User login
AGA President Brings Forth “Message Of Inclusivity”
“I was always interested in medicine. From a relatively early age I thought that’s what I would be doing,” said Dr. Kim. When his father became disillusioned with his own career as a pathologist, he encouraged his son to look in other directions.
“In college I had the opportunity to study and learn broadly and I became interested in public policy and eventually majored in that discipline,” he said.
The mentorship of the late Uwe Reinhardt, a well-respected health economist at Princeton University, had a major impact on Dr. Kim during his senior year of college. Reinhardt told him that physicians are afforded a special position in society. “They have a moral responsibility to take the lead in terms of guiding and shaping healthcare. His message made a big impression upon me,” said Dr. Kim.
Ultimately, he decided to go into clinical medicine, but maintained his interest in healthcare policy. Experiences outside of the standard approach to medicine “helped me stay in the big picture of healthcare, to make a difference beyond just my individual patients. And that’s played a big part in keeping me involved in organized medicine,” said Dr. Kim, who began his term as AGA president in May 2025.
Dr. Kim is also a partner at South Denver Gastroenterology, a 33-provider, independent gastroenterology practice in Colorado. As the first physician in Colorado with fellowship training in endoscopic ultrasound, he introduced this service line into South Denver’s advanced endoscopy practice.
Dr. Kim has served in numerous roles with AGA, among them the co-director of the AGA Clinical Congress, the Partners in Quality program, and the Nurse Practitioner and Physician Assistant Course. He is a Digestive Disease Week® abstract reviewer, has served as AGA representative to the Accreditation Association for Ambulatory Health Care and to the Alliance of Specialty Medicine. He has also served on the AGA Governing Board as clinical private practice councilor and secretary treasurer.
He discussed the high points of his career in an interview, revealing his plans as AGA president for unifying the sectors of GI medicine and fostering GI innovation and technology.
As the new AGA president, what are your goals for the society?
Dr. Kim: I want to put out a message of inclusivity. I think what’s special about AGA is that we’re the society for all gastroenterologists. Among all the other GI organizations, I think we really have the biggest tent and we work to unite clinicians, educators, and researchers – all gastroenterologists, regardless of their individual practice situation. These days, there is a tendency toward tribalism. People are starting to gravitate toward limiting their interactions to others that are from the same backgrounds. But as gastroenterologists we have more that unites us than divides us. It’s only by working together that we can make things better for everyone.
I think the second point is that we’re on the cusp of some important transformations in gastroenterology. The screening colonoscopy model that has sustained our specialty for decades is rapidly evolving. In addition, there is an increasing ability for patients as consumers to direct their own care through advances in technology, such as virtual health platforms. We’re seeing this as patients increasingly adopt things like complementary and alternative medicine outside of the standard model of physician-directed healthcare. These are two important trends that gastroenterologists need to be aware of and learn how to manage and to adapt to. I think AGA’s role is to help guide that evolution and to give physicians the tools to be able to respond.
We want to focus on innovation and we want to focus on practical solutions.
In terms of fostering innovation in gastroenterology, we’re the first medical professional society to create an incubator for new technologies. Not only do we provide that resource to our members, but we’re also putting our money where our mouth is. Through venture capital initiatives such as our GI Opportunity Fund, we directly invest in companies that we’re helping to develop.
On the practice side, we have been engaging directly with payers to foster improved communication and address pain points on both sides. I think we’re the only medical society that’s taking this type of approach and moving away from the traditional adversarial approach to dealing with payers. Recently, we had a very productive discussion with UnitedHealthcare around some of their upcoming formulary changes for inflammatory bowel disease. We used that opportunity to highlight how nonmedical switching between existing therapies can adversely impact patients, as well as increasing burden of red tape for practices.
Your practice was one of the original groups that formed the Digestive Health Physicians Association (DPHA). What accomplishments of the association are you most proud of?
Dr. Kim: DHPA formed about 10 years ago as an advocacy organization to combat a specific perceived threat, which was the in-office ancillary exception. This is the legislative pathway that allows gastroenterologists to provide ancillary services within their practice. An example of this is pathology for endoscopic procedures, which is an incredible value to patients and improves quality of care. This was under a significant legislative threat at that time. As independent physicians, DHPA took the lead in advocating against eliminating that exception.
I think the larger accomplishment was it demonstrated that gastroenterologists, specifically independent community practice gastroenterologists, could come together successfully and advocate for issues that were of importance to our specialty. AGA and DHPA have worked very well together, collaborating on shared policy interests and have worked closely on both legislative as well as regulatory issues. We’ve sponsored joint meetings that we’ve programmed together and we’re looking forward to continuing a robust partnership.
You have introduced several new clinical practice and practice management models. Can you discuss the part-time partnership model and what it has achieved?
Dr. Kim: Like many practices, South Denver Gastroenterology historically required physician partners to work full time. This conflicted with our desire and our need to attract more women gastroenterologists into our practice. The process involved careful analysis of our direct and indirect expenses, but more importantly it required a negotiation and a meeting of the minds among our partners. A lot of this ultimately came down to trust. It helped a great deal that our practice has always had strong cohesiveness. That helped us to build that trust that partners would stay engaged in the practice even if they worked part time.
Our practice has also always prioritized work-life balance. We were able to come up with a formula that allows partners to work three days per week, retaining their partnership interest and their participation in practice decisions. They stay involved but are also financially sustainable for the practice. It’s been very successful. It’s been a big draw, not just for women, but it has allowed us to create a situation where women are fully one third of our partnership. It’s something we’re all extremely proud of.
How did you get involved in AGA?
Dr. Kim: One of the first projects I participated in was the Roadmap to the Future of GI Practice. This was an initiative to help prepare GI practices for value-based care. We did things like develop quality measure sets for GI conditions such as inflammatory bowel disease and hepatitis C. We published a bundled payment model for screening colonoscopies. We also created a model for obesity management by gastroenterologists. This was 15 years ago, and I think it was about 15 years ahead of its time! It’s interesting to see how many of these changes in GI practice that we envisioned are slowly coming to pass.
I saw that AGA was interested in me as a community-based clinician. They focused on trying to develop those practical tools to help me succeed. It’s one of the reasons I’ve stayed engaged.
What is your approach to patient communication and education?
Dr. Kim: There are two things that I always tell both my staff as well as young people who come to me asking for advice. I think the first and most important is that you should always strive to treat your patients the way that you would want your family treated. Of course, we’re not perfect, but when that doesn’t happen, look at your behavior, the way that you’re interacting, but also the way the system is treating your patients and try to improve things within your own practice. And then the other thing that I tell folks is try to spend more time listening to your patients than talking or speaking at them.
What do you think is the biggest misconception about GI?
Dr. Kim: We’re not just about colonoscopies! I went into GI not just because I enjoy performing procedures, but because our specialty covers such a broad spectrum of physiology and diseases. We also have the ability as gastroenterologists to develop long-term relationships with our patients. I’ve been in practice now more than 25 years, and the greatest satisfaction in my career doesn’t come from the endoscopy center, although I still enjoy performing procedures. It comes from the clinic; it comes from the patients whom I’ve known for decades, and the interaction and conversations that I can have with them, the ability to see their families, their parents, and now in some cases their kids or even their grandkids. It’s incredibly satisfying. It makes my job fun.
What advice would you give to aspiring medical students?
Dr. Kim: One of the things I would say is stay involved in organized medicine. As physicians, we are endowed with great trust. We also have a great responsibility to help shape our healthcare care system. If we work together, we really can make a difference, not just for our profession, but also for society at large and for the patients whom we serve.
I really hope that young people don’t lose their optimism. We hear a lot these days about how much negativity and pessimism there is about the future, especially among young people in our society. But I think it’s a great time to be in medicine. Advances in medical science have made huge strides in our ability to make real differences for our patients. And the pace of technology progress is only going to continue to accelerate. Sure, there are lots of shortcomings in the practice of medicine, but honestly, that’s always been the case. I have faith that as a profession, we are smart people, we’re committed people, and we will be successful in overcoming those challenges. That’s the message that I have for young folks.
Lightning Round
Coffee or tea?
Coffee, black
What’s one hobby you’d like to pick up?
Anything except pickleball
What’s your favorite season of the year?
Winter, I’m a skier
What’s your favorite way to spend a weekend?
Doing anything outside
If you could have dinner with any historical figure, who would it be?
Ben Franklin
What’s your go-to karaoke song?
You don’t want to hear me sing
What’s one thing on your bucket list?
Skiing in South America
What’s the best piece of advice you’ve ever received?
Follow your heart
“I was always interested in medicine. From a relatively early age I thought that’s what I would be doing,” said Dr. Kim. When his father became disillusioned with his own career as a pathologist, he encouraged his son to look in other directions.
“In college I had the opportunity to study and learn broadly and I became interested in public policy and eventually majored in that discipline,” he said.
The mentorship of the late Uwe Reinhardt, a well-respected health economist at Princeton University, had a major impact on Dr. Kim during his senior year of college. Reinhardt told him that physicians are afforded a special position in society. “They have a moral responsibility to take the lead in terms of guiding and shaping healthcare. His message made a big impression upon me,” said Dr. Kim.
Ultimately, he decided to go into clinical medicine, but maintained his interest in healthcare policy. Experiences outside of the standard approach to medicine “helped me stay in the big picture of healthcare, to make a difference beyond just my individual patients. And that’s played a big part in keeping me involved in organized medicine,” said Dr. Kim, who began his term as AGA president in May 2025.
Dr. Kim is also a partner at South Denver Gastroenterology, a 33-provider, independent gastroenterology practice in Colorado. As the first physician in Colorado with fellowship training in endoscopic ultrasound, he introduced this service line into South Denver’s advanced endoscopy practice.
Dr. Kim has served in numerous roles with AGA, among them the co-director of the AGA Clinical Congress, the Partners in Quality program, and the Nurse Practitioner and Physician Assistant Course. He is a Digestive Disease Week® abstract reviewer, has served as AGA representative to the Accreditation Association for Ambulatory Health Care and to the Alliance of Specialty Medicine. He has also served on the AGA Governing Board as clinical private practice councilor and secretary treasurer.
He discussed the high points of his career in an interview, revealing his plans as AGA president for unifying the sectors of GI medicine and fostering GI innovation and technology.
As the new AGA president, what are your goals for the society?
Dr. Kim: I want to put out a message of inclusivity. I think what’s special about AGA is that we’re the society for all gastroenterologists. Among all the other GI organizations, I think we really have the biggest tent and we work to unite clinicians, educators, and researchers – all gastroenterologists, regardless of their individual practice situation. These days, there is a tendency toward tribalism. People are starting to gravitate toward limiting their interactions to others that are from the same backgrounds. But as gastroenterologists we have more that unites us than divides us. It’s only by working together that we can make things better for everyone.
I think the second point is that we’re on the cusp of some important transformations in gastroenterology. The screening colonoscopy model that has sustained our specialty for decades is rapidly evolving. In addition, there is an increasing ability for patients as consumers to direct their own care through advances in technology, such as virtual health platforms. We’re seeing this as patients increasingly adopt things like complementary and alternative medicine outside of the standard model of physician-directed healthcare. These are two important trends that gastroenterologists need to be aware of and learn how to manage and to adapt to. I think AGA’s role is to help guide that evolution and to give physicians the tools to be able to respond.
We want to focus on innovation and we want to focus on practical solutions.
In terms of fostering innovation in gastroenterology, we’re the first medical professional society to create an incubator for new technologies. Not only do we provide that resource to our members, but we’re also putting our money where our mouth is. Through venture capital initiatives such as our GI Opportunity Fund, we directly invest in companies that we’re helping to develop.
On the practice side, we have been engaging directly with payers to foster improved communication and address pain points on both sides. I think we’re the only medical society that’s taking this type of approach and moving away from the traditional adversarial approach to dealing with payers. Recently, we had a very productive discussion with UnitedHealthcare around some of their upcoming formulary changes for inflammatory bowel disease. We used that opportunity to highlight how nonmedical switching between existing therapies can adversely impact patients, as well as increasing burden of red tape for practices.
Your practice was one of the original groups that formed the Digestive Health Physicians Association (DPHA). What accomplishments of the association are you most proud of?
Dr. Kim: DHPA formed about 10 years ago as an advocacy organization to combat a specific perceived threat, which was the in-office ancillary exception. This is the legislative pathway that allows gastroenterologists to provide ancillary services within their practice. An example of this is pathology for endoscopic procedures, which is an incredible value to patients and improves quality of care. This was under a significant legislative threat at that time. As independent physicians, DHPA took the lead in advocating against eliminating that exception.
I think the larger accomplishment was it demonstrated that gastroenterologists, specifically independent community practice gastroenterologists, could come together successfully and advocate for issues that were of importance to our specialty. AGA and DHPA have worked very well together, collaborating on shared policy interests and have worked closely on both legislative as well as regulatory issues. We’ve sponsored joint meetings that we’ve programmed together and we’re looking forward to continuing a robust partnership.
You have introduced several new clinical practice and practice management models. Can you discuss the part-time partnership model and what it has achieved?
Dr. Kim: Like many practices, South Denver Gastroenterology historically required physician partners to work full time. This conflicted with our desire and our need to attract more women gastroenterologists into our practice. The process involved careful analysis of our direct and indirect expenses, but more importantly it required a negotiation and a meeting of the minds among our partners. A lot of this ultimately came down to trust. It helped a great deal that our practice has always had strong cohesiveness. That helped us to build that trust that partners would stay engaged in the practice even if they worked part time.
Our practice has also always prioritized work-life balance. We were able to come up with a formula that allows partners to work three days per week, retaining their partnership interest and their participation in practice decisions. They stay involved but are also financially sustainable for the practice. It’s been very successful. It’s been a big draw, not just for women, but it has allowed us to create a situation where women are fully one third of our partnership. It’s something we’re all extremely proud of.
How did you get involved in AGA?
Dr. Kim: One of the first projects I participated in was the Roadmap to the Future of GI Practice. This was an initiative to help prepare GI practices for value-based care. We did things like develop quality measure sets for GI conditions such as inflammatory bowel disease and hepatitis C. We published a bundled payment model for screening colonoscopies. We also created a model for obesity management by gastroenterologists. This was 15 years ago, and I think it was about 15 years ahead of its time! It’s interesting to see how many of these changes in GI practice that we envisioned are slowly coming to pass.
I saw that AGA was interested in me as a community-based clinician. They focused on trying to develop those practical tools to help me succeed. It’s one of the reasons I’ve stayed engaged.
What is your approach to patient communication and education?
Dr. Kim: There are two things that I always tell both my staff as well as young people who come to me asking for advice. I think the first and most important is that you should always strive to treat your patients the way that you would want your family treated. Of course, we’re not perfect, but when that doesn’t happen, look at your behavior, the way that you’re interacting, but also the way the system is treating your patients and try to improve things within your own practice. And then the other thing that I tell folks is try to spend more time listening to your patients than talking or speaking at them.
What do you think is the biggest misconception about GI?
Dr. Kim: We’re not just about colonoscopies! I went into GI not just because I enjoy performing procedures, but because our specialty covers such a broad spectrum of physiology and diseases. We also have the ability as gastroenterologists to develop long-term relationships with our patients. I’ve been in practice now more than 25 years, and the greatest satisfaction in my career doesn’t come from the endoscopy center, although I still enjoy performing procedures. It comes from the clinic; it comes from the patients whom I’ve known for decades, and the interaction and conversations that I can have with them, the ability to see their families, their parents, and now in some cases their kids or even their grandkids. It’s incredibly satisfying. It makes my job fun.
What advice would you give to aspiring medical students?
Dr. Kim: One of the things I would say is stay involved in organized medicine. As physicians, we are endowed with great trust. We also have a great responsibility to help shape our healthcare care system. If we work together, we really can make a difference, not just for our profession, but also for society at large and for the patients whom we serve.
I really hope that young people don’t lose their optimism. We hear a lot these days about how much negativity and pessimism there is about the future, especially among young people in our society. But I think it’s a great time to be in medicine. Advances in medical science have made huge strides in our ability to make real differences for our patients. And the pace of technology progress is only going to continue to accelerate. Sure, there are lots of shortcomings in the practice of medicine, but honestly, that’s always been the case. I have faith that as a profession, we are smart people, we’re committed people, and we will be successful in overcoming those challenges. That’s the message that I have for young folks.
Lightning Round
Coffee or tea?
Coffee, black
What’s one hobby you’d like to pick up?
Anything except pickleball
What’s your favorite season of the year?
Winter, I’m a skier
What’s your favorite way to spend a weekend?
Doing anything outside
If you could have dinner with any historical figure, who would it be?
Ben Franklin
What’s your go-to karaoke song?
You don’t want to hear me sing
What’s one thing on your bucket list?
Skiing in South America
What’s the best piece of advice you’ve ever received?
Follow your heart
“I was always interested in medicine. From a relatively early age I thought that’s what I would be doing,” said Dr. Kim. When his father became disillusioned with his own career as a pathologist, he encouraged his son to look in other directions.
“In college I had the opportunity to study and learn broadly and I became interested in public policy and eventually majored in that discipline,” he said.
The mentorship of the late Uwe Reinhardt, a well-respected health economist at Princeton University, had a major impact on Dr. Kim during his senior year of college. Reinhardt told him that physicians are afforded a special position in society. “They have a moral responsibility to take the lead in terms of guiding and shaping healthcare. His message made a big impression upon me,” said Dr. Kim.
Ultimately, he decided to go into clinical medicine, but maintained his interest in healthcare policy. Experiences outside of the standard approach to medicine “helped me stay in the big picture of healthcare, to make a difference beyond just my individual patients. And that’s played a big part in keeping me involved in organized medicine,” said Dr. Kim, who began his term as AGA president in May 2025.
Dr. Kim is also a partner at South Denver Gastroenterology, a 33-provider, independent gastroenterology practice in Colorado. As the first physician in Colorado with fellowship training in endoscopic ultrasound, he introduced this service line into South Denver’s advanced endoscopy practice.
Dr. Kim has served in numerous roles with AGA, among them the co-director of the AGA Clinical Congress, the Partners in Quality program, and the Nurse Practitioner and Physician Assistant Course. He is a Digestive Disease Week® abstract reviewer, has served as AGA representative to the Accreditation Association for Ambulatory Health Care and to the Alliance of Specialty Medicine. He has also served on the AGA Governing Board as clinical private practice councilor and secretary treasurer.
He discussed the high points of his career in an interview, revealing his plans as AGA president for unifying the sectors of GI medicine and fostering GI innovation and technology.
As the new AGA president, what are your goals for the society?
Dr. Kim: I want to put out a message of inclusivity. I think what’s special about AGA is that we’re the society for all gastroenterologists. Among all the other GI organizations, I think we really have the biggest tent and we work to unite clinicians, educators, and researchers – all gastroenterologists, regardless of their individual practice situation. These days, there is a tendency toward tribalism. People are starting to gravitate toward limiting their interactions to others that are from the same backgrounds. But as gastroenterologists we have more that unites us than divides us. It’s only by working together that we can make things better for everyone.
I think the second point is that we’re on the cusp of some important transformations in gastroenterology. The screening colonoscopy model that has sustained our specialty for decades is rapidly evolving. In addition, there is an increasing ability for patients as consumers to direct their own care through advances in technology, such as virtual health platforms. We’re seeing this as patients increasingly adopt things like complementary and alternative medicine outside of the standard model of physician-directed healthcare. These are two important trends that gastroenterologists need to be aware of and learn how to manage and to adapt to. I think AGA’s role is to help guide that evolution and to give physicians the tools to be able to respond.
We want to focus on innovation and we want to focus on practical solutions.
In terms of fostering innovation in gastroenterology, we’re the first medical professional society to create an incubator for new technologies. Not only do we provide that resource to our members, but we’re also putting our money where our mouth is. Through venture capital initiatives such as our GI Opportunity Fund, we directly invest in companies that we’re helping to develop.
On the practice side, we have been engaging directly with payers to foster improved communication and address pain points on both sides. I think we’re the only medical society that’s taking this type of approach and moving away from the traditional adversarial approach to dealing with payers. Recently, we had a very productive discussion with UnitedHealthcare around some of their upcoming formulary changes for inflammatory bowel disease. We used that opportunity to highlight how nonmedical switching between existing therapies can adversely impact patients, as well as increasing burden of red tape for practices.
Your practice was one of the original groups that formed the Digestive Health Physicians Association (DPHA). What accomplishments of the association are you most proud of?
Dr. Kim: DHPA formed about 10 years ago as an advocacy organization to combat a specific perceived threat, which was the in-office ancillary exception. This is the legislative pathway that allows gastroenterologists to provide ancillary services within their practice. An example of this is pathology for endoscopic procedures, which is an incredible value to patients and improves quality of care. This was under a significant legislative threat at that time. As independent physicians, DHPA took the lead in advocating against eliminating that exception.
I think the larger accomplishment was it demonstrated that gastroenterologists, specifically independent community practice gastroenterologists, could come together successfully and advocate for issues that were of importance to our specialty. AGA and DHPA have worked very well together, collaborating on shared policy interests and have worked closely on both legislative as well as regulatory issues. We’ve sponsored joint meetings that we’ve programmed together and we’re looking forward to continuing a robust partnership.
You have introduced several new clinical practice and practice management models. Can you discuss the part-time partnership model and what it has achieved?
Dr. Kim: Like many practices, South Denver Gastroenterology historically required physician partners to work full time. This conflicted with our desire and our need to attract more women gastroenterologists into our practice. The process involved careful analysis of our direct and indirect expenses, but more importantly it required a negotiation and a meeting of the minds among our partners. A lot of this ultimately came down to trust. It helped a great deal that our practice has always had strong cohesiveness. That helped us to build that trust that partners would stay engaged in the practice even if they worked part time.
Our practice has also always prioritized work-life balance. We were able to come up with a formula that allows partners to work three days per week, retaining their partnership interest and their participation in practice decisions. They stay involved but are also financially sustainable for the practice. It’s been very successful. It’s been a big draw, not just for women, but it has allowed us to create a situation where women are fully one third of our partnership. It’s something we’re all extremely proud of.
How did you get involved in AGA?
Dr. Kim: One of the first projects I participated in was the Roadmap to the Future of GI Practice. This was an initiative to help prepare GI practices for value-based care. We did things like develop quality measure sets for GI conditions such as inflammatory bowel disease and hepatitis C. We published a bundled payment model for screening colonoscopies. We also created a model for obesity management by gastroenterologists. This was 15 years ago, and I think it was about 15 years ahead of its time! It’s interesting to see how many of these changes in GI practice that we envisioned are slowly coming to pass.
I saw that AGA was interested in me as a community-based clinician. They focused on trying to develop those practical tools to help me succeed. It’s one of the reasons I’ve stayed engaged.
What is your approach to patient communication and education?
Dr. Kim: There are two things that I always tell both my staff as well as young people who come to me asking for advice. I think the first and most important is that you should always strive to treat your patients the way that you would want your family treated. Of course, we’re not perfect, but when that doesn’t happen, look at your behavior, the way that you’re interacting, but also the way the system is treating your patients and try to improve things within your own practice. And then the other thing that I tell folks is try to spend more time listening to your patients than talking or speaking at them.
What do you think is the biggest misconception about GI?
Dr. Kim: We’re not just about colonoscopies! I went into GI not just because I enjoy performing procedures, but because our specialty covers such a broad spectrum of physiology and diseases. We also have the ability as gastroenterologists to develop long-term relationships with our patients. I’ve been in practice now more than 25 years, and the greatest satisfaction in my career doesn’t come from the endoscopy center, although I still enjoy performing procedures. It comes from the clinic; it comes from the patients whom I’ve known for decades, and the interaction and conversations that I can have with them, the ability to see their families, their parents, and now in some cases their kids or even their grandkids. It’s incredibly satisfying. It makes my job fun.
What advice would you give to aspiring medical students?
Dr. Kim: One of the things I would say is stay involved in organized medicine. As physicians, we are endowed with great trust. We also have a great responsibility to help shape our healthcare care system. If we work together, we really can make a difference, not just for our profession, but also for society at large and for the patients whom we serve.
I really hope that young people don’t lose their optimism. We hear a lot these days about how much negativity and pessimism there is about the future, especially among young people in our society. But I think it’s a great time to be in medicine. Advances in medical science have made huge strides in our ability to make real differences for our patients. And the pace of technology progress is only going to continue to accelerate. Sure, there are lots of shortcomings in the practice of medicine, but honestly, that’s always been the case. I have faith that as a profession, we are smart people, we’re committed people, and we will be successful in overcoming those challenges. That’s the message that I have for young folks.
Lightning Round
Coffee or tea?
Coffee, black
What’s one hobby you’d like to pick up?
Anything except pickleball
What’s your favorite season of the year?
Winter, I’m a skier
What’s your favorite way to spend a weekend?
Doing anything outside
If you could have dinner with any historical figure, who would it be?
Ben Franklin
What’s your go-to karaoke song?
You don’t want to hear me sing
What’s one thing on your bucket list?
Skiing in South America
What’s the best piece of advice you’ve ever received?
Follow your heart

Patient Navigators for Serious Illnesses Can Now Bill Under New Medicare Codes
In a move that acknowledges the gauntlet the US health system poses for people facing serious and fatal illnesses, Medicare will pay for a new class of workers to help patients manage treatments for conditions like cancer and heart failure.
The 2024 Medicare physician fee schedule includes new billing codes, including G0023, to pay for 60 minutes a month of care coordination by certified or trained auxiliary personnel working under the direction of a clinician.
A diagnosis of cancer or another serious illness takes a toll beyond the physical effects of the disease. Patients often scramble to make adjustments in family and work schedules to manage treatment, said Samyukta Mullangi, MD, MBA, medical director of oncology at Thyme Care, a Nashville, Tennessee–based firm that provides navigation and coordination services to oncology practices and insurers.
“It just really does create a bit of a pressure cooker for patients,” Dr. Mullangi told this news organization.
Medicare has for many years paid for medical professionals to help patients cope with the complexities of disease, such as chronic care management (CCM) provided by physicians, nurses, and physician assistants.
The new principal illness navigation (PIN) payments are intended to pay for work that to date typically has been done by people without medical degrees, including those involved in peer support networks and community health programs. The US Centers for Medicare and Medicaid Services(CMS) expects these navigators will undergo training and work under the supervision of clinicians.
The new navigators may coordinate care transitions between medical settings, follow up with patients after emergency department (ED) visits, or communicate with skilled nursing facilities regarding the psychosocial needs and functional deficits of a patient, among other functions.
CMS expects the new navigators may:
- Conduct assessments to understand a patient’s life story, strengths, needs, goals, preferences, and desired outcomes, including understanding cultural and linguistic factors.
- Provide support to accomplish the clinician’s treatment plan.
- Coordinate the receipt of needed services from healthcare facilities, home- and community-based service providers, and caregivers.
Peers as Navigators
The new navigators can be former patients who have undergone similar treatments for serious diseases, CMS said. This approach sets the new program apart from other care management services Medicare already covers, program officials wrote in the 2024 physician fee schedule.
“For some conditions, patients are best able to engage with the healthcare system and access care if they have assistance from a single, dedicated individual who has ‘lived experience,’ ” according to the rule.
The agency has taken a broad initial approach in defining what kinds of illnesses a patient may have to qualify for services. Patients must have a serious condition that is expected to last at least 3 months, such as cancer, heart failure, or substance use disorder.
But those without a definitive diagnosis may also qualify to receive navigator services.
In the rule, CMS cited a case in which a CT scan identified a suspicious mass in a patient’s colon. A clinician might decide this person would benefit from navigation services due to the potential risks for an undiagnosed illness.
“Regardless of the definitive diagnosis of the mass, presence of a colonic mass for that patient may be a serious high-risk condition that could, for example, cause obstruction and lead the patient to present to the emergency department, as well as be potentially indicative of an underlying life-threatening illness such as colon cancer,” CMS wrote in the rule.
