cardiovasc Surg. 119:946, 2000.
Safi HJ, Miller CC 3rd, Reardon MJ, et al: Operation for acute and chronic aortic dissection: Recent outcome with regard to neurologic deficit and early death. Ann Thorac Surg 1998; 66:402
TSDAWeekly Curriculum - "Acute Aortic Dissection" http://tsda.org/documents/PDF/Weekly%20Curricula/E-mail%20Archive/03.11.10.pdf
Images courtesy Dr. Michael Davidson
A) Axial CT chest at level of aortic root: green arrow = right coronary artery filling from true lumen, traversing false lumen; blue arrow = dissection in descending thoracic aorta; B) CT chest coronal reconstruction; blue arrows = true lumen in ascending aorta and innominate artery opacified with intravenous contrast; green arrows = false lumen; C) Transesophageal echocardiography of ascending aorta; green arrow= true lumen, blue arrow = false lumen.
BTX
A 71-year-old female with known ascending aortic aneurysm previously 4.5 cm presents to the emergency room with sharp chest pain of acute onset radiating to her back. She has diminished right radial and left femoral pulses. Chest x-ray shows a moderately widened mediastinum. Representative images are shown from the computed tomography of chest with contrast and a transesophageal echo with views of the ascending aorta.
Directed questions:
1. What is the diagnosis?
2. What are the two most common classification systems of this disease process?
3. What is the mortality associated with this diagnosis?
4. What is the best method of diagnosis in a stable patient? In an unstable patient?
5. What is the recommended treatment strategy?
6. What options are available for arterial cannulation?
Answers to the Clinical Challenge
1) Acute Aortic dissection of the ascending aorta, aortic arch and descending aorta
2) Stanford system (A=ascending arch, B=descending arch), Debakey system (I=ascending, arch and descending aorta, II - ascending aorta only, III - descending aorta only)
3) An acute type A dissection has been classically described as having a mortality of 1% per hour. Common causes of death are aortic free rupture, pericardial tamponade, acute aortic regurgitation, acute myocardial ischemia from coronary malperfusion.
4) In a stable patient, computed tomography with intravenous contrast is best due its ease and a sensitivity and a specificity nearing 90-100%. In unstable patients transesophageal echocardiography in the operating room is an excellent strategy for diagnosis to avoid delay in definitive surgical repair.
5) Initial medical management is aimed at control of blood pressure and pain. Esmolol and nitroprusside are good options. Unstable patients belong in the operating room and all delays should be avoided. Surgical repair is indicated in nearly all type A acute aortic dissections except maybe in the highest risk patients. At surgery, the ascending aorta, the aortic root, aortic valve, coronary arteries, aortic arch and arch vessels must all be assessed and repaired or replaced as necessary. As dissections frequently will extend into the arch, a short period of deep hypothermic circulatory arrest is common.
6) Most commonly, peripheral arterial cannulation is performed via the femoral or axillary artery. Care must be taken if dissection into the peripheral vessels is suspected. The ascending aorta may be cannulated but one must ensure perfusion through the true lumen. Transapical cannulation has been described as well. Transesophageal echocardiography can be used to guide cannulation placement into the ascending aorta.
Selected References and Additional Resources:
Bolman, R. Acute Type A Aortic Dissection. Operative Techniques in Thoracic and Cardiovascular Surgery. 14(2):124, 2009.
Coady MA, et al. Natural history, pathogenesis, and etiology of thoracic aortic aneurysms and dissections. Cardiology Clinics. 17:615, 1999.
Sabik JF, et al: Long-term effectiveness of operations for ascending aortic dissections. J Thorac Cardiovasc Surg. 119:946, 2000.
Safi HJ, Miller CC 3rd, Reardon MJ, et al: Operation for acute and chronic aortic dissection: Recent outcome with regard to neurologic deficit and early death. Ann Thorac Surg 1998; 66:402
TSDAWeekly Curriculum - "Acute Aortic Dissection" http://tsda.org/documents/PDF/Weekly%20Curricula/E-mail%20Archive/03.11.10.pdf