User login
Reflections on women in surgery
As I reflect upon the past year, 2018 has certainly made a mark for addressing burnout among medical professionals, enforcing wellness, and targeting implicit and explicit gender bias in medicine and surgery.
Looking back, I entered surgery with a dream to change the culture of surgery. I knew I didn’t fit the traditional mold of an aggressive or arrogant surgeon. But I thought that my empathetic, open, and compassionate ways may spark a change in paradigm for that traditional surgical ideology. However, what I encountered as I made my way on this long, ever-winding journey was a system, culture, and tradition that beats you down, and what I thought were my strengths were quickly turned into weaknesses. As I grew and matured, this loss of identity in a culture of depersonalization surrounded by gender bias, for me, was a perfect recipe leading straight to burnout. However, this was an impetus for change, to be that voice and spark for a cultural transformation of surgery and for the women who work in the specialty.
More women are entering medical and surgical specialties. However, despite the advances made there are still clear gender-based disparities influencing overall wellness and work satisfaction. For instance, a study by Meyerson et al. demonstrated that female residents receive less operating room autonomy than male ones. I see it daily within my own curriculum and in observing other female residents in other surgical specialties. Furthermore, female residents are less often introduced by their physician titles, compared with their male counterparts, are often confused as nonphysicians, and are perceived as being less competent. This influences, to no small extent, overall confidence. It’s discouraging and disheartening to have worked so hard and yet still be treated in a sexist paradigm. And to top it all off, female physicians face a motherhood penalty.
In a recent study by Magudia et al., out of 12 top medical institutions that provided maternity leave, only 8 did so for residents with a grant total of 6.6 weeks on average. Furthermore, women with children or women who plan to have children have constrained career opportunities and are less likely to get full professorship or leadership positions. Anecdotally, a surgeon in passing semijokingly told me that if I were to take a specific academic vascular position, I may have to sign an agreement not to get pregnant ... probably not the job for me.
It’s appalling that, in this day and age, these explicit beliefs still exist, but what scares me more are all the implicit unconscious biases that affect all women not only in surgery but in medicine as well.
Looking back, 2018 is a year of beginning difficult conversations about physician and surgeon wellness, burnout, and gender bias. What’s obvious is that there is a hell of a lot of work to do. But change is slowly starting. We are now recognizing what the issues are, and the next step is to take action. It’s difficult to steer big ships, but there is an active community investing in strategies to improve the cultural scope of surgery and supporting and valuing women and what they have to offer.
References
Magudia K et al. JAMA. 2018;320(22):2372-4.
Meyerson SL et al. J Surg Educ. 2017;74(6):e111-18.
Dr. Drudi is a vascular surgery resident at McGill University, Montreal, and the resident medical editor of Vascular Specialist.
As I reflect upon the past year, 2018 has certainly made a mark for addressing burnout among medical professionals, enforcing wellness, and targeting implicit and explicit gender bias in medicine and surgery.
Looking back, I entered surgery with a dream to change the culture of surgery. I knew I didn’t fit the traditional mold of an aggressive or arrogant surgeon. But I thought that my empathetic, open, and compassionate ways may spark a change in paradigm for that traditional surgical ideology. However, what I encountered as I made my way on this long, ever-winding journey was a system, culture, and tradition that beats you down, and what I thought were my strengths were quickly turned into weaknesses. As I grew and matured, this loss of identity in a culture of depersonalization surrounded by gender bias, for me, was a perfect recipe leading straight to burnout. However, this was an impetus for change, to be that voice and spark for a cultural transformation of surgery and for the women who work in the specialty.
More women are entering medical and surgical specialties. However, despite the advances made there are still clear gender-based disparities influencing overall wellness and work satisfaction. For instance, a study by Meyerson et al. demonstrated that female residents receive less operating room autonomy than male ones. I see it daily within my own curriculum and in observing other female residents in other surgical specialties. Furthermore, female residents are less often introduced by their physician titles, compared with their male counterparts, are often confused as nonphysicians, and are perceived as being less competent. This influences, to no small extent, overall confidence. It’s discouraging and disheartening to have worked so hard and yet still be treated in a sexist paradigm. And to top it all off, female physicians face a motherhood penalty.
In a recent study by Magudia et al., out of 12 top medical institutions that provided maternity leave, only 8 did so for residents with a grant total of 6.6 weeks on average. Furthermore, women with children or women who plan to have children have constrained career opportunities and are less likely to get full professorship or leadership positions. Anecdotally, a surgeon in passing semijokingly told me that if I were to take a specific academic vascular position, I may have to sign an agreement not to get pregnant ... probably not the job for me.
It’s appalling that, in this day and age, these explicit beliefs still exist, but what scares me more are all the implicit unconscious biases that affect all women not only in surgery but in medicine as well.
Looking back, 2018 is a year of beginning difficult conversations about physician and surgeon wellness, burnout, and gender bias. What’s obvious is that there is a hell of a lot of work to do. But change is slowly starting. We are now recognizing what the issues are, and the next step is to take action. It’s difficult to steer big ships, but there is an active community investing in strategies to improve the cultural scope of surgery and supporting and valuing women and what they have to offer.
References
Magudia K et al. JAMA. 2018;320(22):2372-4.
Meyerson SL et al. J Surg Educ. 2017;74(6):e111-18.
Dr. Drudi is a vascular surgery resident at McGill University, Montreal, and the resident medical editor of Vascular Specialist.
As I reflect upon the past year, 2018 has certainly made a mark for addressing burnout among medical professionals, enforcing wellness, and targeting implicit and explicit gender bias in medicine and surgery.
Looking back, I entered surgery with a dream to change the culture of surgery. I knew I didn’t fit the traditional mold of an aggressive or arrogant surgeon. But I thought that my empathetic, open, and compassionate ways may spark a change in paradigm for that traditional surgical ideology. However, what I encountered as I made my way on this long, ever-winding journey was a system, culture, and tradition that beats you down, and what I thought were my strengths were quickly turned into weaknesses. As I grew and matured, this loss of identity in a culture of depersonalization surrounded by gender bias, for me, was a perfect recipe leading straight to burnout. However, this was an impetus for change, to be that voice and spark for a cultural transformation of surgery and for the women who work in the specialty.
More women are entering medical and surgical specialties. However, despite the advances made there are still clear gender-based disparities influencing overall wellness and work satisfaction. For instance, a study by Meyerson et al. demonstrated that female residents receive less operating room autonomy than male ones. I see it daily within my own curriculum and in observing other female residents in other surgical specialties. Furthermore, female residents are less often introduced by their physician titles, compared with their male counterparts, are often confused as nonphysicians, and are perceived as being less competent. This influences, to no small extent, overall confidence. It’s discouraging and disheartening to have worked so hard and yet still be treated in a sexist paradigm. And to top it all off, female physicians face a motherhood penalty.
In a recent study by Magudia et al., out of 12 top medical institutions that provided maternity leave, only 8 did so for residents with a grant total of 6.6 weeks on average. Furthermore, women with children or women who plan to have children have constrained career opportunities and are less likely to get full professorship or leadership positions. Anecdotally, a surgeon in passing semijokingly told me that if I were to take a specific academic vascular position, I may have to sign an agreement not to get pregnant ... probably not the job for me.
It’s appalling that, in this day and age, these explicit beliefs still exist, but what scares me more are all the implicit unconscious biases that affect all women not only in surgery but in medicine as well.
Looking back, 2018 is a year of beginning difficult conversations about physician and surgeon wellness, burnout, and gender bias. What’s obvious is that there is a hell of a lot of work to do. But change is slowly starting. We are now recognizing what the issues are, and the next step is to take action. It’s difficult to steer big ships, but there is an active community investing in strategies to improve the cultural scope of surgery and supporting and valuing women and what they have to offer.
References
Magudia K et al. JAMA. 2018;320(22):2372-4.
Meyerson SL et al. J Surg Educ. 2017;74(6):e111-18.
Dr. Drudi is a vascular surgery resident at McGill University, Montreal, and the resident medical editor of Vascular Specialist.
Taking a leap of faith
After a grueling first two years of surgical residency, I welcomed with open arms my surgical research years. Junior surgical residency was arguably the toughest years of my training to date. Long hours at the hospital; the uncertainty of being called in to the hospital when on-call, which led to chronic anxiety and at times insomnia; and the pressures I put on myself to excel in all aspects of my training were draining, to say the least.
Of course, when it came time to leave my clinical responsibilities and pursue my Master’s degree, I was overcome with relief. First, I got my life back on track, leading a life of optimal nutrition, physical activity, and sleep and exploring different horizons in surgery.
Second, this time allowed me to grow as a person, learning techniques to remain calm in the face of adversity, to take at least 10 minutes a day for mindfulness, and to be cognizant and gauge when I am creeping upon that tipping point. I believe the key to success and happiness is to keep re-evaluating and being honest with ourselves, our happiness, our stresses, and our anxieties and to reach out to pillars of support, whoever they may be.
And finally, we are fundamentally teachers and inspirations to the next generation of surgeons who will follow in our footsteps. By being open, encouraging, and sharing our enthusiasm for our specialty, our patients, and our research, we may see the seeds of the future flourish under our wings.
That being said, I am terrified of returning to vascular surgery. I know it will be a challenge transitioning to senior resident, and I am scared that the progress I made over these years in terms of wellness and wellbeing will regress; however, in the end, I have to take a leap of faith and hope it all pulls together ... seamlessly.
Dr. Drudi is a vascular surgery resident at McGill University, Montreal, and the resident medical editor of Vascular Specialist.
After a grueling first two years of surgical residency, I welcomed with open arms my surgical research years. Junior surgical residency was arguably the toughest years of my training to date. Long hours at the hospital; the uncertainty of being called in to the hospital when on-call, which led to chronic anxiety and at times insomnia; and the pressures I put on myself to excel in all aspects of my training were draining, to say the least.
Of course, when it came time to leave my clinical responsibilities and pursue my Master’s degree, I was overcome with relief. First, I got my life back on track, leading a life of optimal nutrition, physical activity, and sleep and exploring different horizons in surgery.
Second, this time allowed me to grow as a person, learning techniques to remain calm in the face of adversity, to take at least 10 minutes a day for mindfulness, and to be cognizant and gauge when I am creeping upon that tipping point. I believe the key to success and happiness is to keep re-evaluating and being honest with ourselves, our happiness, our stresses, and our anxieties and to reach out to pillars of support, whoever they may be.
And finally, we are fundamentally teachers and inspirations to the next generation of surgeons who will follow in our footsteps. By being open, encouraging, and sharing our enthusiasm for our specialty, our patients, and our research, we may see the seeds of the future flourish under our wings.
That being said, I am terrified of returning to vascular surgery. I know it will be a challenge transitioning to senior resident, and I am scared that the progress I made over these years in terms of wellness and wellbeing will regress; however, in the end, I have to take a leap of faith and hope it all pulls together ... seamlessly.
Dr. Drudi is a vascular surgery resident at McGill University, Montreal, and the resident medical editor of Vascular Specialist.
After a grueling first two years of surgical residency, I welcomed with open arms my surgical research years. Junior surgical residency was arguably the toughest years of my training to date. Long hours at the hospital; the uncertainty of being called in to the hospital when on-call, which led to chronic anxiety and at times insomnia; and the pressures I put on myself to excel in all aspects of my training were draining, to say the least.
Of course, when it came time to leave my clinical responsibilities and pursue my Master’s degree, I was overcome with relief. First, I got my life back on track, leading a life of optimal nutrition, physical activity, and sleep and exploring different horizons in surgery.
Second, this time allowed me to grow as a person, learning techniques to remain calm in the face of adversity, to take at least 10 minutes a day for mindfulness, and to be cognizant and gauge when I am creeping upon that tipping point. I believe the key to success and happiness is to keep re-evaluating and being honest with ourselves, our happiness, our stresses, and our anxieties and to reach out to pillars of support, whoever they may be.
And finally, we are fundamentally teachers and inspirations to the next generation of surgeons who will follow in our footsteps. By being open, encouraging, and sharing our enthusiasm for our specialty, our patients, and our research, we may see the seeds of the future flourish under our wings.
That being said, I am terrified of returning to vascular surgery. I know it will be a challenge transitioning to senior resident, and I am scared that the progress I made over these years in terms of wellness and wellbeing will regress; however, in the end, I have to take a leap of faith and hope it all pulls together ... seamlessly.
Dr. Drudi is a vascular surgery resident at McGill University, Montreal, and the resident medical editor of Vascular Specialist.
Residency is like an IRONMAN
At the end of my junior surgical residency years, I was in a pretty bad physical and mental space. With resident coverage shortages, long hours, chronic fatigue, and personal pressures to perform and shine, I wound up digging myself into a hole, heading straight to resident burnout. Although there were others around me experiencing similar environmental stressors, I certainly felt alone – not knowing how to climb out of the hole I created for myself.
This was probably the lowest I have been in my life, but I finally got myself back on track. Coming from a fairly physically active background, I returned to a life of proper nutrition and physical activity. I began swimming, biking, and running, with the hopes of maybe one day doing a triathlon. There were a few health care professionals at my institution who competed in yearly triathlons, which certainly inspired me to take up the sport. So, last August, I signed up for my first Half-IRONMAN in Mont-Tremblant, Quebec, and had roughly 10 months to train. Looking back, I am not sure what possessed me to think I could achieve such a feat, but it was certainly a goal to work toward.
First, take it slow and steady. Residency is long and arduous, and it is easy to overpace yourself in the first few months – but keep in mind that you are in it for the long haul (for some, it’s longer than 5 years).
Second, be nice to your body and mind. You wouldn’t believe how some of the most-challenging experiences are all psychological; therefore, eat well, sleep well, and practice mindfulness every day. Develop a routine early on, so that when you meet grueling experiences and challenges, your routine will make you equipped to overcome them. The practice of mindfulness (a mental state of being aware in the present moment) will be unique to each individual and may be performed through exercising, yoga, or more traditionally, through meditation. Third, develop or strengthen a support system to help you identify and overcome problems that you may face during residency.
Ideally, this will be a support system (for example, residents, coworkers, and staff) that know exactly what you will be facing and offer constructive advice for the trials and tribulations you will be confronting. Finally, residency will be the most-challenging experience you may go through yet in your pursuit of postgraduate medical education. You are not alone on this journey, and the path to success will be burdened with physical and mental exhaustion, tears, groans, as well as smiles. But when you cross that finish line, let me tell you that the emotions that will overwhelm you will be those of complete exuberance and utter disbelief that you had the courage and determination to not only undertake the challenge but to succeed, as well.
At the end of my junior surgical residency years, I was in a pretty bad physical and mental space. With resident coverage shortages, long hours, chronic fatigue, and personal pressures to perform and shine, I wound up digging myself into a hole, heading straight to resident burnout. Although there were others around me experiencing similar environmental stressors, I certainly felt alone – not knowing how to climb out of the hole I created for myself.
This was probably the lowest I have been in my life, but I finally got myself back on track. Coming from a fairly physically active background, I returned to a life of proper nutrition and physical activity. I began swimming, biking, and running, with the hopes of maybe one day doing a triathlon. There were a few health care professionals at my institution who competed in yearly triathlons, which certainly inspired me to take up the sport. So, last August, I signed up for my first Half-IRONMAN in Mont-Tremblant, Quebec, and had roughly 10 months to train. Looking back, I am not sure what possessed me to think I could achieve such a feat, but it was certainly a goal to work toward.
First, take it slow and steady. Residency is long and arduous, and it is easy to overpace yourself in the first few months – but keep in mind that you are in it for the long haul (for some, it’s longer than 5 years).
Second, be nice to your body and mind. You wouldn’t believe how some of the most-challenging experiences are all psychological; therefore, eat well, sleep well, and practice mindfulness every day. Develop a routine early on, so that when you meet grueling experiences and challenges, your routine will make you equipped to overcome them. The practice of mindfulness (a mental state of being aware in the present moment) will be unique to each individual and may be performed through exercising, yoga, or more traditionally, through meditation. Third, develop or strengthen a support system to help you identify and overcome problems that you may face during residency.
Ideally, this will be a support system (for example, residents, coworkers, and staff) that know exactly what you will be facing and offer constructive advice for the trials and tribulations you will be confronting. Finally, residency will be the most-challenging experience you may go through yet in your pursuit of postgraduate medical education. You are not alone on this journey, and the path to success will be burdened with physical and mental exhaustion, tears, groans, as well as smiles. But when you cross that finish line, let me tell you that the emotions that will overwhelm you will be those of complete exuberance and utter disbelief that you had the courage and determination to not only undertake the challenge but to succeed, as well.
At the end of my junior surgical residency years, I was in a pretty bad physical and mental space. With resident coverage shortages, long hours, chronic fatigue, and personal pressures to perform and shine, I wound up digging myself into a hole, heading straight to resident burnout. Although there were others around me experiencing similar environmental stressors, I certainly felt alone – not knowing how to climb out of the hole I created for myself.
This was probably the lowest I have been in my life, but I finally got myself back on track. Coming from a fairly physically active background, I returned to a life of proper nutrition and physical activity. I began swimming, biking, and running, with the hopes of maybe one day doing a triathlon. There were a few health care professionals at my institution who competed in yearly triathlons, which certainly inspired me to take up the sport. So, last August, I signed up for my first Half-IRONMAN in Mont-Tremblant, Quebec, and had roughly 10 months to train. Looking back, I am not sure what possessed me to think I could achieve such a feat, but it was certainly a goal to work toward.
First, take it slow and steady. Residency is long and arduous, and it is easy to overpace yourself in the first few months – but keep in mind that you are in it for the long haul (for some, it’s longer than 5 years).