Navigators often start their work when cancer patients are screened and guide them through initial diagnosis, potential surgery, radiation, or chemotherapy, said Sharon Gentry, MSN, RN, a former nurse navigator who is now the editor in chief of the Journal of the Academy of Oncology Nurse & Patient Navigators.
The navigators are meant to be a trusted and continual presence for patients, who otherwise might be left to start anew in finding help at each phase of care.
The navigators “see the whole picture. They see the whole journey the patient takes, from pre-diagnosis all the way through diagnosis care out through survival,” Ms. Gentry said.
Gaining a special Medicare payment for these kinds of services will elevate this work, she said.
Many newer drugs can target specific mechanisms and proteins of cancer. Often, oncology treatment involves testing to find out if mutations are allowing the cancer cells to evade a patient’s immune system.
Checking these biomarkers takes time, however. Patients sometimes become frustrated because they are anxious to begin treatment. Patients may receive inaccurate information from friends or family who went through treatment previously. Navigators can provide knowledge on the current state of care for a patient’s disease, helping them better manage anxieties.
“You have to explain to them that things have changed since the guy you drink coffee with was diagnosed with cancer, and there may be a drug that could target that,” Ms. Gentry said.
Potential Challenges
Initial uptake of the new PIN codes may be slow going, however, as clinicians and health systems may already use well-established codes. These include CCM and principal care management services, which may pay higher rates, Mullangi said.
“There might be sensitivity around not wanting to cannibalize existing programs with a new program,” Dr. Mullangi said.
In addition, many patients will have a copay for the services of principal illness navigators, Dr. Mullangi said.
While many patients have additional insurance that would cover the service, not all do. People with traditional Medicare coverage can sometimes pay 20% of the cost of some medical services.
“I think that may give patients pause, particularly if they’re already feeling the financial burden of a cancer treatment journey,” Dr. Mullangi said.
Pay rates for PIN services involve calculations of regional price differences, which are posted publicly by CMS, and potential added fees for services provided by hospital-affiliated organizations.
Consider payments for code G0023, covering 60 minutes of principal navigation services provided in a single month.
A set reimbursement for patients cared for in independent medical practices exists, with variation for local costs. Medicare’s non-facility price for G0023 would be $102.41 in some parts of Silicon Valley in California, including San Jose. In Arkansas, where costs are lower, reimbursement would be $73.14 for this same service.
Patients who get services covered by code G0023 in independent medical practices would have monthly copays of about $15-$20, depending on where they live.
The tab for patients tends to be higher for these same services if delivered through a medical practice owned by a hospital, as this would trigger the addition of facility fees to the payments made to cover the services. Facility fees are difficult for the public to ascertain before getting a treatment or service.
Dr. Mullangi and Ms. Gentry reported no relevant financial disclosures outside of their employers.
A version of this article first appeared on Medscape.com.
In a move that acknowledges the gauntlet the US health system poses for people facing serious and fatal illnesses, Medicare will pay for a new class of workers to help patients manage treatments for conditions like cancer and heart failure.
The 2024 Medicare physician fee schedule includes new billing codes, including G0023, to pay for 60 minutes a month of care coordination by certified or trained auxiliary personnel working under the direction of a clinician.
A diagnosis of cancer or another serious illness takes a toll beyond the physical effects of the disease. Patients often scramble to make adjustments in family and work schedules to manage treatment, said Samyukta Mullangi, MD, MBA, medical director of oncology at Thyme Care, a Nashville, Tennessee–based firm that provides navigation and coordination services to oncology practices and insurers.
“It just really does create a bit of a pressure cooker for patients,” Dr. Mullangi told this news organization.
Medicare has for many years paid for medical professionals to help patients cope with the complexities of disease, such as chronic care management (CCM) provided by physicians, nurses, and physician assistants.
The new principal illness navigation (PIN) payments are intended to pay for work that to date typically has been done by people without medical degrees, including those involved in peer support networks and community health programs. The US Centers for Medicare and Medicaid Services(CMS) expects these navigators will undergo training and work under the supervision of clinicians.
The new navigators may coordinate care transitions between medical settings, follow up with patients after emergency department (ED) visits, or communicate with skilled nursing facilities regarding the psychosocial needs and functional deficits of a patient, among other functions.
CMS expects the new navigators may:
- Conduct assessments to understand a patient’s life story, strengths, needs, goals, preferences, and desired outcomes, including understanding cultural and linguistic factors.
- Provide support to accomplish the clinician’s treatment plan.
- Coordinate the receipt of needed services from healthcare facilities, home- and community-based service providers, and caregivers.
Peers as Navigators
The new navigators can be former patients who have undergone similar treatments for serious diseases, CMS said. This approach sets the new program apart from other care management services Medicare already covers, program officials wrote in the 2024 physician fee schedule.
“For some conditions, patients are best able to engage with the healthcare system and access care if they have assistance from a single, dedicated individual who has ‘lived experience,’ ” according to the rule.
The agency has taken a broad initial approach in defining what kinds of illnesses a patient may have to qualify for services. Patients must have a serious condition that is expected to last at least 3 months, such as cancer, heart failure, or substance use disorder.
But those without a definitive diagnosis may also qualify to receive navigator services.
In the rule, CMS cited a case in which a CT scan identified a suspicious mass in a patient’s colon. A clinician might decide this person would benefit from navigation services due to the potential risks for an undiagnosed illness.
“Regardless of the definitive diagnosis of the mass, presence of a colonic mass for that patient may be a serious high-risk condition that could, for example, cause obstruction and lead the patient to present to the emergency department, as well as be potentially indicative of an underlying life-threatening illness such as colon cancer,” CMS wrote in the rule.
Navigators often start their work when cancer patients are screened and guide them through initial diagnosis, potential surgery, radiation, or chemotherapy, said Sharon Gentry, MSN, RN, a former nurse navigator who is now the editor in chief of the Journal of the Academy of Oncology Nurse & Patient Navigators.
The navigators are meant to be a trusted and continual presence for patients, who otherwise might be left to start anew in finding help at each phase of care.
The navigators “see the whole picture. They see the whole journey the patient takes, from pre-diagnosis all the way through diagnosis care out through survival,” Ms. Gentry said.
Gaining a special Medicare payment for these kinds of services will elevate this work, she said.
Many newer drugs can target specific mechanisms and proteins of cancer. Often, oncology treatment involves testing to find out if mutations are allowing the cancer cells to evade a patient’s immune system.
Checking these biomarkers takes time, however. Patients sometimes become frustrated because they are anxious to begin treatment. Patients may receive inaccurate information from friends or family who went through treatment previously. Navigators can provide knowledge on the current state of care for a patient’s disease, helping them better manage anxieties.
“You have to explain to them that things have changed since the guy you drink coffee with was diagnosed with cancer, and there may be a drug that could target that,” Ms. Gentry said.
Potential Challenges
Initial uptake of the new PIN codes may be slow going, however, as clinicians and health systems may already use well-established codes. These include CCM and principal care management services, which may pay higher rates, Mullangi said.
“There might be sensitivity around not wanting to cannibalize existing programs with a new program,” Dr. Mullangi said.
In addition, many patients will have a copay for the services of principal illness navigators, Dr. Mullangi said.
While many patients have additional insurance that would cover the service, not all do. People with traditional Medicare coverage can sometimes pay 20% of the cost of some medical services.
“I think that may give patients pause, particularly if they’re already feeling the financial burden of a cancer treatment journey,” Dr. Mullangi said.
Pay rates for PIN services involve calculations of regional price differences, which are posted publicly by CMS, and potential added fees for services provided by hospital-affiliated organizations.
Consider payments for code G0023, covering 60 minutes of principal navigation services provided in a single month.
A set reimbursement for patients cared for in independent medical practices exists, with variation for local costs. Medicare’s non-facility price for G0023 would be $102.41 in some parts of Silicon Valley in California, including San Jose. In Arkansas, where costs are lower, reimbursement would be $73.14 for this same service.
Patients who get services covered by code G0023 in independent medical practices would have monthly copays of about $15-$20, depending on where they live.
The tab for patients tends to be higher for these same services if delivered through a medical practice owned by a hospital, as this would trigger the addition of facility fees to the payments made to cover the services. Facility fees are difficult for the public to ascertain before getting a treatment or service.
Dr. Mullangi and Ms. Gentry reported no relevant financial disclosures outside of their employers.
A version of this article first appeared on Medscape.com.
In a move that acknowledges the gauntlet the US health system poses for people facing serious and fatal illnesses, Medicare will pay for a new class of workers to help patients manage treatments for conditions like cancer and heart failure.
The 2024 Medicare physician fee schedule includes new billing codes, including G0023, to pay for 60 minutes a month of care coordination by certified or trained auxiliary personnel working under the direction of a clinician.
A diagnosis of cancer or another serious illness takes a toll beyond the physical effects of the disease. Patients often scramble to make adjustments in family and work schedules to manage treatment, said Samyukta Mullangi, MD, MBA, medical director of oncology at Thyme Care, a Nashville, Tennessee–based firm that provides navigation and coordination services to oncology practices and insurers.
“It just really does create a bit of a pressure cooker for patients,” Dr. Mullangi told this news organization.
Medicare has for many years paid for medical professionals to help patients cope with the complexities of disease, such as chronic care management (CCM) provided by physicians, nurses, and physician assistants.
The new principal illness navigation (PIN) payments are intended to pay for work that to date typically has been done by people without medical degrees, including those involved in peer support networks and community health programs. The US Centers for Medicare and Medicaid Services(CMS) expects these navigators will undergo training and work under the supervision of clinicians.
The new navigators may coordinate care transitions between medical settings, follow up with patients after emergency department (ED) visits, or communicate with skilled nursing facilities regarding the psychosocial needs and functional deficits of a patient, among other functions.
CMS expects the new navigators may:
- Conduct assessments to understand a patient’s life story, strengths, needs, goals, preferences, and desired outcomes, including understanding cultural and linguistic factors.
- Provide support to accomplish the clinician’s treatment plan.
- Coordinate the receipt of needed services from healthcare facilities, home- and community-based service providers, and caregivers.
Peers as Navigators
The new navigators can be former patients who have undergone similar treatments for serious diseases, CMS said. This approach sets the new program apart from other care management services Medicare already covers, program officials wrote in the 2024 physician fee schedule.
“For some conditions, patients are best able to engage with the healthcare system and access care if they have assistance from a single, dedicated individual who has ‘lived experience,’ ” according to the rule.
The agency has taken a broad initial approach in defining what kinds of illnesses a patient may have to qualify for services. Patients must have a serious condition that is expected to last at least 3 months, such as cancer, heart failure, or substance use disorder.
But those without a definitive diagnosis may also qualify to receive navigator services.
In the rule, CMS cited a case in which a CT scan identified a suspicious mass in a patient’s colon. A clinician might decide this person would benefit from navigation services due to the potential risks for an undiagnosed illness.
“Regardless of the definitive diagnosis of the mass, presence of a colonic mass for that patient may be a serious high-risk condition that could, for example, cause obstruction and lead the patient to present to the emergency department, as well as be potentially indicative of an underlying life-threatening illness such as colon cancer,” CMS wrote in the rule.
Navigators often start their work when cancer patients are screened and guide them through initial diagnosis, potential surgery, radiation, or chemotherapy, said Sharon Gentry, MSN, RN, a former nurse navigator who is now the editor in chief of the Journal of the Academy of Oncology Nurse & Patient Navigators.
The navigators are meant to be a trusted and continual presence for patients, who otherwise might be left to start anew in finding help at each phase of care.
The navigators “see the whole picture. They see the whole journey the patient takes, from pre-diagnosis all the way through diagnosis care out through survival,” Ms. Gentry said.
Gaining a special Medicare payment for these kinds of services will elevate this work, she said.
Many newer drugs can target specific mechanisms and proteins of cancer. Often, oncology treatment involves testing to find out if mutations are allowing the cancer cells to evade a patient’s immune system.
Checking these biomarkers takes time, however. Patients sometimes become frustrated because they are anxious to begin treatment. Patients may receive inaccurate information from friends or family who went through treatment previously. Navigators can provide knowledge on the current state of care for a patient’s disease, helping them better manage anxieties.
“You have to explain to them that things have changed since the guy you drink coffee with was diagnosed with cancer, and there may be a drug that could target that,” Ms. Gentry said.
Potential Challenges
Initial uptake of the new PIN codes may be slow going, however, as clinicians and health systems may already use well-established codes. These include CCM and principal care management services, which may pay higher rates, Mullangi said.
“There might be sensitivity around not wanting to cannibalize existing programs with a new program,” Dr. Mullangi said.
In addition, many patients will have a copay for the services of principal illness navigators, Dr. Mullangi said.
While many patients have additional insurance that would cover the service, not all do. People with traditional Medicare coverage can sometimes pay 20% of the cost of some medical services.
“I think that may give patients pause, particularly if they’re already feeling the financial burden of a cancer treatment journey,” Dr. Mullangi said.
Pay rates for PIN services involve calculations of regional price differences, which are posted publicly by CMS, and potential added fees for services provided by hospital-affiliated organizations.
Consider payments for code G0023, covering 60 minutes of principal navigation services provided in a single month.
A set reimbursement for patients cared for in independent medical practices exists, with variation for local costs. Medicare’s non-facility price for G0023 would be $102.41 in some parts of Silicon Valley in California, including San Jose. In Arkansas, where costs are lower, reimbursement would be $73.14 for this same service.
Patients who get services covered by code G0023 in independent medical practices would have monthly copays of about $15-$20, depending on where they live.
The tab for patients tends to be higher for these same services if delivered through a medical practice owned by a hospital, as this would trigger the addition of facility fees to the payments made to cover the services. Facility fees are difficult for the public to ascertain before getting a treatment or service.
Dr. Mullangi and Ms. Gentry reported no relevant financial disclosures outside of their employers.
A version of this article first appeared on Medscape.com.

Special Report II: Tackling Burnout
Last month, we introduced the epidemic of burnout and the adverse consequences for both our vascular surgery patients and ourselves. Today we will outline a framework for addressing these issues. The foundation of this framework is informed by the social and neurosciences.
From the perspective of the social scientist: Christina Maslach, the originator of the widely used Maslach Burnout Inventory, theorized that burnout arises from a chronic mismatch between people and their work setting in some or all of the following domains: Workload (too much, wrong kind); control (lack of autonomy, or insufficient control over resources); reward (insufficient financial or social rewards commensurate with achievements); community (loss of positive connection with others); fairness (lack of perceived fairness, inequity of work, pay, or promotion); and values (conflict of personal and organizational values). The reality of practicing medicine in today’s business milieu – of achieving service efficiencies by meeting performance targets – brings many of these mismatches into sharp focus.
From the perspective of the neuroscientist: Recent advances, including functional MRI, have demonstrated that the human brain is hard wired for compassion. Compassion is the deep feeling that arises when confronted with another’s suffering, coupled with a strong desire to alleviate that suffering. There are at least two neural pathways: one activated during empathy, having us experience another’s pain; and the other activated during compassion, resulting in our sense of reward. Thus, burnout is thought to occur when you know what your patient needs but you are unable to deliver it. Compassionate medical care is purposeful work, which promotes a sense of reward and mitigates burnout.
Because burnout affects all caregivers (anyone who touches the patient), a successful program addressing workforce well-being must be comprehensive and organization wide, similar to successful patient safety, CPI [continuous process improvement] and LEAN [Six Sigma] initiatives.
There are no shortcuts. Creating a culture of compassionate, collaborative care requires an understanding of the interrelationships between the individual provider, the unit or team, and organizational leadership.
1) The individual provider: There is evidence to support the use of programs that build personal resilience. A recently published meta-analysis by West and colleagues concluded that while no specific physician burnout intervention has been shown to be better than other types of interventions, mindfulness, stress management, and small-group discussions can be effective approaches to reducing burnout scores. Strategies to build individual resilience, such as mindfulness and meditation, are easy to teach but place the burden for success on the individual. No amount of resilience can withstand an unsupportive or toxic workplace environment, so both individual and organizational strategies in combination are necessary.
2) The unit or team: Scheduling time for open and honest discussion of social and emotional issues that arise in caring for patients helps nourish caregiver to caregiver compassion. The Schwartz Center for Compassionate Healthcare is a national nonprofit leading the movement to bring compassion to every patient-caregiver interaction. More than 425 health care organization are Schwartz Center members and conduct Schwartz Rounds™ to bring doctors, nurses, and other caregivers together to discuss the human side of health care. (www.theschwartzcenter.org). Team member to team member support is essential for navigating the stressors of practice. With having lunch in front of your computer being the norm, and the disappearance of traditional spaces for colleagues to connect (for example, nurses’ lounge, physician dining rooms), the opportunity for caregivers to have a safe place to escape, a place to have their own humanity reaffirmed, a place to offer support to their peers, has been eliminated.
3) Organizational Leadership: Making compassion a core value, articulating it, and establishing metrics whereby it can be measured, is a good start. The barriers to a culture of compassion are related to our systems of care. There are burgeoning administrative and documentation tasks to be performed, and productivity expectations that turn our clinics and hospitals into assembly lines. No, we cannot expect the EMR [electronic medical records] to be eliminated, but workforce well-being cannot be sustainable in the context of inadequate resources. A culture of compassionate collaborative care requires programs and policies that are implemented by the organization itself. Examples of organization-wide initiatives that support workforce well-being and provider engagement include: screening for caregiver burnout, establishing policies for managing adverse events with an eye toward the second victim, and most importantly, supporting systems that preserve work control autonomy of physicians and nurses in clinical settings. The business sector has long recognized that workplace stress is a function of how demanding a person’s job is and how much control that person has over his or her responsibilities. The business community has also recognized that the experience of the worker (provider) drives the experience of the customer (patient). In a study of hospital compassionate practices and HCAHPS [the Hospital Consumer Assessment of Healthcare Providers and Systems], McClelland and Vogus reported that how well a hospital compassionately supports it employees and rewards compassionate acts is significantly and positively is associated with that hospital’s ratings and likelihood of patients recommending it.
How does the Society of Vascular Surgery, or any professional medical/nursing society for that matter, fit into this model?
We propose that the SVS find ways to empower their members to be agents for culture change within their own health care organizations. How might this be done:
- Teach organizational leadership skills, starting with the SVS Board of Directors, the presidential line, and the chairs of committees. Offer leadership courses at the Annual Meeting.
- Develop a community of caregivers committed to creating a compassionate collaborative culture. The SVS is a founding member of the Schwartz Center Healthcare Society Leadership Council, and you, as members of the SVS benefit from reduced registration at the Annual Compassion in Action Healthcare Conference, June 24-27, 2017 in Boston. (http://compassioninactionconference.org) This conference is designed to be highly experiential, using a hands-on “how to do it” model.
- The SVS should make improving the overall wellness of its members a specific goal and find specific metrics to monitor our progress towards this goal. Members can be provided with the tools to identify, monitor, and measure burnout and compassion. Each committee and council of the SVS can reexamine their objectives through the lens of reducing burnout and improving the wellness of vascular surgeons.
- Provide members with evidence-based programs that build personal resilience. This will not be a successful initiative unless our surgeons recognize and acknowledge the symptoms of burnout, and are willing to admit vulnerability. Without doing so, it is difficult to reach out for help.
- Redesign postgraduate resident and fellowship education. Standardizing clinical care may reduce variation and promote efficiency. However, when processes such as time-limited appointment scheduling, EMR templates, and protocols that drive physician-patient interactions are embedded in Resident and Fellowship education, the result may well be inflexibility in practice, reduced face time with patients, and interactions that lack compassion; all leading to burnout. Graduate Medical Education leaders must develop programs that support the learner’s ability to connect with patients and families, cultivate and role-model skills and behaviors that strengthen compassionate interactions, and strive to develop clinical practice models that increase Resident and Fellow work control autonomy.
The SVS should work proactively to optimize workload, fairness, and reward on a larger scale for its members as it relates to the EMR, reimbursement, and systems coverage. While we may be relatively small in size, as leaders, we are perfectly poised to address these larger, global issues. Perhaps working within the current system (i.e., PAC and APM task force) and considering innovative solutions at a national leadership scale, the SVS can direct real change!
Changing culture is not easy, nor quick, nor does it have an easy-to-follow blueprint. The first step is recognizing the need. The second is taking a leadership role. The third is thinking deeply about implementation.
*The authors extend their thanks and appreciation for the guidance, resources and support of Michael Goldberg, MD, scholar in residence, Schwartz Center for Compassionate Care, Boston and clinical professor of orthopedics at Seattle Children’s Hospital.
REFERENCES
1. J Managerial Psychol. (2007) 22:309-28
2. Annu Rev Neurosci. (2012) 35:1-23
3. Medicine. (2016) 44:583-5
4. J Health Organization Manag. (2015) 29:973-87
5. De Zulueta P Developing compassionate leadership in health care: an integrative review. J Healthcare Leadership. (2016) 8:1-10
6. Dolan ED, Morh D, Lempa M et al. Using a single item to measure burnout in primary care staff: A psychometry evaluation. J Gen Intern Med. (2015) 30:582-7
7. Karasek RA Job demands, job decision latitude, and mental strain: implications for job design. Administrative Sciences Quarterly (1979) 24: 285-308
8. Lee VS, Miller T, Daniels C, et al. Creating the exceptional patient experience in one academic health system. Acad Med. (2016) 91:338-44
9. Linzer M, Levine R, Meltzer D, et al. 10 bold steps to prevent burnout in general internal medicine. J Gen Intern Med. (2013) 29:18-20
10. Lown BA, Manning CF The Schwartz Center Rounds: Evaluation of an interdisciplinary approach to enhancing patient-centered communication, teamwork, and provider support. Acad Med. (2010) 85:1073-81
11. Lown BA, Muncer SJ, Chadwick R Can compassionate healthcare be measured? The Schwartz Center Compassionate Care Scale. Patient Education and Counseling (2015) 98:1005-10
12. Lown BA, McIntosh S, Gaines ME, et. al. Integrating compassionate collaborative care (“the Triple C”) into health professional education to advance the triple aim of health care. Acad Med (2016) 91:1-7
13. Lown BA A social neuroscience-informed model for teaching and practicing compassion in health care. Medical Education (2016) 50: 332-342
14. Maslach C, Schaufeli WG, Leiter MP Job burnout. Annu Rev Psychol (2001) 52:397-422
15. McClelland LE, Vogus TJ Compassion practices and HCAHPS: Does rewarding and supporting workplace compassion influence patient perceptions? HSR: Health Serv Res. (2014) 49:1670-83
16. Shanafelt TD, Noseworthy JH Executive leadership and physician well-being: Nine organizational strategies to promote engagement and reduce burnout. Mayo Clin Proc. (2016) 6:1-18
17. Shanafelt TD, Dyrbye LN, West CP Addressing physician burnout: the way forward. JAMA (2017) 317:901-2
18. Singer T, Klimecki OM Empathy and compassion Curr Biol. (2014) 24: R875-8
19. West CP, Dyrbye LN, Satele DV et. al. Concurrent validity of single-item measures of emotional exhaustion and depersonalization in burnout assessment. J Gen Intern Med. (2012) 27:1445-52
20. West CP, Dyrbye LN, Erwin PJ, et al. Interventions to address and reduce physician burnout: a systematic review and meta-analysis. Lancet. (2016) 388:2272-81
21. Wuest TK, Goldberg MJ, Kelly JD Clinical faceoff: Physician burnout-Fact, fantasy, or the fourth component of the triple aim? Clin Orthop Relat Res. (2016) doi: 10.1007/5-11999-016-5193-5
Last month, we introduced the epidemic of burnout and the adverse consequences for both our vascular surgery patients and ourselves. Today we will outline a framework for addressing these issues. The foundation of this framework is informed by the social and neurosciences.
From the perspective of the social scientist: Christina Maslach, the originator of the widely used Maslach Burnout Inventory, theorized that burnout arises from a chronic mismatch between people and their work setting in some or all of the following domains: Workload (too much, wrong kind); control (lack of autonomy, or insufficient control over resources); reward (insufficient financial or social rewards commensurate with achievements); community (loss of positive connection with others); fairness (lack of perceived fairness, inequity of work, pay, or promotion); and values (conflict of personal and organizational values). The reality of practicing medicine in today’s business milieu – of achieving service efficiencies by meeting performance targets – brings many of these mismatches into sharp focus.
From the perspective of the neuroscientist: Recent advances, including functional MRI, have demonstrated that the human brain is hard wired for compassion. Compassion is the deep feeling that arises when confronted with another’s suffering, coupled with a strong desire to alleviate that suffering. There are at least two neural pathways: one activated during empathy, having us experience another’s pain; and the other activated during compassion, resulting in our sense of reward. Thus, burnout is thought to occur when you know what your patient needs but you are unable to deliver it. Compassionate medical care is purposeful work, which promotes a sense of reward and mitigates burnout.
Because burnout affects all caregivers (anyone who touches the patient), a successful program addressing workforce well-being must be comprehensive and organization wide, similar to successful patient safety, CPI [continuous process improvement] and LEAN [Six Sigma] initiatives.
There are no shortcuts. Creating a culture of compassionate, collaborative care requires an understanding of the interrelationships between the individual provider, the unit or team, and organizational leadership.
1) The individual provider: There is evidence to support the use of programs that build personal resilience. A recently published meta-analysis by West and colleagues concluded that while no specific physician burnout intervention has been shown to be better than other types of interventions, mindfulness, stress management, and small-group discussions can be effective approaches to reducing burnout scores. Strategies to build individual resilience, such as mindfulness and meditation, are easy to teach but place the burden for success on the individual. No amount of resilience can withstand an unsupportive or toxic workplace environment, so both individual and organizational strategies in combination are necessary.
2) The unit or team: Scheduling time for open and honest discussion of social and emotional issues that arise in caring for patients helps nourish caregiver to caregiver compassion. The Schwartz Center for Compassionate Healthcare is a national nonprofit leading the movement to bring compassion to every patient-caregiver interaction. More than 425 health care organization are Schwartz Center members and conduct Schwartz Rounds™ to bring doctors, nurses, and other caregivers together to discuss the human side of health care. (www.theschwartzcenter.org). Team member to team member support is essential for navigating the stressors of practice. With having lunch in front of your computer being the norm, and the disappearance of traditional spaces for colleagues to connect (for example, nurses’ lounge, physician dining rooms), the opportunity for caregivers to have a safe place to escape, a place to have their own humanity reaffirmed, a place to offer support to their peers, has been eliminated.
3) Organizational Leadership: Making compassion a core value, articulating it, and establishing metrics whereby it can be measured, is a good start. The barriers to a culture of compassion are related to our systems of care. There are burgeoning administrative and documentation tasks to be performed, and productivity expectations that turn our clinics and hospitals into assembly lines. No, we cannot expect the EMR [electronic medical records] to be eliminated, but workforce well-being cannot be sustainable in the context of inadequate resources. A culture of compassionate collaborative care requires programs and policies that are implemented by the organization itself. Examples of organization-wide initiatives that support workforce well-being and provider engagement include: screening for caregiver burnout, establishing policies for managing adverse events with an eye toward the second victim, and most importantly, supporting systems that preserve work control autonomy of physicians and nurses in clinical settings. The business sector has long recognized that workplace stress is a function of how demanding a person’s job is and how much control that person has over his or her responsibilities. The business community has also recognized that the experience of the worker (provider) drives the experience of the customer (patient). In a study of hospital compassionate practices and HCAHPS [the Hospital Consumer Assessment of Healthcare Providers and Systems], McClelland and Vogus reported that how well a hospital compassionately supports it employees and rewards compassionate acts is significantly and positively is associated with that hospital’s ratings and likelihood of patients recommending it.
How does the Society of Vascular Surgery, or any professional medical/nursing society for that matter, fit into this model?
