User login
A woman in her 50s underwent hysterectomy performed by a surgeon, who then assigned an ObGyn to her follow-up care. The day after surgery, the patient had severe abdominal pain with decreased blood pressure and increased heart and respiration rates. The ObGyn admitted the patient to the intensive care unit (ICU), and then designated Dr. A, the patient’s family practitioner to continue her care. Dr. A was not available, so his associate, Dr. B, took over. Over the phone, Dr. B requested pulmonary, cardiology, and infectious disease consults. In the ICU the next day, the patient suffered respiratory arrest and was intubated. When her abdomen became rigid and swollen, emergency surgery revealed that a colon perforation had allowed fecal matter to reach the abdominal cavity. The woman died the next day from complications of sepsis, peritonitis, and multiple organ failure.
ESTATE’S CLAIM None of the physicians assigned to her care ever saw the patient in the ICU. Earlier surgery could have prevented her death. The physicians involved in her care failed to communicate with each other properly.
DEFENDANTS’ DEFENSE The case was settled during the trial.
VERDICT A $3.2 million Illinois settlement was reached with the hospital.
BOTH PARENTS HAD PLATELET ANTIBODIES
When a 32-year-old woman became pregnant with her third child, she sought treatment at a clinic. The mother informed the nurse practi-tioner that her two other children had been diagnosed with low platelets at birth, but they were now healthy and had no further problems.
The woman gave birth vaginally to her third child at term. The newborn had Apgar scores of 8 and 8, at 1 and 5 minutes, respectively. However, the child’s platelet level was 26 x 103/µL. The baby was transferred to another hospital the next day, where he was diagnosed with hydrocephalus and neonatal alloimmune thrombocytopenia. He suffered a massive intracranial hemorrhage, which caused severe neurologic injuries and brain damage. A shunt was placed. The child has significant cognitive deficits as well as cerebral palsy with mild developmental delays. Testing showed that each parent had a different genotype for platelet antibodies.
PARENTS’ CLAIM The parents should have been tested for platelet antibodies prior to this birth due to the family’s history. A prenatal diagnosis of neonatal alloimmune thrombocytopenia would have allowed for treatment with gamma globulin, which could have avoided the intracranial hemorrhage.
DEFENDANTS’ DEFENSE The case was settled during the trial.
VERDICT A $4.8 million California settlement was reached.
CORD PROLAPSE NOT CARED FOR IN AMBULANCE
At 36 weeks’ gestation, a mother called an ambulance when her membranes ruptured and she noticed an umbilical cord prolapse.
The child was in a breech presentation, experienced oxygen deprivation, and sustained severe neurologic damage.
PARENTS’ CLAIM The ambulance service was negligent in its care. The ambulance service dispatcher advised the mother to stand, squat, and push before the ambulance arrived. The ambulance attendants failed to take basic actions to relieve pressure on the prolapsed umbilical cord. The ambulance did not stop at two closer hospitals, which delayed arrival for an additional 20 minutes.
DEFENDANTS’ DEFENSE The case was settled during the trial.
VERDICT A $2.7 million settlement was reached, but before it was submitted to the court for approval, the child died. The defendants then sought to revoke the settlement, but the parents claimed breach of contract. The defendants claimed that the agreement was orally negotiated independent of defense counsel and was unenforceable due to the child’s death and lack of court approval. A Texas judge issued summary judgment on breach of contract and awarded $2.7 million plus $40,000 in attorney fees to the parents.
SECOND- AND THIRD-DEGREE BURNS TO PERINEUM
A mother received an epidural injection during vaginal delivery. Six hours later, the patient asked a nurse for a warm compress to place on her perineum. The nurse heated the compress in a microwave and then applied it to the perineal area. The compress caused second- and third-degree burns to the patient’s labia and inner left thigh. She underwent surgical repair of the burned area, and, a year later, had plastic surgery.
PATIENT’S CLAIM The nurse was negligent in overheating the compress.
DEFENDANTS’ DEFENSE The hospital agreed that the nurse who heated and applied the compress had been negligent. The hospital paid all medical expenses relating to the burns, including follow-up surgeries.
VERDICT A $190,000 Utah verdict was returned for noneconomic damages.