Second, be nice to your body and mind. You wouldn’t believe how some of the most-challenging experiences are all psychological; therefore, eat well, sleep well, and practice mindfulness every day. Develop a routine early on, so that when you meet grueling experiences and challenges, your routine will make you equipped to overcome them. The practice of mindfulness (a mental state of being aware in the present moment) will be unique to each individual and may be performed through exercising, yoga, or more traditionally, through meditation. Third, develop or strengthen a support system to help you identify and overcome problems that you may face during residency.
Ideally, this will be a support system (for example, residents, coworkers, and staff) that know exactly what you will be facing and offer constructive advice for the trials and tribulations you will be confronting. Finally, residency will be the most-challenging experience you may go through yet in your pursuit of postgraduate medical education. You are not alone on this journey, and the path to success will be burdened with physical and mental exhaustion, tears, groans, as well as smiles. But when you cross that finish line, let me tell you that the emotions that will overwhelm you will be those of complete exuberance and utter disbelief that you had the courage and determination to not only undertake the challenge but to succeed, as well.
Commentary: Should board exams include a technical skill assessment? A European perspective
The incidence of vascular diseases is steadily increasing because of an aging population. Vascular surgery is the only specialty that can offer all modalities of vascular therapy (endovascular, open, and conservative). It is therefore necessary to ensure implementation of all these modalities in a modern vascular surgical curricula. The creation of a vascular specialist curriculum is undoubtedly the best way to overcome further fragmentation of vascular provision and to prevent the increasingly financially-driven incentives that can mislead treatment. For obvious reasons this would be a major benefit for our patients and for our specialty.
Another reason for updating the vascular surgical curricula is the significant reduction of open aortic and peripheral vascular surgical training cases, such as abdominal aortic aneurysms and superficial femoral artery occlusions.1 Since the vast majority of these patients are now treated by endovascular means, the remaining vascular disease morphologies can technically be very demanding when requiring open vascular surgery procedures.
Nevertheless, the public and our patients quite understandably expect to be treated by well trained and competent vascular surgeons/specialists. As in all other professions, a proper assessment of all vascular competencies is therefore considered to be mandatory at the end of the training period for a vascular specialist. To this end, several proposals have been made to improve both the structure and different assessment tools including the Vascular Surgical Milestones Project,2 the Vascular Surgery In-Training Examinations (VSITE),3 the use of procedure-based assessments (PBA),4 or objective structured assessments of technical skills (OSATS).5 In addition, simulation workshops (using computer- or life-like synthetic models) play an increasing role in teaching vascular residents the ever-increasing number of different open and endovascular surgical techniques.6,7
Traditionally, the final board examination at the end of the vascular surgical training period consists of an oral assessment or a computer-based test. The obvious crucial question is whether a practical examination should be a added as a mandatory part of a vascular exit exam. This article gives an overview of the board examination of the European Board of Vascular Surgery (EBVS) at the UEMS (Union of European Medical Specialists), which adopted a technical skills assessment in 2006.
The European Vascular Surgical Examination
The UEMS was founded in 1958 as an official body of the European Union (EU). The UEMS has the remits to accredit medical meetings,8 to promote free professional movement of all doctors within Europe, and to ensure high quality of training and associated specialist standards via UEMS examinations.9,10 Currently, the UEMS represents the national medical societies of 37 member states. To date there are 42 UEMS Specialist Sections (separate and independent disciplines), UEMS Divisions (key areas within the independent disciplines, such as Interventional Radiology) and some so-called “Multidisciplinary Joint Committees” (such as Phlebology).
Since 2005, vascular surgery has been represented as an independent medical discipline within the UEMS.Politically, this was a tremendously important step that has helped many European countries to establish vascular surgery on a national level as a separate specialty. The most recent examples are Switzerland (since 2014) and Austria (since 2015).
European vascular surgical examinations have been offered since 1996. The Fellowship of the European Board in Vascular Surgery (FEBVS) is voluntary in most European countries, but in some countries, such as Switzerland and the Netherlands, the European exam has now replaced the national specialist exam.12 Other countries also are in the process of accepting this European standard as a national standard, including Romania, Austria, and Sweden.
The European exam consists of a written section and a combined oral and practical exam. Candidates must be in possession of a national specialist title for surgery or vascular surgery (in countries with a monospecialty). Applications from non-EU countries also are accepted.
Applications must be made in writing, giving details of open-operative and endovascular experience. A distinction is made between assisted operations, independently performed surgery with assistance, and actual independently performed surgical procedures without specialist tutorial assistance. All candidates admitted to the examination have to pass a one-day oral and practical examination, which includes questioning on theoretical background knowledge and its practical application. This takes place mostly in the context of specific clinical case studies as well as via practical examinations on pulsatile perfused lifelike models.
The following procedures are assessed: an infrarenal aortic anastomosis, a carotid endarterectomy, and a distal bypass anastomosis.6,13,14 In the endovascular part of the examination, the applicant’s ability to introduce a guide-wire into the renal artery is assessed.15 Unlike the case in many national tests, FEBVS candidates are also presented with a specialist English-language publication (usually from the European Journal of Vascular and Endovascular Surgery). This article is then discussed with two examiners, with respect to its quality as well as its methodological content and significance. Many examination candidates fear this hurdle the most, but in fact very few participants fail this part of the test.
The European exam is designed to be unbiased and fair, with two examiners at each test station who carry out their assessments independent of each other. During the course of the examination, each candidate is interviewed by approximately 10 assessors. The assessment is validated by way of an evaluation form. The assessing auditors’ communications skills are themselves judged by observers. In the event of communication difficulties, observers are subsequently consulted.
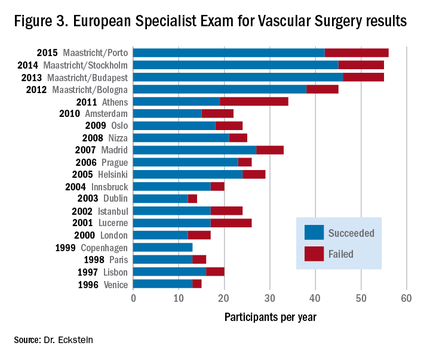
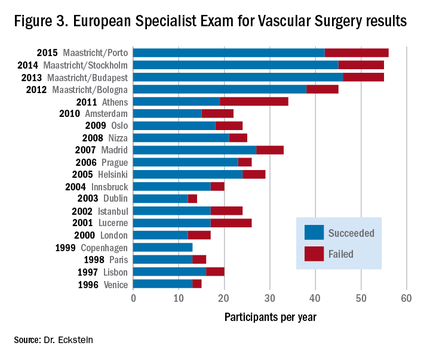
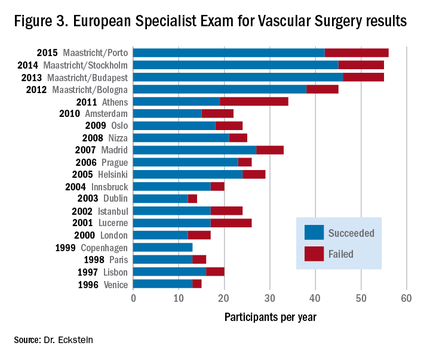
Despite the challenging test procedures, the number of participants in the European Specialist Exam for Vascular Surgery has steadily increased in recent years. For this reason, since 2012, two examination sessions per year have been offered, one during the Annual Meeting of the European Society for Vascular Surgery (ESVS) and one at the European Vascular Course (EVC) in Maastricht. The failure rate each year fluctuates around 20%.
Benefits of being a Fellow of the European Board of Vascular Surgery (FEBVS)
There are a number of very good reasons to sit a European examination and acquire the title of Fellow of the European Board of Vascular Surgery (FEBVS). Some of them are:
Evidence of competency in job applications. Many managers know that the European exam is theoretically and practically challenging, and comprehensive. Confidence in candidates (specialists and senior physicians) who have passed the European test is therefore higher. That in turn increases the chances of getting the desired position especially when applying abroad!
Verification of open surgical and endovascular skills. Filling in the logbook16 helps to maintain a transparent open/endovascular portfolio. It is an extremely sophisticated tool to capture expertise and experience.
Commitment to the need for a European standard. The UEMS has set itself the goal of setting a European standard for medical specialists at the highest level. The European specialist exam projects this. All FEBVS support this goal via their application.
Commitment to academic knowledge-based vascular surgery. The European Vascular Surgery specialist exam covers theoretical background, knowledge of the main studies, basic academic skills, and the ability to comprehensively apply this knowledge to case studies from the entire vascular field. By obtaining this exam, all FEBVS confirm their commitment to an evidence-based approach to vascular surgery.
Commitment to competency-based vascular surgery. The European Vascular Surgery specialist exam covers a practical assessment on open vascular surgical and endovascular key competencies. By passing this part of the exam, all FEBVS give evidence that they are technically competent vascular surgeons.
Desire to belong to the best of the profession. The European specialist exam is certainly more demanding than many national board certifications. However, it offers an opportunity to belong to the European vascular surgical elite.
In conclusion, the European experience on board examinations including skills assessment shows pretty clearly that this sort of comprehensive examination is feasible. Moreover, the increasing number of applications indicates the growing attractiveness of the European certification and qualification as FEBVS. The long-term goal will be to make this examination mandatory for all EU countries – still a long way to go. By the way, since the status of FEBVS is also achievable by non-EU countries, Brexit will not prevent vascular surgeons from the United Kingdom to qualify as FEBVS in the future!
Dr. Eckstein is the Past President of the Board and Section of Vascular Surgery at the Union of European Medical Specialists (UEMS) and Past President of the German Vascular Society (DGG), and an associate editor for Vascular Specialist.
References
1. J Vasc Surg. 2014;60:945-49
2. J Vasc Surg. 2009;49:1140-6
3. Vascular surgery qualifying examination and Vsite
4. Health Technol Assess. 2011;15:i-xxi, 1-162
6. J Vasc Surg. 2013;57:1422-8
8. International Angiology. 2007;26:361-6
9. Eur J Vasc Endovasc Surg. 2009;37:109-15
10. J Vasc Surg. 2008;48:69S-75S; discussion 75S
12. Eur J Vasc Endovasc Surg. 2013;46:719-25
13. J Vasc Surg. 2013;57:1148-54
14. Brit J Surg. 2006;93:1132-8

|
Dr. Malachi Sheahan III |
Dr. Eckstein’s excellent review highlights the challenges the European Union faces in trying to standardize its certification in vascular surgery. Among European nations, the training pathways in vascular surgery are extremely varied, yet the European Economic Union calls for a medical specialist who is certified in one country to be able to practice that specialty in any EEU nation. While participation in the Fellowship of the European Board in Vascular Surgery is still mostly optional, it does provide a path toward a standard of quality that includes competence in open and endovascular procedures. In the United States, we face a similar dilemma with the advent of the integrated vascular residencies. Curricula, case volumes, and rotations still vary wildly between programs and in comparison with traditional fellowships. One solution is the Fundamentals of Vascular and Endovascular Surgery (FVEVS) project. Currently in its pilot stage, the FVEVS is designed to ensure the attainment of basic technical competencies by the mid-trainee level so the later years are focused on advanced open and endovascular training.
Dr. Malachi Sheahan III is the Associate Medical Editor for Vascular Specialist.

|
Dr. Malachi Sheahan III |
Dr. Eckstein’s excellent review highlights the challenges the European Union faces in trying to standardize its certification in vascular surgery. Among European nations, the training pathways in vascular surgery are extremely varied, yet the European Economic Union calls for a medical specialist who is certified in one country to be able to practice that specialty in any EEU nation. While participation in the Fellowship of the European Board in Vascular Surgery is still mostly optional, it does provide a path toward a standard of quality that includes competence in open and endovascular procedures. In the United States, we face a similar dilemma with the advent of the integrated vascular residencies. Curricula, case volumes, and rotations still vary wildly between programs and in comparison with traditional fellowships. One solution is the Fundamentals of Vascular and Endovascular Surgery (FVEVS) project. Currently in its pilot stage, the FVEVS is designed to ensure the attainment of basic technical competencies by the mid-trainee level so the later years are focused on advanced open and endovascular training.
Dr. Malachi Sheahan III is the Associate Medical Editor for Vascular Specialist.

|
Dr. Malachi Sheahan III |
Dr. Eckstein’s excellent review highlights the challenges the European Union faces in trying to standardize its certification in vascular surgery. Among European nations, the training pathways in vascular surgery are extremely varied, yet the European Economic Union calls for a medical specialist who is certified in one country to be able to practice that specialty in any EEU nation. While participation in the Fellowship of the European Board in Vascular Surgery is still mostly optional, it does provide a path toward a standard of quality that includes competence in open and endovascular procedures. In the United States, we face a similar dilemma with the advent of the integrated vascular residencies. Curricula, case volumes, and rotations still vary wildly between programs and in comparison with traditional fellowships. One solution is the Fundamentals of Vascular and Endovascular Surgery (FVEVS) project. Currently in its pilot stage, the FVEVS is designed to ensure the attainment of basic technical competencies by the mid-trainee level so the later years are focused on advanced open and endovascular training.
Dr. Malachi Sheahan III is the Associate Medical Editor for Vascular Specialist.
The incidence of vascular diseases is steadily increasing because of an aging population. Vascular surgery is the only specialty that can offer all modalities of vascular therapy (endovascular, open, and conservative). It is therefore necessary to ensure implementation of all these modalities in a modern vascular surgical curricula. The creation of a vascular specialist curriculum is undoubtedly the best way to overcome further fragmentation of vascular provision and to prevent the increasingly financially-driven incentives that can mislead treatment. For obvious reasons this would be a major benefit for our patients and for our specialty.
Another reason for updating the vascular surgical curricula is the significant reduction of open aortic and peripheral vascular surgical training cases, such as abdominal aortic aneurysms and superficial femoral artery occlusions.1 Since the vast majority of these patients are now treated by endovascular means, the remaining vascular disease morphologies can technically be very demanding when requiring open vascular surgery procedures.
Nevertheless, the public and our patients quite understandably expect to be treated by well trained and competent vascular surgeons/specialists. As in all other professions, a proper assessment of all vascular competencies is therefore considered to be mandatory at the end of the training period for a vascular specialist. To this end, several proposals have been made to improve both the structure and different assessment tools including the Vascular Surgical Milestones Project,2 the Vascular Surgery In-Training Examinations (VSITE),3 the use of procedure-based assessments (PBA),4 or objective structured assessments of technical skills (OSATS).5 In addition, simulation workshops (using computer- or life-like synthetic models) play an increasing role in teaching vascular residents the ever-increasing number of different open and endovascular surgical techniques.6,7
Traditionally, the final board examination at the end of the vascular surgical training period consists of an oral assessment or a computer-based test. The obvious crucial question is whether a practical examination should be a added as a mandatory part of a vascular exit exam. This article gives an overview of the board examination of the European Board of Vascular Surgery (EBVS) at the UEMS (Union of European Medical Specialists), which adopted a technical skills assessment in 2006.
The European Vascular Surgical Examination
The UEMS was founded in 1958 as an official body of the European Union (EU). The UEMS has the remits to accredit medical meetings,8 to promote free professional movement of all doctors within Europe, and to ensure high quality of training and associated specialist standards via UEMS examinations.9,10 Currently, the UEMS represents the national medical societies of 37 member states. To date there are 42 UEMS Specialist Sections (separate and independent disciplines), UEMS Divisions (key areas within the independent disciplines, such as Interventional Radiology) and some so-called “Multidisciplinary Joint Committees” (such as Phlebology).
Since 2005, vascular surgery has been represented as an independent medical discipline within the UEMS.Politically, this was a tremendously important step that has helped many European countries to establish vascular surgery on a national level as a separate specialty. The most recent examples are Switzerland (since 2014) and Austria (since 2015).
European vascular surgical examinations have been offered since 1996. The Fellowship of the European Board in Vascular Surgery (FEBVS) is voluntary in most European countries, but in some countries, such as Switzerland and the Netherlands, the European exam has now replaced the national specialist exam.12 Other countries also are in the process of accepting this European standard as a national standard, including Romania, Austria, and Sweden.
The European exam consists of a written section and a combined oral and practical exam. Candidates must be in possession of a national specialist title for surgery or vascular surgery (in countries with a monospecialty). Applications from non-EU countries also are accepted.
Applications must be made in writing, giving details of open-operative and endovascular experience. A distinction is made between assisted operations, independently performed surgery with assistance, and actual independently performed surgical procedures without specialist tutorial assistance. All candidates admitted to the examination have to pass a one-day oral and practical examination, which includes questioning on theoretical background knowledge and its practical application. This takes place mostly in the context of specific clinical case studies as well as via practical examinations on pulsatile perfused lifelike models.
The following procedures are assessed: an infrarenal aortic anastomosis, a carotid endarterectomy, and a distal bypass anastomosis.6,13,14 In the endovascular part of the examination, the applicant’s ability to introduce a guide-wire into the renal artery is assessed.15 Unlike the case in many national tests, FEBVS candidates are also presented with a specialist English-language publication (usually from the European Journal of Vascular and Endovascular Surgery). This article is then discussed with two examiners, with respect to its quality as well as its methodological content and significance. Many examination candidates fear this hurdle the most, but in fact very few participants fail this part of the test.
The European exam is designed to be unbiased and fair, with two examiners at each test station who carry out their assessments independent of each other. During the course of the examination, each candidate is interviewed by approximately 10 assessors. The assessment is validated by way of an evaluation form. The assessing auditors’ communications skills are themselves judged by observers. In the event of communication difficulties, observers are subsequently consulted.
Despite the challenging test procedures, the number of participants in the European Specialist Exam for Vascular Surgery has steadily increased in recent years. For this reason, since 2012, two examination sessions per year have been offered, one during the Annual Meeting of the European Society for Vascular Surgery (ESVS) and one at the European Vascular Course (EVC) in Maastricht. The failure rate each year fluctuates around 20%.