We propose that the SVS find ways to empower their members to be agents for culture change within their own health care organizations. How might this be done:
- Teach organizational leadership skills, starting with the SVS Board of Directors, the presidential line, and the chairs of committees. Offer leadership courses at the Annual Meeting.
- Develop a community of caregivers committed to creating a compassionate collaborative culture. The SVS is a founding member of the Schwartz Center Healthcare Society Leadership Council, and you, as members of the SVS benefit from reduced registration at the Annual Compassion in Action Healthcare Conference, June 24-27, 2017 in Boston. (http://compassioninactionconference.org) This conference is designed to be highly experiential, using a hands-on “how to do it” model.
- The SVS should make improving the overall wellness of its members a specific goal and find specific metrics to monitor our progress towards this goal. Members can be provided with the tools to identify, monitor, and measure burnout and compassion. Each committee and council of the SVS can reexamine their objectives through the lens of reducing burnout and improving the wellness of vascular surgeons.
- Provide members with evidence-based programs that build personal resilience. This will not be a successful initiative unless our surgeons recognize and acknowledge the symptoms of burnout, and are willing to admit vulnerability. Without doing so, it is difficult to reach out for help.
- Redesign postgraduate resident and fellowship education. Standardizing clinical care may reduce variation and promote efficiency. However, when processes such as time-limited appointment scheduling, EMR templates, and protocols that drive physician-patient interactions are embedded in Resident and Fellowship education, the result may well be inflexibility in practice, reduced face time with patients, and interactions that lack compassion; all leading to burnout. Graduate Medical Education leaders must develop programs that support the learner’s ability to connect with patients and families, cultivate and role-model skills and behaviors that strengthen compassionate interactions, and strive to develop clinical practice models that increase Resident and Fellow work control autonomy.
The SVS should work proactively to optimize workload, fairness, and reward on a larger scale for its members as it relates to the EMR, reimbursement, and systems coverage. While we may be relatively small in size, as leaders, we are perfectly poised to address these larger, global issues. Perhaps working within the current system (i.e., PAC and APM task force) and considering innovative solutions at a national leadership scale, the SVS can direct real change!
Changing culture is not easy, nor quick, nor does it have an easy-to-follow blueprint. The first step is recognizing the need. The second is taking a leadership role. The third is thinking deeply about implementation.
*The authors extend their thanks and appreciation for the guidance, resources and support of Michael Goldberg, MD, scholar in residence, Schwartz Center for Compassionate Care, Boston and clinical professor of orthopedics at Seattle Children’s Hospital.
REFERENCES
1. J Managerial Psychol. (2007) 22:309-28
2. Annu Rev Neurosci. (2012) 35:1-23
3. Medicine. (2016) 44:583-5
4. J Health Organization Manag. (2015) 29:973-87
5. De Zulueta P Developing compassionate leadership in health care: an integrative review. J Healthcare Leadership. (2016) 8:1-10
6. Dolan ED, Morh D, Lempa M et al. Using a single item to measure burnout in primary care staff: A psychometry evaluation. J Gen Intern Med. (2015) 30:582-7
7. Karasek RA Job demands, job decision latitude, and mental strain: implications for job design. Administrative Sciences Quarterly (1979) 24: 285-308
8. Lee VS, Miller T, Daniels C, et al. Creating the exceptional patient experience in one academic health system. Acad Med. (2016) 91:338-44
9. Linzer M, Levine R, Meltzer D, et al. 10 bold steps to prevent burnout in general internal medicine. J Gen Intern Med. (2013) 29:18-20
10. Lown BA, Manning CF The Schwartz Center Rounds: Evaluation of an interdisciplinary approach to enhancing patient-centered communication, teamwork, and provider support. Acad Med. (2010) 85:1073-81
11. Lown BA, Muncer SJ, Chadwick R Can compassionate healthcare be measured? The Schwartz Center Compassionate Care Scale. Patient Education and Counseling (2015) 98:1005-10
12. Lown BA, McIntosh S, Gaines ME, et. al. Integrating compassionate collaborative care (“the Triple C”) into health professional education to advance the triple aim of health care. Acad Med (2016) 91:1-7
13. Lown BA A social neuroscience-informed model for teaching and practicing compassion in health care. Medical Education (2016) 50: 332-342
14. Maslach C, Schaufeli WG, Leiter MP Job burnout. Annu Rev Psychol (2001) 52:397-422
15. McClelland LE, Vogus TJ Compassion practices and HCAHPS: Does rewarding and supporting workplace compassion influence patient perceptions? HSR: Health Serv Res. (2014) 49:1670-83
16. Shanafelt TD, Noseworthy JH Executive leadership and physician well-being: Nine organizational strategies to promote engagement and reduce burnout. Mayo Clin Proc. (2016) 6:1-18
17. Shanafelt TD, Dyrbye LN, West CP Addressing physician burnout: the way forward. JAMA (2017) 317:901-2
18. Singer T, Klimecki OM Empathy and compassion Curr Biol. (2014) 24: R875-8
19. West CP, Dyrbye LN, Satele DV et. al. Concurrent validity of single-item measures of emotional exhaustion and depersonalization in burnout assessment. J Gen Intern Med. (2012) 27:1445-52
20. West CP, Dyrbye LN, Erwin PJ, et al. Interventions to address and reduce physician burnout: a systematic review and meta-analysis. Lancet. (2016) 388:2272-81
21. Wuest TK, Goldberg MJ, Kelly JD Clinical faceoff: Physician burnout-Fact, fantasy, or the fourth component of the triple aim? Clin Orthop Relat Res. (2016) doi: 10.1007/5-11999-016-5193-5
Last month, we introduced the epidemic of burnout and the adverse consequences for both our vascular surgery patients and ourselves. Today we will outline a framework for addressing these issues. The foundation of this framework is informed by the social and neurosciences.
From the perspective of the social scientist: Christina Maslach, the originator of the widely used Maslach Burnout Inventory, theorized that burnout arises from a chronic mismatch between people and their work setting in some or all of the following domains: Workload (too much, wrong kind); control (lack of autonomy, or insufficient control over resources); reward (insufficient financial or social rewards commensurate with achievements); community (loss of positive connection with others); fairness (lack of perceived fairness, inequity of work, pay, or promotion); and values (conflict of personal and organizational values). The reality of practicing medicine in today’s business milieu – of achieving service efficiencies by meeting performance targets – brings many of these mismatches into sharp focus.
From the perspective of the neuroscientist: Recent advances, including functional MRI, have demonstrated that the human brain is hard wired for compassion. Compassion is the deep feeling that arises when confronted with another’s suffering, coupled with a strong desire to alleviate that suffering. There are at least two neural pathways: one activated during empathy, having us experience another’s pain; and the other activated during compassion, resulting in our sense of reward. Thus, burnout is thought to occur when you know what your patient needs but you are unable to deliver it. Compassionate medical care is purposeful work, which promotes a sense of reward and mitigates burnout.
Because burnout affects all caregivers (anyone who touches the patient), a successful program addressing workforce well-being must be comprehensive and organization wide, similar to successful patient safety, CPI [continuous process improvement] and LEAN [Six Sigma] initiatives.
There are no shortcuts. Creating a culture of compassionate, collaborative care requires an understanding of the interrelationships between the individual provider, the unit or team, and organizational leadership.
1) The individual provider: There is evidence to support the use of programs that build personal resilience. A recently published meta-analysis by West and colleagues concluded that while no specific physician burnout intervention has been shown to be better than other types of interventions, mindfulness, stress management, and small-group discussions can be effective approaches to reducing burnout scores. Strategies to build individual resilience, such as mindfulness and meditation, are easy to teach but place the burden for success on the individual. No amount of resilience can withstand an unsupportive or toxic workplace environment, so both individual and organizational strategies in combination are necessary.
2) The unit or team: Scheduling time for open and honest discussion of social and emotional issues that arise in caring for patients helps nourish caregiver to caregiver compassion. The Schwartz Center for Compassionate Healthcare is a national nonprofit leading the movement to bring compassion to every patient-caregiver interaction. More than 425 health care organization are Schwartz Center members and conduct Schwartz Rounds™ to bring doctors, nurses, and other caregivers together to discuss the human side of health care. (www.theschwartzcenter.org). Team member to team member support is essential for navigating the stressors of practice. With having lunch in front of your computer being the norm, and the disappearance of traditional spaces for colleagues to connect (for example, nurses’ lounge, physician dining rooms), the opportunity for caregivers to have a safe place to escape, a place to have their own humanity reaffirmed, a place to offer support to their peers, has been eliminated.
3) Organizational Leadership: Making compassion a core value, articulating it, and establishing metrics whereby it can be measured, is a good start. The barriers to a culture of compassion are related to our systems of care. There are burgeoning administrative and documentation tasks to be performed, and productivity expectations that turn our clinics and hospitals into assembly lines. No, we cannot expect the EMR [electronic medical records] to be eliminated, but workforce well-being cannot be sustainable in the context of inadequate resources. A culture of compassionate collaborative care requires programs and policies that are implemented by the organization itself. Examples of organization-wide initiatives that support workforce well-being and provider engagement include: screening for caregiver burnout, establishing policies for managing adverse events with an eye toward the second victim, and most importantly, supporting systems that preserve work control autonomy of physicians and nurses in clinical settings. The business sector has long recognized that workplace stress is a function of how demanding a person’s job is and how much control that person has over his or her responsibilities. The business community has also recognized that the experience of the worker (provider) drives the experience of the customer (patient). In a study of hospital compassionate practices and HCAHPS [the Hospital Consumer Assessment of Healthcare Providers and Systems], McClelland and Vogus reported that how well a hospital compassionately supports it employees and rewards compassionate acts is significantly and positively is associated with that hospital’s ratings and likelihood of patients recommending it.
How does the Society of Vascular Surgery, or any professional medical/nursing society for that matter, fit into this model?
We propose that the SVS find ways to empower their members to be agents for culture change within their own health care organizations. How might this be done:
- Teach organizational leadership skills, starting with the SVS Board of Directors, the presidential line, and the chairs of committees. Offer leadership courses at the Annual Meeting.
- Develop a community of caregivers committed to creating a compassionate collaborative culture. The SVS is a founding member of the Schwartz Center Healthcare Society Leadership Council, and you, as members of the SVS benefit from reduced registration at the Annual Compassion in Action Healthcare Conference, June 24-27, 2017 in Boston. (http://compassioninactionconference.org) This conference is designed to be highly experiential, using a hands-on “how to do it” model.
- The SVS should make improving the overall wellness of its members a specific goal and find specific metrics to monitor our progress towards this goal. Members can be provided with the tools to identify, monitor, and measure burnout and compassion. Each committee and council of the SVS can reexamine their objectives through the lens of reducing burnout and improving the wellness of vascular surgeons.
- Provide members with evidence-based programs that build personal resilience. This will not be a successful initiative unless our surgeons recognize and acknowledge the symptoms of burnout, and are willing to admit vulnerability. Without doing so, it is difficult to reach out for help.
- Redesign postgraduate resident and fellowship education. Standardizing clinical care may reduce variation and promote efficiency. However, when processes such as time-limited appointment scheduling, EMR templates, and protocols that drive physician-patient interactions are embedded in Resident and Fellowship education, the result may well be inflexibility in practice, reduced face time with patients, and interactions that lack compassion; all leading to burnout. Graduate Medical Education leaders must develop programs that support the learner’s ability to connect with patients and families, cultivate and role-model skills and behaviors that strengthen compassionate interactions, and strive to develop clinical practice models that increase Resident and Fellow work control autonomy.
The SVS should work proactively to optimize workload, fairness, and reward on a larger scale for its members as it relates to the EMR, reimbursement, and systems coverage. While we may be relatively small in size, as leaders, we are perfectly poised to address these larger, global issues. Perhaps working within the current system (i.e., PAC and APM task force) and considering innovative solutions at a national leadership scale, the SVS can direct real change!
Changing culture is not easy, nor quick, nor does it have an easy-to-follow blueprint. The first step is recognizing the need. The second is taking a leadership role. The third is thinking deeply about implementation.
*The authors extend their thanks and appreciation for the guidance, resources and support of Michael Goldberg, MD, scholar in residence, Schwartz Center for Compassionate Care, Boston and clinical professor of orthopedics at Seattle Children’s Hospital.
REFERENCES
1. J Managerial Psychol. (2007) 22:309-28
2. Annu Rev Neurosci. (2012) 35:1-23
3. Medicine. (2016) 44:583-5
4. J Health Organization Manag. (2015) 29:973-87
5. De Zulueta P Developing compassionate leadership in health care: an integrative review. J Healthcare Leadership. (2016) 8:1-10
6. Dolan ED, Morh D, Lempa M et al. Using a single item to measure burnout in primary care staff: A psychometry evaluation. J Gen Intern Med. (2015) 30:582-7
7. Karasek RA Job demands, job decision latitude, and mental strain: implications for job design. Administrative Sciences Quarterly (1979) 24: 285-308
8. Lee VS, Miller T, Daniels C, et al. Creating the exceptional patient experience in one academic health system. Acad Med. (2016) 91:338-44
9. Linzer M, Levine R, Meltzer D, et al. 10 bold steps to prevent burnout in general internal medicine. J Gen Intern Med. (2013) 29:18-20
10. Lown BA, Manning CF The Schwartz Center Rounds: Evaluation of an interdisciplinary approach to enhancing patient-centered communication, teamwork, and provider support. Acad Med. (2010) 85:1073-81
11. Lown BA, Muncer SJ, Chadwick R Can compassionate healthcare be measured? The Schwartz Center Compassionate Care Scale. Patient Education and Counseling (2015) 98:1005-10
12. Lown BA, McIntosh S, Gaines ME, et. al. Integrating compassionate collaborative care (“the Triple C”) into health professional education to advance the triple aim of health care. Acad Med (2016) 91:1-7
13. Lown BA A social neuroscience-informed model for teaching and practicing compassion in health care. Medical Education (2016) 50: 332-342
14. Maslach C, Schaufeli WG, Leiter MP Job burnout. Annu Rev Psychol (2001) 52:397-422
15. McClelland LE, Vogus TJ Compassion practices and HCAHPS: Does rewarding and supporting workplace compassion influence patient perceptions? HSR: Health Serv Res. (2014) 49:1670-83
16. Shanafelt TD, Noseworthy JH Executive leadership and physician well-being: Nine organizational strategies to promote engagement and reduce burnout. Mayo Clin Proc. (2016) 6:1-18
17. Shanafelt TD, Dyrbye LN, West CP Addressing physician burnout: the way forward. JAMA (2017) 317:901-2
18. Singer T, Klimecki OM Empathy and compassion Curr Biol. (2014) 24: R875-8
19. West CP, Dyrbye LN, Satele DV et. al. Concurrent validity of single-item measures of emotional exhaustion and depersonalization in burnout assessment. J Gen Intern Med. (2012) 27:1445-52
20. West CP, Dyrbye LN, Erwin PJ, et al. Interventions to address and reduce physician burnout: a systematic review and meta-analysis. Lancet. (2016) 388:2272-81
21. Wuest TK, Goldberg MJ, Kelly JD Clinical faceoff: Physician burnout-Fact, fantasy, or the fourth component of the triple aim? Clin Orthop Relat Res. (2016) doi: 10.1007/5-11999-016-5193-5
Ready for post-acute care?
The definition of “hospitalist,” according to the SHM website, is a clinician “dedicated to delivering comprehensive medical care to hospitalized patients.” For years, the hospital setting was the specialties’ identifier. But as hospitalists’ scope has expanded, and post-acute care (PAC) in the United States has grown, more hospitalists are extending their roles into this space.
PAC today is more than the traditional nursing home, according to Manoj K. Mathew, MD, SFHM, national medical director of Agilon Health in Los Angeles.
Many of those expanded settings Dr. Mathew describes emerged as a result of the Affordable Care Act. Since its enactment in 2010, the ACA has heightened providers’ focus on the “Triple Aim” of improving the patient experience (including quality and satisfaction), improving the health of populations, and reducing the per capita cost of healthcare.1 Vishal Kuchaculla, MD, New England regional post-acute medical director of Knoxville,Tenn.-based TeamHealth, says new service lines also developed as Medicare clamped down on long-term inpatient hospital stays by giving financial impetus to discharge patients as soon as possible.
“Over the last few years, there’s been a major shift from fee-for-service to risk-based payment models,” Dr. Kuchaculla says. “The government’s financial incentives are driving outcomes to improve performance initiatives.”
“Today, LTACHs can be used as substitutes for short-term acute care,” says Sean R. Muldoon, MD, MPH, FCCP, chief medical officer of Kindred Healthcare in Louisville, Ky., and former chair of SHM’s Post-Acute Care Committee. “This means that a patient can be directly admitted from their home to an LTACH. In fact, many hospice and home-care patients are referred from physicians’ offices without a preceding hospitalization.”

Hospitalists can fill a need

More hospitalists are working in PACs for a number of reasons. Dr. Mathew says PAC facilities and services have “typically lacked the clinical structure and processes to obtain the results that patients and payors expect.
“These deficits needed to be quickly remedied as patients discharged from hospitals have increased acuity and higher disease burdens,” he adds. “Hospitalists were the natural choice to fill roles requiring their expertise and experience.”
Dr. Muldoon considers the expanded scope of practice into PACs an additional layer to hospital medicine’s value proposition to the healthcare system.
“As experts in the management of inpatient populations, it’s natural for hospitalists to expand to other facilities with inpatient-like populations,” he says, noting SNFs are the most popular choice, with IRFs and LTACHs also being common places to work. Few hospitalists work in home care or hospice.
PAC settings are designed to help patients who are transitioning from an inpatient setting back to their home or other setting.
“Many patients go home after a SNF stay, while others will move to a nursing home or other longer-term care setting for the first time,” says Tiffany Radcliff, PhD, a health economist in the department of health policy and management at Texas A&M University School of Public Health in College Station. “With this in mind, hospitalists working in PAC have the opportunity to address each patient’s ongoing care needs and prepare them for their next setting. Hospitalists can manage medication or other care regimen changes that resulted from an inpatient stay, reinforce discharge instructions to the patient and their caregivers, and identify any other issues with continuing care that need to be addressed before discharge to the next care setting.”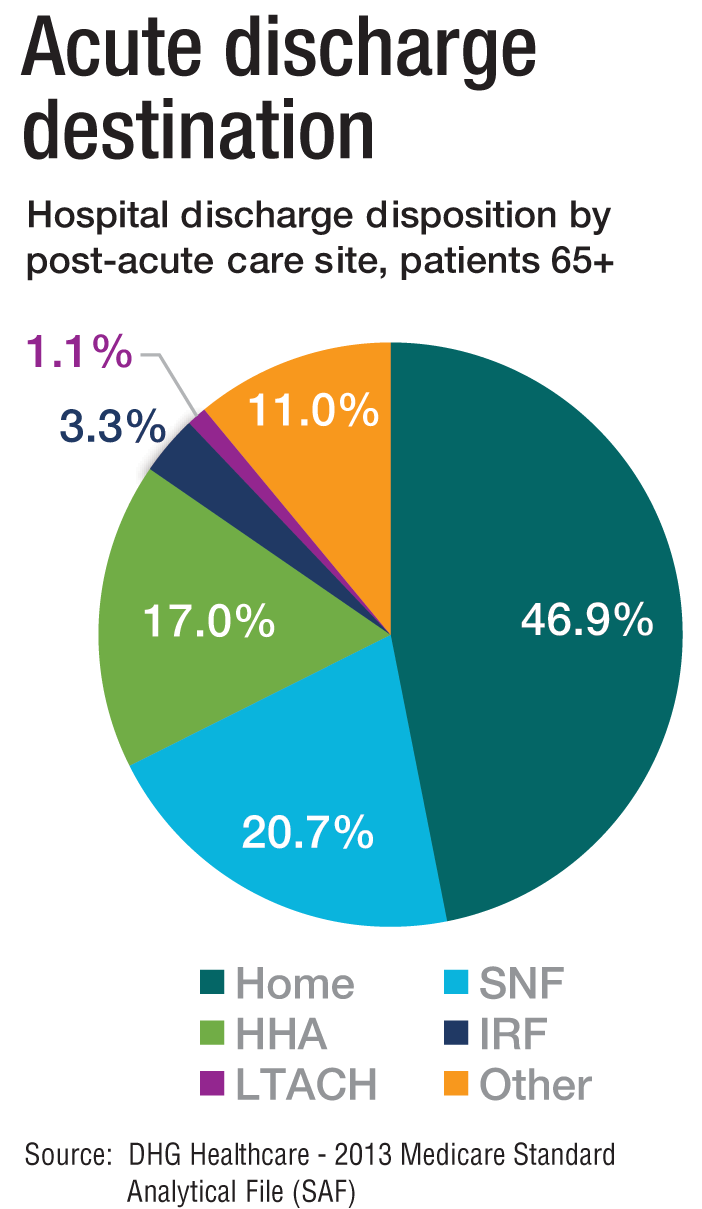
Transitioning Care
Even if a hospitalist is not employed at a PAC, it’s important that they know something about them.
“As patients are moved downstream earlier, hospitalists are being asked to help make a judgment regarding when and where an inpatient is transitioned,” Dr. Muldoon says. As organizations move toward becoming fully risk capable, it is necessary to develop referral networks of high-quality PAC providers to achieve the best clinical outcomes, reduce readmissions, and lower costs.2“Therefore, hospitalists should have a working knowledge of the different sites of service as well as some opinion on the suitability of available options in their community,” Dr. Muldoon says. “The hospitalist can also help to educate the hospitalized patient on what to expect at a PAC.”
If a patient is inappropriately prepared for the PAC setting, it could lead to incomplete management of their condition, which ultimately could lead to readmission.
“When hospitalists know how care is provided in a PAC setting, they are better able to ensure a smoother transition of care between settings,” says Tochi Iroku-Malize, MD, MPH, MBA, FAAFP, SFHM, chair of family medicine at Northwell Health in Long Island, N.Y. “This will ultimately prevent unnecessary readmissions.”
Further, the quality metrics that hospitals and thereby hospitalists are judged by no longer end at the hospital’s exit.
“The ownership of acute-care outcomes requires extending the accountability to outside of the institution’s four walls,” Dr. Mathew says. “The inpatient team needs to place great importance on the transition of care and the subsequent quality of that care when the patient is discharged.”
Robert W. Harrington Jr., MD, SFHM, chief medical officer of Plano, Texas–based Reliant Post-Acute Care Solutions and former SHM president, says the health system landscapes are pushing HM beyond the hospitals’ walls.
How PAC settings differ from hospitals
Practicing in PAC has some important nuances that hospitalists from short-term acute care need to get accustomed to, Dr. Muldoon says. Primarily, the diagnostic capabilities are much more limited, as is the presence of high-level staffing. Further, patients are less resilient to medication changes and interventions, so changes need to be done gradually.
“Hospitalists who try to practice acute-care medicine in a PAC setting may become frustrated by the length of time it takes to do a work-up, get a consultation, and respond to a patient’s change of condition,” Dr. Muldoon says. “Nonetheless, hospitalists can overcome this once recognizing this mind shift.”
According to Dr. Harrington, another challenge hospitalists may face is the inability of the hospital’s and PAC facility’s IT platforms to exchange electronic information.
“The major vendors on both sides need to figure out an interoperability strategy,” he says. “Currently, it often takes 1-3 days to receive a new patient’s discharge summary. The summary may consist of a stack of paper that takes significant time to sort through and requires the PAC facility to perform duplicate data entry. It’s a very highly inefficient process that opens up the doors to mistakes and errors of omission and commission that can result in bad patient outcomes.”
Arif Nazir, MD, CMD, FACP, AGSF, chief medical officer of Signature HealthCARE and president of SHC Medical Partners, both in Louisville, Ky., cites additional reasons the lack of seamless communication between a hospital and PAC facility is problematic. “I see physicians order laboratory tests and investigations that were already done in the hospital because they didn’t know they were already performed or never received the results,” he says. “Similarly, I see patients continue to take medications prescribed in the hospital long term even though they were only supposed to take them short term. I’ve also seen patients come to a PAC setting from a hospital without any formal understanding of their rehabilitative period and expectations for recovery.”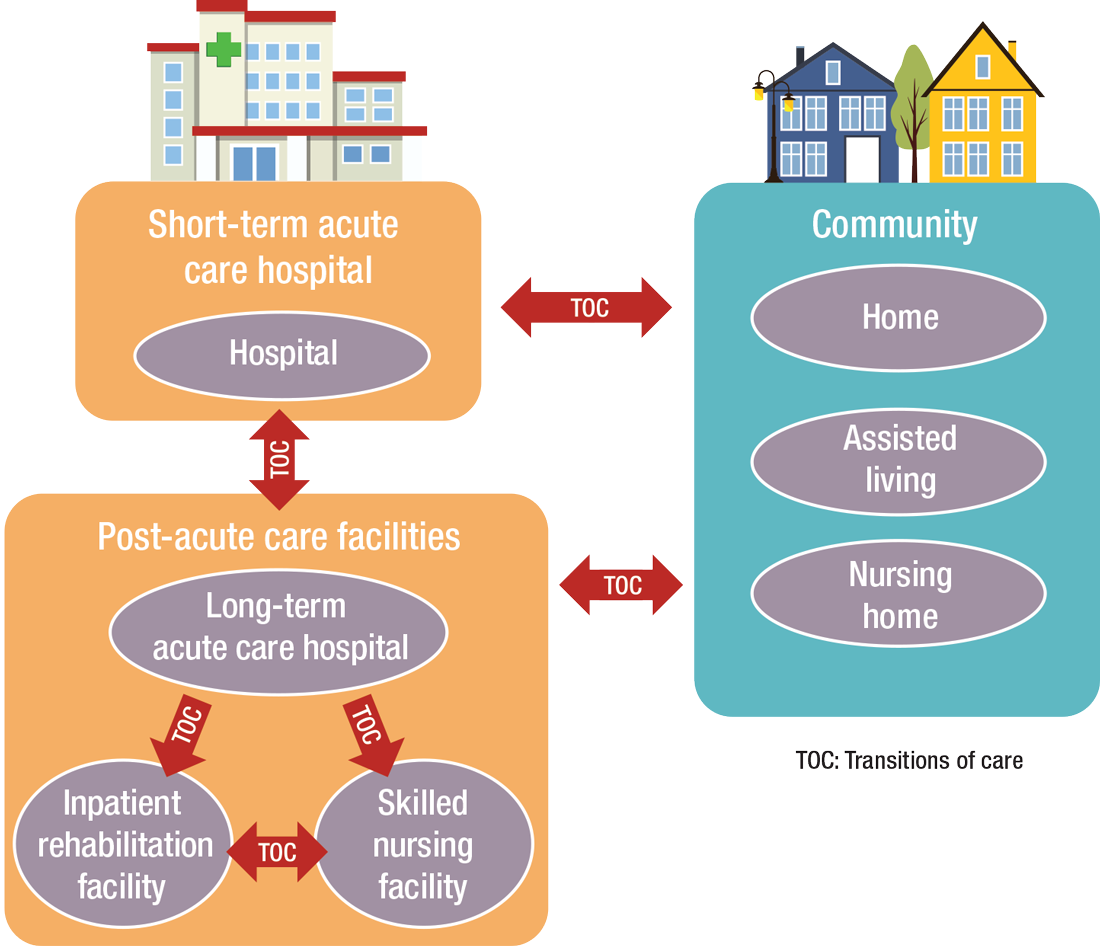
What’s ahead?
Looking to the future, Surafel Tsega, MD, clinical instructor at Mount Sinai Hospital in New York, says he thinks there will be a move toward greater collaboration among inpatient and PAC facilities, particularly in the discharge process, given that hospitals have an added incentive to ensure safe transitions because reimbursement from the Centers for Medicare & Medicaid Services is tied to readmissions and there are penalties for readmission. This involves more comprehensive planning regarding “warm handoffs” (e.g., real-time discussions with PAC providers about a patient’s hospital course and plan of care upon discharge), transferring of information, and so forth.