DOCUMENTATION MAKES A DIFFERENCE FOR OBGYN AFTER CHILD DIES
A 30-year-old physician was pregnant with her first child. Due to a low amniotic fluid index and lagging fetal growth, she saw a maternal-fetal medicine specialist, who suggested labor induction at 39 weeks.
Labor progressed slowly. After three attempts at vacuum-assisted delivery, the ObGyn recommended cesarean delivery. The parents eventually consented to cesarean delivery after another failed vacuum-assisted attempt. Although the ObGyn had recommended cesarean 2 hours earlier, surgery was not ordered on an emergent basis.
At birth, the baby’s resuscitation took more than 20 minutes. The child lost nearly one-third of her blood volume; she had a subgaleal hemorrhage. Both parties agreed that the vacuum device probably caused the bleeding.
The child had hypoxic ischemic encephalopathy and disseminated intravascular coagulation. She suffered a myocardial infarction at 3 days of age. Without electrical brain activity, life support was removed, and the child died at 5 days of age. An autopsy found possible hypereosinophilic syndrome as the concurrent cause of death.
PARENTS’ CLAIM The mother claimed she was not informed of the risks, benefits, and alternatives to vacuum extraction; she would not have consented had she known the risks. The mother, her husband, and two family members maintained that the ObGyn offered the possibility of cesarean delivery as a question, but did not insist on it. The mother claimed she wanted what was best for the baby, and never refused a cesarean. The resuscitation efforts caused eosinophilic infiltration into several organs.
PHYSICIAN’S DEFENSE The ObGyn charted that the parents were “adamant about having a vaginal delivery,” and said she told the parents what she charted. The obstetric nurse testified that the mother delayed consent because she felt vaginal delivery was imminent. The ObGyn acted properly; eosinophilia caused the baby’s death.
VERDICT An Illinois defense verdict was returned.
HIGH BP TO BLAME FOR DEATHS OF BOTH MOTHER AND CHILD
A 23-year-old woman’s pregnancy was at high risk because of very high blood pressure (BP). At 34 weeks’ gestation, she went to a county hospital with symptoms of high BP; she was treated and discharged 3 days later. She returned to the hospital to be checked twice more within a month. The day after the third visit, she suffered a seizure and was taken to a university hospital, where emergency cesarean delivery was performed. The mother died from an aortic rupture during delivery.
The child was born with brain injuries and died at age 4 years due to neurologic complications.
ESTATE’S CLAIM The mother was not properly treated at the county hospital, resulting in both deaths; she should not have been discharged. Under monitoring, she would have undergone delivery before the aortic rupture occurred, avoiding the baby’s brain injury.
DEFENDANTS’ DEFENSE The mother was stable when released; aortic rupture is unpredictable and unpreventable, and would have occurred under any circumstances. It is highly unusual that a woman of her age would have an aortic rupture.
VERDICT A $3,062,803 California verdict was returned. The parties then settled for $1,782,000 (with the county assuming the medical lien).
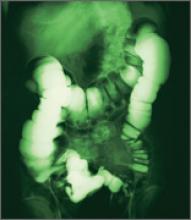
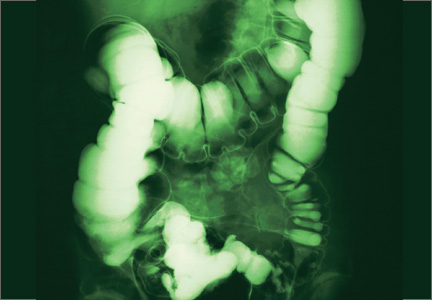
NECROTIZING FASCIITIS FROM PERFORATED COLON
A woman underwent laparoscopic-assisted vaginal hysterectomy performed by her ObGyn, and was discharged after 3 days. The next day, she went to another hospital’s emergency department (ED) with abdominal distention and rigidity, severe abdominal pain, and vomiting. She had a toxic appearance, rapid pulse rate, and hypotension. In emergency surgery, several liters of dark brown, foul-smelling fluid were found in her abdomen, and feculent peritonitis and necrotizing fasciitis were diagnosed due to a perforated sigmoid colon. She required multiple hospitalizations and operations.
PATIENT’S CLAIM Perforation occurred during hysterectomy. The ObGyn failed to recognize the injury prior to discharge. The hospital staff did not properly assess her or communicate her symptoms to the ObGyn.
