User login
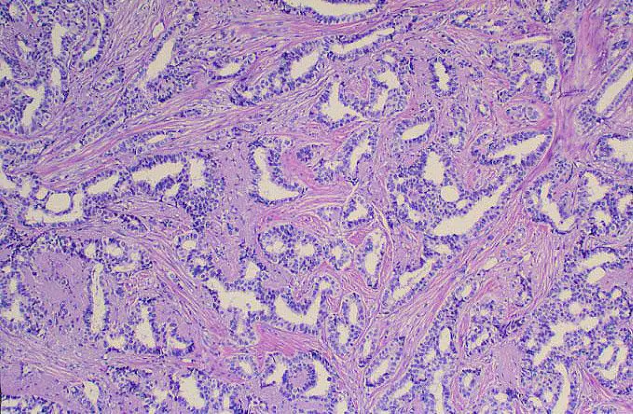
The history and findings in this case are consistent with advanced infiltrating ductal carcinoma.
Breast cancer is the most commonly diagnosed life-threatening cancer and the leading cause of cancer death among women worldwide. In the United States, it is estimated that 287,850 new cases of invasive breast cancer were diagnosed in 2022; in addition, 43,250 deaths because of breast cancer are expected to occur.
Infiltrating ductal carcinoma is the most common type of breast tumor. It accounts for 75% of breast cancers and has a propensity to metastasize via lymphatic vessels. This lesion has no specific histologic characteristics apart from invasion through the basement membrane. This enables it to be differentiated from ductal carcinoma in situ, which remains inside the duct.
All newly diagnosed cases of invasive breast cancers are tested for estrogen receptors, progesterone receptors, and HER2 status. The presence of estrogen and progesterone receptors is tested by immunohistochemistry, whereas HER2 can be tested by either immunohistochemistry or in situ hybridization (usually fluorescent or fluorescence in situ hybridization). Testing results have important treatment implications and prognostic significance.
Surgical treatment of invasive breast cancer consists of either lumpectomy or total mastectomy, followed by radiation therapy. Surgical resection is performed in all patients with nonmetastatic disease.
Systemic therapy options include endocrine therapy, cytotoxic chemotherapy, targeted therapy, and immunotherapy. The choice of systemic therapy is largely determined by subtype. For example, patients with hormone receptor–positive tumors receive endocrine therapy; a minority of these patients may receive chemotherapy as well. Patients with HER2-positive tumors receive HER2–targeted antibody or small-molecule inhibitor therapy combined with chemotherapy. For patients with triple-negative tumors, chemotherapy alone is often used; newer targeted therapies however may improve outcomes. In both the adjuvant and neoadjuvant setting, the primary goal of treatment is to eradicate or control undiscovered distant metastases. In the metastatic setting, the primary goal of treatment is to extend life and alleviate symptoms.
Depending on the individual patient, systemic therapy may be used in the adjuvant or neoadjuvant setting. Systemic therapy is chosen according to breast cancer subtype and recurrence risk, with the treatment for low-risk patients being de-escalated, whereas high-risk patients receive aggressive systemic treatment. When systemic therapy is used in the neoadjuvant setting, treatment response is the most important factor for predicting outcomes and selecting the optimal adjuvant therapy. Novel biological markers enable the selection of appropriate targeted therapy, which can achieve optimal efficacy.
Up-to-date, evidence-based recommendations for pre- and postoperative treatment of breast cancer, including advanced breast cancer, are provided by the National Comprehensive Cancer Network.
Karl J. D'Silva, MD, Clinical Assistant Professor, Department of Medicine, Tufts University School of Medicine, Boston; Medical Director, Department of Oncology and Hematology, Lahey Hospital and Medical Center, Peabody, Massachusetts.
Karl J. D'Silva, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
The history and findings in this case are consistent with advanced infiltrating ductal carcinoma.
Breast cancer is the most commonly diagnosed life-threatening cancer and the leading cause of cancer death among women worldwide. In the United States, it is estimated that 287,850 new cases of invasive breast cancer were diagnosed in 2022; in addition, 43,250 deaths because of breast cancer are expected to occur.
Infiltrating ductal carcinoma is the most common type of breast tumor. It accounts for 75% of breast cancers and has a propensity to metastasize via lymphatic vessels. This lesion has no specific histologic characteristics apart from invasion through the basement membrane. This enables it to be differentiated from ductal carcinoma in situ, which remains inside the duct.
All newly diagnosed cases of invasive breast cancers are tested for estrogen receptors, progesterone receptors, and HER2 status. The presence of estrogen and progesterone receptors is tested by immunohistochemistry, whereas HER2 can be tested by either immunohistochemistry or in situ hybridization (usually fluorescent or fluorescence in situ hybridization). Testing results have important treatment implications and prognostic significance.
Surgical treatment of invasive breast cancer consists of either lumpectomy or total mastectomy, followed by radiation therapy. Surgical resection is performed in all patients with nonmetastatic disease.