Benefits of being a Fellow of the European Board of Vascular Surgery (FEBVS)
There are a number of very good reasons to sit a European examination and acquire the title of Fellow of the European Board of Vascular Surgery (FEBVS). Some of them are:
Evidence of competency in job applications. Many managers know that the European exam is theoretically and practically challenging, and comprehensive. Confidence in candidates (specialists and senior physicians) who have passed the European test is therefore higher. That in turn increases the chances of getting the desired position especially when applying abroad!
Verification of open surgical and endovascular skills. Filling in the logbook16 helps to maintain a transparent open/endovascular portfolio. It is an extremely sophisticated tool to capture expertise and experience.
Commitment to the need for a European standard. The UEMS has set itself the goal of setting a European standard for medical specialists at the highest level. The European specialist exam projects this. All FEBVS support this goal via their application.
Commitment to academic knowledge-based vascular surgery. The European Vascular Surgery specialist exam covers theoretical background, knowledge of the main studies, basic academic skills, and the ability to comprehensively apply this knowledge to case studies from the entire vascular field. By obtaining this exam, all FEBVS confirm their commitment to an evidence-based approach to vascular surgery.
Commitment to competency-based vascular surgery. The European Vascular Surgery specialist exam covers a practical assessment on open vascular surgical and endovascular key competencies. By passing this part of the exam, all FEBVS give evidence that they are technically competent vascular surgeons.
Desire to belong to the best of the profession. The European specialist exam is certainly more demanding than many national board certifications. However, it offers an opportunity to belong to the European vascular surgical elite.
In conclusion, the European experience on board examinations including skills assessment shows pretty clearly that this sort of comprehensive examination is feasible. Moreover, the increasing number of applications indicates the growing attractiveness of the European certification and qualification as FEBVS. The long-term goal will be to make this examination mandatory for all EU countries – still a long way to go. By the way, since the status of FEBVS is also achievable by non-EU countries, Brexit will not prevent vascular surgeons from the United Kingdom to qualify as FEBVS in the future!
Dr. Eckstein is the Past President of the Board and Section of Vascular Surgery at the Union of European Medical Specialists (UEMS) and Past President of the German Vascular Society (DGG), and an associate editor for Vascular Specialist.
References
1. J Vasc Surg. 2014;60:945-49
2. J Vasc Surg. 2009;49:1140-6
3. Vascular surgery qualifying examination and Vsite
4. Health Technol Assess. 2011;15:i-xxi, 1-162
6. J Vasc Surg. 2013;57:1422-8
8. International Angiology. 2007;26:361-6
9. Eur J Vasc Endovasc Surg. 2009;37:109-15
10. J Vasc Surg. 2008;48:69S-75S; discussion 75S
12. Eur J Vasc Endovasc Surg. 2013;46:719-25
13. J Vasc Surg. 2013;57:1148-54
14. Brit J Surg. 2006;93:1132-8
The incidence of vascular diseases is steadily increasing because of an aging population. Vascular surgery is the only specialty that can offer all modalities of vascular therapy (endovascular, open, and conservative). It is therefore necessary to ensure implementation of all these modalities in a modern vascular surgical curricula. The creation of a vascular specialist curriculum is undoubtedly the best way to overcome further fragmentation of vascular provision and to prevent the increasingly financially-driven incentives that can mislead treatment. For obvious reasons this would be a major benefit for our patients and for our specialty.
Another reason for updating the vascular surgical curricula is the significant reduction of open aortic and peripheral vascular surgical training cases, such as abdominal aortic aneurysms and superficial femoral artery occlusions.1 Since the vast majority of these patients are now treated by endovascular means, the remaining vascular disease morphologies can technically be very demanding when requiring open vascular surgery procedures.
Nevertheless, the public and our patients quite understandably expect to be treated by well trained and competent vascular surgeons/specialists. As in all other professions, a proper assessment of all vascular competencies is therefore considered to be mandatory at the end of the training period for a vascular specialist. To this end, several proposals have been made to improve both the structure and different assessment tools including the Vascular Surgical Milestones Project,2 the Vascular Surgery In-Training Examinations (VSITE),3 the use of procedure-based assessments (PBA),4 or objective structured assessments of technical skills (OSATS).5 In addition, simulation workshops (using computer- or life-like synthetic models) play an increasing role in teaching vascular residents the ever-increasing number of different open and endovascular surgical techniques.6,7
Traditionally, the final board examination at the end of the vascular surgical training period consists of an oral assessment or a computer-based test. The obvious crucial question is whether a practical examination should be a added as a mandatory part of a vascular exit exam. This article gives an overview of the board examination of the European Board of Vascular Surgery (EBVS) at the UEMS (Union of European Medical Specialists), which adopted a technical skills assessment in 2006.
The European Vascular Surgical Examination
The UEMS was founded in 1958 as an official body of the European Union (EU). The UEMS has the remits to accredit medical meetings,8 to promote free professional movement of all doctors within Europe, and to ensure high quality of training and associated specialist standards via UEMS examinations.9,10 Currently, the UEMS represents the national medical societies of 37 member states. To date there are 42 UEMS Specialist Sections (separate and independent disciplines), UEMS Divisions (key areas within the independent disciplines, such as Interventional Radiology) and some so-called “Multidisciplinary Joint Committees” (such as Phlebology).
Since 2005, vascular surgery has been represented as an independent medical discipline within the UEMS.Politically, this was a tremendously important step that has helped many European countries to establish vascular surgery on a national level as a separate specialty. The most recent examples are Switzerland (since 2014) and Austria (since 2015).
European vascular surgical examinations have been offered since 1996. The Fellowship of the European Board in Vascular Surgery (FEBVS) is voluntary in most European countries, but in some countries, such as Switzerland and the Netherlands, the European exam has now replaced the national specialist exam.12 Other countries also are in the process of accepting this European standard as a national standard, including Romania, Austria, and Sweden.
The European exam consists of a written section and a combined oral and practical exam. Candidates must be in possession of a national specialist title for surgery or vascular surgery (in countries with a monospecialty). Applications from non-EU countries also are accepted.
Applications must be made in writing, giving details of open-operative and endovascular experience. A distinction is made between assisted operations, independently performed surgery with assistance, and actual independently performed surgical procedures without specialist tutorial assistance. All candidates admitted to the examination have to pass a one-day oral and practical examination, which includes questioning on theoretical background knowledge and its practical application. This takes place mostly in the context of specific clinical case studies as well as via practical examinations on pulsatile perfused lifelike models.
The following procedures are assessed: an infrarenal aortic anastomosis, a carotid endarterectomy, and a distal bypass anastomosis.6,13,14 In the endovascular part of the examination, the applicant’s ability to introduce a guide-wire into the renal artery is assessed.15 Unlike the case in many national tests, FEBVS candidates are also presented with a specialist English-language publication (usually from the European Journal of Vascular and Endovascular Surgery). This article is then discussed with two examiners, with respect to its quality as well as its methodological content and significance. Many examination candidates fear this hurdle the most, but in fact very few participants fail this part of the test.
The European exam is designed to be unbiased and fair, with two examiners at each test station who carry out their assessments independent of each other. During the course of the examination, each candidate is interviewed by approximately 10 assessors. The assessment is validated by way of an evaluation form. The assessing auditors’ communications skills are themselves judged by observers. In the event of communication difficulties, observers are subsequently consulted.
Despite the challenging test procedures, the number of participants in the European Specialist Exam for Vascular Surgery has steadily increased in recent years. For this reason, since 2012, two examination sessions per year have been offered, one during the Annual Meeting of the European Society for Vascular Surgery (ESVS) and one at the European Vascular Course (EVC) in Maastricht. The failure rate each year fluctuates around 20%.
Benefits of being a Fellow of the European Board of Vascular Surgery (FEBVS)
There are a number of very good reasons to sit a European examination and acquire the title of Fellow of the European Board of Vascular Surgery (FEBVS). Some of them are:
Evidence of competency in job applications. Many managers know that the European exam is theoretically and practically challenging, and comprehensive. Confidence in candidates (specialists and senior physicians) who have passed the European test is therefore higher. That in turn increases the chances of getting the desired position especially when applying abroad!
Verification of open surgical and endovascular skills. Filling in the logbook16 helps to maintain a transparent open/endovascular portfolio. It is an extremely sophisticated tool to capture expertise and experience.
Commitment to the need for a European standard. The UEMS has set itself the goal of setting a European standard for medical specialists at the highest level. The European specialist exam projects this. All FEBVS support this goal via their application.
Commitment to academic knowledge-based vascular surgery. The European Vascular Surgery specialist exam covers theoretical background, knowledge of the main studies, basic academic skills, and the ability to comprehensively apply this knowledge to case studies from the entire vascular field. By obtaining this exam, all FEBVS confirm their commitment to an evidence-based approach to vascular surgery.
Commitment to competency-based vascular surgery. The European Vascular Surgery specialist exam covers a practical assessment on open vascular surgical and endovascular key competencies. By passing this part of the exam, all FEBVS give evidence that they are technically competent vascular surgeons.
Desire to belong to the best of the profession. The European specialist exam is certainly more demanding than many national board certifications. However, it offers an opportunity to belong to the European vascular surgical elite.
In conclusion, the European experience on board examinations including skills assessment shows pretty clearly that this sort of comprehensive examination is feasible. Moreover, the increasing number of applications indicates the growing attractiveness of the European certification and qualification as FEBVS. The long-term goal will be to make this examination mandatory for all EU countries – still a long way to go. By the way, since the status of FEBVS is also achievable by non-EU countries, Brexit will not prevent vascular surgeons from the United Kingdom to qualify as FEBVS in the future!
Dr. Eckstein is the Past President of the Board and Section of Vascular Surgery at the Union of European Medical Specialists (UEMS) and Past President of the German Vascular Society (DGG), and an associate editor for Vascular Specialist.
References
1. J Vasc Surg. 2014;60:945-49
2. J Vasc Surg. 2009;49:1140-6
3. Vascular surgery qualifying examination and Vsite
4. Health Technol Assess. 2011;15:i-xxi, 1-162
6. J Vasc Surg. 2013;57:1422-8
8. International Angiology. 2007;26:361-6
9. Eur J Vasc Endovasc Surg. 2009;37:109-15
10. J Vasc Surg. 2008;48:69S-75S; discussion 75S
12. Eur J Vasc Endovasc Surg. 2013;46:719-25
13. J Vasc Surg. 2013;57:1148-54
14. Brit J Surg. 2006;93:1132-8
Does congenital cardiac surgery training need a makeover?
Trainees in congenital cardiac surgery fellowship programs are doing more operations since the programs became accredited in 2007, but no clear parameters have emerged to determine if certification has improved the quality of training, according to an evaluation of fellowship training programs published in the June issue of the Journal of Thoracic and Cardiovascular Surgery (2016 Jun;151:1488-95).
Overall, the training has become standardized, the fellows’ operative experience is “robust,” and fellows are mostly satisfied since the Accreditation Council of Graduate Medical Education (ACGME) recognized congenital cardiac surgery as a fellowship in 2007, lead study author Dr. Brian Kogon of Emory University, Atlanta, said.
However, Dr. Kogon and his colleagues also found some shortcomings in fellowship training. They received survey responses from 36 of 44 fellows in 12 accredited programs nationwide. To determine if fellows were meeting minimum case requirements, they also reviewed operative logs of 38 of the 44 fellows. They compared their findings to a study of congenital cardiac surgery fellowship programs they did pre-ACGME accreditation (J Thorac Cardiovasc Surg. 2006 Dec;132:1280). “The number of operations performed by the fellows during their training was underwhelming, and most of the fellows were dissatisfied with their operative experience,” Dr. Kogon and his colleagues wrote in the earlier study.
The study found that all fellows achieved the minimum number of 75 total cases the standards require for graduation, with a median of 136; and the minimum standard of 36 specific qualifying cases with a median of 63. However, seven did not meet the minimum of five complex neonate cases. Among other types of operations for which fellows failed to meet the minimum cases were atrioventricular septal defect repair, arch reconstruction including coarctation procedures and systemic-to-pulmonary artery shunt procedures.
The comparative lack of adult cardiac surgery operations was also considered a potential problem, the authors noted, pointing out that “the number of adults who have congenital heart disease now exceeds the number of children who have the disease, and many of these patients will require an operation.”
Another shortcoming the study found was a drop-off in international fellowships since 2007. “This change places us at risk of becoming intellectually isolated and losing international relationships that are critical to the future of our specialty,” Dr. Kogon and his colleagues wrote. Graduated fellows also acknowledged dissatisfaction with their lack of exposure to neonate surgery.
The study also determined the following demographics of the fellows: 83% are men and the median age at graduation was 40 years, with a range of 35-48 years. Only 25% of graduates participated in nonsurgical rotations such as cardiac catheterization and echocardiography.
“Although the operative experience seems to be much more robust, and this finding has been corroborated in other surgical disciplines after the advent of ACGME accreditation, comparing training before and after the accreditation process came into existence is difficult,” Dr. Kogon and his colleagues said.
The study also noted that the Thoracic Surgery Directors Association developed a congenital curriculum for congenital cardiothoracic surgery fellows, but only 28% used that curriculum and only 61% used any formal curriculum. “Unfortunately, regardless of the curriculum, only 50% of the graduates found it helpful,” Dr. Kogon and his colleagues said.
And regardless of the curriculum, only half of the graduates have passed the written qualifying and oral certifying examinations after completing their fellowship. “Although the curriculum is quite robust, the latter statistic suggests that we need either more emphasis on education by the program directors or a better and/or different curriculum,” Dr. Kogon and his colleagues said. However, they added that “after training, former fellows have adequate case volumes and mixes and seem to be thriving in the field.”
Dr. Kogon and his study coauthors had no financial disclosures.
In his invited commentary, Dr. Charles D. Fraser Jr. of Texas Children’s Hospital, Baylor University, Houston, called the study findings that only 50% of congenital cardiac surgery fellowship graduates had passed the congenital examination “quite disturbing” and the demographic data and surgical and nonsurgical experience of the trainees “thought provoking” (J Thorac Cardiovasc Surg. 2016;151:1496-7)
“Is the bar too high or too low?” Dr. Fraser asked. He suggested the fellowship training system for congenital cardiac surgeons may be a work in progress. “For one, having a median age of 40 years for graduates is unacceptable,” he said. For half of trainees to not pass the examination “at this advanced age is tragic.” That 25% of fellows participate in nonsurgical rotations “also is concerning.”
|
Dr. Charles D. Fraser |
A challenge is that after fellows complete their training in general and cardiothoracic surgery, opportunities to operate on newborns in a new fellowship setting are extremely limited, Dr. Fraser said. “To expect someone to be able to perform complex newborn heart surgery with excellent outcomes in a brand-new environment after just learning how to perform adult cardiac surgery is unrealistic,” he said.
Dr. Fraser said 1 formal year of training for congenital cardiac surgery fellows may not be enough. “Our colleagues in general pediatric surgery have a 2-year fellowship, and our specialty is every bit as complex as theirs,” he said. The basic American Board of Thoracic Surgery thoracic fellowship should have more latitude in its congenital heart surgery rotations, including exposure to pediatrics, neonatal/pediatric critical care, and the nonsurgical rotations the study referred to. Congenital heart surgery fellowships should also embrace adult congenital heart surgery with a more formalized experience requirement, he said.
“As a specialty, we owe it to our fine young surgeon candidates to offer the most robust and fair pathway to success while never compromising on the public trust and patient well-being,” Dr. Fraser said.
Dr. Fraser is chief of the division of congenital heart surgery at Baylor and codirector of the Texas Children’s Heart Center. He had no financial relationships to disclose.
In his invited commentary, Dr. Charles D. Fraser Jr. of Texas Children’s Hospital, Baylor University, Houston, called the study findings that only 50% of congenital cardiac surgery fellowship graduates had passed the congenital examination “quite disturbing” and the demographic data and surgical and nonsurgical experience of the trainees “thought provoking” (J Thorac Cardiovasc Surg. 2016;151:1496-7)
“Is the bar too high or too low?” Dr. Fraser asked. He suggested the fellowship training system for congenital cardiac surgeons may be a work in progress. “For one, having a median age of 40 years for graduates is unacceptable,” he said. For half of trainees to not pass the examination “at this advanced age is tragic.” That 25% of fellows participate in nonsurgical rotations “also is concerning.”
|
Dr. Charles D. Fraser |
A challenge is that after fellows complete their training in general and cardiothoracic surgery, opportunities to operate on newborns in a new fellowship setting are extremely limited, Dr. Fraser said. “To expect someone to be able to perform complex newborn heart surgery with excellent outcomes in a brand-new environment after just learning how to perform adult cardiac surgery is unrealistic,” he said.
Dr. Fraser said 1 formal year of training for congenital cardiac surgery fellows may not be enough. “Our colleagues in general pediatric surgery have a 2-year fellowship, and our specialty is every bit as complex as theirs,” he said. The basic American Board of Thoracic Surgery thoracic fellowship should have more latitude in its congenital heart surgery rotations, including exposure to pediatrics, neonatal/pediatric critical care, and the nonsurgical rotations the study referred to. Congenital heart surgery fellowships should also embrace adult congenital heart surgery with a more formalized experience requirement, he said.
“As a specialty, we owe it to our fine young surgeon candidates to offer the most robust and fair pathway to success while never compromising on the public trust and patient well-being,” Dr. Fraser said.
Dr. Fraser is chief of the division of congenital heart surgery at Baylor and codirector of the Texas Children’s Heart Center. He had no financial relationships to disclose.