And while it can still be challenging to identify high-risk patients or determine the intensity and duration of their care, Dr. Mathew says risk-stratification tools and care pathways are continually being refined to maximize value with the limited resources available. In addition, with an increased emphasis on employing a team approach to care, there will be better integration of non-medical services to address the social determinants of health, which play significant roles in overall health and healing.
“Working with community-based organizations for this purpose will be a valuable tool for any of the population health–based initiatives,” he says.
Dr. Muldoon says he believes healthcare reform will increasingly view an inpatient admission as something to be avoided.
“If hospitalization can’t be avoided, then it should be shortened as much as possible,” he says. “This will shift inpatient care into LTACHs, SNFs, and IRFs. Hospitalists would be wise to follow patients into those settings as traditional inpatient census is reduced. This will take a few years, so hospitalists should start now in preparing for that downstream transition of individuals who were previously inpatients.”
The cost of care, and other PAC facts and figures
The amount of money that Medicare spends on post-acute care (PAC) has been increasing. In 2012, 12.6% of Medicare beneficiaries used some form of PAC, costing $62 billion.2 That amounts to the Centers for Medicare & Medicaid Services spending close to 25% of Medicare beneficiary expenses on PAC, a 133% increase from 2001 to 2012. Among the different types, $30.4 billion was spent on skilled nursing facilities (SNFs), $18.6 billion on home health, and $13.1 billion on long-term acute care (LTAC) and acute-care rehabilitation.2
It’s also been reported that after short-term acute-care hospitalization, about one in five Medicare beneficiaries requires continued specialized treatment in one of the three typical Medicare PAC settings: inpatient rehabilitation facilities (IRFs), LTAC hospitals, and SNFs.3
What’s more, hospital readmission nearly doubles the cost of an episode, so the financial implications for organizations operating in risk-bearing arrangements are significant. In 2013, 2,213 hospitals were charged $280 million in readmission penalties.2
References
1. The role of post-acute care in new care delivery models. American Hospital Association website. Available at: http://www.aha.org/research/reports/tw/15dec-tw-postacute.pdf. Accessed Nov. 7, 2016.
2. Post-acute care integration: Today and in the future. DHG Healthcare website. Available at: http://www2.dhgllp.com/res_pubs/HCG-Post-Acute-Care-Integration.pdf. Accessed Nov. 7, 2016.
3. Overview: Post-acute care transitions toolkit. Society for Hospital Medicine website. Available at: http://www.hospitalmedicine.org/Web/Quality___Innovation/Implementation_Toolkit/pact/Overview_PACT.aspx?hkey=dea3da3c-8620-46db-a00f-89f07f021958. Accessed Nov. 10, 2016.
The definition of “hospitalist,” according to the SHM website, is a clinician “dedicated to delivering comprehensive medical care to hospitalized patients.” For years, the hospital setting was the specialties’ identifier. But as hospitalists’ scope has expanded, and post-acute care (PAC) in the United States has grown, more hospitalists are extending their roles into this space.
PAC today is more than the traditional nursing home, according to Manoj K. Mathew, MD, SFHM, national medical director of Agilon Health in Los Angeles.
Many of those expanded settings Dr. Mathew describes emerged as a result of the Affordable Care Act. Since its enactment in 2010, the ACA has heightened providers’ focus on the “Triple Aim” of improving the patient experience (including quality and satisfaction), improving the health of populations, and reducing the per capita cost of healthcare.1 Vishal Kuchaculla, MD, New England regional post-acute medical director of Knoxville,Tenn.-based TeamHealth, says new service lines also developed as Medicare clamped down on long-term inpatient hospital stays by giving financial impetus to discharge patients as soon as possible.
“Over the last few years, there’s been a major shift from fee-for-service to risk-based payment models,” Dr. Kuchaculla says. “The government’s financial incentives are driving outcomes to improve performance initiatives.”
“Today, LTACHs can be used as substitutes for short-term acute care,” says Sean R. Muldoon, MD, MPH, FCCP, chief medical officer of Kindred Healthcare in Louisville, Ky., and former chair of SHM’s Post-Acute Care Committee. “This means that a patient can be directly admitted from their home to an LTACH. In fact, many hospice and home-care patients are referred from physicians’ offices without a preceding hospitalization.”

Hospitalists can fill a need

More hospitalists are working in PACs for a number of reasons. Dr. Mathew says PAC facilities and services have “typically lacked the clinical structure and processes to obtain the results that patients and payors expect.
“These deficits needed to be quickly remedied as patients discharged from hospitals have increased acuity and higher disease burdens,” he adds. “Hospitalists were the natural choice to fill roles requiring their expertise and experience.”
Dr. Muldoon considers the expanded scope of practice into PACs an additional layer to hospital medicine’s value proposition to the healthcare system.
“As experts in the management of inpatient populations, it’s natural for hospitalists to expand to other facilities with inpatient-like populations,” he says, noting SNFs are the most popular choice, with IRFs and LTACHs also being common places to work. Few hospitalists work in home care or hospice.
PAC settings are designed to help patients who are transitioning from an inpatient setting back to their home or other setting.
“Many patients go home after a SNF stay, while others will move to a nursing home or other longer-term care setting for the first time,” says Tiffany Radcliff, PhD, a health economist in the department of health policy and management at Texas A&M University School of Public Health in College Station. “With this in mind, hospitalists working in PAC have the opportunity to address each patient’s ongoing care needs and prepare them for their next setting. Hospitalists can manage medication or other care regimen changes that resulted from an inpatient stay, reinforce discharge instructions to the patient and their caregivers, and identify any other issues with continuing care that need to be addressed before discharge to the next care setting.”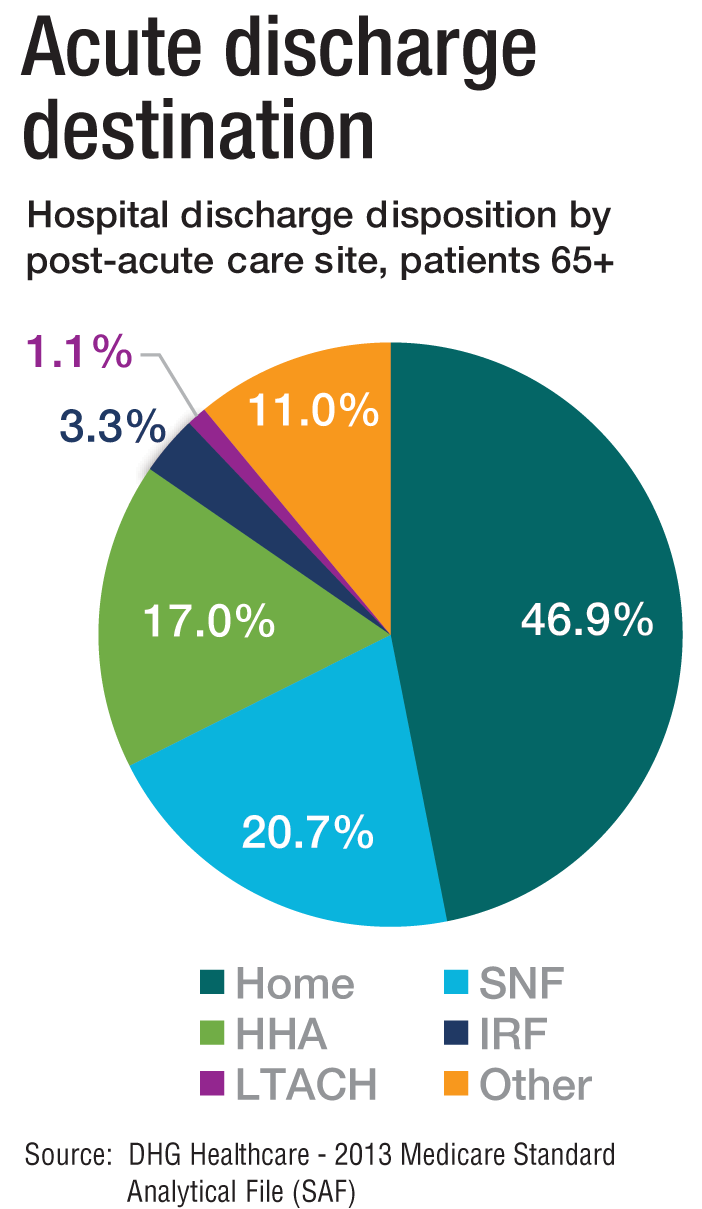
Transitioning Care
Even if a hospitalist is not employed at a PAC, it’s important that they know something about them.
“As patients are moved downstream earlier, hospitalists are being asked to help make a judgment regarding when and where an inpatient is transitioned,” Dr. Muldoon says. As organizations move toward becoming fully risk capable, it is necessary to develop referral networks of high-quality PAC providers to achieve the best clinical outcomes, reduce readmissions, and lower costs.2“Therefore, hospitalists should have a working knowledge of the different sites of service as well as some opinion on the suitability of available options in their community,” Dr. Muldoon says. “The hospitalist can also help to educate the hospitalized patient on what to expect at a PAC.”
If a patient is inappropriately prepared for the PAC setting, it could lead to incomplete management of their condition, which ultimately could lead to readmission.
“When hospitalists know how care is provided in a PAC setting, they are better able to ensure a smoother transition of care between settings,” says Tochi Iroku-Malize, MD, MPH, MBA, FAAFP, SFHM, chair of family medicine at Northwell Health in Long Island, N.Y. “This will ultimately prevent unnecessary readmissions.”
Further, the quality metrics that hospitals and thereby hospitalists are judged by no longer end at the hospital’s exit.
“The ownership of acute-care outcomes requires extending the accountability to outside of the institution’s four walls,” Dr. Mathew says. “The inpatient team needs to place great importance on the transition of care and the subsequent quality of that care when the patient is discharged.”
Robert W. Harrington Jr., MD, SFHM, chief medical officer of Plano, Texas–based Reliant Post-Acute Care Solutions and former SHM president, says the health system landscapes are pushing HM beyond the hospitals’ walls.
How PAC settings differ from hospitals
Practicing in PAC has some important nuances that hospitalists from short-term acute care need to get accustomed to, Dr. Muldoon says. Primarily, the diagnostic capabilities are much more limited, as is the presence of high-level staffing. Further, patients are less resilient to medication changes and interventions, so changes need to be done gradually.
“Hospitalists who try to practice acute-care medicine in a PAC setting may become frustrated by the length of time it takes to do a work-up, get a consultation, and respond to a patient’s change of condition,” Dr. Muldoon says. “Nonetheless, hospitalists can overcome this once recognizing this mind shift.”
According to Dr. Harrington, another challenge hospitalists may face is the inability of the hospital’s and PAC facility’s IT platforms to exchange electronic information.
“The major vendors on both sides need to figure out an interoperability strategy,” he says. “Currently, it often takes 1-3 days to receive a new patient’s discharge summary. The summary may consist of a stack of paper that takes significant time to sort through and requires the PAC facility to perform duplicate data entry. It’s a very highly inefficient process that opens up the doors to mistakes and errors of omission and commission that can result in bad patient outcomes.”
Arif Nazir, MD, CMD, FACP, AGSF, chief medical officer of Signature HealthCARE and president of SHC Medical Partners, both in Louisville, Ky., cites additional reasons the lack of seamless communication between a hospital and PAC facility is problematic. “I see physicians order laboratory tests and investigations that were already done in the hospital because they didn’t know they were already performed or never received the results,” he says. “Similarly, I see patients continue to take medications prescribed in the hospital long term even though they were only supposed to take them short term. I’ve also seen patients come to a PAC setting from a hospital without any formal understanding of their rehabilitative period and expectations for recovery.”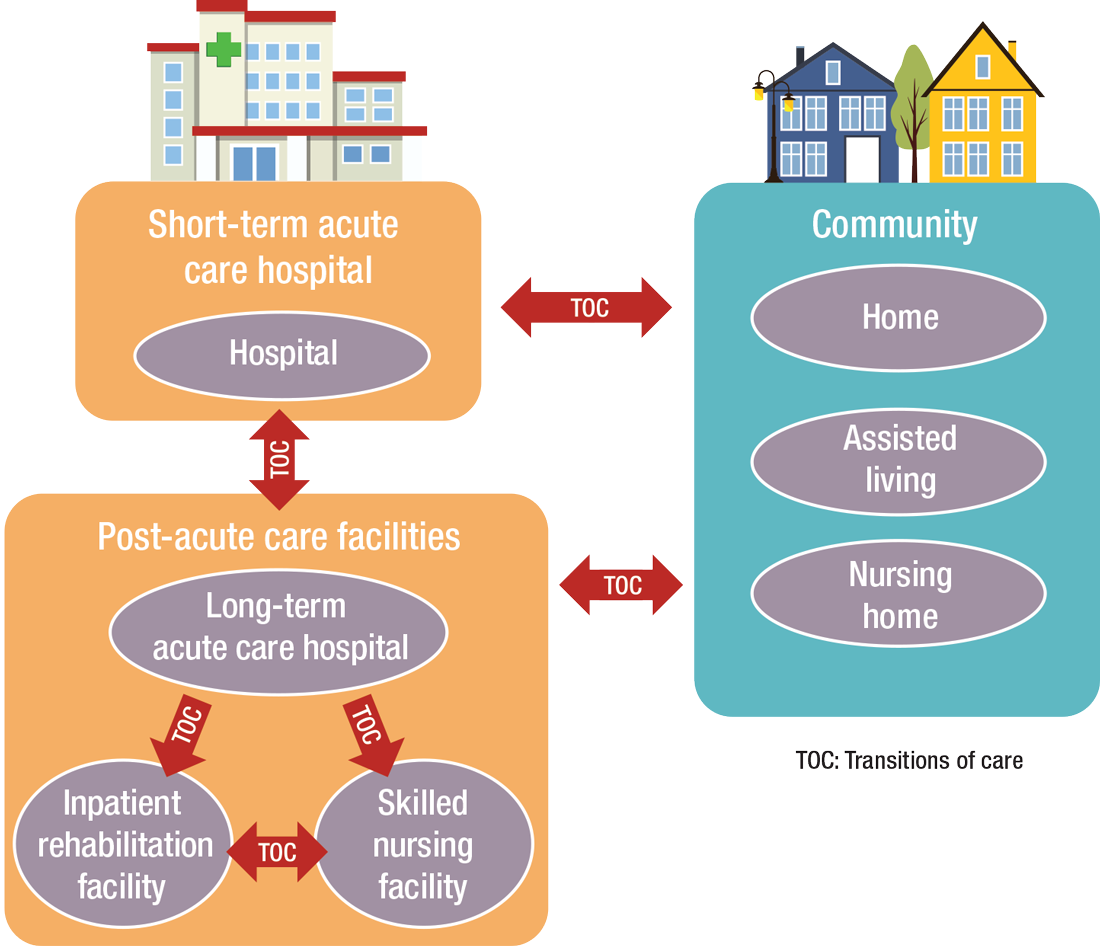
What’s ahead?
Looking to the future, Surafel Tsega, MD, clinical instructor at Mount Sinai Hospital in New York, says he thinks there will be a move toward greater collaboration among inpatient and PAC facilities, particularly in the discharge process, given that hospitals have an added incentive to ensure safe transitions because reimbursement from the Centers for Medicare & Medicaid Services is tied to readmissions and there are penalties for readmission. This involves more comprehensive planning regarding “warm handoffs” (e.g., real-time discussions with PAC providers about a patient’s hospital course and plan of care upon discharge), transferring of information, and so forth.
And while it can still be challenging to identify high-risk patients or determine the intensity and duration of their care, Dr. Mathew says risk-stratification tools and care pathways are continually being refined to maximize value with the limited resources available. In addition, with an increased emphasis on employing a team approach to care, there will be better integration of non-medical services to address the social determinants of health, which play significant roles in overall health and healing.
“Working with community-based organizations for this purpose will be a valuable tool for any of the population health–based initiatives,” he says.
Dr. Muldoon says he believes healthcare reform will increasingly view an inpatient admission as something to be avoided.
“If hospitalization can’t be avoided, then it should be shortened as much as possible,” he says. “This will shift inpatient care into LTACHs, SNFs, and IRFs. Hospitalists would be wise to follow patients into those settings as traditional inpatient census is reduced. This will take a few years, so hospitalists should start now in preparing for that downstream transition of individuals who were previously inpatients.”
The cost of care, and other PAC facts and figures
The amount of money that Medicare spends on post-acute care (PAC) has been increasing. In 2012, 12.6% of Medicare beneficiaries used some form of PAC, costing $62 billion.2 That amounts to the Centers for Medicare & Medicaid Services spending close to 25% of Medicare beneficiary expenses on PAC, a 133% increase from 2001 to 2012. Among the different types, $30.4 billion was spent on skilled nursing facilities (SNFs), $18.6 billion on home health, and $13.1 billion on long-term acute care (LTAC) and acute-care rehabilitation.2
It’s also been reported that after short-term acute-care hospitalization, about one in five Medicare beneficiaries requires continued specialized treatment in one of the three typical Medicare PAC settings: inpatient rehabilitation facilities (IRFs), LTAC hospitals, and SNFs.3
What’s more, hospital readmission nearly doubles the cost of an episode, so the financial implications for organizations operating in risk-bearing arrangements are significant. In 2013, 2,213 hospitals were charged $280 million in readmission penalties.2
References
1. The role of post-acute care in new care delivery models. American Hospital Association website. Available at: http://www.aha.org/research/reports/tw/15dec-tw-postacute.pdf. Accessed Nov. 7, 2016.
2. Post-acute care integration: Today and in the future. DHG Healthcare website. Available at: http://www2.dhgllp.com/res_pubs/HCG-Post-Acute-Care-Integration.pdf. Accessed Nov. 7, 2016.
3. Overview: Post-acute care transitions toolkit. Society for Hospital Medicine website. Available at: http://www.hospitalmedicine.org/Web/Quality___Innovation/Implementation_Toolkit/pact/Overview_PACT.aspx?hkey=dea3da3c-8620-46db-a00f-89f07f021958. Accessed Nov. 10, 2016.
The definition of “hospitalist,” according to the SHM website, is a clinician “dedicated to delivering comprehensive medical care to hospitalized patients.” For years, the hospital setting was the specialties’ identifier. But as hospitalists’ scope has expanded, and post-acute care (PAC) in the United States has grown, more hospitalists are extending their roles into this space.
PAC today is more than the traditional nursing home, according to Manoj K. Mathew, MD, SFHM, national medical director of Agilon Health in Los Angeles.
Many of those expanded settings Dr. Mathew describes emerged as a result of the Affordable Care Act. Since its enactment in 2010, the ACA has heightened providers’ focus on the “Triple Aim” of improving the patient experience (including quality and satisfaction), improving the health of populations, and reducing the per capita cost of healthcare.1 Vishal Kuchaculla, MD, New England regional post-acute medical director of Knoxville,Tenn.-based TeamHealth, says new service lines also developed as Medicare clamped down on long-term inpatient hospital stays by giving financial impetus to discharge patients as soon as possible.
“Over the last few years, there’s been a major shift from fee-for-service to risk-based payment models,” Dr. Kuchaculla says. “The government’s financial incentives are driving outcomes to improve performance initiatives.”
“Today, LTACHs can be used as substitutes for short-term acute care,” says Sean R. Muldoon, MD, MPH, FCCP, chief medical officer of Kindred Healthcare in Louisville, Ky., and former chair of SHM’s Post-Acute Care Committee. “This means that a patient can be directly admitted from their home to an LTACH. In fact, many hospice and home-care patients are referred from physicians’ offices without a preceding hospitalization.”

Hospitalists can fill a need

More hospitalists are working in PACs for a number of reasons. Dr. Mathew says PAC facilities and services have “typically lacked the clinical structure and processes to obtain the results that patients and payors expect.
“These deficits needed to be quickly remedied as patients discharged from hospitals have increased acuity and higher disease burdens,” he adds. “Hospitalists were the natural choice to fill roles requiring their expertise and experience.”
Dr. Muldoon considers the expanded scope of practice into PACs an additional layer to hospital medicine’s value proposition to the healthcare system.
“As experts in the management of inpatient populations, it’s natural for hospitalists to expand to other facilities with inpatient-like populations,” he says, noting SNFs are the most popular choice, with IRFs and LTACHs also being common places to work. Few hospitalists work in home care or hospice.
PAC settings are designed to help patients who are transitioning from an inpatient setting back to their home or other setting.
“Many patients go home after a SNF stay, while others will move to a nursing home or other longer-term care setting for the first time,” says Tiffany Radcliff, PhD, a health economist in the department of health policy and management at Texas A&M University School of Public Health in College Station. “With this in mind, hospitalists working in PAC have the opportunity to address each patient’s ongoing care needs and prepare them for their next setting. Hospitalists can manage medication or other care regimen changes that resulted from an inpatient stay, reinforce discharge instructions to the patient and their caregivers, and identify any other issues with continuing care that need to be addressed before discharge to the next care setting.”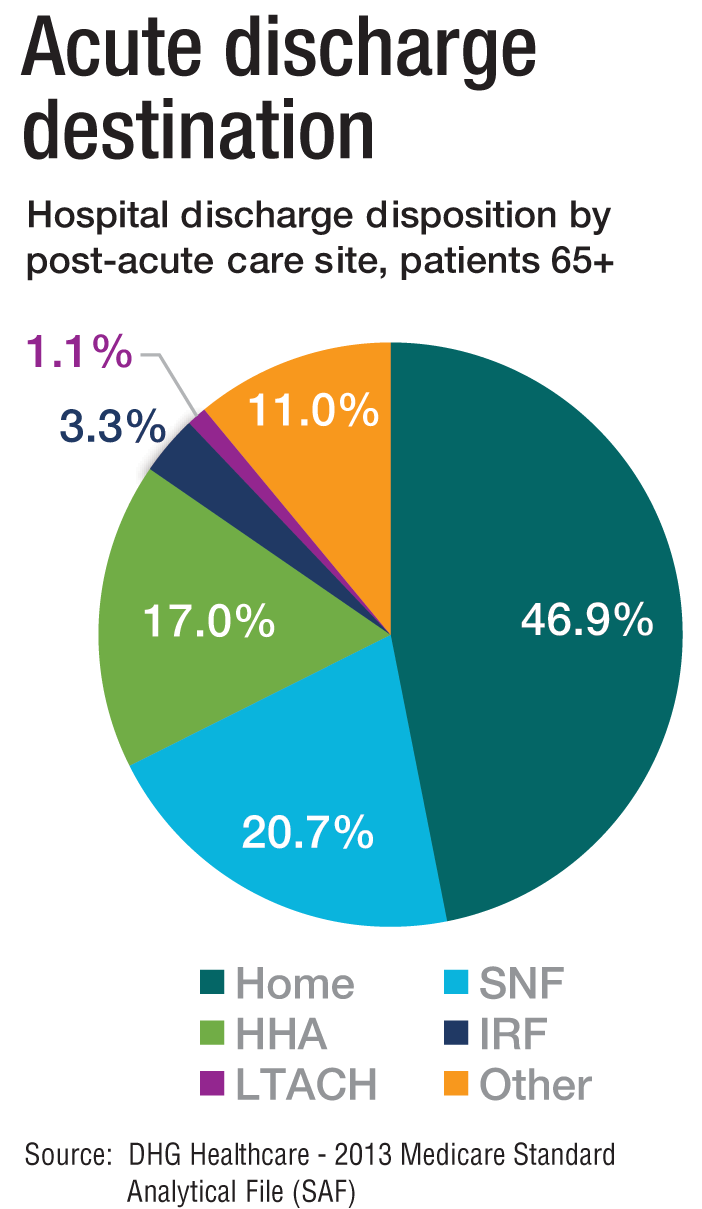
Transitioning Care
Even if a hospitalist is not employed at a PAC, it’s important that they know something about them.
“As patients are moved downstream earlier, hospitalists are being asked to help make a judgment regarding when and where an inpatient is transitioned,” Dr. Muldoon says. As organizations move toward becoming fully risk capable, it is necessary to develop referral networks of high-quality PAC providers to achieve the best clinical outcomes, reduce readmissions, and lower costs.2“Therefore, hospitalists should have a working knowledge of the different sites of service as well as some opinion on the suitability of available options in their community,” Dr. Muldoon says. “The hospitalist can also help to educate the hospitalized patient on what to expect at a PAC.”
If a patient is inappropriately prepared for the PAC setting, it could lead to incomplete management of their condition, which ultimately could lead to readmission.
“When hospitalists know how care is provided in a PAC setting, they are better able to ensure a smoother transition of care between settings,” says Tochi Iroku-Malize, MD, MPH, MBA, FAAFP, SFHM, chair of family medicine at Northwell Health in Long Island, N.Y. “This will ultimately prevent unnecessary readmissions.”
Further, the quality metrics that hospitals and thereby hospitalists are judged by no longer end at the hospital’s exit.
“The ownership of acute-care outcomes requires extending the accountability to outside of the institution’s four walls,” Dr. Mathew says. “The inpatient team needs to place great importance on the transition of care and the subsequent quality of that care when the patient is discharged.”
Robert W. Harrington Jr., MD, SFHM, chief medical officer of Plano, Texas–based Reliant Post-Acute Care Solutions and former SHM president, says the health system landscapes are pushing HM beyond the hospitals’ walls.
How PAC settings differ from hospitals
Practicing in PAC has some important nuances that hospitalists from short-term acute care need to get accustomed to, Dr. Muldoon says. Primarily, the diagnostic capabilities are much more limited, as is the presence of high-level staffing. Further, patients are less resilient to medication changes and interventions, so changes need to be done gradually.
“Hospitalists who try to practice acute-care medicine in a PAC setting may become frustrated by the length of time it takes to do a work-up, get a consultation, and respond to a patient’s change of condition,” Dr. Muldoon says. “Nonetheless, hospitalists can overcome this once recognizing this mind shift.”
According to Dr. Harrington, another challenge hospitalists may face is the inability of the hospital’s and PAC facility’s IT platforms to exchange electronic information.
“The major vendors on both sides need to figure out an interoperability strategy,” he says. “Currently, it often takes 1-3 days to receive a new patient’s discharge summary. The summary may consist of a stack of paper that takes significant time to sort through and requires the PAC facility to perform duplicate data entry. It’s a very highly inefficient process that opens up the doors to mistakes and errors of omission and commission that can result in bad patient outcomes.”