DEFENDANTS’ DEFENSE There was no negligence; proper care was given.
VERDICT A $2,922,503 Florida verdict was returned, with the jury finding the ObGyn 30% at fault and the hospital 70% at fault.
FAILURE TO REACT TO FETAL DISTRESS: $15.6M
After delivery at full term, a child suffered convulsions and seizures on her second day of life. A CT scan showed brain injuries. At age 11 years, she has severe learning and developmental delays, and requires 24-hour care.
PARENTS’ CLAIM Severe decelerations with slow return to baseline occurred several times during labor and delivery. The nurse midwife failed to recognize and react to fetal distress. A cesarean delivery should have been performed instead of a vaginal delivery. The delay in delivery caused the child’s injuries.
DEFENDANTS’ DEFENSE A prenatal neurogenetic disorder caused the child’s injuries.
VERDICT A $15.6 million Maryland verdict was returned. It will not be automatically reduced; the awarded noneconomic damages do not exceed the state cap.
LATE DELIVERY; SEVERE INJURY TO CHILD
At 40 weeks’ gestation, a woman was admitted to the hospital in labor. When the mother’s membranes were ruptured, a small amount of meconium was noted, but the fetal monitor strips were reassuring. Two hours later, the nurse and midwife noted a pattern of decelerations, but they felt the pattern was nonrepetitive and reactive. Thirty minutes later, the nurse and midwife noted decelerations to 90 bpm with pushing, but did not call a physician.
Another midwife arrived to assist the first midwife who was new to practice. The mother was given oxygen, her position was changed, and an IV fluid bolus was administered. Thirty minutes later, the nurses recognized late decelerations and called a Code White twice while the fetal heart rate continued to decelerate. After the attending physician unsuccessfully attempted vacuum extraction, an emergency cesarean delivery was performed.
The child’s Apgar scores were 2, 3, and 3, at 1, 5, and 10 minutes, respectively. The cord blood pH was 6.66, indicating severe metabolic acidosis. She developed seizures within the first few minutes of life. Imaging studies showed global hypoxic ischemic encephalopathy. The child cannot walk, talk, or sit up unsupported at age 8, and requires a G-tube. She is cortically blind and requires antiseizure medication.
PARENTS’ CLAIM The nurse, two midwives, and physician were negligent in their care of the mother and child.
DEFENDANTS’ DEFENSE The case was settled during the trial.
VERDICT A $5 million Massachusetts settlement was reached.
WHAT CAUSED INFECTION AFTER ABORTION?
A 20-year-old woman underwent a surgical termination of pregnancy performed by an ObGyn. After discharge, the patient developed pain and other complications requiring rehospitalization and additional surgery for a pelvic infection.
PATIENT’S CLAIM Complications were due to a uterine perforation that spontaneously sealed before it could be detected. The ObGyn was negligent in the performance of the elective abortion. The patient has a large scar on her abdomen because of the additional operation.
PHYSICIAN’S DEFENSE Perforation of the uterus is a known complication of the procedure. However, no perforation occurred; it was not found on imaging, and spontaneous sealing of a perforation cannot occur. The patient’s complications were due to a subclinical infection that was activated by the surgery.
VERDICT A New York defense verdict was returned.
We want to hear from you. Tell us what you think!
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
A woman in her 50s underwent hysterectomy performed by a surgeon, who then assigned an ObGyn to her follow-up care. The day after surgery, the patient had severe abdominal pain with decreased blood pressure and increased heart and respiration rates. The ObGyn admitted the patient to the intensive care unit (ICU), and then designated Dr. A, the patient’s family practitioner to continue her care. Dr. A was not available, so his associate, Dr. B, took over. Over the phone, Dr. B requested pulmonary, cardiology, and infectious disease consults. In the ICU the next day, the patient suffered respiratory arrest and was intubated. When her abdomen became rigid and swollen, emergency surgery revealed that a colon perforation had allowed fecal matter to reach the abdominal cavity. The woman died the next day from complications of sepsis, peritonitis, and multiple organ failure.
ESTATE’S CLAIM None of the physicians assigned to her care ever saw the patient in the ICU. Earlier surgery could have prevented her death. The physicians involved in her care failed to communicate with each other properly.
DEFENDANTS’ DEFENSE The case was settled during the trial.