In his invited commentary, Dr. Charles D. Fraser Jr. of Texas Children’s Hospital, Baylor University, Houston, called the study findings that only 50% of congenital cardiac surgery fellowship graduates had passed the congenital examination “quite disturbing” and the demographic data and surgical and nonsurgical experience of the trainees “thought provoking” (J Thorac Cardiovasc Surg. 2016;151:1496-7)
“Is the bar too high or too low?” Dr. Fraser asked. He suggested the fellowship training system for congenital cardiac surgeons may be a work in progress. “For one, having a median age of 40 years for graduates is unacceptable,” he said. For half of trainees to not pass the examination “at this advanced age is tragic.” That 25% of fellows participate in nonsurgical rotations “also is concerning.”
|
Dr. Charles D. Fraser |
A challenge is that after fellows complete their training in general and cardiothoracic surgery, opportunities to operate on newborns in a new fellowship setting are extremely limited, Dr. Fraser said. “To expect someone to be able to perform complex newborn heart surgery with excellent outcomes in a brand-new environment after just learning how to perform adult cardiac surgery is unrealistic,” he said.
Dr. Fraser said 1 formal year of training for congenital cardiac surgery fellows may not be enough. “Our colleagues in general pediatric surgery have a 2-year fellowship, and our specialty is every bit as complex as theirs,” he said. The basic American Board of Thoracic Surgery thoracic fellowship should have more latitude in its congenital heart surgery rotations, including exposure to pediatrics, neonatal/pediatric critical care, and the nonsurgical rotations the study referred to. Congenital heart surgery fellowships should also embrace adult congenital heart surgery with a more formalized experience requirement, he said.
“As a specialty, we owe it to our fine young surgeon candidates to offer the most robust and fair pathway to success while never compromising on the public trust and patient well-being,” Dr. Fraser said.
Dr. Fraser is chief of the division of congenital heart surgery at Baylor and codirector of the Texas Children’s Heart Center. He had no financial relationships to disclose.
Trainees in congenital cardiac surgery fellowship programs are doing more operations since the programs became accredited in 2007, but no clear parameters have emerged to determine if certification has improved the quality of training, according to an evaluation of fellowship training programs published in the June issue of the Journal of Thoracic and Cardiovascular Surgery (2016 Jun;151:1488-95).
Overall, the training has become standardized, the fellows’ operative experience is “robust,” and fellows are mostly satisfied since the Accreditation Council of Graduate Medical Education (ACGME) recognized congenital cardiac surgery as a fellowship in 2007, lead study author Dr. Brian Kogon of Emory University, Atlanta, said.
However, Dr. Kogon and his colleagues also found some shortcomings in fellowship training. They received survey responses from 36 of 44 fellows in 12 accredited programs nationwide. To determine if fellows were meeting minimum case requirements, they also reviewed operative logs of 38 of the 44 fellows. They compared their findings to a study of congenital cardiac surgery fellowship programs they did pre-ACGME accreditation (J Thorac Cardiovasc Surg. 2006 Dec;132:1280). “The number of operations performed by the fellows during their training was underwhelming, and most of the fellows were dissatisfied with their operative experience,” Dr. Kogon and his colleagues wrote in the earlier study.
The study found that all fellows achieved the minimum number of 75 total cases the standards require for graduation, with a median of 136; and the minimum standard of 36 specific qualifying cases with a median of 63. However, seven did not meet the minimum of five complex neonate cases. Among other types of operations for which fellows failed to meet the minimum cases were atrioventricular septal defect repair, arch reconstruction including coarctation procedures and systemic-to-pulmonary artery shunt procedures.
The comparative lack of adult cardiac surgery operations was also considered a potential problem, the authors noted, pointing out that “the number of adults who have congenital heart disease now exceeds the number of children who have the disease, and many of these patients will require an operation.”
Another shortcoming the study found was a drop-off in international fellowships since 2007. “This change places us at risk of becoming intellectually isolated and losing international relationships that are critical to the future of our specialty,” Dr. Kogon and his colleagues wrote. Graduated fellows also acknowledged dissatisfaction with their lack of exposure to neonate surgery.
The study also determined the following demographics of the fellows: 83% are men and the median age at graduation was 40 years, with a range of 35-48 years. Only 25% of graduates participated in nonsurgical rotations such as cardiac catheterization and echocardiography.
“Although the operative experience seems to be much more robust, and this finding has been corroborated in other surgical disciplines after the advent of ACGME accreditation, comparing training before and after the accreditation process came into existence is difficult,” Dr. Kogon and his colleagues said.
The study also noted that the Thoracic Surgery Directors Association developed a congenital curriculum for congenital cardiothoracic surgery fellows, but only 28% used that curriculum and only 61% used any formal curriculum. “Unfortunately, regardless of the curriculum, only 50% of the graduates found it helpful,” Dr. Kogon and his colleagues said.
And regardless of the curriculum, only half of the graduates have passed the written qualifying and oral certifying examinations after completing their fellowship. “Although the curriculum is quite robust, the latter statistic suggests that we need either more emphasis on education by the program directors or a better and/or different curriculum,” Dr. Kogon and his colleagues said. However, they added that “after training, former fellows have adequate case volumes and mixes and seem to be thriving in the field.”
Dr. Kogon and his study coauthors had no financial disclosures.
Trainees in congenital cardiac surgery fellowship programs are doing more operations since the programs became accredited in 2007, but no clear parameters have emerged to determine if certification has improved the quality of training, according to an evaluation of fellowship training programs published in the June issue of the Journal of Thoracic and Cardiovascular Surgery (2016 Jun;151:1488-95).
Overall, the training has become standardized, the fellows’ operative experience is “robust,” and fellows are mostly satisfied since the Accreditation Council of Graduate Medical Education (ACGME) recognized congenital cardiac surgery as a fellowship in 2007, lead study author Dr. Brian Kogon of Emory University, Atlanta, said.
However, Dr. Kogon and his colleagues also found some shortcomings in fellowship training. They received survey responses from 36 of 44 fellows in 12 accredited programs nationwide. To determine if fellows were meeting minimum case requirements, they also reviewed operative logs of 38 of the 44 fellows. They compared their findings to a study of congenital cardiac surgery fellowship programs they did pre-ACGME accreditation (J Thorac Cardiovasc Surg. 2006 Dec;132:1280). “The number of operations performed by the fellows during their training was underwhelming, and most of the fellows were dissatisfied with their operative experience,” Dr. Kogon and his colleagues wrote in the earlier study.
The study found that all fellows achieved the minimum number of 75 total cases the standards require for graduation, with a median of 136; and the minimum standard of 36 specific qualifying cases with a median of 63. However, seven did not meet the minimum of five complex neonate cases. Among other types of operations for which fellows failed to meet the minimum cases were atrioventricular septal defect repair, arch reconstruction including coarctation procedures and systemic-to-pulmonary artery shunt procedures.
The comparative lack of adult cardiac surgery operations was also considered a potential problem, the authors noted, pointing out that “the number of adults who have congenital heart disease now exceeds the number of children who have the disease, and many of these patients will require an operation.”
Another shortcoming the study found was a drop-off in international fellowships since 2007. “This change places us at risk of becoming intellectually isolated and losing international relationships that are critical to the future of our specialty,” Dr. Kogon and his colleagues wrote. Graduated fellows also acknowledged dissatisfaction with their lack of exposure to neonate surgery.
The study also determined the following demographics of the fellows: 83% are men and the median age at graduation was 40 years, with a range of 35-48 years. Only 25% of graduates participated in nonsurgical rotations such as cardiac catheterization and echocardiography.
“Although the operative experience seems to be much more robust, and this finding has been corroborated in other surgical disciplines after the advent of ACGME accreditation, comparing training before and after the accreditation process came into existence is difficult,” Dr. Kogon and his colleagues said.
The study also noted that the Thoracic Surgery Directors Association developed a congenital curriculum for congenital cardiothoracic surgery fellows, but only 28% used that curriculum and only 61% used any formal curriculum. “Unfortunately, regardless of the curriculum, only 50% of the graduates found it helpful,” Dr. Kogon and his colleagues said.
And regardless of the curriculum, only half of the graduates have passed the written qualifying and oral certifying examinations after completing their fellowship. “Although the curriculum is quite robust, the latter statistic suggests that we need either more emphasis on education by the program directors or a better and/or different curriculum,” Dr. Kogon and his colleagues said. However, they added that “after training, former fellows have adequate case volumes and mixes and seem to be thriving in the field.”
Dr. Kogon and his study coauthors had no financial disclosures.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: Since congenital cardiac fellowship programs became accredited in 2007, training requirements have been standardized and the surgical experience robust.
Major finding: Recent graduates of fellowship programs are thriving in practice, but shortcomings with existing fellowship training exist, including only 50% gaining certification by passing the written and oral exams.
Data source: The study drew on survey responses from 36 of 44 fellows in 12 accredited programs and a review of operative logs of 38 of the 44 fellows.
Disclosures: Dr. Kogon and his study coauthors had no financial disclosures.
General surgeons getting less vascular training
Vascular surgery fellow case logs reflect an increase in endovascular interventions, but general surgery residents may be missing out on training opportunities, according to a study of national case data.
In addition, general surgery residents saw a decrease in open vascular surgery cases, which was not reflected among the vascular surgery fellows, according to Dr. Rose C. Pedersen and colleagues in the department of surgery, Kaiser Permanente Los Angeles Medical Center. The report was published online in Annals of Vascular Surgery (doi: 10.1016/j.avsg.2016.02.008).
The paper was originally presented at the 2105 annual meeting of the Southern California Vascular Society. The study reports findings of a review of the Accreditation Council for Graduate Medical Education national case log reports from 2001 to 2012.
During that period, the number of general surgery residents increased from 1,021 to 1,098, while the number of vascular surgery fellows increased from 96 to 121. The total number of vascular cases logged by the vascular fellows significantly increased by 161%, from an average of 298 cases to 762 cases over the time period assessed. During that same period, vascular cases done by general surgery residents significantly decreased by 40%, from an average of 186 to 116 cases.
In terms of open cases. vascular fellows saw a significant 43% decrease in open abdominal aortic aneurysm (AAA) cases, going from 26 to 15, and a slight but significant increase in carotid endarterectomy cases logged (44 to 49). Hemodialysis access and major amputations also both increased significantly. A decreases in open surgery for peripheral obstructive disease was small and not significant.
General surgery residents saw decreases in all open surgery areas over the time period: AAA cases fell significantly by 78% (9 cases to 2 cases); carotid endarterectomies decreased significantly from 23 to 12 cases; and surgery for peripheral obstructive disease fell significantly from 21 to 8). Hemodialysis access cases and major amputations both decreased as well, but not significantly.
Endovascular cases increased from 2001 to 2012 for both vascular fellows and general surgery residents. Vascular fellows saw endovascular AAA repair significantly increase from an average of 17 to 46 cases, while those for general surgery residents rosed from roughly 1 to 3 cases. Similarly, endovascular interventions for peripheral obstructive disease significantly increased for vascular fellows from 17 to 85, and from 1.3 to 4 for general surgery residents.
“The contemporary management of abdominal aortic aneurysmal diseases and peripheral obstructive diseases has been particularly changed by endovascular therapies that have been adopted into the training experience of vascular surgery fellows, but not those of general surgery residents. Open surgery experience has decreased overall for general surgery residents in all major categories, a change not seen in vascular fellows,” the researchers concluded.
The authors reported no relevant disclosures.
Vascular surgical practice has evolved with the introduction of minimally invasive technology and advancement of endovascular techniques, and as such, the training of the vascular surgical specialist too has evolved. This article highlights the effect of these technological advancements on the vascular surgical fellowship training experience and points out the effect of this embracing of endovascular techniques by academic centers in their general surgery trainee vascular surgical experience. Open operative case numbers are declining and endovascular case numbers are increasing significantly.
As traditionally performed open procedures are being substituted for endovascular repairs, the open operative experience for vascular surgery trainees is declining or staying stable at the expense of the general surgery resident experience. Open cases (open aneurysm repairs, aortofemoral artery bypasses, visceral artery bypasses, carotid endarterectomies), because they are performed infrequently now, have become fellow cases.

|
Dr. Erica L. Mitchell |
Endovascular cases, which have increased over 300%-400%, too are essentially fellow cases (or in 0+5 programs, which are not discussed in this manuscript, vascular surgery resident cases) because the endovascular skill set does not appear to translate or transfer (and therefore is not considered relevant to the general surgery resident planning on a fellowship or career in the traditional surgical specialties) into open and laparoscopic skills desired by general surgery trainees.
Unfortunately, this open to endovascular operative experience shift will only increase with the introduction and early adoption (in academic centers) of complex endovascular techniques for the management of complex obstructive and aneurysmal arterial disease. A review of case log data for 0+5 and 5+2 residents completing programs in 2014-2015 reveals the operative experience and continued decline in open operative case numbers and increases in endovascular case numbers.
Vascular surgery training programs and their faculties have a responsibility to make sure the operative experience of general surgery residents is a worthwhile one. We, the faculty, need to keep encouraging general surgery residents to come to the operating room, even if they are not the primary surgeons. To make this worthwhile for them (because residents will not come to the operating room if there is nothing to be gained for themselves), we have to let them participate in the case somehow. One of the most critical aspects of a vascular surgical procedure is the operative exposure.
Having the general surgery residents participate in the vascular exposure is not only formative to their understanding of surgical anatomy, and applicable to all aspects of surgical practice, it is also critical to trainee development of decision making, judgment, and situational awareness. These exposures can and should be logged, using the e-code, to receive ACGME case log credit for vascular surgical procedures. E-codes, additionally, allow more than one resident to take credit for an arterial exposure and repair. We must also encourage trainees to come to the angio suite, while these cases, on the outset do not seem relevant to general surgery training, they do provide the learner with a greater appreciation of the complexity of vascular anatomy.
Importantly, as long as we continue to train vascular surgery specialists via the traditional 5+2 paradigm, we must keep general surgery residents, rotating through our services, interested and engaged in the management of vascular diseases. The simplest way to engage them is to make them feel relevant and to make them feel relevant they have to participate, both inside and outside of the operating room. It is, after all, our duty as surgical educators and advocates for our specialty to train the next generation of vascular surgical specialists!
Dr. Erica L. Mitchell is professor of surgery, program director for vascular surgery, and vice-chair of quality, department of surgery, Oregon Health & Science University, Portland. She is an associate medical editor of Vascular Specialist.
Vascular surgical practice has evolved with the introduction of minimally invasive technology and advancement of endovascular techniques, and as such, the training of the vascular surgical specialist too has evolved. This article highlights the effect of these technological advancements on the vascular surgical fellowship training experience and points out the effect of this embracing of endovascular techniques by academic centers in their general surgery trainee vascular surgical experience. Open operative case numbers are declining and endovascular case numbers are increasing significantly.
As traditionally performed open procedures are being substituted for endovascular repairs, the open operative experience for vascular surgery trainees is declining or staying stable at the expense of the general surgery resident experience. Open cases (open aneurysm repairs, aortofemoral artery bypasses, visceral artery bypasses, carotid endarterectomies), because they are performed infrequently now, have become fellow cases.

|
Dr. Erica L. Mitchell |
Endovascular cases, which have increased over 300%-400%, too are essentially fellow cases (or in 0+5 programs, which are not discussed in this manuscript, vascular surgery resident cases) because the endovascular skill set does not appear to translate or transfer (and therefore is not considered relevant to the general surgery resident planning on a fellowship or career in the traditional surgical specialties) into open and laparoscopic skills desired by general surgery trainees.
Unfortunately, this open to endovascular operative experience shift will only increase with the introduction and early adoption (in academic centers) of complex endovascular techniques for the management of complex obstructive and aneurysmal arterial disease. A review of case log data for 0+5 and 5+2 residents completing programs in 2014-2015 reveals the operative experience and continued decline in open operative case numbers and increases in endovascular case numbers.
Vascular surgery training programs and their faculties have a responsibility to make sure the operative experience of general surgery residents is a worthwhile one. We, the faculty, need to keep encouraging general surgery residents to come to the operating room, even if they are not the primary surgeons. To make this worthwhile for them (because residents will not come to the operating room if there is nothing to be gained for themselves), we have to let them participate in the case somehow. One of the most critical aspects of a vascular surgical procedure is the operative exposure.
Having the general surgery residents participate in the vascular exposure is not only formative to their understanding of surgical anatomy, and applicable to all aspects of surgical practice, it is also critical to trainee development of decision making, judgment, and situational awareness. These exposures can and should be logged, using the e-code, to receive ACGME case log credit for vascular surgical procedures. E-codes, additionally, allow more than one resident to take credit for an arterial exposure and repair. We must also encourage trainees to come to the angio suite, while these cases, on the outset do not seem relevant to general surgery training, they do provide the learner with a greater appreciation of the complexity of vascular anatomy.
Importantly, as long as we continue to train vascular surgery specialists via the traditional 5+2 paradigm, we must keep general surgery residents, rotating through our services, interested and engaged in the management of vascular diseases. The simplest way to engage them is to make them feel relevant and to make them feel relevant they have to participate, both inside and outside of the operating room. It is, after all, our duty as surgical educators and advocates for our specialty to train the next generation of vascular surgical specialists!
Dr. Erica L. Mitchell is professor of surgery, program director for vascular surgery, and vice-chair of quality, department of surgery, Oregon Health & Science University, Portland. She is an associate medical editor of Vascular Specialist.
Vascular surgical practice has evolved with the introduction of minimally invasive technology and advancement of endovascular techniques, and as such, the training of the vascular surgical specialist too has evolved. This article highlights the effect of these technological advancements on the vascular surgical fellowship training experience and points out the effect of this embracing of endovascular techniques by academic centers in their general surgery trainee vascular surgical experience. Open operative case numbers are declining and endovascular case numbers are increasing significantly.
As traditionally performed open procedures are being substituted for endovascular repairs, the open operative experience for vascular surgery trainees is declining or staying stable at the expense of the general surgery resident experience. Open cases (open aneurysm repairs, aortofemoral artery bypasses, visceral artery bypasses, carotid endarterectomies), because they are performed infrequently now, have become fellow cases.

|
Dr. Erica L. Mitchell |
Endovascular cases, which have increased over 300%-400%, too are essentially fellow cases (or in 0+5 programs, which are not discussed in this manuscript, vascular surgery resident cases) because the endovascular skill set does not appear to translate or transfer (and therefore is not considered relevant to the general surgery resident planning on a fellowship or career in the traditional surgical specialties) into open and laparoscopic skills desired by general surgery trainees.