Arif Nazir, MD, CMD, FACP, AGSF, chief medical officer of Signature HealthCARE and president of SHC Medical Partners, both in Louisville, Ky., cites additional reasons the lack of seamless communication between a hospital and PAC facility is problematic. “I see physicians order laboratory tests and investigations that were already done in the hospital because they didn’t know they were already performed or never received the results,” he says. “Similarly, I see patients continue to take medications prescribed in the hospital long term even though they were only supposed to take them short term. I’ve also seen patients come to a PAC setting from a hospital without any formal understanding of their rehabilitative period and expectations for recovery.”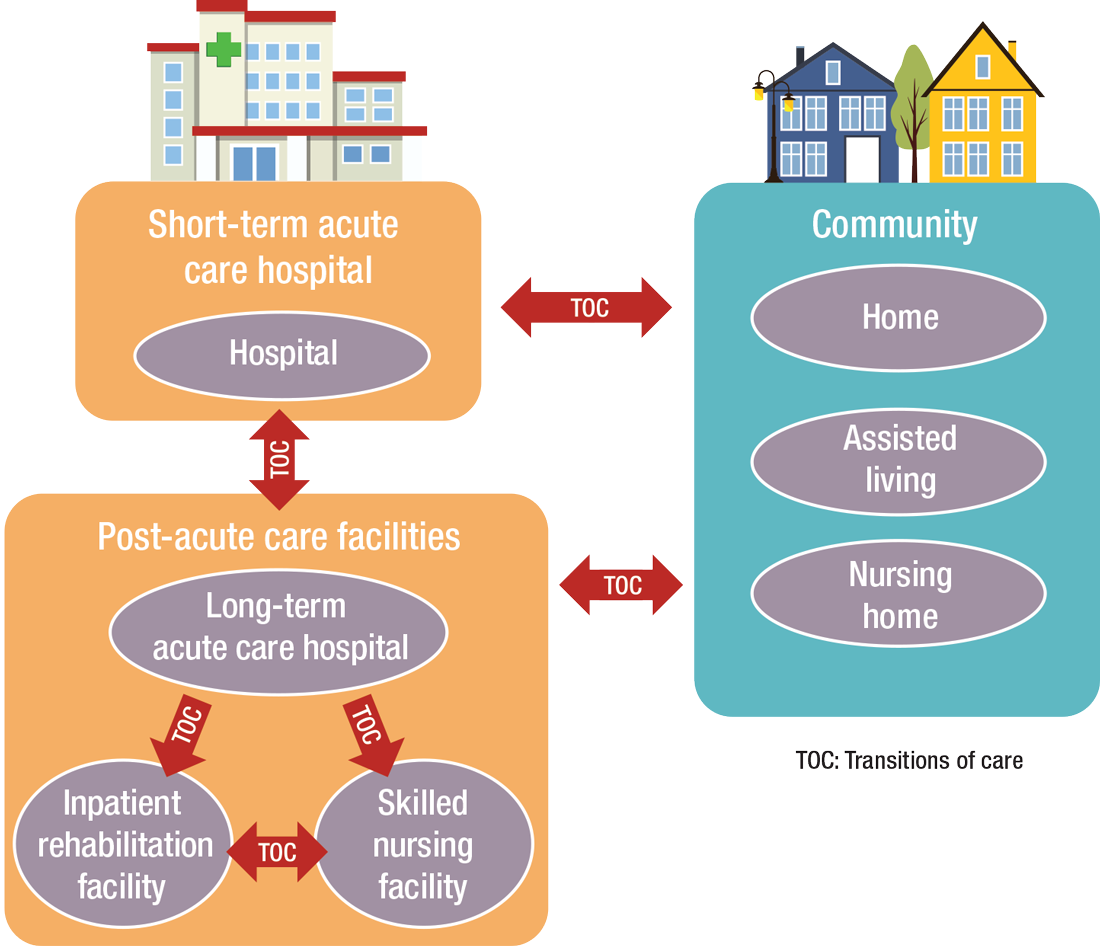
What’s ahead?
Looking to the future, Surafel Tsega, MD, clinical instructor at Mount Sinai Hospital in New York, says he thinks there will be a move toward greater collaboration among inpatient and PAC facilities, particularly in the discharge process, given that hospitals have an added incentive to ensure safe transitions because reimbursement from the Centers for Medicare & Medicaid Services is tied to readmissions and there are penalties for readmission. This involves more comprehensive planning regarding “warm handoffs” (e.g., real-time discussions with PAC providers about a patient’s hospital course and plan of care upon discharge), transferring of information, and so forth.
And while it can still be challenging to identify high-risk patients or determine the intensity and duration of their care, Dr. Mathew says risk-stratification tools and care pathways are continually being refined to maximize value with the limited resources available. In addition, with an increased emphasis on employing a team approach to care, there will be better integration of non-medical services to address the social determinants of health, which play significant roles in overall health and healing.
“Working with community-based organizations for this purpose will be a valuable tool for any of the population health–based initiatives,” he says.
Dr. Muldoon says he believes healthcare reform will increasingly view an inpatient admission as something to be avoided.
“If hospitalization can’t be avoided, then it should be shortened as much as possible,” he says. “This will shift inpatient care into LTACHs, SNFs, and IRFs. Hospitalists would be wise to follow patients into those settings as traditional inpatient census is reduced. This will take a few years, so hospitalists should start now in preparing for that downstream transition of individuals who were previously inpatients.”
The cost of care, and other PAC facts and figures
The amount of money that Medicare spends on post-acute care (PAC) has been increasing. In 2012, 12.6% of Medicare beneficiaries used some form of PAC, costing $62 billion.2 That amounts to the Centers for Medicare & Medicaid Services spending close to 25% of Medicare beneficiary expenses on PAC, a 133% increase from 2001 to 2012. Among the different types, $30.4 billion was spent on skilled nursing facilities (SNFs), $18.6 billion on home health, and $13.1 billion on long-term acute care (LTAC) and acute-care rehabilitation.2
It’s also been reported that after short-term acute-care hospitalization, about one in five Medicare beneficiaries requires continued specialized treatment in one of the three typical Medicare PAC settings: inpatient rehabilitation facilities (IRFs), LTAC hospitals, and SNFs.3
What’s more, hospital readmission nearly doubles the cost of an episode, so the financial implications for organizations operating in risk-bearing arrangements are significant. In 2013, 2,213 hospitals were charged $280 million in readmission penalties.2
References
1. The role of post-acute care in new care delivery models. American Hospital Association website. Available at: http://www.aha.org/research/reports/tw/15dec-tw-postacute.pdf. Accessed Nov. 7, 2016.
2. Post-acute care integration: Today and in the future. DHG Healthcare website. Available at: http://www2.dhgllp.com/res_pubs/HCG-Post-Acute-Care-Integration.pdf. Accessed Nov. 7, 2016.
3. Overview: Post-acute care transitions toolkit. Society for Hospital Medicine website. Available at: http://www.hospitalmedicine.org/Web/Quality___Innovation/Implementation_Toolkit/pact/Overview_PACT.aspx?hkey=dea3da3c-8620-46db-a00f-89f07f021958. Accessed Nov. 10, 2016.
What Dermatology Residents Need to Know About Joining Group Practices
What Dermatology Residents Need to Know About Joining Group Practices
Choosing your first job out of residency can be overwhelming. The things you need to consider go way beyond the job itself: things like geography, work/life balance, and practice focus (eg, skin cancer, cosmetics, medical dermatology, pediatrics) are all relatively independent factors from the specific practice you join. About 1 in 6 dermatologists change practices every year, with even higher rates for new graduates.1
Drawing from my 20 years of experience as a dermatologist (10 in academia and 10 in 3 different private group practice settings—one that was independently owned and 2 with private equity owners, of which I am one), I have seen firsthand what matters and what does not when it comes to joining a group practice, both in my own career and in watching the careers of many young dermatologists. I will do my best to summarize that experience into useful advice.
Important Factors to Consider When Choosing a Practice
As a second- or third-year resident, you likely are excited but nervous about leaping into practice. To approach it with confidence, allow me to outline certain factors that apply to all dermatology practices that you may consider joining as you start your career and beyond.
- Every Practice Owner Has to Prioritize Profit. Independent owners need to build the value of their main asset, academics need to fund research and teaching, and private equity owners need to drive returns for their investors. In other words, there are lots of negative situations in academic and independently owned groups, although private equity gets all the bad press.2-5 Nothing inherently makes one type of practice setting better; it depends on the specific organization. Owners do care about other things beyond just profit (eg, providing quality care, performing cutting-edge research), but when the rubber meets the road, if a practice is providing amazing quality care but losing money doing so, in a short time it won’t be providing any care at all.
- There Is No Free Money. Your long-term compensation will 100% be determined by how much revenue you generate minus the overhead. There is no magic fund to boost your pay long term, no matter how badly the practice needs or wants you. Be clear and even blunt: ask how the practice is going to profit from you. Ask how they plan to make back any signing bonus or guaranteed salary. If they are paying you a higher percentage of collections, ask them how they are able to pay more than competitors. If they say it is because they are more efficient with lower overhead, make sure that increased efficiency does not translate into less support.
- Percent of Collections Is Irrelevant. OK, perhaps not completely irrelevant, but it is one of the least important aspects in determining how much you will make or how happy you will be. Percent of collections is the percentage of the money that the practice actually collects that is paid out to you as compensation. For example, if your percentage of collections is 40%, that means that if the practice collects $1,000,000 for the care you deliver, you will be compensated $400,000. Read on to find out why it is not as important as it seems.
- Don’t Get Too Hung Up on the Details of the Contract. I have seen so many young dermatologists spend enormous amounts of time and money on attorneys and negotiating the fine points of the contract, but not a single one has ever said later that because of all that negotiation they were protected or treated well when things got contentious. What it comes down to is that, if the practice wants to treat you well, they will. If they want to treat you badly, no contract on earth can protect you from all the ways they can do so. And if you leave, no matter what the contract says, they can do whatever they want unless you are willing to spend hundreds of thousands of dollars to fight them in court. So review the contract with an attorney and know what it says, but don’t sweat every period and clause. It isn’t worth it.
- Your Day-to-Day Is Everything. The practice you join may be the best-run practice in the world in every way, except that the office you happen to be going to work in is the one office in the practice that has 2 providers who are jerks and everyone dreads coming to work every morning. There are so many other examples of ways one location can be a disaster even in a great practice—and unfortunately, even great locations can change. The best you can do is to make sure you know where you will be working and with whom. Go and visit the actual office and spend a day shadowing to feel what the vibe is.
What Really Matters
If factors like the percentage of collections you keep are not the big things, what are? The good and bad news is that there isn’t a single answer to this question. Rather, the fundamental question is whether the practice’s plan to maximize profit includes having satisfied, motivated, and engaged long-term providers. Obviously every group practice says this is fundamental to them, but often it isn’t true. Your real job is to find out whether or not it is. The second fundamental question is whether or not the leadership and members of a group practice are competent. It doesn’t matter if they want and intend to do everything right; if the practice is not competent at getting it done, your life practicing dermatology there is not going to be good.
As a dermatologist who has practiced for 20 years in multiple settings, here are some of the questions I would ask when assessing a practice setting I might consider joining. The practice should be able to easily answer all of these questions. If they won’t, can’t, or don’t—or if they answer but don’t give you clear, concrete responses—it is a huge red flag. It could be that they know you won’t like the answers or it could be that they don’t know the answers, but either reason indicates a big problem.
- How do the contracted rates compare to other practices? Pick 5 to 10 Current Procedural Terminology codes you expect to bill the most and ask the practice to tell you the contracted rates for each of those codes with their top 5 payers. Get the same information from all the practices you are considering joining and compare them. The variation between 2 practices in the same market can be as high as 30%. That means that for doing the same work at Practice A you could collect $800,000 and at Practice B in the same market you could collect more than $1,000,000. Getting 45% of your collection from Practice A is a losing proposition compared to getting 40% at Practice B.
- What is the collection rate? If the practice has great contracted rates but terrible revenue cycle management operations, the rates don’t matter. For example, maybe their contracted rate for a given code is $150, compared to another practice whose contracted rate is $125. But if their collection rate is only 60% and the other practice has a collection rate of 80%, they are only getting $90 while the practice with the lower contracted rate is getting $100.
- What billing and coding support does the practice offer? Are you expected to know and keep up with all the procedure codes, modifiers, etc, and use them correctly yourself or do they have professional coders who review every visit? Do they appeal every denied claim? Will you get reports on what charges get denied and why so that you can adjust your practices to avoid further denials?
- How do they train and assign medical assistants (MAs)? The single biggest determinant of your day-to-day productivity and happiness will be your MAs. Having 3 experienced, efficient MAs will allow you to see 50 patients per day with less effort and more fun than seeing 30 patients per day with 2 inexperienced, inefficient MAs. Seeing 50 patients per day at 40% of collections leads to you earning a lot more than seeing 30 per day at 50% of collections. Beyond the basic question of how many MAs you will have, also ask: Will you be expected to train them yourself, or does the practice have a formal training program? Who assesses how well they are performing? Will you have the same MAs every day? When more senior providers have MAs call off sick or leave the practice, will your MAs be pulled to cover their clinics? If that happens, will you be compensated in some way? Get the answers in writing.
- What is the “feel” of the office you will be working in? Ideally you will go and spend a day seeing patients in the office with one of the existing providers to get a sense of whether it’s a place you will be excited to come to every morning. Do you like the other providers? Is there someone who could act as a mentor for you? Does the staff seem happy? Will the physical layout and square footage accommodate the way you imagine practicing? Are the sociodemographics of the patients a fit for what you want?
- Who will be the office manager responsible for your personal practice? Some practices have an on-site manager for every location; others have district or regional managers who are split between multiple practices. Some have both. All can work, but having a competent, supportive office manager with whom you get along with whom and who “gets it” is crucial. You should ask about office manager turnover (high rates are bad, of course) and should ask to meet and interview the office manager who will be the boots on the ground for the practice in your location.
- How much demand for services is there and how are new patients scheduled? If the new hire gets all the hair loss, acne, and eczema cases and the established providers get all the skin cancer/Medicare patients, you are not going to have a balanced patient mix, and you are not going to meet productivity goals because you won’t be doing enough procedures. If there is not enough demand to fill your schedule, what kind of marketing support does the practice offer and what other approaches might they take? If you want to do cosmetics, how are they going to help you grow in that area? Are there other providers who don’t do cosmetics and will refer to you? Is there already someone in the practice who all the referrals go to? Is your percentage of collections based on total collections or on collections after the cost of injectables is deducted?
- What educational support does the practice offer? Do they have an annual meeting for networking and continuing medical education (CME)? If so, will you be expected to use your CME budget to pay to attend? Are there restrictions on what you can use your CME budget for? Is your CME budget considered part of your percentage of collections? Are there experts in the practice you can go to if you have a challenging case or difficult situation?
- Are physician associates and nurse practitioners a big part of the practice? Will you have the opportunity to increase your compensation by supervising them? If so, what is expected of supervising physicians and how are they compensated (flat fee vs percentage of collections vs another model)?
- What does the noncompete say? Obviously the shorter the time period and the smaller the distance, the better. For most practices, a noncompete is nonnegotiable. But there are some nuances to consider: Is the restricted distance from any location that the practice has in the market, or from any location(s) in which you personally have practiced, or from the primary location(s) in which you have practiced? If it is from the primary location(s), get details on how this term is defined: How much do you have to be at a location before it is considered primary? If you stop going to a location, after what period of time is it no longer considered a primary location? Additional questions to ask about noncompetes include: Is there a nonsolicitation clause for employees or patients? Will the practice include a buy-out clause in which you can pay them a set amount to waive the noncompete? Will they make the noncompete time dependent? In other words, if it is a terrible fit and you want to leave in the first year, there is very little justification for them to enforce a noncompete—but unless it is in your contract that they won’t enforce it if you leave before a certain amount of time, they will enforce it.
- Is there a path to having equity in the practice? In academia, this obviously is not a possibility. In independent practices it generally is referred to as an ownership stake or becoming a partner, and in private-equity groups it is literally referred to as “equity,” but they mean essentially the same thing for our purposes. It benefits the practice if you have equity because it gives you a reason to work to help increase the value of the practice. It benefits you to have equity because it means you have more input into decisions that will affect you (and the influence is proportional to how much equity you have) and the equity is an asset that can become very valuable.
The primary advice I have when it comes to being promised an opportunity to become an owner/partner in an independent group is to get the timing and conditions under which you can become an owner in the contract and strongly advocate for a clause that states that if you are not offered the opportunity as defined in the contract that you will be compensated. Also consider what happens if the current owner(s) sell the practice before you become an owner.
In private-equity groups, ask how many of the current providers have equity and ask how the equity is currently divided (what percentage is held by the private equity group, what percentage is held by the CEO and other executives, and what percentage is held by providers). The more equity held by the executive leadership and providers the better, as that means more people are on the same team of trying to increase the value of the practice. Find out how and when you will be able to buy in and try to get this in the contract or at least in writing. Also ask for a guarantee that your equity will not decrease in value. There are instances in which the practice loses value over time due to mismanagement, and the legal structure typically prioritizes the equity of the private-equity owners over the equity of providers. This is called an equity waterfall. Equity that providers were told was worth millions can literally be worth nothing.
One Key Thing You Need to Know
More important than the formal interviews and meetings that will provide you with answers to the questions outlined here, you need to know if you can trust the answers and you need to know the overall culture of the organization. Are they truly pro-provider, and do they believe that engaged and supported providers are the best route to long-term profit maximization? Or do they see providers primarily as replaceable adversaries who need to be placated and managed in order to minimize overhead? The only way to find out is to talk to providers already working there.
If you ask the practice for contact information for providers you can talk to, they likely will put you in touch with those who they know are going to talk about the practice in the best possible light. Be aware that providers may speak positively about a practice for a few different reasons other than that they are actually happy. Maybe the provider has an ownership stake in the practice and will benefit financially if you join. Keep in mind that, if a friend or colleague introduced you to the practice, they are almost certainly getting a substantial referral bonus if you join, so they may not be unbiased; however, if they are an actual friend, the last thing they want is for you to join and be unhappy in the practice because they didn’t tell the truth.
To learn about the experiences of others in your situation who have joined the practice, go to the website and look through the list of providers. Ideally, look for people who are in their first 3 years out of residency who have been there long enough to know the ins and outs but who still are considered newbies and almost certainly don’t have a meaningful ownership stake or strong allegiance to the practice. If it is a geographically widespread practice, focus on people in the region you will be in, but also talk to at least one person from a distant site.
Next, go to the American Academy of Dermatology’s website to find the email addresses for the providers you want to contact in the member directory. Send them an email explaining that you are thinking about joining the practice and that you would like to have an off-the-record phone conversation with them about their experiences. If they decline or don’t respond, it could be a red flag that likely means they don’t think they can speak positively about the practice. If they do agree to speak with you, you can reiterate at that time that the conversation is off the record and that you won’t relay your discussion to anyone at the practice.
Here is a sample email you can use to reach out to providers from a practice you are considering joining:
Subject: Advice on Joining [Practice Name]
Dear Dr. [Name],
I’m a dermatology resident considering joining [Practice Name] and came across your profile. Would you be willing to have a brief (5 to 10 minutes), off-the-record call about your experience? I’d value your perspective and won’t share our conversation with the practice. Thank you!
Best, [Your Name]
Start the conversation with open-ended questions and see where it goes. Some things to ask might be, are you glad you joined the practice? Was there anything that surprised you after you joined? Is there anything you wish you would have asked or known before you joined? I would recommend not asking specifically about their compensation, as it likely will be different from what you are being offered due to variations in location and current market situations.
Final Thoughts
There is no perfect dermatology practice, but the approach outlined here—rooted in first principles and real-world experience—will help you find one that is right for you. Ask tough questions, talk to other providers, and trust your instincts.
- Cwalina TB, Mazmudar RS, Bordeaux JS, et al. Dermatologist workforce mobility: recent trends and characteristics. JAMA Dermatol. 2022;158:323-325. doi:10.1001/jamadermatol.2021.5862
- Oscherwitz ME, Godinich BM, Patel RH, et al. Effects of private equity on dermatologic quality of patient care. J Eur Acad Dermatol Venereol. 2025;39:E100-E102. doi:10.1111/jdv.20191
- Walsh S, Seaton E. Private equity in dermatology: a cloud on the horizon of quality care? J Eur Acad Dermatol Venereol. 2025;39:9-10. doi:10.1111/jdv.20272
- Konda S, Patel S, Francis J. Private equity: the bad and the ugly. Dermatol Clin. 2023;41:597-610. doi:10.1016/j.det.2023.04.004
- Novice T, Portney D, Eshaq M. Dermatology resident perspectives on practice ownership structures and private equity-backed group practices. Clin Dermatol. 2020;38:296-302. doi:10.1016/j.clindermatol.2020.02.008
Choosing your first job out of residency can be overwhelming. The things you need to consider go way beyond the job itself: things like geography, work/life balance, and practice focus (eg, skin cancer, cosmetics, medical dermatology, pediatrics) are all relatively independent factors from the specific practice you join. About 1 in 6 dermatologists change practices every year, with even higher rates for new graduates.1
Drawing from my 20 years of experience as a dermatologist (10 in academia and 10 in 3 different private group practice settings—one that was independently owned and 2 with private equity owners, of which I am one), I have seen firsthand what matters and what does not when it comes to joining a group practice, both in my own career and in watching the careers of many young dermatologists. I will do my best to summarize that experience into useful advice.
Important Factors to Consider When Choosing a Practice
As a second- or third-year resident, you likely are excited but nervous about leaping into practice. To approach it with confidence, allow me to outline certain factors that apply to all dermatology practices that you may consider joining as you start your career and beyond.
- Every Practice Owner Has to Prioritize Profit. Independent owners need to build the value of their main asset, academics need to fund research and teaching, and private equity owners need to drive returns for their investors. In other words, there are lots of negative situations in academic and independently owned groups, although private equity gets all the bad press.2-5 Nothing inherently makes one type of practice setting better; it depends on the specific organization. Owners do care about other things beyond just profit (eg, providing quality care, performing cutting-edge research), but when the rubber meets the road, if a practice is providing amazing quality care but losing money doing so, in a short time it won’t be providing any care at all.
- There Is No Free Money. Your long-term compensation will 100% be determined by how much revenue you generate minus the overhead. There is no magic fund to boost your pay long term, no matter how badly the practice needs or wants you. Be clear and even blunt: ask how the practice is going to profit from you. Ask how they plan to make back any signing bonus or guaranteed salary. If they are paying you a higher percentage of collections, ask them how they are able to pay more than competitors. If they say it is because they are more efficient with lower overhead, make sure that increased efficiency does not translate into less support.
- Percent of Collections Is Irrelevant. OK, perhaps not completely irrelevant, but it is one of the least important aspects in determining how much you will make or how happy you will be. Percent of collections is the percentage of the money that the practice actually collects that is paid out to you as compensation. For example, if your percentage of collections is 40%, that means that if the practice collects $1,000,000 for the care you deliver, you will be compensated $400,000. Read on to find out why it is not as important as it seems.
- Don’t Get Too Hung Up on the Details of the Contract. I have seen so many young dermatologists spend enormous amounts of time and money on attorneys and negotiating the fine points of the contract, but not a single one has ever said later that because of all that negotiation they were protected or treated well when things got contentious. What it comes down to is that, if the practice wants to treat you well, they will. If they want to treat you badly, no contract on earth can protect you from all the ways they can do so. And if you leave, no matter what the contract says, they can do whatever they want unless you are willing to spend hundreds of thousands of dollars to fight them in court. So review the contract with an attorney and know what it says, but don’t sweat every period and clause. It isn’t worth it.
- Your Day-to-Day Is Everything. The practice you join may be the best-run practice in the world in every way, except that the office you happen to be going to work in is the one office in the practice that has 2 providers who are jerks and everyone dreads coming to work every morning. There are so many other examples of ways one location can be a disaster even in a great practice—and unfortunately, even great locations can change. The best you can do is to make sure you know where you will be working and with whom. Go and visit the actual office and spend a day shadowing to feel what the vibe is.
What Really Matters
If factors like the percentage of collections you keep are not the big things, what are? The good and bad news is that there isn’t a single answer to this question. Rather, the fundamental question is whether the practice’s plan to maximize profit includes having satisfied, motivated, and engaged long-term providers. Obviously every group practice says this is fundamental to them, but often it isn’t true. Your real job is to find out whether or not it is. The second fundamental question is whether or not the leadership and members of a group practice are competent. It doesn’t matter if they want and intend to do everything right; if the practice is not competent at getting it done, your life practicing dermatology there is not going to be good.
As a dermatologist who has practiced for 20 years in multiple settings, here are some of the questions I would ask when assessing a practice setting I might consider joining. The practice should be able to easily answer all of these questions. If they won’t, can’t, or don’t—or if they answer but don’t give you clear, concrete responses—it is a huge red flag. It could be that they know you won’t like the answers or it could be that they don’t know the answers, but either reason indicates a big problem.
- How do the contracted rates compare to other practices? Pick 5 to 10 Current Procedural Terminology codes you expect to bill the most and ask the practice to tell you the contracted rates for each of those codes with their top 5 payers. Get the same information from all the practices you are considering joining and compare them. The variation between 2 practices in the same market can be as high as 30%. That means that for doing the same work at Practice A you could collect $800,000 and at Practice B in the same market you could collect more than $1,000,000. Getting 45% of your collection from Practice A is a losing proposition compared to getting 40% at Practice B.
- What is the collection rate? If the practice has great contracted rates but terrible revenue cycle management operations, the rates don’t matter. For example, maybe their contracted rate for a given code is $150, compared to another practice whose contracted rate is $125. But if their collection rate is only 60% and the other practice has a collection rate of 80%, they are only getting $90 while the practice with the lower contracted rate is getting $100.
- What billing and coding support does the practice offer? Are you expected to know and keep up with all the procedure codes, modifiers, etc, and use them correctly yourself or do they have professional coders who review every visit? Do they appeal every denied claim? Will you get reports on what charges get denied and why so that you can adjust your practices to avoid further denials?
- How do they train and assign medical assistants (MAs)? The single biggest determinant of your day-to-day productivity and happiness will be your MAs. Having 3 experienced, efficient MAs will allow you to see 50 patients per day with less effort and more fun than seeing 30 patients per day with 2 inexperienced, inefficient MAs. Seeing 50 patients per day at 40% of collections leads to you earning a lot more than seeing 30 per day at 50% of collections. Beyond the basic question of how many MAs you will have, also ask: Will you be expected to train them yourself, or does the practice have a formal training program? Who assesses how well they are performing? Will you have the same MAs every day? When more senior providers have MAs call off sick or leave the practice, will your MAs be pulled to cover their clinics? If that happens, will you be compensated in some way? Get the answers in writing.
- What is the “feel” of the office you will be working in? Ideally you will go and spend a day seeing patients in the office with one of the existing providers to get a sense of whether it’s a place you will be excited to come to every morning. Do you like the other providers? Is there someone who could act as a mentor for you? Does the staff seem happy? Will the physical layout and square footage accommodate the way you imagine practicing? Are the sociodemographics of the patients a fit for what you want?
- Who will be the office manager responsible for your personal practice? Some practices have an on-site manager for every location; others have district or regional managers who are split between multiple practices. Some have both. All can work, but having a competent, supportive office manager with whom you get along with whom and who “gets it” is crucial. You should ask about office manager turnover (high rates are bad, of course) and should ask to meet and interview the office manager who will be the boots on the ground for the practice in your location.
- How much demand for services is there and how are new patients scheduled? If the new hire gets all the hair loss, acne, and eczema cases and the established providers get all the skin cancer/Medicare patients, you are not going to have a balanced patient mix, and you are not going to meet productivity goals because you won’t be doing enough procedures. If there is not enough demand to fill your schedule, what kind of marketing support does the practice offer and what other approaches might they take? If you want to do cosmetics, how are they going to help you grow in that area? Are there other providers who don’t do cosmetics and will refer to you? Is there already someone in the practice who all the referrals go to? Is your percentage of collections based on total collections or on collections after the cost of injectables is deducted?
- What educational support does the practice offer? Do they have an annual meeting for networking and continuing medical education (CME)? If so, will you be expected to use your CME budget to pay to attend? Are there restrictions on what you can use your CME budget for? Is your CME budget considered part of your percentage of collections? Are there experts in the practice you can go to if you have a challenging case or difficult situation?
- Are physician associates and nurse practitioners a big part of the practice? Will you have the opportunity to increase your compensation by supervising them? If so, what is expected of supervising physicians and how are they compensated (flat fee vs percentage of collections vs another model)?
- What does the noncompete say? Obviously the shorter the time period and the smaller the distance, the better. For most practices, a noncompete is nonnegotiable. But there are some nuances to consider: Is the restricted distance from any location that the practice has in the market, or from any location(s) in which you personally have practiced, or from the primary location(s) in which you have practiced? If it is from the primary location(s), get details on how this term is defined: How much do you have to be at a location before it is considered primary? If you stop going to a location, after what period of time is it no longer considered a primary location? Additional questions to ask about noncompetes include: Is there a nonsolicitation clause for employees or patients? Will the practice include a buy-out clause in which you can pay them a set amount to waive the noncompete? Will they make the noncompete time dependent? In other words, if it is a terrible fit and you want to leave in the first year, there is very little justification for them to enforce a noncompete—but unless it is in your contract that they won’t enforce it if you leave before a certain amount of time, they will enforce it.