VERDICT A $3.2 million Illinois settlement was reached with the hospital.
BOTH PARENTS HAD PLATELET ANTIBODIES
When a 32-year-old woman became pregnant with her third child, she sought treatment at a clinic. The mother informed the nurse practi-tioner that her two other children had been diagnosed with low platelets at birth, but they were now healthy and had no further problems.
The woman gave birth vaginally to her third child at term. The newborn had Apgar scores of 8 and 8, at 1 and 5 minutes, respectively. However, the child’s platelet level was 26 x 103/µL. The baby was transferred to another hospital the next day, where he was diagnosed with hydrocephalus and neonatal alloimmune thrombocytopenia. He suffered a massive intracranial hemorrhage, which caused severe neurologic injuries and brain damage. A shunt was placed. The child has significant cognitive deficits as well as cerebral palsy with mild developmental delays. Testing showed that each parent had a different genotype for platelet antibodies.
PARENTS’ CLAIM The parents should have been tested for platelet antibodies prior to this birth due to the family’s history. A prenatal diagnosis of neonatal alloimmune thrombocytopenia would have allowed for treatment with gamma globulin, which could have avoided the intracranial hemorrhage.
DEFENDANTS’ DEFENSE The case was settled during the trial.
VERDICT A $4.8 million California settlement was reached.
CORD PROLAPSE NOT CARED FOR IN AMBULANCE
At 36 weeks’ gestation, a mother called an ambulance when her membranes ruptured and she noticed an umbilical cord prolapse.
The child was in a breech presentation, experienced oxygen deprivation, and sustained severe neurologic damage.
PARENTS’ CLAIM The ambulance service was negligent in its care. The ambulance service dispatcher advised the mother to stand, squat, and push before the ambulance arrived. The ambulance attendants failed to take basic actions to relieve pressure on the prolapsed umbilical cord. The ambulance did not stop at two closer hospitals, which delayed arrival for an additional 20 minutes.
DEFENDANTS’ DEFENSE The case was settled during the trial.
VERDICT A $2.7 million settlement was reached, but before it was submitted to the court for approval, the child died. The defendants then sought to revoke the settlement, but the parents claimed breach of contract. The defendants claimed that the agreement was orally negotiated independent of defense counsel and was unenforceable due to the child’s death and lack of court approval. A Texas judge issued summary judgment on breach of contract and awarded $2.7 million plus $40,000 in attorney fees to the parents.
SECOND- AND THIRD-DEGREE BURNS TO PERINEUM
A mother received an epidural injection during vaginal delivery. Six hours later, the patient asked a nurse for a warm compress to place on her perineum. The nurse heated the compress in a microwave and then applied it to the perineal area. The compress caused second- and third-degree burns to the patient’s labia and inner left thigh. She underwent surgical repair of the burned area, and, a year later, had plastic surgery.
PATIENT’S CLAIM The nurse was negligent in overheating the compress.
DEFENDANTS’ DEFENSE The hospital agreed that the nurse who heated and applied the compress had been negligent. The hospital paid all medical expenses relating to the burns, including follow-up surgeries.
VERDICT A $190,000 Utah verdict was returned for noneconomic damages.
DOCUMENTATION MAKES A DIFFERENCE FOR OBGYN AFTER CHILD DIES
A 30-year-old physician was pregnant with her first child. Due to a low amniotic fluid index and lagging fetal growth, she saw a maternal-fetal medicine specialist, who suggested labor induction at 39 weeks.
Labor progressed slowly. After three attempts at vacuum-assisted delivery, the ObGyn recommended cesarean delivery. The parents eventually consented to cesarean delivery after another failed vacuum-assisted attempt. Although the ObGyn had recommended cesarean 2 hours earlier, surgery was not ordered on an emergent basis.
At birth, the baby’s resuscitation took more than 20 minutes. The child lost nearly one-third of her blood volume; she had a subgaleal hemorrhage. Both parties agreed that the vacuum device probably caused the bleeding.
The child had hypoxic ischemic encephalopathy and disseminated intravascular coagulation. She suffered a myocardial infarction at 3 days of age. Without electrical brain activity, life support was removed, and the child died at 5 days of age. An autopsy found possible hypereosinophilic syndrome as the concurrent cause of death.