Unfortunately, this open to endovascular operative experience shift will only increase with the introduction and early adoption (in academic centers) of complex endovascular techniques for the management of complex obstructive and aneurysmal arterial disease. A review of case log data for 0+5 and 5+2 residents completing programs in 2014-2015 reveals the operative experience and continued decline in open operative case numbers and increases in endovascular case numbers.
Vascular surgery training programs and their faculties have a responsibility to make sure the operative experience of general surgery residents is a worthwhile one. We, the faculty, need to keep encouraging general surgery residents to come to the operating room, even if they are not the primary surgeons. To make this worthwhile for them (because residents will not come to the operating room if there is nothing to be gained for themselves), we have to let them participate in the case somehow. One of the most critical aspects of a vascular surgical procedure is the operative exposure.
Having the general surgery residents participate in the vascular exposure is not only formative to their understanding of surgical anatomy, and applicable to all aspects of surgical practice, it is also critical to trainee development of decision making, judgment, and situational awareness. These exposures can and should be logged, using the e-code, to receive ACGME case log credit for vascular surgical procedures. E-codes, additionally, allow more than one resident to take credit for an arterial exposure and repair. We must also encourage trainees to come to the angio suite, while these cases, on the outset do not seem relevant to general surgery training, they do provide the learner with a greater appreciation of the complexity of vascular anatomy.
Importantly, as long as we continue to train vascular surgery specialists via the traditional 5+2 paradigm, we must keep general surgery residents, rotating through our services, interested and engaged in the management of vascular diseases. The simplest way to engage them is to make them feel relevant and to make them feel relevant they have to participate, both inside and outside of the operating room. It is, after all, our duty as surgical educators and advocates for our specialty to train the next generation of vascular surgical specialists!
Dr. Erica L. Mitchell is professor of surgery, program director for vascular surgery, and vice-chair of quality, department of surgery, Oregon Health & Science University, Portland. She is an associate medical editor of Vascular Specialist.
Vascular surgery fellow case logs reflect an increase in endovascular interventions, but general surgery residents may be missing out on training opportunities, according to a study of national case data.
In addition, general surgery residents saw a decrease in open vascular surgery cases, which was not reflected among the vascular surgery fellows, according to Dr. Rose C. Pedersen and colleagues in the department of surgery, Kaiser Permanente Los Angeles Medical Center. The report was published online in Annals of Vascular Surgery (doi: 10.1016/j.avsg.2016.02.008).
The paper was originally presented at the 2105 annual meeting of the Southern California Vascular Society. The study reports findings of a review of the Accreditation Council for Graduate Medical Education national case log reports from 2001 to 2012.
During that period, the number of general surgery residents increased from 1,021 to 1,098, while the number of vascular surgery fellows increased from 96 to 121. The total number of vascular cases logged by the vascular fellows significantly increased by 161%, from an average of 298 cases to 762 cases over the time period assessed. During that same period, vascular cases done by general surgery residents significantly decreased by 40%, from an average of 186 to 116 cases.
In terms of open cases. vascular fellows saw a significant 43% decrease in open abdominal aortic aneurysm (AAA) cases, going from 26 to 15, and a slight but significant increase in carotid endarterectomy cases logged (44 to 49). Hemodialysis access and major amputations also both increased significantly. A decreases in open surgery for peripheral obstructive disease was small and not significant.
General surgery residents saw decreases in all open surgery areas over the time period: AAA cases fell significantly by 78% (9 cases to 2 cases); carotid endarterectomies decreased significantly from 23 to 12 cases; and surgery for peripheral obstructive disease fell significantly from 21 to 8). Hemodialysis access cases and major amputations both decreased as well, but not significantly.
Endovascular cases increased from 2001 to 2012 for both vascular fellows and general surgery residents. Vascular fellows saw endovascular AAA repair significantly increase from an average of 17 to 46 cases, while those for general surgery residents rosed from roughly 1 to 3 cases. Similarly, endovascular interventions for peripheral obstructive disease significantly increased for vascular fellows from 17 to 85, and from 1.3 to 4 for general surgery residents.
“The contemporary management of abdominal aortic aneurysmal diseases and peripheral obstructive diseases has been particularly changed by endovascular therapies that have been adopted into the training experience of vascular surgery fellows, but not those of general surgery residents. Open surgery experience has decreased overall for general surgery residents in all major categories, a change not seen in vascular fellows,” the researchers concluded.
The authors reported no relevant disclosures.
Vascular surgery fellow case logs reflect an increase in endovascular interventions, but general surgery residents may be missing out on training opportunities, according to a study of national case data.
In addition, general surgery residents saw a decrease in open vascular surgery cases, which was not reflected among the vascular surgery fellows, according to Dr. Rose C. Pedersen and colleagues in the department of surgery, Kaiser Permanente Los Angeles Medical Center. The report was published online in Annals of Vascular Surgery (doi: 10.1016/j.avsg.2016.02.008).
The paper was originally presented at the 2105 annual meeting of the Southern California Vascular Society. The study reports findings of a review of the Accreditation Council for Graduate Medical Education national case log reports from 2001 to 2012.
During that period, the number of general surgery residents increased from 1,021 to 1,098, while the number of vascular surgery fellows increased from 96 to 121. The total number of vascular cases logged by the vascular fellows significantly increased by 161%, from an average of 298 cases to 762 cases over the time period assessed. During that same period, vascular cases done by general surgery residents significantly decreased by 40%, from an average of 186 to 116 cases.
In terms of open cases. vascular fellows saw a significant 43% decrease in open abdominal aortic aneurysm (AAA) cases, going from 26 to 15, and a slight but significant increase in carotid endarterectomy cases logged (44 to 49). Hemodialysis access and major amputations also both increased significantly. A decreases in open surgery for peripheral obstructive disease was small and not significant.
General surgery residents saw decreases in all open surgery areas over the time period: AAA cases fell significantly by 78% (9 cases to 2 cases); carotid endarterectomies decreased significantly from 23 to 12 cases; and surgery for peripheral obstructive disease fell significantly from 21 to 8). Hemodialysis access cases and major amputations both decreased as well, but not significantly.
Endovascular cases increased from 2001 to 2012 for both vascular fellows and general surgery residents. Vascular fellows saw endovascular AAA repair significantly increase from an average of 17 to 46 cases, while those for general surgery residents rosed from roughly 1 to 3 cases. Similarly, endovascular interventions for peripheral obstructive disease significantly increased for vascular fellows from 17 to 85, and from 1.3 to 4 for general surgery residents.
“The contemporary management of abdominal aortic aneurysmal diseases and peripheral obstructive diseases has been particularly changed by endovascular therapies that have been adopted into the training experience of vascular surgery fellows, but not those of general surgery residents. Open surgery experience has decreased overall for general surgery residents in all major categories, a change not seen in vascular fellows,” the researchers concluded.
The authors reported no relevant disclosures.
FROM ANNALS OF VASCULAR SURGERY
FIRST reflections: Impact of ACGME duty hours on CT practitioners
Several months ago, Dr. Bilimoria and his colleagues published the long awaited study in NEJM essentially contradicting adverse effects of strict duty hours on patient outcomes (N Engl J Med. 2016 374:713-2). The study, known as the FIRST trial, was published in the March issue of Thoracic Surgery News. Although the study enrolled general surgery residents, its conclusion impacts no specialty more than cardiothoracic surgery, where frequent handoffs complicate tedious perioperative care of sick patients stall learning opportunities for young trainees.
As Dr. Shari Meyerson eloquently noted in her perspective piece for Thoracic Surgery News (March 2016, page 4), surgery training needs to adapt to meet the modern day needs of trainees to rest and spend time with family and friends, with those of exposure to complex clinical scenarios in a short residency period. Arguably, CT surgery trainees are some of the most motivated and driven; to limit their experience on a national level may be shortsighted. On the other hand, appropriate incorporation of advanced practice providers (APPs) may help allay some patient care challenges, free valuable family time, and allow thoracic residents to function well in a more flexible ACGME duty-hour paradigm. To add thoracic relevance to the findings of Dr. Bilimoria and his colleagues, the debate is brought to Thoracic Surgery News by our colleagues from different training pathways below:
Dr. Antonoff: “Due to the timing of my medical school matriculation, I completed my surgical clerkships in the preregulated duty-hour era. I had expectations of what my life would be like as a surgeon when I applied for the general surgery match, and frankly, my expectations prepared me for a life that would revolve around my education, my technical training, and my commitment to patient care. During my years as a junior resident, my surgical training program gradually adapted in recognition of the new guidelines, but it took time. I spent 3 years in the research lab, and, after I came out as a senior resident, I discovered that the rules of the game had totally changed. While duty hours for me, as a senior trainee, were still fairly open, I found that my interns and junior residents had to play by completely new rules. In some ways, on rare occasions, I felt frustrated and resentful of the fact that my duties as a chief resident and thoracic fellow included many of the tasks that I’d done as an intern, because my interns would ‘expire’ after 16 hours. However, much more often, I felt bad for those who came after me.
They seemed desperate to operate, eager to see their patients’ problems through to resolution, and embarrassed to have to end their days earlier than the more senior members of the team. I feel fortunate that I had years of frequent in-house call after long days in the operating room and followed by post-call days of more operating. I finished my junior years without fear of any sick patient in the hospital, I finished my general surgery training without fear of any emergent operation, and I finished my fellowship with confidence that I could get a patient through just about anything if I had access to a cannula.
My early experiences as an attending have certainly kept me humble, and I’ve spent many a night worried about my patients, rethinking choices that I’ve made and stitches that I’ve thrown. But I thank my lucky stars that I was exposed to phenomenal training, and that I had the privilege and opportunity to work the hours needed to reach a reasonable level of safety! I can only imagine that if I’d have spent fewer nights in the hospital, that I’d feel even more anxiety and nausea at this early stage of my surgical career.
As elaborated in the editorial by Dr. Birkmeyer (N Engl J Med. 2016;374:783-4), it is not surprising that patient outcomes did not immediately depend on whether the programs had adhered strictly to the ACGME duty-hour rules. Limited numbers of patients experience critical events during shift change, and hospitals are evolving to function with greater reliance on midlevel practitioners and attending physicians. I would not expect the short-term results of duty-hour flexibility to demonstrate any impact on patient care. However, I do fear that there will be a mid-term impact on trainee accountability and autonomy, which will ultimately impact the competence of the attending surgeons of the future, and downstream potential long-term impact on day-to-day patient outcomes.
As a wife and mother of 3, I recognize that we, as a specialty, need to find ways to support our trainees and their families and to help them live happy lives conducive to functioning outside the hospital. I believe that we can do this with support, mentorship, and advocacy; I do not believe that it requires cutting back on the training that we are all, in the end, so incredibly grateful to receive.”
Dr. Mara Antonoff is an assistant professor of thoracic and cardiovascular surgery at UT MD Anderson Cancer Center. She performed her General Surgery training at the University of Minnesota, 2004-2012, and her Thoracic Surgery Training at Washington University, as a traditional 2-year resident, 2012-2014.
Dr. Stephens: “There is nothing that replaces being bedside. Whether it be a postoperative patient struggling with low cardiac output syndrome overnight, or a patient with a high pressor requirement the etiology of which you are trying to uncover, or a patient you have been following who suddenly arrests, the value of seeing a patient’s trajectory longitudinally is critical to developing clinical acumen. When as an attending I will get called in the middle of the night about a postoperative patient not “doing well,” I will be drawing on my years of being on call and being bedside with my patients.
Patient care is the ultimate goal, and it is clear that overworked residents are at higher risk for making mistakes that jeopardize patient care, which nobody wants. However, the restrictions that duty hours place don’t allow the flexibility necessary for a specialty such as ours, and in fact strict adherence to such regulations inhibits opportunities for our learning. Also concerning is the “shift-work” mentality that seems to be increasingly pervasive with the implementation of duty hours. As has been well documented, and as I have seen personally, the constant patient handoffs that are requisite to implementation of duty hours pose their own perils in terms of patient safety.
Ultimately, these are our patients and we are responsible. Once we are attendings, those responsibilities will not be turned off after we have reached some prespecified hour limit.
The question then remains how best to implement a system across a wide variety of programs that ensures both patient safety and adequate clinical experience in the context of a culture of patient responsibility for the residents. As the NEJM study (N Engl J Med. 2016 374:713-2) shows, flexibility in implementation of duty hours did not result in increased complications, but resulted in improved resident satisfaction in continuity of care and handoffs. In my opinion, this study then encourages specialties such as ours to be more flexible in work hours, to encourage residents when there is a learning opportunity that previously they would be prohibited from taking part in to take hold of that opportunity, and to use this flexibility in implementation of duty hours to combat the invading “shift-work” mentality that will only jeopardize patient care.”
Dr. Elizabeth H. Stephens, MD, PhD is a Cardiothoracic Surgery, resident, PGY4, at Columbia University, New York, as an Integrated I-6 Resident.
Dr. Brown: “I took the traditional 5-year of General Surgery + 2 years of Cardiothoracic Surgery training route to becoming a General Thoracic Surgeon. My General Surgery experience was invaluable to my development as a surgeon. However, after all of those years of General Surgery cases and minimal exposure to Cardiothoracic Surgery cases, coupled with minimal overlap between the two specialties with regard to patient care, I found the learning curve in fellowship to be very steep. I was fortunate to train in a program with phenomenal physician extender support [APPs] in addition to top-notch colleagues in other specialties and excellent nursing, which allowed me to spend the majority of those 2 years in the operating room and completely focused on patient care. During that final phase of training, I welcomed flexibility with regard to the work-hour restrictions to ensure that I was acquiring the experience I needed prior to starting my own practice.”
Lisa M. Brown, MD, MAS, Assistant Professor of Thoracic Surgery, UC Davis Health System, Calif.; Training Institution: Washington University
Dr. Lee: “I started my surgical training in 2005, 2 years after the implementation of the 80-hour workweek restriction. Fortunately for my personal life, my training program took the restriction very seriously and strictly enforced it. As a result, I had scheduled periods off from work, and rarely worked more than 80 hours per week over the course of general surgery. On those occasions that I did, the next weeks, or preceding weeks would be shorter, to compensate. As a product of a 4+3 Thoracic Surgery residency in this environment, the 80-hour workweek extended to my subspecialty training. Our cardiac surgery time strictly enforced the go-home post-call policy. As a result, I believe my duty hours during Thoracic Surgery are likely shorter overall than many other programs.
Everyone hears the rumors of other programs lying about their duty hours. Fortunately, mine was not one of these. Despite this, or because of this, I received top-notch training. At the same time and more importantly, I started a family. I married my wife a week before my internship started, and am still married to the same person. We had two precious daughters during my Thoracic Surgery years. I don’t believe this would have been possible without duty-hours restrictions.
To create an environment where such a task was possible, my program hired an army of mid-level practitioners to deal with the day-to-day tasks of providing cardiothoracic surgical care to the patients, both in the intensive care unit and on the ward.
I rarely had to write a history and physical during Thoracic Surgery training. I consented fewer patients than I have fingers on my hands. I pulled even fewer chest tubes. I can now no longer remember having pulled a central line. I learned these tasks when I was a junior resident. What I did instead as a senior resident was perform over 900 cardiothoracic procedures as the primary surgeon. Now, as an attending surgeon, I still don’t write full histories and physicals by myself. I certainly don’t pull chest tubes and central lines. I consent patients by having a conversation with them, which I did as a resident, but I don’t bring a piece of paper with me in to the clinic room. I have a physician assistant who helps me fill in the gaps.
In 8 months of practice, I have performed over 15 thoracic organ transplants, repaired over 15 aortic dissections, half of whom required root replacements, performed more double-valve surgeries than straightforward single-valve replacements, started a minimally invasive atrial fibrillation surgical program, and applied almost every shred of knowledge and experience gained in 3 years of Thoracic Surgery Residency to a busy clinical practice. Most importantly, I continue to come home and watch my two daughters grow up.
With that perspective, I don’t believe the question should be whether or not programs should have the flexibility to enforce or not enforce duty-hours restrictions. It should be, how could every program find a way to effectively train residents to be good physicians and still allow them a personal life?”
Dr. Anson Lee is an Assistant Professor of Cardiac Surgery, Stanford University, Calif.; Training: 4+3 CT Residency, at Washington University, St. Louis.
Ms. Bohlman: “As a physician assistant in cardiac surgery, I represent the reality that physicians with a critical patient population appreciate consistency in their patient management. However, working in a university hospital setting also requires that surgical residents receive appropriate training. With the recently implemented duty restriction hours on resident training programs, advanced practice providers (APPs) have been utilized as an excellent solution for scheduling conflicts without compromising patient care. An example to this point is evident in my own place of work.
Approximately 1 year ago, our surgical intensive care unit transitioned from resident care to a combination of residents and APPs. At that time, the APPs were tasked with the complete care of all cardiac surgery patients. This change reduced the quantity and acuity of patients for which the residents were responsible and therefore allowed for more flexible hours along with a more manageable patient load. These changes, among others, have contributed to improved patient outcomes in the cardiac surgery patient population within our institution. With the increase in APPs that have training in various specialties, there comes an increasing ability to not only fill the gaps in scheduling but to do so with an extension of the providing physician. Although the NEJM article demonstrated no difference in patient outcomes between resident programs with restricted duty hours versus more flexible duty-hour policies, I foresee the future of medicine focusing on trained APPs as a complement to the care that the residents provide.”
Allison Bohlman is a Physician Assistant at Rush University Medical Center in the Integrated cardiovascular thoracic intensive care unit.