Systemic therapy options include endocrine therapy, cytotoxic chemotherapy, targeted therapy, and immunotherapy. The choice of systemic therapy is largely determined by subtype. For example, patients with hormone receptor–positive tumors receive endocrine therapy; a minority of these patients may receive chemotherapy as well. Patients with HER2-positive tumors receive HER2–targeted antibody or small-molecule inhibitor therapy combined with chemotherapy. For patients with triple-negative tumors, chemotherapy alone is often used; newer targeted therapies however may improve outcomes. In both the adjuvant and neoadjuvant setting, the primary goal of treatment is to eradicate or control undiscovered distant metastases. In the metastatic setting, the primary goal of treatment is to extend life and alleviate symptoms.
Depending on the individual patient, systemic therapy may be used in the adjuvant or neoadjuvant setting. Systemic therapy is chosen according to breast cancer subtype and recurrence risk, with the treatment for low-risk patients being de-escalated, whereas high-risk patients receive aggressive systemic treatment. When systemic therapy is used in the neoadjuvant setting, treatment response is the most important factor for predicting outcomes and selecting the optimal adjuvant therapy. Novel biological markers enable the selection of appropriate targeted therapy, which can achieve optimal efficacy.
Up-to-date, evidence-based recommendations for pre- and postoperative treatment of breast cancer, including advanced breast cancer, are provided by the National Comprehensive Cancer Network.
Karl J. D'Silva, MD, Clinical Assistant Professor, Department of Medicine, Tufts University School of Medicine, Boston; Medical Director, Department of Oncology and Hematology, Lahey Hospital and Medical Center, Peabody, Massachusetts.
Karl J. D'Silva, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
The history and findings in this case are consistent with advanced infiltrating ductal carcinoma.
Breast cancer is the most commonly diagnosed life-threatening cancer and the leading cause of cancer death among women worldwide. In the United States, it is estimated that 287,850 new cases of invasive breast cancer were diagnosed in 2022; in addition, 43,250 deaths because of breast cancer are expected to occur.
Infiltrating ductal carcinoma is the most common type of breast tumor. It accounts for 75% of breast cancers and has a propensity to metastasize via lymphatic vessels. This lesion has no specific histologic characteristics apart from invasion through the basement membrane. This enables it to be differentiated from ductal carcinoma in situ, which remains inside the duct.
All newly diagnosed cases of invasive breast cancers are tested for estrogen receptors, progesterone receptors, and HER2 status. The presence of estrogen and progesterone receptors is tested by immunohistochemistry, whereas HER2 can be tested by either immunohistochemistry or in situ hybridization (usually fluorescent or fluorescence in situ hybridization). Testing results have important treatment implications and prognostic significance.
Surgical treatment of invasive breast cancer consists of either lumpectomy or total mastectomy, followed by radiation therapy. Surgical resection is performed in all patients with nonmetastatic disease.
Systemic therapy options include endocrine therapy, cytotoxic chemotherapy, targeted therapy, and immunotherapy. The choice of systemic therapy is largely determined by subtype. For example, patients with hormone receptor–positive tumors receive endocrine therapy; a minority of these patients may receive chemotherapy as well. Patients with HER2-positive tumors receive HER2–targeted antibody or small-molecule inhibitor therapy combined with chemotherapy. For patients with triple-negative tumors, chemotherapy alone is often used; newer targeted therapies however may improve outcomes. In both the adjuvant and neoadjuvant setting, the primary goal of treatment is to eradicate or control undiscovered distant metastases. In the metastatic setting, the primary goal of treatment is to extend life and alleviate symptoms.
Depending on the individual patient, systemic therapy may be used in the adjuvant or neoadjuvant setting. Systemic therapy is chosen according to breast cancer subtype and recurrence risk, with the treatment for low-risk patients being de-escalated, whereas high-risk patients receive aggressive systemic treatment. When systemic therapy is used in the neoadjuvant setting, treatment response is the most important factor for predicting outcomes and selecting the optimal adjuvant therapy. Novel biological markers enable the selection of appropriate targeted therapy, which can achieve optimal efficacy.
Up-to-date, evidence-based recommendations for pre- and postoperative treatment of breast cancer, including advanced breast cancer, are provided by the National Comprehensive Cancer Network.
Karl J. D'Silva, MD, Clinical Assistant Professor, Department of Medicine, Tufts University School of Medicine, Boston; Medical Director, Department of Oncology and Hematology, Lahey Hospital and Medical Center, Peabody, Massachusetts.
Karl J. D'Silva, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
A 40-year-old woman presents with a left breast mass that she discovered while showering. The patient has no significant medical history and does not take any medications. She has not yet undergone any routine mammography screening. Clinical breast examination reveals a large palpable immobile mass in the inner quadrant of the left breast. The nipple is retracted. Left axial lymphadenopathy is also detected. There are no palpable abnormalities in the right breast. The remainder of the physical examination is unremarkable. Laboratory findings are all within normal range, apart from C-reactive protein, which is elevated (8 mg/L). The patient is 5 ft 4 in and weighs 142 lb.
The patient is sent for a mammogram and needle biopsy of the mass and axial lymph nodes. Mammogram findings include an irregular mass 4.2 cm in size in the left breast with heterogeneous echotexture, abrupt interface, and intramass calcifications as well as overlying skin thickening. The mass is predominately in the inner left breast and is extending into the outside quadrant. Multiple morphologically abnormal lymph nodes are noted in the left axilla. Biopsy results include atypical glands infiltrating the surrounding stroma in an irregular pattern. Immunohistochemistry results show p53 expression.