- Is there a path to having equity in the practice? In academia, this obviously is not a possibility. In independent practices it generally is referred to as an ownership stake or becoming a partner, and in private-equity groups it is literally referred to as “equity,” but they mean essentially the same thing for our purposes. It benefits the practice if you have equity because it gives you a reason to work to help increase the value of the practice. It benefits you to have equity because it means you have more input into decisions that will affect you (and the influence is proportional to how much equity you have) and the equity is an asset that can become very valuable.
The primary advice I have when it comes to being promised an opportunity to become an owner/partner in an independent group is to get the timing and conditions under which you can become an owner in the contract and strongly advocate for a clause that states that if you are not offered the opportunity as defined in the contract that you will be compensated. Also consider what happens if the current owner(s) sell the practice before you become an owner.
In private-equity groups, ask how many of the current providers have equity and ask how the equity is currently divided (what percentage is held by the private equity group, what percentage is held by the CEO and other executives, and what percentage is held by providers). The more equity held by the executive leadership and providers the better, as that means more people are on the same team of trying to increase the value of the practice. Find out how and when you will be able to buy in and try to get this in the contract or at least in writing. Also ask for a guarantee that your equity will not decrease in value. There are instances in which the practice loses value over time due to mismanagement, and the legal structure typically prioritizes the equity of the private-equity owners over the equity of providers. This is called an equity waterfall. Equity that providers were told was worth millions can literally be worth nothing.
One Key Thing You Need to Know
More important than the formal interviews and meetings that will provide you with answers to the questions outlined here, you need to know if you can trust the answers and you need to know the overall culture of the organization. Are they truly pro-provider, and do they believe that engaged and supported providers are the best route to long-term profit maximization? Or do they see providers primarily as replaceable adversaries who need to be placated and managed in order to minimize overhead? The only way to find out is to talk to providers already working there.
If you ask the practice for contact information for providers you can talk to, they likely will put you in touch with those who they know are going to talk about the practice in the best possible light. Be aware that providers may speak positively about a practice for a few different reasons other than that they are actually happy. Maybe the provider has an ownership stake in the practice and will benefit financially if you join. Keep in mind that, if a friend or colleague introduced you to the practice, they are almost certainly getting a substantial referral bonus if you join, so they may not be unbiased; however, if they are an actual friend, the last thing they want is for you to join and be unhappy in the practice because they didn’t tell the truth.
To learn about the experiences of others in your situation who have joined the practice, go to the website and look through the list of providers. Ideally, look for people who are in their first 3 years out of residency who have been there long enough to know the ins and outs but who still are considered newbies and almost certainly don’t have a meaningful ownership stake or strong allegiance to the practice. If it is a geographically widespread practice, focus on people in the region you will be in, but also talk to at least one person from a distant site.
Next, go to the American Academy of Dermatology’s website to find the email addresses for the providers you want to contact in the member directory. Send them an email explaining that you are thinking about joining the practice and that you would like to have an off-the-record phone conversation with them about their experiences. If they decline or don’t respond, it could be a red flag that likely means they don’t think they can speak positively about the practice. If they do agree to speak with you, you can reiterate at that time that the conversation is off the record and that you won’t relay your discussion to anyone at the practice.
Here is a sample email you can use to reach out to providers from a practice you are considering joining:
Subject: Advice on Joining [Practice Name]
Dear Dr. [Name],
I’m a dermatology resident considering joining [Practice Name] and came across your profile. Would you be willing to have a brief (5 to 10 minutes), off-the-record call about your experience? I’d value your perspective and won’t share our conversation with the practice. Thank you!
Best, [Your Name]
Start the conversation with open-ended questions and see where it goes. Some things to ask might be, are you glad you joined the practice? Was there anything that surprised you after you joined? Is there anything you wish you would have asked or known before you joined? I would recommend not asking specifically about their compensation, as it likely will be different from what you are being offered due to variations in location and current market situations.
Final Thoughts
There is no perfect dermatology practice, but the approach outlined here—rooted in first principles and real-world experience—will help you find one that is right for you. Ask tough questions, talk to other providers, and trust your instincts.
Choosing your first job out of residency can be overwhelming. The things you need to consider go way beyond the job itself: things like geography, work/life balance, and practice focus (eg, skin cancer, cosmetics, medical dermatology, pediatrics) are all relatively independent factors from the specific practice you join. About 1 in 6 dermatologists change practices every year, with even higher rates for new graduates.1
Drawing from my 20 years of experience as a dermatologist (10 in academia and 10 in 3 different private group practice settings—one that was independently owned and 2 with private equity owners, of which I am one), I have seen firsthand what matters and what does not when it comes to joining a group practice, both in my own career and in watching the careers of many young dermatologists. I will do my best to summarize that experience into useful advice.
Important Factors to Consider When Choosing a Practice
As a second- or third-year resident, you likely are excited but nervous about leaping into practice. To approach it with confidence, allow me to outline certain factors that apply to all dermatology practices that you may consider joining as you start your career and beyond.
- Every Practice Owner Has to Prioritize Profit. Independent owners need to build the value of their main asset, academics need to fund research and teaching, and private equity owners need to drive returns for their investors. In other words, there are lots of negative situations in academic and independently owned groups, although private equity gets all the bad press.2-5 Nothing inherently makes one type of practice setting better; it depends on the specific organization. Owners do care about other things beyond just profit (eg, providing quality care, performing cutting-edge research), but when the rubber meets the road, if a practice is providing amazing quality care but losing money doing so, in a short time it won’t be providing any care at all.
- There Is No Free Money. Your long-term compensation will 100% be determined by how much revenue you generate minus the overhead. There is no magic fund to boost your pay long term, no matter how badly the practice needs or wants you. Be clear and even blunt: ask how the practice is going to profit from you. Ask how they plan to make back any signing bonus or guaranteed salary. If they are paying you a higher percentage of collections, ask them how they are able to pay more than competitors. If they say it is because they are more efficient with lower overhead, make sure that increased efficiency does not translate into less support.
- Percent of Collections Is Irrelevant. OK, perhaps not completely irrelevant, but it is one of the least important aspects in determining how much you will make or how happy you will be. Percent of collections is the percentage of the money that the practice actually collects that is paid out to you as compensation. For example, if your percentage of collections is 40%, that means that if the practice collects $1,000,000 for the care you deliver, you will be compensated $400,000. Read on to find out why it is not as important as it seems.
- Don’t Get Too Hung Up on the Details of the Contract. I have seen so many young dermatologists spend enormous amounts of time and money on attorneys and negotiating the fine points of the contract, but not a single one has ever said later that because of all that negotiation they were protected or treated well when things got contentious. What it comes down to is that, if the practice wants to treat you well, they will. If they want to treat you badly, no contract on earth can protect you from all the ways they can do so. And if you leave, no matter what the contract says, they can do whatever they want unless you are willing to spend hundreds of thousands of dollars to fight them in court. So review the contract with an attorney and know what it says, but don’t sweat every period and clause. It isn’t worth it.
- Your Day-to-Day Is Everything. The practice you join may be the best-run practice in the world in every way, except that the office you happen to be going to work in is the one office in the practice that has 2 providers who are jerks and everyone dreads coming to work every morning. There are so many other examples of ways one location can be a disaster even in a great practice—and unfortunately, even great locations can change. The best you can do is to make sure you know where you will be working and with whom. Go and visit the actual office and spend a day shadowing to feel what the vibe is.
What Really Matters
If factors like the percentage of collections you keep are not the big things, what are? The good and bad news is that there isn’t a single answer to this question. Rather, the fundamental question is whether the practice’s plan to maximize profit includes having satisfied, motivated, and engaged long-term providers. Obviously every group practice says this is fundamental to them, but often it isn’t true. Your real job is to find out whether or not it is. The second fundamental question is whether or not the leadership and members of a group practice are competent. It doesn’t matter if they want and intend to do everything right; if the practice is not competent at getting it done, your life practicing dermatology there is not going to be good.
As a dermatologist who has practiced for 20 years in multiple settings, here are some of the questions I would ask when assessing a practice setting I might consider joining. The practice should be able to easily answer all of these questions. If they won’t, can’t, or don’t—or if they answer but don’t give you clear, concrete responses—it is a huge red flag. It could be that they know you won’t like the answers or it could be that they don’t know the answers, but either reason indicates a big problem.
- How do the contracted rates compare to other practices? Pick 5 to 10 Current Procedural Terminology codes you expect to bill the most and ask the practice to tell you the contracted rates for each of those codes with their top 5 payers. Get the same information from all the practices you are considering joining and compare them. The variation between 2 practices in the same market can be as high as 30%. That means that for doing the same work at Practice A you could collect $800,000 and at Practice B in the same market you could collect more than $1,000,000. Getting 45% of your collection from Practice A is a losing proposition compared to getting 40% at Practice B.
- What is the collection rate? If the practice has great contracted rates but terrible revenue cycle management operations, the rates don’t matter. For example, maybe their contracted rate for a given code is $150, compared to another practice whose contracted rate is $125. But if their collection rate is only 60% and the other practice has a collection rate of 80%, they are only getting $90 while the practice with the lower contracted rate is getting $100.
- What billing and coding support does the practice offer? Are you expected to know and keep up with all the procedure codes, modifiers, etc, and use them correctly yourself or do they have professional coders who review every visit? Do they appeal every denied claim? Will you get reports on what charges get denied and why so that you can adjust your practices to avoid further denials?
- How do they train and assign medical assistants (MAs)? The single biggest determinant of your day-to-day productivity and happiness will be your MAs. Having 3 experienced, efficient MAs will allow you to see 50 patients per day with less effort and more fun than seeing 30 patients per day with 2 inexperienced, inefficient MAs. Seeing 50 patients per day at 40% of collections leads to you earning a lot more than seeing 30 per day at 50% of collections. Beyond the basic question of how many MAs you will have, also ask: Will you be expected to train them yourself, or does the practice have a formal training program? Who assesses how well they are performing? Will you have the same MAs every day? When more senior providers have MAs call off sick or leave the practice, will your MAs be pulled to cover their clinics? If that happens, will you be compensated in some way? Get the answers in writing.
- What is the “feel” of the office you will be working in? Ideally you will go and spend a day seeing patients in the office with one of the existing providers to get a sense of whether it’s a place you will be excited to come to every morning. Do you like the other providers? Is there someone who could act as a mentor for you? Does the staff seem happy? Will the physical layout and square footage accommodate the way you imagine practicing? Are the sociodemographics of the patients a fit for what you want?
- Who will be the office manager responsible for your personal practice? Some practices have an on-site manager for every location; others have district or regional managers who are split between multiple practices. Some have both. All can work, but having a competent, supportive office manager with whom you get along with whom and who “gets it” is crucial. You should ask about office manager turnover (high rates are bad, of course) and should ask to meet and interview the office manager who will be the boots on the ground for the practice in your location.
- How much demand for services is there and how are new patients scheduled? If the new hire gets all the hair loss, acne, and eczema cases and the established providers get all the skin cancer/Medicare patients, you are not going to have a balanced patient mix, and you are not going to meet productivity goals because you won’t be doing enough procedures. If there is not enough demand to fill your schedule, what kind of marketing support does the practice offer and what other approaches might they take? If you want to do cosmetics, how are they going to help you grow in that area? Are there other providers who don’t do cosmetics and will refer to you? Is there already someone in the practice who all the referrals go to? Is your percentage of collections based on total collections or on collections after the cost of injectables is deducted?
- What educational support does the practice offer? Do they have an annual meeting for networking and continuing medical education (CME)? If so, will you be expected to use your CME budget to pay to attend? Are there restrictions on what you can use your CME budget for? Is your CME budget considered part of your percentage of collections? Are there experts in the practice you can go to if you have a challenging case or difficult situation?
- Are physician associates and nurse practitioners a big part of the practice? Will you have the opportunity to increase your compensation by supervising them? If so, what is expected of supervising physicians and how are they compensated (flat fee vs percentage of collections vs another model)?
- What does the noncompete say? Obviously the shorter the time period and the smaller the distance, the better. For most practices, a noncompete is nonnegotiable. But there are some nuances to consider: Is the restricted distance from any location that the practice has in the market, or from any location(s) in which you personally have practiced, or from the primary location(s) in which you have practiced? If it is from the primary location(s), get details on how this term is defined: How much do you have to be at a location before it is considered primary? If you stop going to a location, after what period of time is it no longer considered a primary location? Additional questions to ask about noncompetes include: Is there a nonsolicitation clause for employees or patients? Will the practice include a buy-out clause in which you can pay them a set amount to waive the noncompete? Will they make the noncompete time dependent? In other words, if it is a terrible fit and you want to leave in the first year, there is very little justification for them to enforce a noncompete—but unless it is in your contract that they won’t enforce it if you leave before a certain amount of time, they will enforce it.
- Is there a path to having equity in the practice? In academia, this obviously is not a possibility. In independent practices it generally is referred to as an ownership stake or becoming a partner, and in private-equity groups it is literally referred to as “equity,” but they mean essentially the same thing for our purposes. It benefits the practice if you have equity because it gives you a reason to work to help increase the value of the practice. It benefits you to have equity because it means you have more input into decisions that will affect you (and the influence is proportional to how much equity you have) and the equity is an asset that can become very valuable.
The primary advice I have when it comes to being promised an opportunity to become an owner/partner in an independent group is to get the timing and conditions under which you can become an owner in the contract and strongly advocate for a clause that states that if you are not offered the opportunity as defined in the contract that you will be compensated. Also consider what happens if the current owner(s) sell the practice before you become an owner.
In private-equity groups, ask how many of the current providers have equity and ask how the equity is currently divided (what percentage is held by the private equity group, what percentage is held by the CEO and other executives, and what percentage is held by providers). The more equity held by the executive leadership and providers the better, as that means more people are on the same team of trying to increase the value of the practice. Find out how and when you will be able to buy in and try to get this in the contract or at least in writing. Also ask for a guarantee that your equity will not decrease in value. There are instances in which the practice loses value over time due to mismanagement, and the legal structure typically prioritizes the equity of the private-equity owners over the equity of providers. This is called an equity waterfall. Equity that providers were told was worth millions can literally be worth nothing.
One Key Thing You Need to Know
More important than the formal interviews and meetings that will provide you with answers to the questions outlined here, you need to know if you can trust the answers and you need to know the overall culture of the organization. Are they truly pro-provider, and do they believe that engaged and supported providers are the best route to long-term profit maximization? Or do they see providers primarily as replaceable adversaries who need to be placated and managed in order to minimize overhead? The only way to find out is to talk to providers already working there.
If you ask the practice for contact information for providers you can talk to, they likely will put you in touch with those who they know are going to talk about the practice in the best possible light. Be aware that providers may speak positively about a practice for a few different reasons other than that they are actually happy. Maybe the provider has an ownership stake in the practice and will benefit financially if you join. Keep in mind that, if a friend or colleague introduced you to the practice, they are almost certainly getting a substantial referral bonus if you join, so they may not be unbiased; however, if they are an actual friend, the last thing they want is for you to join and be unhappy in the practice because they didn’t tell the truth.
To learn about the experiences of others in your situation who have joined the practice, go to the website and look through the list of providers. Ideally, look for people who are in their first 3 years out of residency who have been there long enough to know the ins and outs but who still are considered newbies and almost certainly don’t have a meaningful ownership stake or strong allegiance to the practice. If it is a geographically widespread practice, focus on people in the region you will be in, but also talk to at least one person from a distant site.
Next, go to the American Academy of Dermatology’s website to find the email addresses for the providers you want to contact in the member directory. Send them an email explaining that you are thinking about joining the practice and that you would like to have an off-the-record phone conversation with them about their experiences. If they decline or don’t respond, it could be a red flag that likely means they don’t think they can speak positively about the practice. If they do agree to speak with you, you can reiterate at that time that the conversation is off the record and that you won’t relay your discussion to anyone at the practice.
Here is a sample email you can use to reach out to providers from a practice you are considering joining:
Subject: Advice on Joining [Practice Name]
Dear Dr. [Name],
I’m a dermatology resident considering joining [Practice Name] and came across your profile. Would you be willing to have a brief (5 to 10 minutes), off-the-record call about your experience? I’d value your perspective and won’t share our conversation with the practice. Thank you!
Best, [Your Name]
Start the conversation with open-ended questions and see where it goes. Some things to ask might be, are you glad you joined the practice? Was there anything that surprised you after you joined? Is there anything you wish you would have asked or known before you joined? I would recommend not asking specifically about their compensation, as it likely will be different from what you are being offered due to variations in location and current market situations.
Final Thoughts
There is no perfect dermatology practice, but the approach outlined here—rooted in first principles and real-world experience—will help you find one that is right for you. Ask tough questions, talk to other providers, and trust your instincts.
- Cwalina TB, Mazmudar RS, Bordeaux JS, et al. Dermatologist workforce mobility: recent trends and characteristics. JAMA Dermatol. 2022;158:323-325. doi:10.1001/jamadermatol.2021.5862
- Oscherwitz ME, Godinich BM, Patel RH, et al. Effects of private equity on dermatologic quality of patient care. J Eur Acad Dermatol Venereol. 2025;39:E100-E102. doi:10.1111/jdv.20191
- Walsh S, Seaton E. Private equity in dermatology: a cloud on the horizon of quality care? J Eur Acad Dermatol Venereol. 2025;39:9-10. doi:10.1111/jdv.20272
- Konda S, Patel S, Francis J. Private equity: the bad and the ugly. Dermatol Clin. 2023;41:597-610. doi:10.1016/j.det.2023.04.004
- Novice T, Portney D, Eshaq M. Dermatology resident perspectives on practice ownership structures and private equity-backed group practices. Clin Dermatol. 2020;38:296-302. doi:10.1016/j.clindermatol.2020.02.008
- Cwalina TB, Mazmudar RS, Bordeaux JS, et al. Dermatologist workforce mobility: recent trends and characteristics. JAMA Dermatol. 2022;158:323-325. doi:10.1001/jamadermatol.2021.5862
- Oscherwitz ME, Godinich BM, Patel RH, et al. Effects of private equity on dermatologic quality of patient care. J Eur Acad Dermatol Venereol. 2025;39:E100-E102. doi:10.1111/jdv.20191
- Walsh S, Seaton E. Private equity in dermatology: a cloud on the horizon of quality care? J Eur Acad Dermatol Venereol. 2025;39:9-10. doi:10.1111/jdv.20272
- Konda S, Patel S, Francis J. Private equity: the bad and the ugly. Dermatol Clin. 2023;41:597-610. doi:10.1016/j.det.2023.04.004
- Novice T, Portney D, Eshaq M. Dermatology resident perspectives on practice ownership structures and private equity-backed group practices. Clin Dermatol. 2020;38:296-302. doi:10.1016/j.clindermatol.2020.02.008
What Dermatology Residents Need to Know About Joining Group Practices
What Dermatology Residents Need to Know About Joining Group Practices
PRACTICE POINTS
- Finding the right fit in the first position out of dermatology residency can be difficult and feel overwhelming.
- Leaving one practice and joining another is especially common in the first 10 years after residency.
- Asking the right questions can increase the probability of finding the right practice for you and receiving fair compensation.
Noncompete Agreements and Their Impact on the Medical Landscape
In April 2024, the Federal Trade Commission (FTC) issued a nationwide rule to ban most employee noncompete agreements, including many used in health care1; however, that rule never took effect. In August 2024, a federal district court ruled that the FTC had exceeded its statutory authority and blocked the ban,2 and subsequent litigation and agency actions followed. On September 5, 2025, the FTC formally moved to accede to vacatur—in other words, it will not enforce the rule and backed away from defending it on appeal.3 As of December 2025, there is no active federal ban on physician noncompetes. The obligations of the physician employee are dictated by state law and the precise language of the contract that is signed.
In this article, we discuss the historical origins of noncompetes, employer and physician perspectives, and the downstream consequences for patient continuity, access, and health care costs.
Background
The concept of noncompete agreements is not new—this legal principle dates back several centuries, but it was not until several hundred years later, between the 1950s and 1980s, that noncompete agreements became routine in physician contracts. This trend emerged, at least in part, from the growing commoditization of medicine, the expansion of hospital infrastructure, and the rise of physicians employed by entities rather than owning a private practice. Medical practices, hospitals, and increasingly large private groups began using noncompete agreements to prevent physicians from leaving and establishing competing practices nearby. Since then, noncompetes have remained a contentious issue within both the legal system and the broader physician-employer relationship.
Employer vs Employee Perspective
From the employer’s perspective, health care systems and medical groups argue that noncompete agreements are necessary to protect legitimate business interests, citing physician training, established patient relationships, and proprietary information gained from employment with that entity as supporting reasons. Additionally, employers maintain that recouping the cost of recruitment and onboarding investments as well as sustaining continuity of care within the organization should take precedence. On occasion, health care systems will invest time and financial resources in recruiting physicians, provide administrative and clinical support, and integrate new employees into established referral pathways and patient populations. In this view, noncompetes serve as a tool to ensure stability within the health care system, discouraging abrupt departures that could fracture patient care or lead to unfair competition using institutional resources. While these arguments hold merit in certain cases, many physicians do not receive employer-funded education or training beyond what is required in residency and fellowship. As a result, the financial justifications for noncompetes often are overstated; on the contrary, the cost of a “buy-out” or the financial barrier imposed by a noncompete clause can amount to a considerable portion of a physician’s annual salary—sometimes multiple times that amount—creating an imbalance that favors the employer and limits professional mobility.
When a physician is prohibited from practicing in a specific area after leaving an employer, a complex web of adverse consequences can arise, impacting both the physician and the patients they serve. Physician mobility and career choice become restricted, effectively constraining the physicians’ livelihood and ability to provide for themselves and their dependents; in single-earner physician families, this can have devastating financial consequences. These limitations contribute to growing burnout and dissatisfaction within the medical profession, which already is facing unprecedented levels of stress and physician workforce shortages.4
Effect on Patients
When a physician is forced to relocate to a new geographic region because of a noncompete clause, their patients can experience substantial disruptions in care. Access to medical services may be affected, leading to longer wait-times and fewer available appointments, especially in areas that already have a shortage of providers. Patients may lose longstanding relationships with doctors who know their medical histories, which can interrupt treatment plans and increase the risk of complications. Those with chronic illnesses, complex conditions, or time-sensitive treatments are particularly vulnerable to adverse outcomes. Many patients must travel farther—sometimes out of their insurance network—to find replacement care, increasing both financial and logistical burdens. These abrupt transitions also can raise health care costs due to emergency department use, inefficient handoffs, and higher incidence of morbidity/mortality.5 Noncompete restrictions often prevent physicians from informing patients where they are relocating, creating confusion and fragmentation of care. As a result, trust in the health care system may decline when patients perceive that business agreements are being prioritized above their wellbeing. The impact may be even more severe in rural or underserved communities where alternative providers are scarce.
Final Thoughts
In recent years, noncompete agreements in health care have come under intensified scrutiny for their potential to stifle physician mobility, reduce competition, and inflate health care costs by limiting where and how physicians can practice. The trajectory of noncompetes in physician employment reflects broader shifts in how medicine is structured and delivered in the United States. In the latter half of the 20th century, what began as a centuries-old legal concept became a standard feature of physician employment contracts. That evolution largely was driven by the corporatization of medicine and large hospital group/private equity employment of physicians. As these agreements proliferated, public policy questions emerged: What does restricting a physician’s mobility do to patient access? To competition in provider markets? To the cost and availability of care? To the current epidemic of physician burnout?
These questions moved from the legal sidelines to center stage in the 2020s, when the FTC sought to tackle noncompetes across the entire economy—physicians included—on the theory they suppressed labor mobility, entrepreneurship, and competition. In February 2020, the American Medical Association submitted comments to the FTC on the utility of noncompete agreements in employee contracts stating that they restrict competition, can disrupt continuity of care, and may limit access to care.6 Although the FTC’s regulatory attempt in April 2024 provoked strong policy signals, it was challenged and ultimately blocked. Rather than a clear federal prohibition, the outcome is a more incremental state-based shift in rules governing physician noncompetes. For physicians today, this means more awareness and more leverage, but also more complexity. Whether a noncompete will be enforceable depends heavily on the state, the wording of the contract, the structure of the employer, and the specialty. From a negotiation standpoint, physicians need more guidance and awareness on the exact ramifications of their employee contract. For newly minted physicians, many of whom enter the workforce with considerable training debt, the priority often is securing employment to work toward financial stability, building a family, or both; however, all physicians should press for shorter durations, tighter geographic limits, narrower scopes of service, clear buy-out options, and explicit patient-continuity protections. Better yet, physicians can exercise the right of refusal to any noncompete clause at all. Becoming involved with a local medical organization or foundation can provide immense support, both in reviewing contracts as well as learning how to become advocates for physicians in this environment. As more physicians stand together to protect both practice autonomy and the right to quality care, we all become closer to rediscovering the beauty and fulfillment in the purest form of medicine.
- Federal Trade Commission. FTC announces rule banning noncompetes. April 23, 2024. Accessed December 1, 2025. https://www.ftc.gov/news-events/news/press-releases/2024/04/ftc-announces-rule-banning-noncompetes
- US Chamber of Commerce. Ryan LLC v FTC. August 20, 2024. Accessed December 1, 2025. https://www.uschamber.com/cases/antitrust-and-competition-law/ryan-llc-v.-ftc
- Federal Trade Commission. Federal Trade Commission files to accede to vacatur of non-compete clause rule. September 5, 2025. Accessed December 1, 2025. https://www.ftc.gov/news-events/news/press-releases/2025/09/federal-trade-commission-files-accede-vacatur-non-compete-clause-rule
- Marshall JJ, Ashwath ML, Jefferies JL, et al. Restrictive covenants and noncompete clauses for physicians. JACC Adv. 2023;2:100547.
- Sabety A. The value of relationships in healthcare. J Publich Economics. 2023;225:104927.
- American Medical Association. AMA provides comment to FTC on non-compete agreements. National Advocacy Update. February 14, 2020. Accessed November 25, 2025. https://www.ama-assn.org/health-care-advocacy/advocacy-update/feb-14-2020-national-advocacy-update
In April 2024, the Federal Trade Commission (FTC) issued a nationwide rule to ban most employee noncompete agreements, including many used in health care1; however, that rule never took effect. In August 2024, a federal district court ruled that the FTC had exceeded its statutory authority and blocked the ban,2 and subsequent litigation and agency actions followed. On September 5, 2025, the FTC formally moved to accede to vacatur—in other words, it will not enforce the rule and backed away from defending it on appeal.3 As of December 2025, there is no active federal ban on physician noncompetes. The obligations of the physician employee are dictated by state law and the precise language of the contract that is signed.
In this article, we discuss the historical origins of noncompetes, employer and physician perspectives, and the downstream consequences for patient continuity, access, and health care costs.
Background
The concept of noncompete agreements is not new—this legal principle dates back several centuries, but it was not until several hundred years later, between the 1950s and 1980s, that noncompete agreements became routine in physician contracts. This trend emerged, at least in part, from the growing commoditization of medicine, the expansion of hospital infrastructure, and the rise of physicians employed by entities rather than owning a private practice. Medical practices, hospitals, and increasingly large private groups began using noncompete agreements to prevent physicians from leaving and establishing competing practices nearby. Since then, noncompetes have remained a contentious issue within both the legal system and the broader physician-employer relationship.