Several months ago, Dr. Bilimoria and his colleagues published the long awaited study in NEJM essentially contradicting adverse effects of strict duty hours on patient outcomes (N Engl J Med. 2016 374:713-2). The study, known as the FIRST trial, was published in the March issue of Thoracic Surgery News. Although the study enrolled general surgery residents, its conclusion impacts no specialty more than cardiothoracic surgery, where frequent handoffs complicate tedious perioperative care of sick patients stall learning opportunities for young trainees.
As Dr. Shari Meyerson eloquently noted in her perspective piece for Thoracic Surgery News (March 2016, page 4), surgery training needs to adapt to meet the modern day needs of trainees to rest and spend time with family and friends, with those of exposure to complex clinical scenarios in a short residency period. Arguably, CT surgery trainees are some of the most motivated and driven; to limit their experience on a national level may be shortsighted. On the other hand, appropriate incorporation of advanced practice providers (APPs) may help allay some patient care challenges, free valuable family time, and allow thoracic residents to function well in a more flexible ACGME duty-hour paradigm. To add thoracic relevance to the findings of Dr. Bilimoria and his colleagues, the debate is brought to Thoracic Surgery News by our colleagues from different training pathways below:
Dr. Antonoff: “Due to the timing of my medical school matriculation, I completed my surgical clerkships in the preregulated duty-hour era. I had expectations of what my life would be like as a surgeon when I applied for the general surgery match, and frankly, my expectations prepared me for a life that would revolve around my education, my technical training, and my commitment to patient care. During my years as a junior resident, my surgical training program gradually adapted in recognition of the new guidelines, but it took time. I spent 3 years in the research lab, and, after I came out as a senior resident, I discovered that the rules of the game had totally changed. While duty hours for me, as a senior trainee, were still fairly open, I found that my interns and junior residents had to play by completely new rules. In some ways, on rare occasions, I felt frustrated and resentful of the fact that my duties as a chief resident and thoracic fellow included many of the tasks that I’d done as an intern, because my interns would ‘expire’ after 16 hours. However, much more often, I felt bad for those who came after me.
They seemed desperate to operate, eager to see their patients’ problems through to resolution, and embarrassed to have to end their days earlier than the more senior members of the team. I feel fortunate that I had years of frequent in-house call after long days in the operating room and followed by post-call days of more operating. I finished my junior years without fear of any sick patient in the hospital, I finished my general surgery training without fear of any emergent operation, and I finished my fellowship with confidence that I could get a patient through just about anything if I had access to a cannula.
My early experiences as an attending have certainly kept me humble, and I’ve spent many a night worried about my patients, rethinking choices that I’ve made and stitches that I’ve thrown. But I thank my lucky stars that I was exposed to phenomenal training, and that I had the privilege and opportunity to work the hours needed to reach a reasonable level of safety! I can only imagine that if I’d have spent fewer nights in the hospital, that I’d feel even more anxiety and nausea at this early stage of my surgical career.
As elaborated in the editorial by Dr. Birkmeyer (N Engl J Med. 2016;374:783-4), it is not surprising that patient outcomes did not immediately depend on whether the programs had adhered strictly to the ACGME duty-hour rules. Limited numbers of patients experience critical events during shift change, and hospitals are evolving to function with greater reliance on midlevel practitioners and attending physicians. I would not expect the short-term results of duty-hour flexibility to demonstrate any impact on patient care. However, I do fear that there will be a mid-term impact on trainee accountability and autonomy, which will ultimately impact the competence of the attending surgeons of the future, and downstream potential long-term impact on day-to-day patient outcomes.
As a wife and mother of 3, I recognize that we, as a specialty, need to find ways to support our trainees and their families and to help them live happy lives conducive to functioning outside the hospital. I believe that we can do this with support, mentorship, and advocacy; I do not believe that it requires cutting back on the training that we are all, in the end, so incredibly grateful to receive.”
Dr. Mara Antonoff is an assistant professor of thoracic and cardiovascular surgery at UT MD Anderson Cancer Center. She performed her General Surgery training at the University of Minnesota, 2004-2012, and her Thoracic Surgery Training at Washington University, as a traditional 2-year resident, 2012-2014.
Dr. Stephens: “There is nothing that replaces being bedside. Whether it be a postoperative patient struggling with low cardiac output syndrome overnight, or a patient with a high pressor requirement the etiology of which you are trying to uncover, or a patient you have been following who suddenly arrests, the value of seeing a patient’s trajectory longitudinally is critical to developing clinical acumen. When as an attending I will get called in the middle of the night about a postoperative patient not “doing well,” I will be drawing on my years of being on call and being bedside with my patients.
Patient care is the ultimate goal, and it is clear that overworked residents are at higher risk for making mistakes that jeopardize patient care, which nobody wants. However, the restrictions that duty hours place don’t allow the flexibility necessary for a specialty such as ours, and in fact strict adherence to such regulations inhibits opportunities for our learning. Also concerning is the “shift-work” mentality that seems to be increasingly pervasive with the implementation of duty hours. As has been well documented, and as I have seen personally, the constant patient handoffs that are requisite to implementation of duty hours pose their own perils in terms of patient safety.
Ultimately, these are our patients and we are responsible. Once we are attendings, those responsibilities will not be turned off after we have reached some prespecified hour limit.
The question then remains how best to implement a system across a wide variety of programs that ensures both patient safety and adequate clinical experience in the context of a culture of patient responsibility for the residents. As the NEJM study (N Engl J Med. 2016 374:713-2) shows, flexibility in implementation of duty hours did not result in increased complications, but resulted in improved resident satisfaction in continuity of care and handoffs. In my opinion, this study then encourages specialties such as ours to be more flexible in work hours, to encourage residents when there is a learning opportunity that previously they would be prohibited from taking part in to take hold of that opportunity, and to use this flexibility in implementation of duty hours to combat the invading “shift-work” mentality that will only jeopardize patient care.”
Dr. Elizabeth H. Stephens, MD, PhD is a Cardiothoracic Surgery, resident, PGY4, at Columbia University, New York, as an Integrated I-6 Resident.
Dr. Brown: “I took the traditional 5-year of General Surgery + 2 years of Cardiothoracic Surgery training route to becoming a General Thoracic Surgeon. My General Surgery experience was invaluable to my development as a surgeon. However, after all of those years of General Surgery cases and minimal exposure to Cardiothoracic Surgery cases, coupled with minimal overlap between the two specialties with regard to patient care, I found the learning curve in fellowship to be very steep. I was fortunate to train in a program with phenomenal physician extender support [APPs] in addition to top-notch colleagues in other specialties and excellent nursing, which allowed me to spend the majority of those 2 years in the operating room and completely focused on patient care. During that final phase of training, I welcomed flexibility with regard to the work-hour restrictions to ensure that I was acquiring the experience I needed prior to starting my own practice.”
Lisa M. Brown, MD, MAS, Assistant Professor of Thoracic Surgery, UC Davis Health System, Calif.; Training Institution: Washington University
Dr. Lee: “I started my surgical training in 2005, 2 years after the implementation of the 80-hour workweek restriction. Fortunately for my personal life, my training program took the restriction very seriously and strictly enforced it. As a result, I had scheduled periods off from work, and rarely worked more than 80 hours per week over the course of general surgery. On those occasions that I did, the next weeks, or preceding weeks would be shorter, to compensate. As a product of a 4+3 Thoracic Surgery residency in this environment, the 80-hour workweek extended to my subspecialty training. Our cardiac surgery time strictly enforced the go-home post-call policy. As a result, I believe my duty hours during Thoracic Surgery are likely shorter overall than many other programs.
Everyone hears the rumors of other programs lying about their duty hours. Fortunately, mine was not one of these. Despite this, or because of this, I received top-notch training. At the same time and more importantly, I started a family. I married my wife a week before my internship started, and am still married to the same person. We had two precious daughters during my Thoracic Surgery years. I don’t believe this would have been possible without duty-hours restrictions.
To create an environment where such a task was possible, my program hired an army of mid-level practitioners to deal with the day-to-day tasks of providing cardiothoracic surgical care to the patients, both in the intensive care unit and on the ward.
I rarely had to write a history and physical during Thoracic Surgery training. I consented fewer patients than I have fingers on my hands. I pulled even fewer chest tubes. I can now no longer remember having pulled a central line. I learned these tasks when I was a junior resident. What I did instead as a senior resident was perform over 900 cardiothoracic procedures as the primary surgeon. Now, as an attending surgeon, I still don’t write full histories and physicals by myself. I certainly don’t pull chest tubes and central lines. I consent patients by having a conversation with them, which I did as a resident, but I don’t bring a piece of paper with me in to the clinic room. I have a physician assistant who helps me fill in the gaps.
In 8 months of practice, I have performed over 15 thoracic organ transplants, repaired over 15 aortic dissections, half of whom required root replacements, performed more double-valve surgeries than straightforward single-valve replacements, started a minimally invasive atrial fibrillation surgical program, and applied almost every shred of knowledge and experience gained in 3 years of Thoracic Surgery Residency to a busy clinical practice. Most importantly, I continue to come home and watch my two daughters grow up.
With that perspective, I don’t believe the question should be whether or not programs should have the flexibility to enforce or not enforce duty-hours restrictions. It should be, how could every program find a way to effectively train residents to be good physicians and still allow them a personal life?”
Dr. Anson Lee is an Assistant Professor of Cardiac Surgery, Stanford University, Calif.; Training: 4+3 CT Residency, at Washington University, St. Louis.
Ms. Bohlman: “As a physician assistant in cardiac surgery, I represent the reality that physicians with a critical patient population appreciate consistency in their patient management. However, working in a university hospital setting also requires that surgical residents receive appropriate training. With the recently implemented duty restriction hours on resident training programs, advanced practice providers (APPs) have been utilized as an excellent solution for scheduling conflicts without compromising patient care. An example to this point is evident in my own place of work.
Approximately 1 year ago, our surgical intensive care unit transitioned from resident care to a combination of residents and APPs. At that time, the APPs were tasked with the complete care of all cardiac surgery patients. This change reduced the quantity and acuity of patients for which the residents were responsible and therefore allowed for more flexible hours along with a more manageable patient load. These changes, among others, have contributed to improved patient outcomes in the cardiac surgery patient population within our institution. With the increase in APPs that have training in various specialties, there comes an increasing ability to not only fill the gaps in scheduling but to do so with an extension of the providing physician. Although the NEJM article demonstrated no difference in patient outcomes between resident programs with restricted duty hours versus more flexible duty-hour policies, I foresee the future of medicine focusing on trained APPs as a complement to the care that the residents provide.”
Allison Bohlman is a Physician Assistant at Rush University Medical Center in the Integrated cardiovascular thoracic intensive care unit.
Several months ago, Dr. Bilimoria and his colleagues published the long awaited study in NEJM essentially contradicting adverse effects of strict duty hours on patient outcomes (N Engl J Med. 2016 374:713-2). The study, known as the FIRST trial, was published in the March issue of Thoracic Surgery News. Although the study enrolled general surgery residents, its conclusion impacts no specialty more than cardiothoracic surgery, where frequent handoffs complicate tedious perioperative care of sick patients stall learning opportunities for young trainees.
As Dr. Shari Meyerson eloquently noted in her perspective piece for Thoracic Surgery News (March 2016, page 4), surgery training needs to adapt to meet the modern day needs of trainees to rest and spend time with family and friends, with those of exposure to complex clinical scenarios in a short residency period. Arguably, CT surgery trainees are some of the most motivated and driven; to limit their experience on a national level may be shortsighted. On the other hand, appropriate incorporation of advanced practice providers (APPs) may help allay some patient care challenges, free valuable family time, and allow thoracic residents to function well in a more flexible ACGME duty-hour paradigm. To add thoracic relevance to the findings of Dr. Bilimoria and his colleagues, the debate is brought to Thoracic Surgery News by our colleagues from different training pathways below:
Dr. Antonoff: “Due to the timing of my medical school matriculation, I completed my surgical clerkships in the preregulated duty-hour era. I had expectations of what my life would be like as a surgeon when I applied for the general surgery match, and frankly, my expectations prepared me for a life that would revolve around my education, my technical training, and my commitment to patient care. During my years as a junior resident, my surgical training program gradually adapted in recognition of the new guidelines, but it took time. I spent 3 years in the research lab, and, after I came out as a senior resident, I discovered that the rules of the game had totally changed. While duty hours for me, as a senior trainee, were still fairly open, I found that my interns and junior residents had to play by completely new rules. In some ways, on rare occasions, I felt frustrated and resentful of the fact that my duties as a chief resident and thoracic fellow included many of the tasks that I’d done as an intern, because my interns would ‘expire’ after 16 hours. However, much more often, I felt bad for those who came after me.
They seemed desperate to operate, eager to see their patients’ problems through to resolution, and embarrassed to have to end their days earlier than the more senior members of the team. I feel fortunate that I had years of frequent in-house call after long days in the operating room and followed by post-call days of more operating. I finished my junior years without fear of any sick patient in the hospital, I finished my general surgery training without fear of any emergent operation, and I finished my fellowship with confidence that I could get a patient through just about anything if I had access to a cannula.
My early experiences as an attending have certainly kept me humble, and I’ve spent many a night worried about my patients, rethinking choices that I’ve made and stitches that I’ve thrown. But I thank my lucky stars that I was exposed to phenomenal training, and that I had the privilege and opportunity to work the hours needed to reach a reasonable level of safety! I can only imagine that if I’d have spent fewer nights in the hospital, that I’d feel even more anxiety and nausea at this early stage of my surgical career.
As elaborated in the editorial by Dr. Birkmeyer (N Engl J Med. 2016;374:783-4), it is not surprising that patient outcomes did not immediately depend on whether the programs had adhered strictly to the ACGME duty-hour rules. Limited numbers of patients experience critical events during shift change, and hospitals are evolving to function with greater reliance on midlevel practitioners and attending physicians. I would not expect the short-term results of duty-hour flexibility to demonstrate any impact on patient care. However, I do fear that there will be a mid-term impact on trainee accountability and autonomy, which will ultimately impact the competence of the attending surgeons of the future, and downstream potential long-term impact on day-to-day patient outcomes.
As a wife and mother of 3, I recognize that we, as a specialty, need to find ways to support our trainees and their families and to help them live happy lives conducive to functioning outside the hospital. I believe that we can do this with support, mentorship, and advocacy; I do not believe that it requires cutting back on the training that we are all, in the end, so incredibly grateful to receive.”
Dr. Mara Antonoff is an assistant professor of thoracic and cardiovascular surgery at UT MD Anderson Cancer Center. She performed her General Surgery training at the University of Minnesota, 2004-2012, and her Thoracic Surgery Training at Washington University, as a traditional 2-year resident, 2012-2014.
Dr. Stephens: “There is nothing that replaces being bedside. Whether it be a postoperative patient struggling with low cardiac output syndrome overnight, or a patient with a high pressor requirement the etiology of which you are trying to uncover, or a patient you have been following who suddenly arrests, the value of seeing a patient’s trajectory longitudinally is critical to developing clinical acumen. When as an attending I will get called in the middle of the night about a postoperative patient not “doing well,” I will be drawing on my years of being on call and being bedside with my patients.
Patient care is the ultimate goal, and it is clear that overworked residents are at higher risk for making mistakes that jeopardize patient care, which nobody wants. However, the restrictions that duty hours place don’t allow the flexibility necessary for a specialty such as ours, and in fact strict adherence to such regulations inhibits opportunities for our learning. Also concerning is the “shift-work” mentality that seems to be increasingly pervasive with the implementation of duty hours. As has been well documented, and as I have seen personally, the constant patient handoffs that are requisite to implementation of duty hours pose their own perils in terms of patient safety.
Ultimately, these are our patients and we are responsible. Once we are attendings, those responsibilities will not be turned off after we have reached some prespecified hour limit.
The question then remains how best to implement a system across a wide variety of programs that ensures both patient safety and adequate clinical experience in the context of a culture of patient responsibility for the residents. As the NEJM study (N Engl J Med. 2016 374:713-2) shows, flexibility in implementation of duty hours did not result in increased complications, but resulted in improved resident satisfaction in continuity of care and handoffs. In my opinion, this study then encourages specialties such as ours to be more flexible in work hours, to encourage residents when there is a learning opportunity that previously they would be prohibited from taking part in to take hold of that opportunity, and to use this flexibility in implementation of duty hours to combat the invading “shift-work” mentality that will only jeopardize patient care.”
Dr. Elizabeth H. Stephens, MD, PhD is a Cardiothoracic Surgery, resident, PGY4, at Columbia University, New York, as an Integrated I-6 Resident.
Dr. Brown: “I took the traditional 5-year of General Surgery + 2 years of Cardiothoracic Surgery training route to becoming a General Thoracic Surgeon. My General Surgery experience was invaluable to my development as a surgeon. However, after all of those years of General Surgery cases and minimal exposure to Cardiothoracic Surgery cases, coupled with minimal overlap between the two specialties with regard to patient care, I found the learning curve in fellowship to be very steep. I was fortunate to train in a program with phenomenal physician extender support [APPs] in addition to top-notch colleagues in other specialties and excellent nursing, which allowed me to spend the majority of those 2 years in the operating room and completely focused on patient care. During that final phase of training, I welcomed flexibility with regard to the work-hour restrictions to ensure that I was acquiring the experience I needed prior to starting my own practice.”
Lisa M. Brown, MD, MAS, Assistant Professor of Thoracic Surgery, UC Davis Health System, Calif.; Training Institution: Washington University
Dr. Lee: “I started my surgical training in 2005, 2 years after the implementation of the 80-hour workweek restriction. Fortunately for my personal life, my training program took the restriction very seriously and strictly enforced it. As a result, I had scheduled periods off from work, and rarely worked more than 80 hours per week over the course of general surgery. On those occasions that I did, the next weeks, or preceding weeks would be shorter, to compensate. As a product of a 4+3 Thoracic Surgery residency in this environment, the 80-hour workweek extended to my subspecialty training. Our cardiac surgery time strictly enforced the go-home post-call policy. As a result, I believe my duty hours during Thoracic Surgery are likely shorter overall than many other programs.
