User login
The diagnosis: Metastatic insulinoma surrounded by steatotic hepatocytes
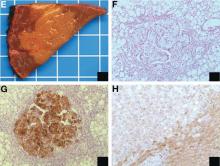
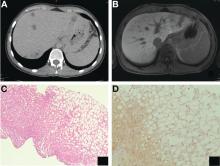
The loss of L-FABP expression in steatotic hepatocytes is the hallmark of HNF1alpha-inactivated liver adenoma,1 and clearly suggested this diagnosis. However, the emergence of multiple steatotic lesions over a short period of time was uncommon for liver adenomas. Despite the absence of radiologically detectable metastasis, this diagnosis could not be ruled out, and the patient underwent a surgical liver biopsy (tip of the right lobe). The specimen showed a 0.2 cm greyish nodule surrounded by a steatotic map-like area of 3.5 cm in the largest dimension (Figure E). Histopathologic examination showed neuroendocrine cells (Figures F [hematoxylin and eosin staining] and G [insulin immunostaining]), confirming the diagnosis of metastatic insulinoma surrounded by steatotic hepatocytes.
The key interest of the case is the reduction of L-FABP expression in the steatotic hepatocytes (Figure H [L-FABP immunostaining]), which was an unexpected finding and could have led to an incorrect diagnosis of HNF1α-inactivated liver adenoma.
In contrast with other functional neuroendocrine tumors, insulinomas are frequently benign tumors, and only about 10% of patients develop metastasis. In the liver, they are often surrounded by microscopic or radiologically detectable steatotic areas thanks to the paracrine effect of insulin. Such a feature has been previously described both with liver insulinoma metastases2 and after pancreatic islet transplantation.3 The reduction of L-FABP expression within the steatotic hepatocytes seems to be less frequent because it was not observed in an additional patient with G3 insulinoma (neuroendocrine carcinoma) metastases and in 3 pancreatic islet recipients (data not shown).
The present patient with multiple liver G2 insulinoma metastases illustrates 1) the potential of foci of steatosis to represent early signs of insulinoma liver metastasis, and 2) the presence of a reduction or even a loss of L-FABP expression in other liver lesions than HNF1alpha-inactivated liver adenoma.
Acknowledgment
Claudio De Vito’s current affiliation is Institute of Liver Studies, King’s College Hospital, London, UK.
The authors thank A.M.J. Shapiro from the University of Alberta, Edmonton, Canada and A. Quaglia from the King’s College Hospital, London, UK for sharing the liver samples of transplanted pancreatic islets and G3 insulinoma metastasis. They are also grateful to the members of the Geneva Hepato-Biliary and Pancreatic Center for the discussion of the case.
References
1. Bioulac-Sage P., Cubel G., Taouji S., et al. Immunohistochemical markers on needle biopsies are helpful for the diagnosis of focal nodular hyperplasia and hepatocellular adenoma subtypes. Am J Surg Pathol. 2012;36:1691-9.
2. Sohn J., Siegelman E., Osiason, A. Unusual patterns of hepatic steatosis caused by the local effect of insulin revealed on chemical shift MR imaging. AJR Am J Roentgenol. 2001;176:471-4.
3. Toso C., Isse K., Demetris A.J., et al. Histologic graft assessment after clinical islet transplantation. Transplantation. 2009;88:1286-93.
The diagnosis: Metastatic insulinoma surrounded by steatotic hepatocytes
The loss of L-FABP expression in steatotic hepatocytes is the hallmark of HNF1alpha-inactivated liver adenoma,1 and clearly suggested this diagnosis. However, the emergence of multiple steatotic lesions over a short period of time was uncommon for liver adenomas. Despite the absence of radiologically detectable metastasis, this diagnosis could not be ruled out, and the patient underwent a surgical liver biopsy (tip of the right lobe). The specimen showed a 0.2 cm greyish nodule surrounded by a steatotic map-like area of 3.5 cm in the largest dimension (Figure E). Histopathologic examination showed neuroendocrine cells (Figures F [hematoxylin and eosin staining] and G [insulin immunostaining]), confirming the diagnosis of metastatic insulinoma surrounded by steatotic hepatocytes.
The key interest of the case is the reduction of L-FABP expression in the steatotic hepatocytes (Figure H [L-FABP immunostaining]), which was an unexpected finding and could have led to an incorrect diagnosis of HNF1α-inactivated liver adenoma.
In contrast with other functional neuroendocrine tumors, insulinomas are frequently benign tumors, and only about 10% of patients develop metastasis. In the liver, they are often surrounded by microscopic or radiologically detectable steatotic areas thanks to the paracrine effect of insulin. Such a feature has been previously described both with liver insulinoma metastases2 and after pancreatic islet transplantation.3 The reduction of L-FABP expression within the steatotic hepatocytes seems to be less frequent because it was not observed in an additional patient with G3 insulinoma (neuroendocrine carcinoma) metastases and in 3 pancreatic islet recipients (data not shown).