Employer vs Employee Perspective
From the employer’s perspective, health care systems and medical groups argue that noncompete agreements are necessary to protect legitimate business interests, citing physician training, established patient relationships, and proprietary information gained from employment with that entity as supporting reasons. Additionally, employers maintain that recouping the cost of recruitment and onboarding investments as well as sustaining continuity of care within the organization should take precedence. On occasion, health care systems will invest time and financial resources in recruiting physicians, provide administrative and clinical support, and integrate new employees into established referral pathways and patient populations. In this view, noncompetes serve as a tool to ensure stability within the health care system, discouraging abrupt departures that could fracture patient care or lead to unfair competition using institutional resources. While these arguments hold merit in certain cases, many physicians do not receive employer-funded education or training beyond what is required in residency and fellowship. As a result, the financial justifications for noncompetes often are overstated; on the contrary, the cost of a “buy-out” or the financial barrier imposed by a noncompete clause can amount to a considerable portion of a physician’s annual salary—sometimes multiple times that amount—creating an imbalance that favors the employer and limits professional mobility.
When a physician is prohibited from practicing in a specific area after leaving an employer, a complex web of adverse consequences can arise, impacting both the physician and the patients they serve. Physician mobility and career choice become restricted, effectively constraining the physicians’ livelihood and ability to provide for themselves and their dependents; in single-earner physician families, this can have devastating financial consequences. These limitations contribute to growing burnout and dissatisfaction within the medical profession, which already is facing unprecedented levels of stress and physician workforce shortages.4
Effect on Patients
When a physician is forced to relocate to a new geographic region because of a noncompete clause, their patients can experience substantial disruptions in care. Access to medical services may be affected, leading to longer wait-times and fewer available appointments, especially in areas that already have a shortage of providers. Patients may lose longstanding relationships with doctors who know their medical histories, which can interrupt treatment plans and increase the risk of complications. Those with chronic illnesses, complex conditions, or time-sensitive treatments are particularly vulnerable to adverse outcomes. Many patients must travel farther—sometimes out of their insurance network—to find replacement care, increasing both financial and logistical burdens. These abrupt transitions also can raise health care costs due to emergency department use, inefficient handoffs, and higher incidence of morbidity/mortality.5 Noncompete restrictions often prevent physicians from informing patients where they are relocating, creating confusion and fragmentation of care. As a result, trust in the health care system may decline when patients perceive that business agreements are being prioritized above their wellbeing. The impact may be even more severe in rural or underserved communities where alternative providers are scarce.
Final Thoughts
In recent years, noncompete agreements in health care have come under intensified scrutiny for their potential to stifle physician mobility, reduce competition, and inflate health care costs by limiting where and how physicians can practice. The trajectory of noncompetes in physician employment reflects broader shifts in how medicine is structured and delivered in the United States. In the latter half of the 20th century, what began as a centuries-old legal concept became a standard feature of physician employment contracts. That evolution largely was driven by the corporatization of medicine and large hospital group/private equity employment of physicians. As these agreements proliferated, public policy questions emerged: What does restricting a physician’s mobility do to patient access? To competition in provider markets? To the cost and availability of care? To the current epidemic of physician burnout?
These questions moved from the legal sidelines to center stage in the 2020s, when the FTC sought to tackle noncompetes across the entire economy—physicians included—on the theory they suppressed labor mobility, entrepreneurship, and competition. In February 2020, the American Medical Association submitted comments to the FTC on the utility of noncompete agreements in employee contracts stating that they restrict competition, can disrupt continuity of care, and may limit access to care.6 Although the FTC’s regulatory attempt in April 2024 provoked strong policy signals, it was challenged and ultimately blocked. Rather than a clear federal prohibition, the outcome is a more incremental state-based shift in rules governing physician noncompetes. For physicians today, this means more awareness and more leverage, but also more complexity. Whether a noncompete will be enforceable depends heavily on the state, the wording of the contract, the structure of the employer, and the specialty. From a negotiation standpoint, physicians need more guidance and awareness on the exact ramifications of their employee contract. For newly minted physicians, many of whom enter the workforce with considerable training debt, the priority often is securing employment to work toward financial stability, building a family, or both; however, all physicians should press for shorter durations, tighter geographic limits, narrower scopes of service, clear buy-out options, and explicit patient-continuity protections. Better yet, physicians can exercise the right of refusal to any noncompete clause at all. Becoming involved with a local medical organization or foundation can provide immense support, both in reviewing contracts as well as learning how to become advocates for physicians in this environment. As more physicians stand together to protect both practice autonomy and the right to quality care, we all become closer to rediscovering the beauty and fulfillment in the purest form of medicine.
In April 2024, the Federal Trade Commission (FTC) issued a nationwide rule to ban most employee noncompete agreements, including many used in health care1; however, that rule never took effect. In August 2024, a federal district court ruled that the FTC had exceeded its statutory authority and blocked the ban,2 and subsequent litigation and agency actions followed. On September 5, 2025, the FTC formally moved to accede to vacatur—in other words, it will not enforce the rule and backed away from defending it on appeal.3 As of December 2025, there is no active federal ban on physician noncompetes. The obligations of the physician employee are dictated by state law and the precise language of the contract that is signed.
In this article, we discuss the historical origins of noncompetes, employer and physician perspectives, and the downstream consequences for patient continuity, access, and health care costs.
Background
The concept of noncompete agreements is not new—this legal principle dates back several centuries, but it was not until several hundred years later, between the 1950s and 1980s, that noncompete agreements became routine in physician contracts. This trend emerged, at least in part, from the growing commoditization of medicine, the expansion of hospital infrastructure, and the rise of physicians employed by entities rather than owning a private practice. Medical practices, hospitals, and increasingly large private groups began using noncompete agreements to prevent physicians from leaving and establishing competing practices nearby. Since then, noncompetes have remained a contentious issue within both the legal system and the broader physician-employer relationship.
Employer vs Employee Perspective
From the employer’s perspective, health care systems and medical groups argue that noncompete agreements are necessary to protect legitimate business interests, citing physician training, established patient relationships, and proprietary information gained from employment with that entity as supporting reasons. Additionally, employers maintain that recouping the cost of recruitment and onboarding investments as well as sustaining continuity of care within the organization should take precedence. On occasion, health care systems will invest time and financial resources in recruiting physicians, provide administrative and clinical support, and integrate new employees into established referral pathways and patient populations. In this view, noncompetes serve as a tool to ensure stability within the health care system, discouraging abrupt departures that could fracture patient care or lead to unfair competition using institutional resources. While these arguments hold merit in certain cases, many physicians do not receive employer-funded education or training beyond what is required in residency and fellowship. As a result, the financial justifications for noncompetes often are overstated; on the contrary, the cost of a “buy-out” or the financial barrier imposed by a noncompete clause can amount to a considerable portion of a physician’s annual salary—sometimes multiple times that amount—creating an imbalance that favors the employer and limits professional mobility.
When a physician is prohibited from practicing in a specific area after leaving an employer, a complex web of adverse consequences can arise, impacting both the physician and the patients they serve. Physician mobility and career choice become restricted, effectively constraining the physicians’ livelihood and ability to provide for themselves and their dependents; in single-earner physician families, this can have devastating financial consequences. These limitations contribute to growing burnout and dissatisfaction within the medical profession, which already is facing unprecedented levels of stress and physician workforce shortages.4
Effect on Patients
When a physician is forced to relocate to a new geographic region because of a noncompete clause, their patients can experience substantial disruptions in care. Access to medical services may be affected, leading to longer wait-times and fewer available appointments, especially in areas that already have a shortage of providers. Patients may lose longstanding relationships with doctors who know their medical histories, which can interrupt treatment plans and increase the risk of complications. Those with chronic illnesses, complex conditions, or time-sensitive treatments are particularly vulnerable to adverse outcomes. Many patients must travel farther—sometimes out of their insurance network—to find replacement care, increasing both financial and logistical burdens. These abrupt transitions also can raise health care costs due to emergency department use, inefficient handoffs, and higher incidence of morbidity/mortality.5 Noncompete restrictions often prevent physicians from informing patients where they are relocating, creating confusion and fragmentation of care. As a result, trust in the health care system may decline when patients perceive that business agreements are being prioritized above their wellbeing. The impact may be even more severe in rural or underserved communities where alternative providers are scarce.
Final Thoughts
In recent years, noncompete agreements in health care have come under intensified scrutiny for their potential to stifle physician mobility, reduce competition, and inflate health care costs by limiting where and how physicians can practice. The trajectory of noncompetes in physician employment reflects broader shifts in how medicine is structured and delivered in the United States. In the latter half of the 20th century, what began as a centuries-old legal concept became a standard feature of physician employment contracts. That evolution largely was driven by the corporatization of medicine and large hospital group/private equity employment of physicians. As these agreements proliferated, public policy questions emerged: What does restricting a physician’s mobility do to patient access? To competition in provider markets? To the cost and availability of care? To the current epidemic of physician burnout?
These questions moved from the legal sidelines to center stage in the 2020s, when the FTC sought to tackle noncompetes across the entire economy—physicians included—on the theory they suppressed labor mobility, entrepreneurship, and competition. In February 2020, the American Medical Association submitted comments to the FTC on the utility of noncompete agreements in employee contracts stating that they restrict competition, can disrupt continuity of care, and may limit access to care.6 Although the FTC’s regulatory attempt in April 2024 provoked strong policy signals, it was challenged and ultimately blocked. Rather than a clear federal prohibition, the outcome is a more incremental state-based shift in rules governing physician noncompetes. For physicians today, this means more awareness and more leverage, but also more complexity. Whether a noncompete will be enforceable depends heavily on the state, the wording of the contract, the structure of the employer, and the specialty. From a negotiation standpoint, physicians need more guidance and awareness on the exact ramifications of their employee contract. For newly minted physicians, many of whom enter the workforce with considerable training debt, the priority often is securing employment to work toward financial stability, building a family, or both; however, all physicians should press for shorter durations, tighter geographic limits, narrower scopes of service, clear buy-out options, and explicit patient-continuity protections. Better yet, physicians can exercise the right of refusal to any noncompete clause at all. Becoming involved with a local medical organization or foundation can provide immense support, both in reviewing contracts as well as learning how to become advocates for physicians in this environment. As more physicians stand together to protect both practice autonomy and the right to quality care, we all become closer to rediscovering the beauty and fulfillment in the purest form of medicine.
- Federal Trade Commission. FTC announces rule banning noncompetes. April 23, 2024. Accessed December 1, 2025. https://www.ftc.gov/news-events/news/press-releases/2024/04/ftc-announces-rule-banning-noncompetes
- US Chamber of Commerce. Ryan LLC v FTC. August 20, 2024. Accessed December 1, 2025. https://www.uschamber.com/cases/antitrust-and-competition-law/ryan-llc-v.-ftc
- Federal Trade Commission. Federal Trade Commission files to accede to vacatur of non-compete clause rule. September 5, 2025. Accessed December 1, 2025. https://www.ftc.gov/news-events/news/press-releases/2025/09/federal-trade-commission-files-accede-vacatur-non-compete-clause-rule
- Marshall JJ, Ashwath ML, Jefferies JL, et al. Restrictive covenants and noncompete clauses for physicians. JACC Adv. 2023;2:100547.
- Sabety A. The value of relationships in healthcare. J Publich Economics. 2023;225:104927.
- American Medical Association. AMA provides comment to FTC on non-compete agreements. National Advocacy Update. February 14, 2020. Accessed November 25, 2025. https://www.ama-assn.org/health-care-advocacy/advocacy-update/feb-14-2020-national-advocacy-update
- Federal Trade Commission. FTC announces rule banning noncompetes. April 23, 2024. Accessed December 1, 2025. https://www.ftc.gov/news-events/news/press-releases/2024/04/ftc-announces-rule-banning-noncompetes
- US Chamber of Commerce. Ryan LLC v FTC. August 20, 2024. Accessed December 1, 2025. https://www.uschamber.com/cases/antitrust-and-competition-law/ryan-llc-v.-ftc
- Federal Trade Commission. Federal Trade Commission files to accede to vacatur of non-compete clause rule. September 5, 2025. Accessed December 1, 2025. https://www.ftc.gov/news-events/news/press-releases/2025/09/federal-trade-commission-files-accede-vacatur-non-compete-clause-rule
- Marshall JJ, Ashwath ML, Jefferies JL, et al. Restrictive covenants and noncompete clauses for physicians. JACC Adv. 2023;2:100547.
- Sabety A. The value of relationships in healthcare. J Publich Economics. 2023;225:104927.
- American Medical Association. AMA provides comment to FTC on non-compete agreements. National Advocacy Update. February 14, 2020. Accessed November 25, 2025. https://www.ama-assn.org/health-care-advocacy/advocacy-update/feb-14-2020-national-advocacy-update
PRACTICE POINTS
- There is no active federal ban on physician noncompete agreements as of late 2025.
- Physician noncompetes have expanded alongside the corporatization of medicine but raise serious concerns about physician mobility, burnout, workforce shortages, and patient access to care, particularly in underserved areas.
- Physicians should critically evaluate noncompetes prior to signing an agreement, advocating for narrower limits or refusal altogether to protect professional autonomy, continuity of care, and patient welfare.
Dermatology on Duty: Pathways to a Career in Military Medicine
Dermatology on Duty: Pathways to a Career in Military Medicine
Serving those who serve has been one of the most meaningful parts of my career. A career in military medicine offers dermatologists not only a chance to practice within a unique and diverse patient population but also an opportunity to contribute to something larger than themselves. Whether working with active-duty service members and their families within the Military Health System (MHS) or caring for veterans through the Department of Veterans Affairs (VA), the experience can be both enriching and rewarding. This article will explore the various pathways available to dermatologists to serve military communities, whether they are at the start of their careers or are looking for a change of pace within their established practice.
Care Pathways for Military and Veterans
To care for uniformed service members, their families, and retired personnel, dermatologists typically serve within the MHS—a global, integrated network of military hospitals and clinics dedicated to delivering health care to this population.1 TRICARE is the health insurance program that covers those eligible for care within the system, including active-duty and retired service members.2 In this context, it is important to clarify what the term retired actually means, as it differs from the term veteran when it comes to accessing health care options, and these terms frequently are conflated. A retired service member is an individual who completed at least 20 years of active-duty service or who has been medically retired because of a condition or injury incurred while on active duty.3 In contrast, a veteran may not have completed 20 years of service but has separated honorably after serving at least 24 continuous months.4 Veterans typically receive care through the VA system.5
Serving on Active Duty
In general, there are 2 main pathways to serve as a dermatologist within the MHS. The first is to commission in the military and serve on active duty. Most often, this pathway begins with a premedical student applying to medical school. Those considering military service typically explore scholarship programs such as the Health Professions Scholarship Program (HPSP)(https://www.medicineandthemilitary.com/applying-and-what-to-expect/medical-school-programs/hpsp) or the Health Services Collegiate Program (HSCP), or they apply to the Uniformed Services University of the Health Sciences (USU)(https://www.usuhs.edu/about). The HPSP and HSCP programs financially support medical students training at civilian medical schools, though in different ways—the HPSP covers tuition and fees, while the HSCP provides a salary during training but does not cover tuition.6 In contrast, students of USU attend the nation’s only military medical school, serving in uniform for 4 years while earning the pay and benefits of a junior officer in their respective service branch. Any premedical student considering the HPSP, HSCP or USU routes for service must meet the commissioning standards of their chosen branch—Army, Navy, or Air Force—and enter service as an officer before beginning medical school.
While direct commission prior to medical school is the most common route to active-duty service, board-certified dermatologists also can join a military branch later through what is called Direct Accession or Direct Commission; for example, the Navy offers a Residency to Direct Accession program, which commissions residents in their final year of training to join the Navy upon graduation. In some cases, commissioning at this stage includes a bonus of up to $600,000 in exchange for a 4-year active-duty commitment.7 The Army and Air Force offer similar direct commission programs, though specific incentives vary.8 Interested residents or practitioners can contact a local recruiting office within their branch of interest to learn more. Direct accession is open at many points in a dermatologist’s career—after residency, after fellowship, or even as an established civilian practitioner—and the initial commissioning rank and bonus generally reflect one’s level of experience.
Serving as a Civilian
Outside of uniformed service, dermatologists can find opportunities to provide care for active-duty service members, veterans, and military families through employment as General Schedule (GS) employees. The GS is a role classification and pay system that covers most federal employees in professional, administrative, and technical positions (eg, physicians). The GS system classifies most of these employees based on the complexity, responsibility, and qualifications required for their role.9 Such positions often are at the highest level of the GS pay scale, reflecting the expertise and years of education required to become a dermatologist, though pay varies by location and experience. In contrast, physicians employed through the VA system are classified as Title 38 federal employees, governed by a different pay structure and regulatory framework under the US Code of Federal Regulations.10 These regulations govern the hiring, retention, and firing guidelines for VA physicians, which differ from those of GS physicians. A full explanation is outside of the scope of this article, however.
Final Thoughts
In summary, uniformed or federal service as a dermatologist offers a meaningful and impactful way to give back to those who have served our country. Opportunities exist throughout the United States for dermatologists interested in serving within the MHS or VA. The most transparent and up-to-date resource for identifying open positions in both large metropolitan areas and smaller communities is USAJOBS.gov. While financial compensation may not always match that of private practice, the intangible benefits are considerable—stable employment, comprehensive benefits, malpractice coverage, and secure retirement, among others. There is something deeply fulfilling about using one’s medical skills in service of a larger mission. The relationships built with service members, the sense of shared purpose, and the opportunity to contribute to the readiness and well-being of those who serve all make this career path profoundly rewarding. For dermatologists seeking a practice that combines professional growth with purpose and patriotism, military medicine offers a truly special calling.
- Military Health System. Elements of the military health system. Accessed October 11, 2025. https://www.health.mil/About-MHS/MHS-Elements
- TRICARE. Plans and eligibility. Accessed October 11, 2025. https://tricare.mil/Plans/Eligibility
- Military Benefit. TRICARE for retirees. Accessed October 11, 2025. https://www.militarybenefit.org/get-educated/tricareforretirees/
- US Department of Veterans Affairs. Eligibility for VA health care. Accessed October 11, 2025. https://www.va.gov/health-care/eligibility/
- US Department of Veterans Affairs. VA priority groups. Accessed October 11, 2025. https://www.va.gov/health-care/eligibility/priority-groups/
- Navy Medicine. Health Professions Scholarship Program (HPSP) and Financial Assistance Program (FAP). Accessed October 12, 2025. https://www.med.navy.mil/Accessions/Health-Professions-Scholarship-Program-HPSP-and-Financial-Assistance-Program-FAP/
- US Navy. Navy Medicine R2DA program. Accessed October 12, 2025. https://www.navy.com/navy-medicine
- US Army Medical Department. Student programs. Accessed October 12, 2025. https://goamedd.com/student-programs
- US Office of Personnel Management. General Schedule. Accessed October 12, 2025. https://www.opm.gov/policy-data-oversight/pay-leave/pay-systems/general-schedule/
- Pines Federal Employment Attorneys. Title 38 employees: medical professionals. Accessed October 12, 2025. https://www.pinesfederal.com/va-federal-employees/title-38-employees-medical-professionals/
Serving those who serve has been one of the most meaningful parts of my career. A career in military medicine offers dermatologists not only a chance to practice within a unique and diverse patient population but also an opportunity to contribute to something larger than themselves. Whether working with active-duty service members and their families within the Military Health System (MHS) or caring for veterans through the Department of Veterans Affairs (VA), the experience can be both enriching and rewarding. This article will explore the various pathways available to dermatologists to serve military communities, whether they are at the start of their careers or are looking for a change of pace within their established practice.
Care Pathways for Military and Veterans
To care for uniformed service members, their families, and retired personnel, dermatologists typically serve within the MHS—a global, integrated network of military hospitals and clinics dedicated to delivering health care to this population.1 TRICARE is the health insurance program that covers those eligible for care within the system, including active-duty and retired service members.2 In this context, it is important to clarify what the term retired actually means, as it differs from the term veteran when it comes to accessing health care options, and these terms frequently are conflated. A retired service member is an individual who completed at least 20 years of active-duty service or who has been medically retired because of a condition or injury incurred while on active duty.3 In contrast, a veteran may not have completed 20 years of service but has separated honorably after serving at least 24 continuous months.4 Veterans typically receive care through the VA system.5
Serving on Active Duty
In general, there are 2 main pathways to serve as a dermatologist within the MHS. The first is to commission in the military and serve on active duty. Most often, this pathway begins with a premedical student applying to medical school. Those considering military service typically explore scholarship programs such as the Health Professions Scholarship Program (HPSP)(https://www.medicineandthemilitary.com/applying-and-what-to-expect/medical-school-programs/hpsp) or the Health Services Collegiate Program (HSCP), or they apply to the Uniformed Services University of the Health Sciences (USU)(https://www.usuhs.edu/about). The HPSP and HSCP programs financially support medical students training at civilian medical schools, though in different ways—the HPSP covers tuition and fees, while the HSCP provides a salary during training but does not cover tuition.6 In contrast, students of USU attend the nation’s only military medical school, serving in uniform for 4 years while earning the pay and benefits of a junior officer in their respective service branch. Any premedical student considering the HPSP, HSCP or USU routes for service must meet the commissioning standards of their chosen branch—Army, Navy, or Air Force—and enter service as an officer before beginning medical school.
While direct commission prior to medical school is the most common route to active-duty service, board-certified dermatologists also can join a military branch later through what is called Direct Accession or Direct Commission; for example, the Navy offers a Residency to Direct Accession program, which commissions residents in their final year of training to join the Navy upon graduation. In some cases, commissioning at this stage includes a bonus of up to $600,000 in exchange for a 4-year active-duty commitment.7 The Army and Air Force offer similar direct commission programs, though specific incentives vary.8 Interested residents or practitioners can contact a local recruiting office within their branch of interest to learn more. Direct accession is open at many points in a dermatologist’s career—after residency, after fellowship, or even as an established civilian practitioner—and the initial commissioning rank and bonus generally reflect one’s level of experience.
Serving as a Civilian
Outside of uniformed service, dermatologists can find opportunities to provide care for active-duty service members, veterans, and military families through employment as General Schedule (GS) employees. The GS is a role classification and pay system that covers most federal employees in professional, administrative, and technical positions (eg, physicians). The GS system classifies most of these employees based on the complexity, responsibility, and qualifications required for their role.9 Such positions often are at the highest level of the GS pay scale, reflecting the expertise and years of education required to become a dermatologist, though pay varies by location and experience. In contrast, physicians employed through the VA system are classified as Title 38 federal employees, governed by a different pay structure and regulatory framework under the US Code of Federal Regulations.10 These regulations govern the hiring, retention, and firing guidelines for VA physicians, which differ from those of GS physicians. A full explanation is outside of the scope of this article, however.
Final Thoughts
In summary, uniformed or federal service as a dermatologist offers a meaningful and impactful way to give back to those who have served our country. Opportunities exist throughout the United States for dermatologists interested in serving within the MHS or VA. The most transparent and up-to-date resource for identifying open positions in both large metropolitan areas and smaller communities is USAJOBS.gov. While financial compensation may not always match that of private practice, the intangible benefits are considerable—stable employment, comprehensive benefits, malpractice coverage, and secure retirement, among others. There is something deeply fulfilling about using one’s medical skills in service of a larger mission. The relationships built with service members, the sense of shared purpose, and the opportunity to contribute to the readiness and well-being of those who serve all make this career path profoundly rewarding. For dermatologists seeking a practice that combines professional growth with purpose and patriotism, military medicine offers a truly special calling.
Serving those who serve has been one of the most meaningful parts of my career. A career in military medicine offers dermatologists not only a chance to practice within a unique and diverse patient population but also an opportunity to contribute to something larger than themselves. Whether working with active-duty service members and their families within the Military Health System (MHS) or caring for veterans through the Department of Veterans Affairs (VA), the experience can be both enriching and rewarding. This article will explore the various pathways available to dermatologists to serve military communities, whether they are at the start of their careers or are looking for a change of pace within their established practice.
Care Pathways for Military and Veterans
To care for uniformed service members, their families, and retired personnel, dermatologists typically serve within the MHS—a global, integrated network of military hospitals and clinics dedicated to delivering health care to this population.1 TRICARE is the health insurance program that covers those eligible for care within the system, including active-duty and retired service members.2 In this context, it is important to clarify what the term retired actually means, as it differs from the term veteran when it comes to accessing health care options, and these terms frequently are conflated. A retired service member is an individual who completed at least 20 years of active-duty service or who has been medically retired because of a condition or injury incurred while on active duty.3 In contrast, a veteran may not have completed 20 years of service but has separated honorably after serving at least 24 continuous months.4 Veterans typically receive care through the VA system.5
Serving on Active Duty
In general, there are 2 main pathways to serve as a dermatologist within the MHS. The first is to commission in the military and serve on active duty. Most often, this pathway begins with a premedical student applying to medical school. Those considering military service typically explore scholarship programs such as the Health Professions Scholarship Program (HPSP)(https://www.medicineandthemilitary.com/applying-and-what-to-expect/medical-school-programs/hpsp) or the Health Services Collegiate Program (HSCP), or they apply to the Uniformed Services University of the Health Sciences (USU)(https://www.usuhs.edu/about). The HPSP and HSCP programs financially support medical students training at civilian medical schools, though in different ways—the HPSP covers tuition and fees, while the HSCP provides a salary during training but does not cover tuition.6 In contrast, students of USU attend the nation’s only military medical school, serving in uniform for 4 years while earning the pay and benefits of a junior officer in their respective service branch. Any premedical student considering the HPSP, HSCP or USU routes for service must meet the commissioning standards of their chosen branch—Army, Navy, or Air Force—and enter service as an officer before beginning medical school.
While direct commission prior to medical school is the most common route to active-duty service, board-certified dermatologists also can join a military branch later through what is called Direct Accession or Direct Commission; for example, the Navy offers a Residency to Direct Accession program, which commissions residents in their final year of training to join the Navy upon graduation. In some cases, commissioning at this stage includes a bonus of up to $600,000 in exchange for a 4-year active-duty commitment.7 The Army and Air Force offer similar direct commission programs, though specific incentives vary.8 Interested residents or practitioners can contact a local recruiting office within their branch of interest to learn more. Direct accession is open at many points in a dermatologist’s career—after residency, after fellowship, or even as an established civilian practitioner—and the initial commissioning rank and bonus generally reflect one’s level of experience.
Serving as a Civilian
Outside of uniformed service, dermatologists can find opportunities to provide care for active-duty service members, veterans, and military families through employment as General Schedule (GS) employees. The GS is a role classification and pay system that covers most federal employees in professional, administrative, and technical positions (eg, physicians). The GS system classifies most of these employees based on the complexity, responsibility, and qualifications required for their role.9 Such positions often are at the highest level of the GS pay scale, reflecting the expertise and years of education required to become a dermatologist, though pay varies by location and experience. In contrast, physicians employed through the VA system are classified as Title 38 federal employees, governed by a different pay structure and regulatory framework under the US Code of Federal Regulations.10 These regulations govern the hiring, retention, and firing guidelines for VA physicians, which differ from those of GS physicians. A full explanation is outside of the scope of this article, however.
Final Thoughts
In summary, uniformed or federal service as a dermatologist offers a meaningful and impactful way to give back to those who have served our country. Opportunities exist throughout the United States for dermatologists interested in serving within the MHS or VA. The most transparent and up-to-date resource for identifying open positions in both large metropolitan areas and smaller communities is USAJOBS.gov. While financial compensation may not always match that of private practice, the intangible benefits are considerable—stable employment, comprehensive benefits, malpractice coverage, and secure retirement, among others. There is something deeply fulfilling about using one’s medical skills in service of a larger mission. The relationships built with service members, the sense of shared purpose, and the opportunity to contribute to the readiness and well-being of those who serve all make this career path profoundly rewarding. For dermatologists seeking a practice that combines professional growth with purpose and patriotism, military medicine offers a truly special calling.