PARENTS’ CLAIM The mother claimed she was not informed of the risks, benefits, and alternatives to vacuum extraction; she would not have consented had she known the risks. The mother, her husband, and two family members maintained that the ObGyn offered the possibility of cesarean delivery as a question, but did not insist on it. The mother claimed she wanted what was best for the baby, and never refused a cesarean. The resuscitation efforts caused eosinophilic infiltration into several organs.
PHYSICIAN’S DEFENSE The ObGyn charted that the parents were “adamant about having a vaginal delivery,” and said she told the parents what she charted. The obstetric nurse testified that the mother delayed consent because she felt vaginal delivery was imminent. The ObGyn acted properly; eosinophilia caused the baby’s death.
VERDICT An Illinois defense verdict was returned.
HIGH BP TO BLAME FOR DEATHS OF BOTH MOTHER AND CHILD
A 23-year-old woman’s pregnancy was at high risk because of very high blood pressure (BP). At 34 weeks’ gestation, she went to a county hospital with symptoms of high BP; she was treated and discharged 3 days later. She returned to the hospital to be checked twice more within a month. The day after the third visit, she suffered a seizure and was taken to a university hospital, where emergency cesarean delivery was performed. The mother died from an aortic rupture during delivery.
The child was born with brain injuries and died at age 4 years due to neurologic complications.
ESTATE’S CLAIM The mother was not properly treated at the county hospital, resulting in both deaths; she should not have been discharged. Under monitoring, she would have undergone delivery before the aortic rupture occurred, avoiding the baby’s brain injury.
DEFENDANTS’ DEFENSE The mother was stable when released; aortic rupture is unpredictable and unpreventable, and would have occurred under any circumstances. It is highly unusual that a woman of her age would have an aortic rupture.
VERDICT A $3,062,803 California verdict was returned. The parties then settled for $1,782,000 (with the county assuming the medical lien).
NECROTIZING FASCIITIS FROM PERFORATED COLON
A woman underwent laparoscopic-assisted vaginal hysterectomy performed by her ObGyn, and was discharged after 3 days. The next day, she went to another hospital’s emergency department (ED) with abdominal distention and rigidity, severe abdominal pain, and vomiting. She had a toxic appearance, rapid pulse rate, and hypotension. In emergency surgery, several liters of dark brown, foul-smelling fluid were found in her abdomen, and feculent peritonitis and necrotizing fasciitis were diagnosed due to a perforated sigmoid colon. She required multiple hospitalizations and operations.
PATIENT’S CLAIM Perforation occurred during hysterectomy. The ObGyn failed to recognize the injury prior to discharge. The hospital staff did not properly assess her or communicate her symptoms to the ObGyn.
DEFENDANTS’ DEFENSE There was no negligence; proper care was given.
VERDICT A $2,922,503 Florida verdict was returned, with the jury finding the ObGyn 30% at fault and the hospital 70% at fault.
FAILURE TO REACT TO FETAL DISTRESS: $15.6M
After delivery at full term, a child suffered convulsions and seizures on her second day of life. A CT scan showed brain injuries. At age 11 years, she has severe learning and developmental delays, and requires 24-hour care.
PARENTS’ CLAIM Severe decelerations with slow return to baseline occurred several times during labor and delivery. The nurse midwife failed to recognize and react to fetal distress. A cesarean delivery should have been performed instead of a vaginal delivery. The delay in delivery caused the child’s injuries.
DEFENDANTS’ DEFENSE A prenatal neurogenetic disorder caused the child’s injuries.
VERDICT A $15.6 million Maryland verdict was returned. It will not be automatically reduced; the awarded noneconomic damages do not exceed the state cap.
LATE DELIVERY; SEVERE INJURY TO CHILD
At 40 weeks’ gestation, a woman was admitted to the hospital in labor. When the mother’s membranes were ruptured, a small amount of meconium was noted, but the fetal monitor strips were reassuring. Two hours later, the nurse and midwife noted a pattern of decelerations, but they felt the pattern was nonrepetitive and reactive. Thirty minutes later, the nurse and midwife noted decelerations to 90 bpm with pushing, but did not call a physician.
Another midwife arrived to assist the first midwife who was new to practice. The mother was given oxygen, her position was changed, and an IV fluid bolus was administered. Thirty minutes later, the nurses recognized late decelerations and called a Code White twice while the fetal heart rate continued to decelerate. After the attending physician unsuccessfully attempted vacuum extraction, an emergency cesarean delivery was performed.