Everyone hears the rumors of other programs lying about their duty hours. Fortunately, mine was not one of these. Despite this, or because of this, I received top-notch training. At the same time and more importantly, I started a family. I married my wife a week before my internship started, and am still married to the same person. We had two precious daughters during my Thoracic Surgery years. I don’t believe this would have been possible without duty-hours restrictions.
To create an environment where such a task was possible, my program hired an army of mid-level practitioners to deal with the day-to-day tasks of providing cardiothoracic surgical care to the patients, both in the intensive care unit and on the ward.
I rarely had to write a history and physical during Thoracic Surgery training. I consented fewer patients than I have fingers on my hands. I pulled even fewer chest tubes. I can now no longer remember having pulled a central line. I learned these tasks when I was a junior resident. What I did instead as a senior resident was perform over 900 cardiothoracic procedures as the primary surgeon. Now, as an attending surgeon, I still don’t write full histories and physicals by myself. I certainly don’t pull chest tubes and central lines. I consent patients by having a conversation with them, which I did as a resident, but I don’t bring a piece of paper with me in to the clinic room. I have a physician assistant who helps me fill in the gaps.
In 8 months of practice, I have performed over 15 thoracic organ transplants, repaired over 15 aortic dissections, half of whom required root replacements, performed more double-valve surgeries than straightforward single-valve replacements, started a minimally invasive atrial fibrillation surgical program, and applied almost every shred of knowledge and experience gained in 3 years of Thoracic Surgery Residency to a busy clinical practice. Most importantly, I continue to come home and watch my two daughters grow up.
With that perspective, I don’t believe the question should be whether or not programs should have the flexibility to enforce or not enforce duty-hours restrictions. It should be, how could every program find a way to effectively train residents to be good physicians and still allow them a personal life?”
Dr. Anson Lee is an Assistant Professor of Cardiac Surgery, Stanford University, Calif.; Training: 4+3 CT Residency, at Washington University, St. Louis.
Ms. Bohlman: “As a physician assistant in cardiac surgery, I represent the reality that physicians with a critical patient population appreciate consistency in their patient management. However, working in a university hospital setting also requires that surgical residents receive appropriate training. With the recently implemented duty restriction hours on resident training programs, advanced practice providers (APPs) have been utilized as an excellent solution for scheduling conflicts without compromising patient care. An example to this point is evident in my own place of work.
Approximately 1 year ago, our surgical intensive care unit transitioned from resident care to a combination of residents and APPs. At that time, the APPs were tasked with the complete care of all cardiac surgery patients. This change reduced the quantity and acuity of patients for which the residents were responsible and therefore allowed for more flexible hours along with a more manageable patient load. These changes, among others, have contributed to improved patient outcomes in the cardiac surgery patient population within our institution. With the increase in APPs that have training in various specialties, there comes an increasing ability to not only fill the gaps in scheduling but to do so with an extension of the providing physician. Although the NEJM article demonstrated no difference in patient outcomes between resident programs with restricted duty hours versus more flexible duty-hour policies, I foresee the future of medicine focusing on trained APPs as a complement to the care that the residents provide.”
Allison Bohlman is a Physician Assistant at Rush University Medical Center in the Integrated cardiovascular thoracic intensive care unit.
Noncompete clauses: Be wary, negotiate early
Noncompete clauses can severely limit a doctor’s business options and create serious financial challenges, so negotiate with employers early and watch out for tricky contract terms that could stifle future opportunities.
That is the advice from health law experts around the country. They point out that when it comes to noncompete clauses – employment contract language that limits where physicians can practice after employment ends or is terminated – doctors should pay close attention, especially to the following:
Geographical limitations
Distance requirements within noncompete provisions are a top issue that can trip up doctors, Bloomfield Hills, Mich., health law attorney Mark S. Kopson said. The clause typically specifies that a physician cannot practice within a certain radius of the former employer. However, if an employer has three offices for instance, that 10-mile radius can quickly become a 30-mile radius or more depending how the provision is worded. Mr. Kopson recalled a recent client who practiced for 5 years in one office and was transferred to an office in another town for 30 days. He was then terminated, and his employer attempted to enforce contract terms that would prevent him from practicing within a 10-mile radius of both offices. A court determined that the employer was acting in bad faith and sought an unfair competitive advantage.
“But No. 1, you don’t want to have to go to court,” Mr. Kopson said. “And No. 2, you can have the best lawyer, but once it’s in the hands of the judge or the jury, anything can happen. That’s why you really want to do the work on this up front.”
When negotiating noncompete clauses, be cognizant of where distances are being measured from and around, the legal experts stress. Also, be clear with employers about what defines a reasonable distance, based on the geographic spread of their patient base.
“What’s reasonable for a family practice physician is probably not going to be reasonable for a pediatric neurosurgeon, as they draw their patients from varying distances,” he said. “Also, negotiate to ensure that the length of time of the restriction is reasonable. Taking into account, both the distance and time period, the physician must still be able to earn a living.”
Time frame restrictions
Negotiate the shortest duration that you can, advises Greenbelt, Md., labor and employment attorney Jay P. Holland. Noncompete provisions typically limit a doctor from practicing around a certain radius for 1-5 years, but some employers may try to enforce longer time periods.
“Consider your career and lifestyle goals carefully prior to entering into a noncompete,” Mr. Holland said. “The first approach should always be an attempt to exclude the noncompete from your prospective agreement if you are joining a practice. If a noncompete is unavoidable, then strive to make it the least onerous possible. Ask yourself prior to signing an agreement, ‘If I were to leave this practice, what are the restrictions I could live with? Are the restrictions reasonable?’ ”
Knowing your state’s law is key. State regulation of noncompete provisions widely differ. States such as California broadly hold that noncompete contracts are per se invalid – even if narrowly tailored – unless necessary to protect trade secrets. States such as Maryland allow the provisions only if area and duration restrictions are reasonable and do not impose undue hardship on employees. Three states – Colorado, Delaware, and Massachusetts – have laws that strictly prohibit noncompete clauses in physician contracts.
“Most other states will generally enforce noncompete clauses so long as their terms are reasonable in light of the interests of the employer, the employee, and the general public,” Mr. Holland said. “Therefore, noncompete clauses should be no greater in scope than is necessary to protect the business or goodwill of the employer.”
Patient retention problems
Watch out for contract language referring to “trade secrets,” adds Los Angeles health law attorney Andrew H. Selesnick. Trade secret clauses are often lengthy and typically state that physicians cannot use or retain information from the employer that is considered confidential. Because patient lists are usually considered confidential, these terms could potentially prohibit patients from following their doctor.
“If you want to leave and take your patients with you, there may be some trade secret implications associated with that,” Mr. Selesnick said. “The ability to be able to move patients is significant and can have significant financial impacts. Know what you’re getting into.”
If bringing patients with them to a new practice, doctors should make sure the employment agreement excludes these patients from any nonsolicitation provision at the time the doctor leaves, notes Mr. Holland. Include language that states physicians can retain patients they originally brought to the practice when they depart without violating the agreement.
Make sure to review any proposed noncompete clauses in relation to proposed termination provisions, Mr. Kopson said. Doctors should negotiate language that ensures noncompete obligations will be null and void if physicians are terminated without cause (if such terminations are permitted by the contract), or if the employer breaches the contract.
Seeking the advice of an experienced contract attorney before signing a noncompete clause can save doctors significant time, money, and heartache in the long run, Mr. Kopson notes.
“The biggest risk is signing a contract that has such a clause with an expectation that it will not be enforced,” he said. “If [clauses are] properly drafted, they’re going to be binding. If you get the help up front, it’s going to be a lot less expensive than having your life turned upside down because you’re stuck with a noncompete that has bad terms in it.”
Unreasonable terms
Once signed, getting out of non-compete clauses can be tricky, Mr. Selesnick said. However, doctors can usually escape them if they can prove the terms are unreasonable.
“You can get out of them, especially if they’re very restrictive and say you can’t practice within an area that may prevent you from earning your livelihood,” Mr. Selesnick said. “Courts [generally] think that employees should be able to leave and be able to get a job elsewhere, even if it’s across the street.”
Courts are typically more favorable to physician-employees than independent contractors when it comes to noncompete clauses, Mr. Selesnick said. Independent contractors are generally viewed as having more power over their work than physician-employees. They may have a tougher time convincing a court that such provisions will harm their employment options.
When seeking to enforce a disputed noncompete agreement, employers frequently will request a court-ordered temporary restraining order or injunction to enforce the clause, Mr. Holland said. Judges consider general principles of fairness and equity, and balance the relative harm to the employer and the employee, when deciding whether to issue the injunction. The employee-physician can also try to beat the employer to the courthouse steps by filing a “declaratory judgment” lawsuit that seeks guidance from the court on the contract’s enforceability.
“Typically, employers attempt to do that which is in their best economic interest,” Mr. Holland said. “If a proposal can be negotiated where the employer’s economic well-being is not threatened, then the employer should have a strong interest in a compromise.”
On Twitter @legal_med
Noncompete clauses can severely limit a doctor’s business options and create serious financial challenges, so negotiate with employers early and watch out for tricky contract terms that could stifle future opportunities.
That is the advice from health law experts around the country. They point out that when it comes to noncompete clauses – employment contract language that limits where physicians can practice after employment ends or is terminated – doctors should pay close attention, especially to the following:
Geographical limitations
Distance requirements within noncompete provisions are a top issue that can trip up doctors, Bloomfield Hills, Mich., health law attorney Mark S. Kopson said. The clause typically specifies that a physician cannot practice within a certain radius of the former employer. However, if an employer has three offices for instance, that 10-mile radius can quickly become a 30-mile radius or more depending how the provision is worded. Mr. Kopson recalled a recent client who practiced for 5 years in one office and was transferred to an office in another town for 30 days. He was then terminated, and his employer attempted to enforce contract terms that would prevent him from practicing within a 10-mile radius of both offices. A court determined that the employer was acting in bad faith and sought an unfair competitive advantage.
“But No. 1, you don’t want to have to go to court,” Mr. Kopson said. “And No. 2, you can have the best lawyer, but once it’s in the hands of the judge or the jury, anything can happen. That’s why you really want to do the work on this up front.”
When negotiating noncompete clauses, be cognizant of where distances are being measured from and around, the legal experts stress. Also, be clear with employers about what defines a reasonable distance, based on the geographic spread of their patient base.
“What’s reasonable for a family practice physician is probably not going to be reasonable for a pediatric neurosurgeon, as they draw their patients from varying distances,” he said. “Also, negotiate to ensure that the length of time of the restriction is reasonable. Taking into account, both the distance and time period, the physician must still be able to earn a living.”
Time frame restrictions
Negotiate the shortest duration that you can, advises Greenbelt, Md., labor and employment attorney Jay P. Holland. Noncompete provisions typically limit a doctor from practicing around a certain radius for 1-5 years, but some employers may try to enforce longer time periods.
“Consider your career and lifestyle goals carefully prior to entering into a noncompete,” Mr. Holland said. “The first approach should always be an attempt to exclude the noncompete from your prospective agreement if you are joining a practice. If a noncompete is unavoidable, then strive to make it the least onerous possible. Ask yourself prior to signing an agreement, ‘If I were to leave this practice, what are the restrictions I could live with? Are the restrictions reasonable?’ ”
Knowing your state’s law is key. State regulation of noncompete provisions widely differ. States such as California broadly hold that noncompete contracts are per se invalid – even if narrowly tailored – unless necessary to protect trade secrets. States such as Maryland allow the provisions only if area and duration restrictions are reasonable and do not impose undue hardship on employees. Three states – Colorado, Delaware, and Massachusetts – have laws that strictly prohibit noncompete clauses in physician contracts.
“Most other states will generally enforce noncompete clauses so long as their terms are reasonable in light of the interests of the employer, the employee, and the general public,” Mr. Holland said. “Therefore, noncompete clauses should be no greater in scope than is necessary to protect the business or goodwill of the employer.”
Patient retention problems
Watch out for contract language referring to “trade secrets,” adds Los Angeles health law attorney Andrew H. Selesnick. Trade secret clauses are often lengthy and typically state that physicians cannot use or retain information from the employer that is considered confidential. Because patient lists are usually considered confidential, these terms could potentially prohibit patients from following their doctor.
“If you want to leave and take your patients with you, there may be some trade secret implications associated with that,” Mr. Selesnick said. “The ability to be able to move patients is significant and can have significant financial impacts. Know what you’re getting into.”
If bringing patients with them to a new practice, doctors should make sure the employment agreement excludes these patients from any nonsolicitation provision at the time the doctor leaves, notes Mr. Holland. Include language that states physicians can retain patients they originally brought to the practice when they depart without violating the agreement.
Make sure to review any proposed noncompete clauses in relation to proposed termination provisions, Mr. Kopson said. Doctors should negotiate language that ensures noncompete obligations will be null and void if physicians are terminated without cause (if such terminations are permitted by the contract), or if the employer breaches the contract.
Seeking the advice of an experienced contract attorney before signing a noncompete clause can save doctors significant time, money, and heartache in the long run, Mr. Kopson notes.
“The biggest risk is signing a contract that has such a clause with an expectation that it will not be enforced,” he said. “If [clauses are] properly drafted, they’re going to be binding. If you get the help up front, it’s going to be a lot less expensive than having your life turned upside down because you’re stuck with a noncompete that has bad terms in it.”
Unreasonable terms
Once signed, getting out of non-compete clauses can be tricky, Mr. Selesnick said. However, doctors can usually escape them if they can prove the terms are unreasonable.
“You can get out of them, especially if they’re very restrictive and say you can’t practice within an area that may prevent you from earning your livelihood,” Mr. Selesnick said. “Courts [generally] think that employees should be able to leave and be able to get a job elsewhere, even if it’s across the street.”
Courts are typically more favorable to physician-employees than independent contractors when it comes to noncompete clauses, Mr. Selesnick said. Independent contractors are generally viewed as having more power over their work than physician-employees. They may have a tougher time convincing a court that such provisions will harm their employment options.
When seeking to enforce a disputed noncompete agreement, employers frequently will request a court-ordered temporary restraining order or injunction to enforce the clause, Mr. Holland said. Judges consider general principles of fairness and equity, and balance the relative harm to the employer and the employee, when deciding whether to issue the injunction. The employee-physician can also try to beat the employer to the courthouse steps by filing a “declaratory judgment” lawsuit that seeks guidance from the court on the contract’s enforceability.
“Typically, employers attempt to do that which is in their best economic interest,” Mr. Holland said. “If a proposal can be negotiated where the employer’s economic well-being is not threatened, then the employer should have a strong interest in a compromise.”
On Twitter @legal_med
Noncompete clauses can severely limit a doctor’s business options and create serious financial challenges, so negotiate with employers early and watch out for tricky contract terms that could stifle future opportunities.
That is the advice from health law experts around the country. They point out that when it comes to noncompete clauses – employment contract language that limits where physicians can practice after employment ends or is terminated – doctors should pay close attention, especially to the following:
Geographical limitations
Distance requirements within noncompete provisions are a top issue that can trip up doctors, Bloomfield Hills, Mich., health law attorney Mark S. Kopson said. The clause typically specifies that a physician cannot practice within a certain radius of the former employer. However, if an employer has three offices for instance, that 10-mile radius can quickly become a 30-mile radius or more depending how the provision is worded. Mr. Kopson recalled a recent client who practiced for 5 years in one office and was transferred to an office in another town for 30 days. He was then terminated, and his employer attempted to enforce contract terms that would prevent him from practicing within a 10-mile radius of both offices. A court determined that the employer was acting in bad faith and sought an unfair competitive advantage.
“But No. 1, you don’t want to have to go to court,” Mr. Kopson said. “And No. 2, you can have the best lawyer, but once it’s in the hands of the judge or the jury, anything can happen. That’s why you really want to do the work on this up front.”
When negotiating noncompete clauses, be cognizant of where distances are being measured from and around, the legal experts stress. Also, be clear with employers about what defines a reasonable distance, based on the geographic spread of their patient base.
“What’s reasonable for a family practice physician is probably not going to be reasonable for a pediatric neurosurgeon, as they draw their patients from varying distances,” he said. “Also, negotiate to ensure that the length of time of the restriction is reasonable. Taking into account, both the distance and time period, the physician must still be able to earn a living.”
Time frame restrictions
Negotiate the shortest duration that you can, advises Greenbelt, Md., labor and employment attorney Jay P. Holland. Noncompete provisions typically limit a doctor from practicing around a certain radius for 1-5 years, but some employers may try to enforce longer time periods.
“Consider your career and lifestyle goals carefully prior to entering into a noncompete,” Mr. Holland said. “The first approach should always be an attempt to exclude the noncompete from your prospective agreement if you are joining a practice. If a noncompete is unavoidable, then strive to make it the least onerous possible. Ask yourself prior to signing an agreement, ‘If I were to leave this practice, what are the restrictions I could live with? Are the restrictions reasonable?’ ”
Knowing your state’s law is key. State regulation of noncompete provisions widely differ. States such as California broadly hold that noncompete contracts are per se invalid – even if narrowly tailored – unless necessary to protect trade secrets. States such as Maryland allow the provisions only if area and duration restrictions are reasonable and do not impose undue hardship on employees. Three states – Colorado, Delaware, and Massachusetts – have laws that strictly prohibit noncompete clauses in physician contracts.
“Most other states will generally enforce noncompete clauses so long as their terms are reasonable in light of the interests of the employer, the employee, and the general public,” Mr. Holland said. “Therefore, noncompete clauses should be no greater in scope than is necessary to protect the business or goodwill of the employer.”
Patient retention problems
Watch out for contract language referring to “trade secrets,” adds Los Angeles health law attorney Andrew H. Selesnick. Trade secret clauses are often lengthy and typically state that physicians cannot use or retain information from the employer that is considered confidential. Because patient lists are usually considered confidential, these terms could potentially prohibit patients from following their doctor.