The present patient with multiple liver G2 insulinoma metastases illustrates 1) the potential of foci of steatosis to represent early signs of insulinoma liver metastasis, and 2) the presence of a reduction or even a loss of L-FABP expression in other liver lesions than HNF1alpha-inactivated liver adenoma.
Acknowledgment
Claudio De Vito’s current affiliation is Institute of Liver Studies, King’s College Hospital, London, UK.
The authors thank A.M.J. Shapiro from the University of Alberta, Edmonton, Canada and A. Quaglia from the King’s College Hospital, London, UK for sharing the liver samples of transplanted pancreatic islets and G3 insulinoma metastasis. They are also grateful to the members of the Geneva Hepato-Biliary and Pancreatic Center for the discussion of the case.
References
1. Bioulac-Sage P., Cubel G., Taouji S., et al. Immunohistochemical markers on needle biopsies are helpful for the diagnosis of focal nodular hyperplasia and hepatocellular adenoma subtypes. Am J Surg Pathol. 2012;36:1691-9.
2. Sohn J., Siegelman E., Osiason, A. Unusual patterns of hepatic steatosis caused by the local effect of insulin revealed on chemical shift MR imaging. AJR Am J Roentgenol. 2001;176:471-4.
3. Toso C., Isse K., Demetris A.J., et al. Histologic graft assessment after clinical islet transplantation. Transplantation. 2009;88:1286-93.
The diagnosis: Metastatic insulinoma surrounded by steatotic hepatocytes
The loss of L-FABP expression in steatotic hepatocytes is the hallmark of HNF1alpha-inactivated liver adenoma,1 and clearly suggested this diagnosis. However, the emergence of multiple steatotic lesions over a short period of time was uncommon for liver adenomas. Despite the absence of radiologically detectable metastasis, this diagnosis could not be ruled out, and the patient underwent a surgical liver biopsy (tip of the right lobe). The specimen showed a 0.2 cm greyish nodule surrounded by a steatotic map-like area of 3.5 cm in the largest dimension (Figure E). Histopathologic examination showed neuroendocrine cells (Figures F [hematoxylin and eosin staining] and G [insulin immunostaining]), confirming the diagnosis of metastatic insulinoma surrounded by steatotic hepatocytes.
The key interest of the case is the reduction of L-FABP expression in the steatotic hepatocytes (Figure H [L-FABP immunostaining]), which was an unexpected finding and could have led to an incorrect diagnosis of HNF1α-inactivated liver adenoma.
In contrast with other functional neuroendocrine tumors, insulinomas are frequently benign tumors, and only about 10% of patients develop metastasis. In the liver, they are often surrounded by microscopic or radiologically detectable steatotic areas thanks to the paracrine effect of insulin. Such a feature has been previously described both with liver insulinoma metastases2 and after pancreatic islet transplantation.3 The reduction of L-FABP expression within the steatotic hepatocytes seems to be less frequent because it was not observed in an additional patient with G3 insulinoma (neuroendocrine carcinoma) metastases and in 3 pancreatic islet recipients (data not shown).
The present patient with multiple liver G2 insulinoma metastases illustrates 1) the potential of foci of steatosis to represent early signs of insulinoma liver metastasis, and 2) the presence of a reduction or even a loss of L-FABP expression in other liver lesions than HNF1alpha-inactivated liver adenoma.
Acknowledgment
Claudio De Vito’s current affiliation is Institute of Liver Studies, King’s College Hospital, London, UK.
The authors thank A.M.J. Shapiro from the University of Alberta, Edmonton, Canada and A. Quaglia from the King’s College Hospital, London, UK for sharing the liver samples of transplanted pancreatic islets and G3 insulinoma metastasis. They are also grateful to the members of the Geneva Hepato-Biliary and Pancreatic Center for the discussion of the case.
References
1. Bioulac-Sage P., Cubel G., Taouji S., et al. Immunohistochemical markers on needle biopsies are helpful for the diagnosis of focal nodular hyperplasia and hepatocellular adenoma subtypes. Am J Surg Pathol. 2012;36:1691-9.
2. Sohn J., Siegelman E., Osiason, A. Unusual patterns of hepatic steatosis caused by the local effect of insulin revealed on chemical shift MR imaging. AJR Am J Roentgenol. 2001;176:471-4.
3. Toso C., Isse K., Demetris A.J., et al. Histologic graft assessment after clinical islet transplantation. Transplantation. 2009;88:1286-93.
By Claudio De Vito, MD, PhD, Laura Rubbia-Brandt, MD, PhD, and Christian Toso, MD, PhD. Published previously in Gastroenterology (2016;151[1]32, 330).
A 22-year-old woman with no past medical history was investigated for hypoglycemia episodes. A nodule located in the head of the pancreas was identified, with radiologic features of a neuroendocrine neoplasm. The overall clinical presentation was consistent with an insulinoma. No distant lesion was detected. She underwent a Whipple procedure, and the histopathologic examination reported a 2.2-cm, well-differentiated neuroendocrine tumor (insulinoma) G2 (4% Ki-67 index), with no lymphovascular invasion or lymph node metastasis (0 of 30 lymph nodes).