The child’s Apgar scores were 2, 3, and 3, at 1, 5, and 10 minutes, respectively. The cord blood pH was 6.66, indicating severe metabolic acidosis. She developed seizures within the first few minutes of life. Imaging studies showed global hypoxic ischemic encephalopathy. The child cannot walk, talk, or sit up unsupported at age 8, and requires a G-tube. She is cortically blind and requires antiseizure medication.
PARENTS’ CLAIM The nurse, two midwives, and physician were negligent in their care of the mother and child.
DEFENDANTS’ DEFENSE The case was settled during the trial.
VERDICT A $5 million Massachusetts settlement was reached.
WHAT CAUSED INFECTION AFTER ABORTION?
A 20-year-old woman underwent a surgical termination of pregnancy performed by an ObGyn. After discharge, the patient developed pain and other complications requiring rehospitalization and additional surgery for a pelvic infection.
PATIENT’S CLAIM Complications were due to a uterine perforation that spontaneously sealed before it could be detected. The ObGyn was negligent in the performance of the elective abortion. The patient has a large scar on her abdomen because of the additional operation.
PHYSICIAN’S DEFENSE Perforation of the uterus is a known complication of the procedure. However, no perforation occurred; it was not found on imaging, and spontaneous sealing of a perforation cannot occur. The patient’s complications were due to a subclinical infection that was activated by the surgery.
VERDICT A New York defense verdict was returned.
We want to hear from you. Tell us what you think!
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
A woman in her 50s underwent hysterectomy performed by a surgeon, who then assigned an ObGyn to her follow-up care. The day after surgery, the patient had severe abdominal pain with decreased blood pressure and increased heart and respiration rates. The ObGyn admitted the patient to the intensive care unit (ICU), and then designated Dr. A, the patient’s family practitioner to continue her care. Dr. A was not available, so his associate, Dr. B, took over. Over the phone, Dr. B requested pulmonary, cardiology, and infectious disease consults. In the ICU the next day, the patient suffered respiratory arrest and was intubated. When her abdomen became rigid and swollen, emergency surgery revealed that a colon perforation had allowed fecal matter to reach the abdominal cavity. The woman died the next day from complications of sepsis, peritonitis, and multiple organ failure.
ESTATE’S CLAIM None of the physicians assigned to her care ever saw the patient in the ICU. Earlier surgery could have prevented her death. The physicians involved in her care failed to communicate with each other properly.
DEFENDANTS’ DEFENSE The case was settled during the trial.
VERDICT A $3.2 million Illinois settlement was reached with the hospital.
BOTH PARENTS HAD PLATELET ANTIBODIES
When a 32-year-old woman became pregnant with her third child, she sought treatment at a clinic. The mother informed the nurse practi-tioner that her two other children had been diagnosed with low platelets at birth, but they were now healthy and had no further problems.
The woman gave birth vaginally to her third child at term. The newborn had Apgar scores of 8 and 8, at 1 and 5 minutes, respectively. However, the child’s platelet level was 26 x 103/µL. The baby was transferred to another hospital the next day, where he was diagnosed with hydrocephalus and neonatal alloimmune thrombocytopenia. He suffered a massive intracranial hemorrhage, which caused severe neurologic injuries and brain damage. A shunt was placed. The child has significant cognitive deficits as well as cerebral palsy with mild developmental delays. Testing showed that each parent had a different genotype for platelet antibodies.
PARENTS’ CLAIM The parents should have been tested for platelet antibodies prior to this birth due to the family’s history. A prenatal diagnosis of neonatal alloimmune thrombocytopenia would have allowed for treatment with gamma globulin, which could have avoided the intracranial hemorrhage.
DEFENDANTS’ DEFENSE The case was settled during the trial.
VERDICT A $4.8 million California settlement was reached.
CORD PROLAPSE NOT CARED FOR IN AMBULANCE
At 36 weeks’ gestation, a mother called an ambulance when her membranes ruptured and she noticed an umbilical cord prolapse.
The child was in a breech presentation, experienced oxygen deprivation, and sustained severe neurologic damage.