“If you want to leave and take your patients with you, there may be some trade secret implications associated with that,” Mr. Selesnick said. “The ability to be able to move patients is significant and can have significant financial impacts. Know what you’re getting into.”
If bringing patients with them to a new practice, doctors should make sure the employment agreement excludes these patients from any nonsolicitation provision at the time the doctor leaves, notes Mr. Holland. Include language that states physicians can retain patients they originally brought to the practice when they depart without violating the agreement.
Make sure to review any proposed noncompete clauses in relation to proposed termination provisions, Mr. Kopson said. Doctors should negotiate language that ensures noncompete obligations will be null and void if physicians are terminated without cause (if such terminations are permitted by the contract), or if the employer breaches the contract.
Seeking the advice of an experienced contract attorney before signing a noncompete clause can save doctors significant time, money, and heartache in the long run, Mr. Kopson notes.
“The biggest risk is signing a contract that has such a clause with an expectation that it will not be enforced,” he said. “If [clauses are] properly drafted, they’re going to be binding. If you get the help up front, it’s going to be a lot less expensive than having your life turned upside down because you’re stuck with a noncompete that has bad terms in it.”
Unreasonable terms
Once signed, getting out of non-compete clauses can be tricky, Mr. Selesnick said. However, doctors can usually escape them if they can prove the terms are unreasonable.
“You can get out of them, especially if they’re very restrictive and say you can’t practice within an area that may prevent you from earning your livelihood,” Mr. Selesnick said. “Courts [generally] think that employees should be able to leave and be able to get a job elsewhere, even if it’s across the street.”
Courts are typically more favorable to physician-employees than independent contractors when it comes to noncompete clauses, Mr. Selesnick said. Independent contractors are generally viewed as having more power over their work than physician-employees. They may have a tougher time convincing a court that such provisions will harm their employment options.
When seeking to enforce a disputed noncompete agreement, employers frequently will request a court-ordered temporary restraining order or injunction to enforce the clause, Mr. Holland said. Judges consider general principles of fairness and equity, and balance the relative harm to the employer and the employee, when deciding whether to issue the injunction. The employee-physician can also try to beat the employer to the courthouse steps by filing a “declaratory judgment” lawsuit that seeks guidance from the court on the contract’s enforceability.
“Typically, employers attempt to do that which is in their best economic interest,” Mr. Holland said. “If a proposal can be negotiated where the employer’s economic well-being is not threatened, then the employer should have a strong interest in a compromise.”
On Twitter @legal_med
Vascular: The Final Frontier - Pushing vascular science where no science has gone before
Space is truly a magical place, enchanting philosophers, scientists, artists and dreamers. From ancient civilizations that found pantheons of gods among the stars, to novelist Andy Weir’s visionary tale of human efforts to colonize Mars recently portrayed in the movie “The Martian,” to George Lucas’ epic drama between Jedis and Sith lords in “Star Wars,” it is clear that space draws humanity to push the frontiers of science and technology – or maybe just draws us to the box office.
Nonetheless, in this day and age there are astronauts and cosmonauts who have colonized lower earth orbit (LEO) on the International Space Station (ISS), in a situation quite similar to that of the station Arthur C. Clark envisioned in his 1968 science fiction novel, “2001: A Space Odyssey.”
Unfortunately, human physiology, which has evolved in and grown accustomed to Earth’s gravity, is completely altered in space where there is either no gravity effect or different gravitational pulls result from different planetary bodies. Because of this unique medical anomaly, the ISS is a platform for research of interest to a forward-thinking vascular specialist.
Dr. Richard Hughson, from the University of Waterloo in Waterloo, Ontario, is researching vascular aging in spaceflight crew members. His work is a part of the Schlegel-University of Waterloo Research Institute for Aging, where he is theme leader/chair of vascular aging and brain health and holds the Schlegel Research Chair in that discipline.
Dr. Hughson is supported by the Canadian Space Agency (CSA) and Canadian Institute for Health Research (CIHR) He discussed his research in a recent audio interview (http://cihr-irsc.gc.ca/e/49523.html).
Observations have demonstrated that short-duration and extended spaceflight missions may simulate accelerated vascular aging in some of these highly fit individuals traveling to space. Specifically, spaceflight crew members have been shown to have difficulty controlling a rise in their blood pressure, perhaps secondary to the loss of Earth’s gravity, but rather in the inherent cephalad fluid shift (as blood no longer pools in the legs). In addition, significant postflight postural hypotension and physical deconditioning with resultant sarcopenia and osteopenia are known to occur.
Dr. Hughson has shown through ultrasonography that the carotid arteries of spaceflight crew members are considerably stiffer compared to their preflight arteries and that they appear to have “aged the equivalent of 20-30 years in stiffness.” The ramifications of this type of research on the study of the normal earthbound vascular aging processes are under investigation.
To counteract the effects of vascular aging and physical deconditioning in space, physical activity is key; however, the 30 minutes per day allotted to busy astronauts amid their responsibilities is just not cutting it, according to Dr. Hughson. Missions are being extended for longer periods of time, leading to serious physical consequences, For example, American astronaut Scott Kelly’s year in space will certainly result in considerable accelerated aging in his arterial system. Thus, it becomes increasingly necessary to understand and prevent the vascular aging process in astronauts, future spaceflight crew members, and perhaps one day those seeking to colonize the Moon, Mars, and beyond.
When colonization time arrives, space agencies certainly should be in the market for well-qualified vascular specialists.
Perhaps great job opportunities await those in our profession who will be brave enough to leave Earth’s cradle.
Dr Drudi is a vascular surgery resident at McGill University, Montreal.
Space is truly a magical place, enchanting philosophers, scientists, artists and dreamers. From ancient civilizations that found pantheons of gods among the stars, to novelist Andy Weir’s visionary tale of human efforts to colonize Mars recently portrayed in the movie “The Martian,” to George Lucas’ epic drama between Jedis and Sith lords in “Star Wars,” it is clear that space draws humanity to push the frontiers of science and technology – or maybe just draws us to the box office.
Nonetheless, in this day and age there are astronauts and cosmonauts who have colonized lower earth orbit (LEO) on the International Space Station (ISS), in a situation quite similar to that of the station Arthur C. Clark envisioned in his 1968 science fiction novel, “2001: A Space Odyssey.”
Unfortunately, human physiology, which has evolved in and grown accustomed to Earth’s gravity, is completely altered in space where there is either no gravity effect or different gravitational pulls result from different planetary bodies. Because of this unique medical anomaly, the ISS is a platform for research of interest to a forward-thinking vascular specialist.
Dr. Richard Hughson, from the University of Waterloo in Waterloo, Ontario, is researching vascular aging in spaceflight crew members. His work is a part of the Schlegel-University of Waterloo Research Institute for Aging, where he is theme leader/chair of vascular aging and brain health and holds the Schlegel Research Chair in that discipline.
Dr. Hughson is supported by the Canadian Space Agency (CSA) and Canadian Institute for Health Research (CIHR) He discussed his research in a recent audio interview (http://cihr-irsc.gc.ca/e/49523.html).
Observations have demonstrated that short-duration and extended spaceflight missions may simulate accelerated vascular aging in some of these highly fit individuals traveling to space. Specifically, spaceflight crew members have been shown to have difficulty controlling a rise in their blood pressure, perhaps secondary to the loss of Earth’s gravity, but rather in the inherent cephalad fluid shift (as blood no longer pools in the legs). In addition, significant postflight postural hypotension and physical deconditioning with resultant sarcopenia and osteopenia are known to occur.
Dr. Hughson has shown through ultrasonography that the carotid arteries of spaceflight crew members are considerably stiffer compared to their preflight arteries and that they appear to have “aged the equivalent of 20-30 years in stiffness.” The ramifications of this type of research on the study of the normal earthbound vascular aging processes are under investigation.
To counteract the effects of vascular aging and physical deconditioning in space, physical activity is key; however, the 30 minutes per day allotted to busy astronauts amid their responsibilities is just not cutting it, according to Dr. Hughson. Missions are being extended for longer periods of time, leading to serious physical consequences, For example, American astronaut Scott Kelly’s year in space will certainly result in considerable accelerated aging in his arterial system. Thus, it becomes increasingly necessary to understand and prevent the vascular aging process in astronauts, future spaceflight crew members, and perhaps one day those seeking to colonize the Moon, Mars, and beyond.
When colonization time arrives, space agencies certainly should be in the market for well-qualified vascular specialists.
Perhaps great job opportunities await those in our profession who will be brave enough to leave Earth’s cradle.
Dr Drudi is a vascular surgery resident at McGill University, Montreal.
Space is truly a magical place, enchanting philosophers, scientists, artists and dreamers. From ancient civilizations that found pantheons of gods among the stars, to novelist Andy Weir’s visionary tale of human efforts to colonize Mars recently portrayed in the movie “The Martian,” to George Lucas’ epic drama between Jedis and Sith lords in “Star Wars,” it is clear that space draws humanity to push the frontiers of science and technology – or maybe just draws us to the box office.
Nonetheless, in this day and age there are astronauts and cosmonauts who have colonized lower earth orbit (LEO) on the International Space Station (ISS), in a situation quite similar to that of the station Arthur C. Clark envisioned in his 1968 science fiction novel, “2001: A Space Odyssey.”
Unfortunately, human physiology, which has evolved in and grown accustomed to Earth’s gravity, is completely altered in space where there is either no gravity effect or different gravitational pulls result from different planetary bodies. Because of this unique medical anomaly, the ISS is a platform for research of interest to a forward-thinking vascular specialist.
Dr. Richard Hughson, from the University of Waterloo in Waterloo, Ontario, is researching vascular aging in spaceflight crew members. His work is a part of the Schlegel-University of Waterloo Research Institute for Aging, where he is theme leader/chair of vascular aging and brain health and holds the Schlegel Research Chair in that discipline.
Dr. Hughson is supported by the Canadian Space Agency (CSA) and Canadian Institute for Health Research (CIHR) He discussed his research in a recent audio interview (http://cihr-irsc.gc.ca/e/49523.html).
Observations have demonstrated that short-duration and extended spaceflight missions may simulate accelerated vascular aging in some of these highly fit individuals traveling to space. Specifically, spaceflight crew members have been shown to have difficulty controlling a rise in their blood pressure, perhaps secondary to the loss of Earth’s gravity, but rather in the inherent cephalad fluid shift (as blood no longer pools in the legs). In addition, significant postflight postural hypotension and physical deconditioning with resultant sarcopenia and osteopenia are known to occur.
Dr. Hughson has shown through ultrasonography that the carotid arteries of spaceflight crew members are considerably stiffer compared to their preflight arteries and that they appear to have “aged the equivalent of 20-30 years in stiffness.” The ramifications of this type of research on the study of the normal earthbound vascular aging processes are under investigation.
To counteract the effects of vascular aging and physical deconditioning in space, physical activity is key; however, the 30 minutes per day allotted to busy astronauts amid their responsibilities is just not cutting it, according to Dr. Hughson. Missions are being extended for longer periods of time, leading to serious physical consequences, For example, American astronaut Scott Kelly’s year in space will certainly result in considerable accelerated aging in his arterial system. Thus, it becomes increasingly necessary to understand and prevent the vascular aging process in astronauts, future spaceflight crew members, and perhaps one day those seeking to colonize the Moon, Mars, and beyond.
When colonization time arrives, space agencies certainly should be in the market for well-qualified vascular specialists.
Perhaps great job opportunities await those in our profession who will be brave enough to leave Earth’s cradle.
Dr Drudi is a vascular surgery resident at McGill University, Montreal.
Residents’ Forum: Searching for a Thoracic Job in 2016
In the thick of a job search for this coming July, I fondly remember my first experience at the 47th Annual STS meeting in San Diego in 2011. The presidential address was delivered by Dr. Mathisen and focused nearly an entire hour on encouraging and mentoring young trainees to pursue a career in cardiothoracic surgery. Citing concerns about job availability and security, declining compensation, and increasing scrutiny on outcome measures, the president attempted to individually address these.
Most vividly I remember the emphasis on baby boomers getting older, median CT surgeon age approaching the retirement point, and the overall increased need for young, motivated, and highly skilled junior attendings. Until this year, the number of STS and CTSnet job posts was abysmally low. This led many new graduates to consider advanced fellowships or alternative avenues. Half a decade after Dr. Mathisen’s prediction at STS, the proverbial flood gates have opened.
This past year, I’ve seen at least a dozen quality academic positions looking for new graduates in thoracic surgery. Additionally, at least another dozen hybrid practice or private/community practice groups are looking to hire junior attendings. What is also interesting is the direction that many practices are headed: thoracic service lines, where volume is accrued from surrounding community practices and brought to centralized, multidisciplinary tertiary care institutions.
In many models, mentorship has been built in with involved senior partners, especially now that expertise in advanced techniques in bronchoscopy (EBUS, navigational bronchoscopy), endoscopy (RFA, EMR, and other ablative strategies) and minimally invasive surgery (VATS, MIS esophagectomy, robotic) are commonly expected by patients. These skills are initially learned in training and, with the right support structure, are perfected early in practice.
With more precise earlier stage screening and detection of esophageal and lung malignancies and the general stability or increase in the year-to-year incidence of these cancers, I expect the job market will continue to accommodate a growing need for thoracic surgeons in the United States. This should greatly help recruitment of the best young medical talent into what is truly an exciting and blossoming field of surgery.
Reference
Mathisen DJ. “It’s Not the Destination, It’s the Journey: Lessons Learned”. 47th Annual STS Presidential Address. San Diego, CA. January 2011. www.sts.org/news/mathisen-delivers-presidential-address.
Dr. Shersher is at Rush University Medical Center, Chicago.
In the thick of a job search for this coming July, I fondly remember my first experience at the 47th Annual STS meeting in San Diego in 2011. The presidential address was delivered by Dr. Mathisen and focused nearly an entire hour on encouraging and mentoring young trainees to pursue a career in cardiothoracic surgery. Citing concerns about job availability and security, declining compensation, and increasing scrutiny on outcome measures, the president attempted to individually address these.
Most vividly I remember the emphasis on baby boomers getting older, median CT surgeon age approaching the retirement point, and the overall increased need for young, motivated, and highly skilled junior attendings. Until this year, the number of STS and CTSnet job posts was abysmally low. This led many new graduates to consider advanced fellowships or alternative avenues. Half a decade after Dr. Mathisen’s prediction at STS, the proverbial flood gates have opened.
This past year, I’ve seen at least a dozen quality academic positions looking for new graduates in thoracic surgery. Additionally, at least another dozen hybrid practice or private/community practice groups are looking to hire junior attendings. What is also interesting is the direction that many practices are headed: thoracic service lines, where volume is accrued from surrounding community practices and brought to centralized, multidisciplinary tertiary care institutions.
In many models, mentorship has been built in with involved senior partners, especially now that expertise in advanced techniques in bronchoscopy (EBUS, navigational bronchoscopy), endoscopy (RFA, EMR, and other ablative strategies) and minimally invasive surgery (VATS, MIS esophagectomy, robotic) are commonly expected by patients. These skills are initially learned in training and, with the right support structure, are perfected early in practice.
With more precise earlier stage screening and detection of esophageal and lung malignancies and the general stability or increase in the year-to-year incidence of these cancers, I expect the job market will continue to accommodate a growing need for thoracic surgeons in the United States. This should greatly help recruitment of the best young medical talent into what is truly an exciting and blossoming field of surgery.
Reference
Mathisen DJ. “It’s Not the Destination, It’s the Journey: Lessons Learned”. 47th Annual STS Presidential Address. San Diego, CA. January 2011. www.sts.org/news/mathisen-delivers-presidential-address.
Dr. Shersher is at Rush University Medical Center, Chicago.
In the thick of a job search for this coming July, I fondly remember my first experience at the 47th Annual STS meeting in San Diego in 2011. The presidential address was delivered by Dr. Mathisen and focused nearly an entire hour on encouraging and mentoring young trainees to pursue a career in cardiothoracic surgery. Citing concerns about job availability and security, declining compensation, and increasing scrutiny on outcome measures, the president attempted to individually address these.
Most vividly I remember the emphasis on baby boomers getting older, median CT surgeon age approaching the retirement point, and the overall increased need for young, motivated, and highly skilled junior attendings. Until this year, the number of STS and CTSnet job posts was abysmally low. This led many new graduates to consider advanced fellowships or alternative avenues. Half a decade after Dr. Mathisen’s prediction at STS, the proverbial flood gates have opened.
This past year, I’ve seen at least a dozen quality academic positions looking for new graduates in thoracic surgery. Additionally, at least another dozen hybrid practice or private/community practice groups are looking to hire junior attendings. What is also interesting is the direction that many practices are headed: thoracic service lines, where volume is accrued from surrounding community practices and brought to centralized, multidisciplinary tertiary care institutions.
In many models, mentorship has been built in with involved senior partners, especially now that expertise in advanced techniques in bronchoscopy (EBUS, navigational bronchoscopy), endoscopy (RFA, EMR, and other ablative strategies) and minimally invasive surgery (VATS, MIS esophagectomy, robotic) are commonly expected by patients. These skills are initially learned in training and, with the right support structure, are perfected early in practice.
With more precise earlier stage screening and detection of esophageal and lung malignancies and the general stability or increase in the year-to-year incidence of these cancers, I expect the job market will continue to accommodate a growing need for thoracic surgeons in the United States. This should greatly help recruitment of the best young medical talent into what is truly an exciting and blossoming field of surgery.
Reference
Mathisen DJ. “It’s Not the Destination, It’s the Journey: Lessons Learned”. 47th Annual STS Presidential Address. San Diego, CA. January 2011. www.sts.org/news/mathisen-delivers-presidential-address.
Dr. Shersher is at Rush University Medical Center, Chicago.