PARENTS’ CLAIM The ambulance service was negligent in its care. The ambulance service dispatcher advised the mother to stand, squat, and push before the ambulance arrived. The ambulance attendants failed to take basic actions to relieve pressure on the prolapsed umbilical cord. The ambulance did not stop at two closer hospitals, which delayed arrival for an additional 20 minutes.
DEFENDANTS’ DEFENSE The case was settled during the trial.
VERDICT A $2.7 million settlement was reached, but before it was submitted to the court for approval, the child died. The defendants then sought to revoke the settlement, but the parents claimed breach of contract. The defendants claimed that the agreement was orally negotiated independent of defense counsel and was unenforceable due to the child’s death and lack of court approval. A Texas judge issued summary judgment on breach of contract and awarded $2.7 million plus $40,000 in attorney fees to the parents.
SECOND- AND THIRD-DEGREE BURNS TO PERINEUM
A mother received an epidural injection during vaginal delivery. Six hours later, the patient asked a nurse for a warm compress to place on her perineum. The nurse heated the compress in a microwave and then applied it to the perineal area. The compress caused second- and third-degree burns to the patient’s labia and inner left thigh. She underwent surgical repair of the burned area, and, a year later, had plastic surgery.
PATIENT’S CLAIM The nurse was negligent in overheating the compress.
DEFENDANTS’ DEFENSE The hospital agreed that the nurse who heated and applied the compress had been negligent. The hospital paid all medical expenses relating to the burns, including follow-up surgeries.
VERDICT A $190,000 Utah verdict was returned for noneconomic damages.
DOCUMENTATION MAKES A DIFFERENCE FOR OBGYN AFTER CHILD DIES
A 30-year-old physician was pregnant with her first child. Due to a low amniotic fluid index and lagging fetal growth, she saw a maternal-fetal medicine specialist, who suggested labor induction at 39 weeks.
Labor progressed slowly. After three attempts at vacuum-assisted delivery, the ObGyn recommended cesarean delivery. The parents eventually consented to cesarean delivery after another failed vacuum-assisted attempt. Although the ObGyn had recommended cesarean 2 hours earlier, surgery was not ordered on an emergent basis.
At birth, the baby’s resuscitation took more than 20 minutes. The child lost nearly one-third of her blood volume; she had a subgaleal hemorrhage. Both parties agreed that the vacuum device probably caused the bleeding.
The child had hypoxic ischemic encephalopathy and disseminated intravascular coagulation. She suffered a myocardial infarction at 3 days of age. Without electrical brain activity, life support was removed, and the child died at 5 days of age. An autopsy found possible hypereosinophilic syndrome as the concurrent cause of death.
PARENTS’ CLAIM The mother claimed she was not informed of the risks, benefits, and alternatives to vacuum extraction; she would not have consented had she known the risks. The mother, her husband, and two family members maintained that the ObGyn offered the possibility of cesarean delivery as a question, but did not insist on it. The mother claimed she wanted what was best for the baby, and never refused a cesarean. The resuscitation efforts caused eosinophilic infiltration into several organs.
PHYSICIAN’S DEFENSE The ObGyn charted that the parents were “adamant about having a vaginal delivery,” and said she told the parents what she charted. The obstetric nurse testified that the mother delayed consent because she felt vaginal delivery was imminent. The ObGyn acted properly; eosinophilia caused the baby’s death.
VERDICT An Illinois defense verdict was returned.
HIGH BP TO BLAME FOR DEATHS OF BOTH MOTHER AND CHILD
A 23-year-old woman’s pregnancy was at high risk because of very high blood pressure (BP). At 34 weeks’ gestation, she went to a county hospital with symptoms of high BP; she was treated and discharged 3 days later. She returned to the hospital to be checked twice more within a month. The day after the third visit, she suffered a seizure and was taken to a university hospital, where emergency cesarean delivery was performed. The mother died from an aortic rupture during delivery.
The child was born with brain injuries and died at age 4 years due to neurologic complications.
ESTATE’S CLAIM The mother was not properly treated at the county hospital, resulting in both deaths; she should not have been discharged. Under monitoring, she would have undergone delivery before the aortic rupture occurred, avoiding the baby’s brain injury.
DEFENDANTS’ DEFENSE The mother was stable when released; aortic rupture is unpredictable and unpreventable, and would have occurred under any circumstances. It is highly unusual that a woman of her age would have an aortic rupture.
VERDICT A $3,062,803 California verdict was returned. The parties then settled for $1,782,000 (with the county assuming the medical lien).
NECROTIZING FASCIITIS FROM PERFORATED COLON
A woman underwent laparoscopic-assisted vaginal hysterectomy performed by her ObGyn, and was discharged after 3 days. The next day, she went to another hospital’s emergency department (ED) with abdominal distention and rigidity, severe abdominal pain, and vomiting. She had a toxic appearance, rapid pulse rate, and hypotension. In emergency surgery, several liters of dark brown, foul-smelling fluid were found in her abdomen, and feculent peritonitis and necrotizing fasciitis were diagnosed due to a perforated sigmoid colon. She required multiple hospitalizations and operations.
PATIENT’S CLAIM Perforation occurred during hysterectomy. The ObGyn failed to recognize the injury prior to discharge. The hospital staff did not properly assess her or communicate her symptoms to the ObGyn.
DEFENDANTS’ DEFENSE There was no negligence; proper care was given.
VERDICT A $2,922,503 Florida verdict was returned, with the jury finding the ObGyn 30% at fault and the hospital 70% at fault.
FAILURE TO REACT TO FETAL DISTRESS: $15.6M
After delivery at full term, a child suffered convulsions and seizures on her second day of life. A CT scan showed brain injuries. At age 11 years, she has severe learning and developmental delays, and requires 24-hour care.
PARENTS’ CLAIM Severe decelerations with slow return to baseline occurred several times during labor and delivery. The nurse midwife failed to recognize and react to fetal distress. A cesarean delivery should have been performed instead of a vaginal delivery. The delay in delivery caused the child’s injuries.
DEFENDANTS’ DEFENSE A prenatal neurogenetic disorder caused the child’s injuries.
VERDICT A $15.6 million Maryland verdict was returned. It will not be automatically reduced; the awarded noneconomic damages do not exceed the state cap.
LATE DELIVERY; SEVERE INJURY TO CHILD
At 40 weeks’ gestation, a woman was admitted to the hospital in labor. When the mother’s membranes were ruptured, a small amount of meconium was noted, but the fetal monitor strips were reassuring. Two hours later, the nurse and midwife noted a pattern of decelerations, but they felt the pattern was nonrepetitive and reactive. Thirty minutes later, the nurse and midwife noted decelerations to 90 bpm with pushing, but did not call a physician.
Another midwife arrived to assist the first midwife who was new to practice. The mother was given oxygen, her position was changed, and an IV fluid bolus was administered. Thirty minutes later, the nurses recognized late decelerations and called a Code White twice while the fetal heart rate continued to decelerate. After the attending physician unsuccessfully attempted vacuum extraction, an emergency cesarean delivery was performed.
The child’s Apgar scores were 2, 3, and 3, at 1, 5, and 10 minutes, respectively. The cord blood pH was 6.66, indicating severe metabolic acidosis. She developed seizures within the first few minutes of life. Imaging studies showed global hypoxic ischemic encephalopathy. The child cannot walk, talk, or sit up unsupported at age 8, and requires a G-tube. She is cortically blind and requires antiseizure medication.
PARENTS’ CLAIM The nurse, two midwives, and physician were negligent in their care of the mother and child.
DEFENDANTS’ DEFENSE The case was settled during the trial.
VERDICT A $5 million Massachusetts settlement was reached.
WHAT CAUSED INFECTION AFTER ABORTION?
A 20-year-old woman underwent a surgical termination of pregnancy performed by an ObGyn. After discharge, the patient developed pain and other complications requiring rehospitalization and additional surgery for a pelvic infection.
PATIENT’S CLAIM Complications were due to a uterine perforation that spontaneously sealed before it could be detected. The ObGyn was negligent in the performance of the elective abortion. The patient has a large scar on her abdomen because of the additional operation.
PHYSICIAN’S DEFENSE Perforation of the uterus is a known complication of the procedure. However, no perforation occurred; it was not found on imaging, and spontaneous sealing of a perforation cannot occur. The patient’s complications were due to a subclinical infection that was activated by the surgery.
VERDICT A New York defense verdict was returned.
We want to hear from you. Tell us what you think!
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.