- Military Health System. Elements of the military health system. Accessed October 11, 2025. https://www.health.mil/About-MHS/MHS-Elements
- TRICARE. Plans and eligibility. Accessed October 11, 2025. https://tricare.mil/Plans/Eligibility
- Military Benefit. TRICARE for retirees. Accessed October 11, 2025. https://www.militarybenefit.org/get-educated/tricareforretirees/
- US Department of Veterans Affairs. Eligibility for VA health care. Accessed October 11, 2025. https://www.va.gov/health-care/eligibility/
- US Department of Veterans Affairs. VA priority groups. Accessed October 11, 2025. https://www.va.gov/health-care/eligibility/priority-groups/
- Navy Medicine. Health Professions Scholarship Program (HPSP) and Financial Assistance Program (FAP). Accessed October 12, 2025. https://www.med.navy.mil/Accessions/Health-Professions-Scholarship-Program-HPSP-and-Financial-Assistance-Program-FAP/
- US Navy. Navy Medicine R2DA program. Accessed October 12, 2025. https://www.navy.com/navy-medicine
- US Army Medical Department. Student programs. Accessed October 12, 2025. https://goamedd.com/student-programs
- US Office of Personnel Management. General Schedule. Accessed October 12, 2025. https://www.opm.gov/policy-data-oversight/pay-leave/pay-systems/general-schedule/
- Pines Federal Employment Attorneys. Title 38 employees: medical professionals. Accessed October 12, 2025. https://www.pinesfederal.com/va-federal-employees/title-38-employees-medical-professionals/
- Military Health System. Elements of the military health system. Accessed October 11, 2025. https://www.health.mil/About-MHS/MHS-Elements
- TRICARE. Plans and eligibility. Accessed October 11, 2025. https://tricare.mil/Plans/Eligibility
- Military Benefit. TRICARE for retirees. Accessed October 11, 2025. https://www.militarybenefit.org/get-educated/tricareforretirees/
- US Department of Veterans Affairs. Eligibility for VA health care. Accessed October 11, 2025. https://www.va.gov/health-care/eligibility/
- US Department of Veterans Affairs. VA priority groups. Accessed October 11, 2025. https://www.va.gov/health-care/eligibility/priority-groups/
- Navy Medicine. Health Professions Scholarship Program (HPSP) and Financial Assistance Program (FAP). Accessed October 12, 2025. https://www.med.navy.mil/Accessions/Health-Professions-Scholarship-Program-HPSP-and-Financial-Assistance-Program-FAP/
- US Navy. Navy Medicine R2DA program. Accessed October 12, 2025. https://www.navy.com/navy-medicine
- US Army Medical Department. Student programs. Accessed October 12, 2025. https://goamedd.com/student-programs
- US Office of Personnel Management. General Schedule. Accessed October 12, 2025. https://www.opm.gov/policy-data-oversight/pay-leave/pay-systems/general-schedule/
- Pines Federal Employment Attorneys. Title 38 employees: medical professionals. Accessed October 12, 2025. https://www.pinesfederal.com/va-federal-employees/title-38-employees-medical-professionals/
Dermatology on Duty: Pathways to a Career in Military Medicine
Dermatology on Duty: Pathways to a Career in Military Medicine
PRACTICE POINTS
- Dermatologists have diverse pathways to serve the military and veteran communities, either in uniform or as civilians.
- For those considering a military career, options include medical school scholarships or direct commission after residency.
- Those who prefer to remain civilians can find employment opportunities with the Military Heath System or the Department of Veterans Affairs that provide a way to care for this population without a service commitment.
The Road Less Traveled: Why Rural Dermatology Could Be Your Path After Residency
The Road Less Traveled: Why Rural Dermatology Could Be Your Path After Residency
The myths persist: You will lack colleagues. Your practice will be thin. You must sacrifice academic engagement. In reality, rural practice offers variety, leadership opportunities, and the chance to influence the health of entire communities in profound ways. In this article, we aim to unpack what rural dermatology actually looks like as a potential career path for residents, with a focus on private-academic hybrid and hospital-based practice models.
Definitions of the term rural vary. For the US Census Bureau, it is synonymous with nonurban, and for the Office of Management and Budget, the term nonmetropolitan is preferred. The US Department of Agriculture’s Rural-Urban Commuting Area codes recognize a continuum of classifications from micropolitan to remote. In practice, the term rural covers a wide spectrum: the rolling farmlands of the Midwest, the mountains of Montana, the bayous of the South, the Native American reservations in New Mexico, and everything in between. It is not one uniform reality—rural America is diverse, resilient, and deeply connected.
Daily clinic flow may look familiar: a full schedule, a mix of new and established patients, and frequent simple procedures such as biopsies and corticosteroid injections. But the scope of practice is wider. You become the dermatologist for hundreds of miles in every direction, managing most conditions locally while referring select cases to subspecialty centers.
Case variety is striking. Neglected tumors, unusual inflammatory presentations, pediatric conditions, and occupational dermatoses/injuries appear alongside the routine. Each day requires flexibility, judgment, confidence, and the ability to think outside the box. You must consider how a patient’s seasonal work, such as ranching or farming, and/or their total commute time impacts the risk-benefit discussion around treatment recommendations.
Matthew P. Shaffer, MD (Salina, Kansas), who has practiced rural dermatology for more than 20 years, explained that the breadth of dermatologic cases in which he served as the expert was both exciting and intimidating, but it became clear that this was the right professional path for him (email communication, September 5, 2025). In small communities, your role extends beyond the clinic walls. You will see patients at the grocery store, the library, and school events. That continuity fosters loyalty and accountability in ways that are hard to quantify.
Many practice structures exist: independent clinics, multispecialty groups, hospital employment, and increasingly, hybrid partnerships with academic centers.
Academic institutions have recognized the importance of rural exposure, and many now collaborate with rural dermatologists. For example, Heartland Dermatology in Salina, Kansas, where 2 of the authors (B.R.L. and T.G.) practice, partners with St. Louis University in Missouri to provide a residency track and rotations in rural clinics.
Rural-based hospital systems can create similar structures. Monument Health Dermatology in Spearfish, South Dakota, is integrated into the fabric of the community’s larger rural health care model. The physician (M.E.L.) collaborates daily with primary care providers, surgeons, and oncologists through a shared electronic health record (sometimes even through telephone speed-dial given the close collegiality of small-town providers). Patients come from across 4 states, some driving 6 hours each way. Patients who once doubted whether dermatology was worth the trip will consistently return for follow-up care once trust is earned. The stability of hospital employment supports volunteer faculty positions and a free satellite clinic in partnership with a local Lakota Tribal health center. There is never a dull day: the providers see urgent add-ons daily, which keeps them on their toes but in exchange brings immense reward. This includes a recent case from rural Wyoming: a complex mixed infantile hemangioma on the mid face just entering the rapid proliferation phase. Propranolol was started immediately, as opposed to months later when it was too late—a common complication for the majority of rural patients by the time to get to a dermatologist.
Complex cases can overwhelm rural practices, and this is when the hub-and-spoke model is invaluable. Dermatologists embed in local communities as spokes, while subspecialty services such as pediatric dermatology, dermatopathology, or Mohs micrographic surgery remain centralized at hubs. The hubs can be but do not have to be academic institutions; for Heartland Dermatology in Kansas, private practices fulfill both hub and spoke roles. With that said, 10 states do not have academic dermatology programs.1 Mohs surgeons and pediatric dermatologists still can establish robust and successful independent rural subspecialty practices outside academic hubs. Christopher Gasbarre, DO (Spearfish, South Dakota), a board-certified, fellowship-trained Mohs surgeon in rural practice, advises residents to be confident in their abilities and to trust their training, noting that they often will be asked to manage complicated cases because of patient travel and cost constraints; however, clinicians should recognize their own limitations and those of nearby specialists and develop a referral network for cases that require multidisciplinary care (text communication, September 14, 2025).
The hub-and-spoke models—whether they entail an academic center as the hub with private practices as the spokes, or a network of private practices that include rural subspecialists—allows rural dermatologists to remain trusted local experts while ensuring that patients can access advanced care via a more streamlined referral process/network. The challenge is triage: what can be managed locally and what must patients travel for? As Dr. Shaffer explained, decisions about whether care is managed locally or referred to a hub often depend on the experience and comfort level of both the physician and the patient (email communication, September 5, 2025). Ultimately, continuity and trust are central. Patients rely on their local dermatologist to guide these decisions, and that guidance makes the model effective.
The idea that rural practice means being stuck in a small solo clinic is outdated. Multiple pathways exist, each with strengths and challenges. Independent private practice offers maximum autonomy and deep community integration, though financial and staffing risks are yours to manage. Hospital employment with outreach clinics provides stability, benefits, and collegiality, but bureaucracy can limit innovation and efficiency. Private equity platforms supply resources and rapid growth, but alignment with mission and autonomy must be weighed carefully. Hybrid joint ventures with hospitals combine private control and institutional support, but contracts can be complex. Locum tenens–to-permanent arrangements let you try rural life with minimal commitment, but continuity with patients may be sacrificed. A self-screener can clarify your path: How much autonomy do I want? Do I prefer predictability or variety? How important are procedures, teaching, or community roles? Answer these questions honestly and pair that insight with mentor guidance.
Launching a rural dermatology clinic is equal parts vision and structure. A focused 90-day plan can make the difference between a smooth opening and early frustration. Think in 4 domains: site selection, employment and licensing, credentialing and contracting, and operations. Even in a compressed timeline, dozens of small but crucial tasks may surface. There are resources—such as the Medical Group Management Association’s practice start-up checklist—that can provide a roadmap, ensuring no detail is overlooked as you transform a vision into a functioning clinic.2
Site Selection—First, determine whether you are opening a new standalone clinic, extending an existing practice, or creating a part-time satellite. Referral mapping with local primary care providers is essential, as is a scan of payer mix and dermatologist density in the region to ensure sustainability.
Employment and Licensing—Confirm state licensure and Drug Enforcement Administration registration and initiate hospital privileges early. These processes can stretch across the entire 90-day window, so starting immediately is critical.
Credentialing and Contracting—Applications with commercial and federal payers, along with Council for Affordable Quality Healthcare updates, often consume weeks if not months. If you plan to perform office microscopy or establish a dermatopathology laboratory, begin the Clinical Laboratory Improvement Amendments certification process in parallel.
Operations—Once the regulatory wheels are in motion, shift to building your practice infrastructure. Secure space, weigh lease vs purchase, and consider partnerships with local hospitals for shared clinic facilities. Recruit staff with dermatology-specific skills such as clinical photography and biopsy assistance. Implement an electronic health record, set up payroll and malpractice insurance, and establish supply chains for everything from liquid nitrogen to surgical trays. Decide whether revenue cycle management will be in-house or outsourced and finalize dermatopathology workflows including courier and transport agreements.
Compensation in rural dermatology mirrors that of other clinical settings: base salary with productivity bonuses, revenue pooling, or relative value unit structures. Financial planning is crucial. Develop a pro forma that models patient volume, expenses, and realistic growth. Risks exist, including payer mix, staffing, and competition, but the demand for care in underserved areas often offsets these, and communities may support practices with reduced overhead and strong loyalty. Hospital systems may add stipends for supervising advanced practitioners or outreach travel. Loan repayment programs, tax credits, and grants can further enhance packages. Consider checking with the state’s Office of Rural Health.
Career sustainability ultimately depends on more than finances. Geography, amenities, schedule flexibility, autonomy in medical decision-making, work-life balance, the value of being part of and serving a community, and other personal values will shape your “best-fit” practice model. Ask whether you can envision yourself thriving in the community you would be serving.
No one builds a rural dermatology practice alone. That is why one of the authors (M.E.L.) created the Rural Access to Dermatology Society (https://www.radsociety.org/), a nonprofit organization connecting dermatologists, residents, and medical students with a shared mission. The organization supports residents through scholarships, mentorship, and telementoring. Faculty can contribute through advocacy, residency track development, and outreach to uniquely underserved rural populations such as Native American reservations where access to dermatology care remains severely limited. Joining can be as simple as attending a webinar, finding a mentor, or volunteering at a free clinic. You do not need to launch your own clinic to get involved; you can begin by connecting with a network already laying the foundation.
Teledermatology and academic initiatives enhance rural care but do not replace in-person practice. Store-and-forward consultations extend reach but cannot match the continuity and trust of long-term patient relationships. Academic rural tracks prepare residents for unique challenges, but someone must staff the clinics. Private and hybrid models remain the backbone of rural access, where dermatologists take on the responsibility and the joy of being the local expert.
So here’s the invitation: bring one question to your mentor about rural practice and identify one rural site you could visit. The road less traveled in dermatology is closer than you think—and it might just be your path.
- Association of American Medical Colleges. ERAS Directory: Dermatology. Accessed December 11, 2025. https://systems.aamc.org/eras/erasstats/par/display.cfm?NAV_ROW=PAR&SPEC_CD=080
- Medical Group Management Association. Large group or organization practice startup checklist. Accessed December 11, 2025. https://www.mgma.com/member-tools/large-group-or-organization -practice-startup-checklist
The myths persist: You will lack colleagues. Your practice will be thin. You must sacrifice academic engagement. In reality, rural practice offers variety, leadership opportunities, and the chance to influence the health of entire communities in profound ways. In this article, we aim to unpack what rural dermatology actually looks like as a potential career path for residents, with a focus on private-academic hybrid and hospital-based practice models.
Definitions of the term rural vary. For the US Census Bureau, it is synonymous with nonurban, and for the Office of Management and Budget, the term nonmetropolitan is preferred. The US Department of Agriculture’s Rural-Urban Commuting Area codes recognize a continuum of classifications from micropolitan to remote. In practice, the term rural covers a wide spectrum: the rolling farmlands of the Midwest, the mountains of Montana, the bayous of the South, the Native American reservations in New Mexico, and everything in between. It is not one uniform reality—rural America is diverse, resilient, and deeply connected.
Daily clinic flow may look familiar: a full schedule, a mix of new and established patients, and frequent simple procedures such as biopsies and corticosteroid injections. But the scope of practice is wider. You become the dermatologist for hundreds of miles in every direction, managing most conditions locally while referring select cases to subspecialty centers.
Case variety is striking. Neglected tumors, unusual inflammatory presentations, pediatric conditions, and occupational dermatoses/injuries appear alongside the routine. Each day requires flexibility, judgment, confidence, and the ability to think outside the box. You must consider how a patient’s seasonal work, such as ranching or farming, and/or their total commute time impacts the risk-benefit discussion around treatment recommendations.
Matthew P. Shaffer, MD (Salina, Kansas), who has practiced rural dermatology for more than 20 years, explained that the breadth of dermatologic cases in which he served as the expert was both exciting and intimidating, but it became clear that this was the right professional path for him (email communication, September 5, 2025). In small communities, your role extends beyond the clinic walls. You will see patients at the grocery store, the library, and school events. That continuity fosters loyalty and accountability in ways that are hard to quantify.
Many practice structures exist: independent clinics, multispecialty groups, hospital employment, and increasingly, hybrid partnerships with academic centers.
Academic institutions have recognized the importance of rural exposure, and many now collaborate with rural dermatologists. For example, Heartland Dermatology in Salina, Kansas, where 2 of the authors (B.R.L. and T.G.) practice, partners with St. Louis University in Missouri to provide a residency track and rotations in rural clinics.
Rural-based hospital systems can create similar structures. Monument Health Dermatology in Spearfish, South Dakota, is integrated into the fabric of the community’s larger rural health care model. The physician (M.E.L.) collaborates daily with primary care providers, surgeons, and oncologists through a shared electronic health record (sometimes even through telephone speed-dial given the close collegiality of small-town providers). Patients come from across 4 states, some driving 6 hours each way. Patients who once doubted whether dermatology was worth the trip will consistently return for follow-up care once trust is earned. The stability of hospital employment supports volunteer faculty positions and a free satellite clinic in partnership with a local Lakota Tribal health center. There is never a dull day: the providers see urgent add-ons daily, which keeps them on their toes but in exchange brings immense reward. This includes a recent case from rural Wyoming: a complex mixed infantile hemangioma on the mid face just entering the rapid proliferation phase. Propranolol was started immediately, as opposed to months later when it was too late—a common complication for the majority of rural patients by the time to get to a dermatologist.
Complex cases can overwhelm rural practices, and this is when the hub-and-spoke model is invaluable. Dermatologists embed in local communities as spokes, while subspecialty services such as pediatric dermatology, dermatopathology, or Mohs micrographic surgery remain centralized at hubs. The hubs can be but do not have to be academic institutions; for Heartland Dermatology in Kansas, private practices fulfill both hub and spoke roles. With that said, 10 states do not have academic dermatology programs.1 Mohs surgeons and pediatric dermatologists still can establish robust and successful independent rural subspecialty practices outside academic hubs. Christopher Gasbarre, DO (Spearfish, South Dakota), a board-certified, fellowship-trained Mohs surgeon in rural practice, advises residents to be confident in their abilities and to trust their training, noting that they often will be asked to manage complicated cases because of patient travel and cost constraints; however, clinicians should recognize their own limitations and those of nearby specialists and develop a referral network for cases that require multidisciplinary care (text communication, September 14, 2025).
The hub-and-spoke models—whether they entail an academic center as the hub with private practices as the spokes, or a network of private practices that include rural subspecialists—allows rural dermatologists to remain trusted local experts while ensuring that patients can access advanced care via a more streamlined referral process/network. The challenge is triage: what can be managed locally and what must patients travel for? As Dr. Shaffer explained, decisions about whether care is managed locally or referred to a hub often depend on the experience and comfort level of both the physician and the patient (email communication, September 5, 2025). Ultimately, continuity and trust are central. Patients rely on their local dermatologist to guide these decisions, and that guidance makes the model effective.
The idea that rural practice means being stuck in a small solo clinic is outdated. Multiple pathways exist, each with strengths and challenges. Independent private practice offers maximum autonomy and deep community integration, though financial and staffing risks are yours to manage. Hospital employment with outreach clinics provides stability, benefits, and collegiality, but bureaucracy can limit innovation and efficiency. Private equity platforms supply resources and rapid growth, but alignment with mission and autonomy must be weighed carefully. Hybrid joint ventures with hospitals combine private control and institutional support, but contracts can be complex. Locum tenens–to-permanent arrangements let you try rural life with minimal commitment, but continuity with patients may be sacrificed. A self-screener can clarify your path: How much autonomy do I want? Do I prefer predictability or variety? How important are procedures, teaching, or community roles? Answer these questions honestly and pair that insight with mentor guidance.
Launching a rural dermatology clinic is equal parts vision and structure. A focused 90-day plan can make the difference between a smooth opening and early frustration. Think in 4 domains: site selection, employment and licensing, credentialing and contracting, and operations. Even in a compressed timeline, dozens of small but crucial tasks may surface. There are resources—such as the Medical Group Management Association’s practice start-up checklist—that can provide a roadmap, ensuring no detail is overlooked as you transform a vision into a functioning clinic.2
Site Selection—First, determine whether you are opening a new standalone clinic, extending an existing practice, or creating a part-time satellite. Referral mapping with local primary care providers is essential, as is a scan of payer mix and dermatologist density in the region to ensure sustainability.
Employment and Licensing—Confirm state licensure and Drug Enforcement Administration registration and initiate hospital privileges early. These processes can stretch across the entire 90-day window, so starting immediately is critical.
Credentialing and Contracting—Applications with commercial and federal payers, along with Council for Affordable Quality Healthcare updates, often consume weeks if not months. If you plan to perform office microscopy or establish a dermatopathology laboratory, begin the Clinical Laboratory Improvement Amendments certification process in parallel.
Operations—Once the regulatory wheels are in motion, shift to building your practice infrastructure. Secure space, weigh lease vs purchase, and consider partnerships with local hospitals for shared clinic facilities. Recruit staff with dermatology-specific skills such as clinical photography and biopsy assistance. Implement an electronic health record, set up payroll and malpractice insurance, and establish supply chains for everything from liquid nitrogen to surgical trays. Decide whether revenue cycle management will be in-house or outsourced and finalize dermatopathology workflows including courier and transport agreements.
Compensation in rural dermatology mirrors that of other clinical settings: base salary with productivity bonuses, revenue pooling, or relative value unit structures. Financial planning is crucial. Develop a pro forma that models patient volume, expenses, and realistic growth. Risks exist, including payer mix, staffing, and competition, but the demand for care in underserved areas often offsets these, and communities may support practices with reduced overhead and strong loyalty. Hospital systems may add stipends for supervising advanced practitioners or outreach travel. Loan repayment programs, tax credits, and grants can further enhance packages. Consider checking with the state’s Office of Rural Health.
Career sustainability ultimately depends on more than finances. Geography, amenities, schedule flexibility, autonomy in medical decision-making, work-life balance, the value of being part of and serving a community, and other personal values will shape your “best-fit” practice model. Ask whether you can envision yourself thriving in the community you would be serving.
No one builds a rural dermatology practice alone. That is why one of the authors (M.E.L.) created the Rural Access to Dermatology Society (https://www.radsociety.org/), a nonprofit organization connecting dermatologists, residents, and medical students with a shared mission. The organization supports residents through scholarships, mentorship, and telementoring. Faculty can contribute through advocacy, residency track development, and outreach to uniquely underserved rural populations such as Native American reservations where access to dermatology care remains severely limited. Joining can be as simple as attending a webinar, finding a mentor, or volunteering at a free clinic. You do not need to launch your own clinic to get involved; you can begin by connecting with a network already laying the foundation.
Teledermatology and academic initiatives enhance rural care but do not replace in-person practice. Store-and-forward consultations extend reach but cannot match the continuity and trust of long-term patient relationships. Academic rural tracks prepare residents for unique challenges, but someone must staff the clinics. Private and hybrid models remain the backbone of rural access, where dermatologists take on the responsibility and the joy of being the local expert.
So here’s the invitation: bring one question to your mentor about rural practice and identify one rural site you could visit. The road less traveled in dermatology is closer than you think—and it might just be your path.
The myths persist: You will lack colleagues. Your practice will be thin. You must sacrifice academic engagement. In reality, rural practice offers variety, leadership opportunities, and the chance to influence the health of entire communities in profound ways. In this article, we aim to unpack what rural dermatology actually looks like as a potential career path for residents, with a focus on private-academic hybrid and hospital-based practice models.
Definitions of the term rural vary. For the US Census Bureau, it is synonymous with nonurban, and for the Office of Management and Budget, the term nonmetropolitan is preferred. The US Department of Agriculture’s Rural-Urban Commuting Area codes recognize a continuum of classifications from micropolitan to remote. In practice, the term rural covers a wide spectrum: the rolling farmlands of the Midwest, the mountains of Montana, the bayous of the South, the Native American reservations in New Mexico, and everything in between. It is not one uniform reality—rural America is diverse, resilient, and deeply connected.
Daily clinic flow may look familiar: a full schedule, a mix of new and established patients, and frequent simple procedures such as biopsies and corticosteroid injections. But the scope of practice is wider. You become the dermatologist for hundreds of miles in every direction, managing most conditions locally while referring select cases to subspecialty centers.
Case variety is striking. Neglected tumors, unusual inflammatory presentations, pediatric conditions, and occupational dermatoses/injuries appear alongside the routine. Each day requires flexibility, judgment, confidence, and the ability to think outside the box. You must consider how a patient’s seasonal work, such as ranching or farming, and/or their total commute time impacts the risk-benefit discussion around treatment recommendations.
Matthew P. Shaffer, MD (Salina, Kansas), who has practiced rural dermatology for more than 20 years, explained that the breadth of dermatologic cases in which he served as the expert was both exciting and intimidating, but it became clear that this was the right professional path for him (email communication, September 5, 2025). In small communities, your role extends beyond the clinic walls. You will see patients at the grocery store, the library, and school events. That continuity fosters loyalty and accountability in ways that are hard to quantify.
Many practice structures exist: independent clinics, multispecialty groups, hospital employment, and increasingly, hybrid partnerships with academic centers.
Academic institutions have recognized the importance of rural exposure, and many now collaborate with rural dermatologists. For example, Heartland Dermatology in Salina, Kansas, where 2 of the authors (B.R.L. and T.G.) practice, partners with St. Louis University in Missouri to provide a residency track and rotations in rural clinics.
Rural-based hospital systems can create similar structures. Monument Health Dermatology in Spearfish, South Dakota, is integrated into the fabric of the community’s larger rural health care model. The physician (M.E.L.) collaborates daily with primary care providers, surgeons, and oncologists through a shared electronic health record (sometimes even through telephone speed-dial given the close collegiality of small-town providers). Patients come from across 4 states, some driving 6 hours each way. Patients who once doubted whether dermatology was worth the trip will consistently return for follow-up care once trust is earned. The stability of hospital employment supports volunteer faculty positions and a free satellite clinic in partnership with a local Lakota Tribal health center. There is never a dull day: the providers see urgent add-ons daily, which keeps them on their toes but in exchange brings immense reward. This includes a recent case from rural Wyoming: a complex mixed infantile hemangioma on the mid face just entering the rapid proliferation phase. Propranolol was started immediately, as opposed to months later when it was too late—a common complication for the majority of rural patients by the time to get to a dermatologist.
Complex cases can overwhelm rural practices, and this is when the hub-and-spoke model is invaluable. Dermatologists embed in local communities as spokes, while subspecialty services such as pediatric dermatology, dermatopathology, or Mohs micrographic surgery remain centralized at hubs. The hubs can be but do not have to be academic institutions; for Heartland Dermatology in Kansas, private practices fulfill both hub and spoke roles. With that said, 10 states do not have academic dermatology programs.1 Mohs surgeons and pediatric dermatologists still can establish robust and successful independent rural subspecialty practices outside academic hubs. Christopher Gasbarre, DO (Spearfish, South Dakota), a board-certified, fellowship-trained Mohs surgeon in rural practice, advises residents to be confident in their abilities and to trust their training, noting that they often will be asked to manage complicated cases because of patient travel and cost constraints; however, clinicians should recognize their own limitations and those of nearby specialists and develop a referral network for cases that require multidisciplinary care (text communication, September 14, 2025).
The hub-and-spoke models—whether they entail an academic center as the hub with private practices as the spokes, or a network of private practices that include rural subspecialists—allows rural dermatologists to remain trusted local experts while ensuring that patients can access advanced care via a more streamlined referral process/network. The challenge is triage: what can be managed locally and what must patients travel for? As Dr. Shaffer explained, decisions about whether care is managed locally or referred to a hub often depend on the experience and comfort level of both the physician and the patient (email communication, September 5, 2025). Ultimately, continuity and trust are central. Patients rely on their local dermatologist to guide these decisions, and that guidance makes the model effective.
The idea that rural practice means being stuck in a small solo clinic is outdated. Multiple pathways exist, each with strengths and challenges. Independent private practice offers maximum autonomy and deep community integration, though financial and staffing risks are yours to manage. Hospital employment with outreach clinics provides stability, benefits, and collegiality, but bureaucracy can limit innovation and efficiency. Private equity platforms supply resources and rapid growth, but alignment with mission and autonomy must be weighed carefully. Hybrid joint ventures with hospitals combine private control and institutional support, but contracts can be complex. Locum tenens–to-permanent arrangements let you try rural life with minimal commitment, but continuity with patients may be sacrificed. A self-screener can clarify your path: How much autonomy do I want? Do I prefer predictability or variety? How important are procedures, teaching, or community roles? Answer these questions honestly and pair that insight with mentor guidance.
Launching a rural dermatology clinic is equal parts vision and structure. A focused 90-day plan can make the difference between a smooth opening and early frustration. Think in 4 domains: site selection, employment and licensing, credentialing and contracting, and operations. Even in a compressed timeline, dozens of small but crucial tasks may surface. There are resources—such as the Medical Group Management Association’s practice start-up checklist—that can provide a roadmap, ensuring no detail is overlooked as you transform a vision into a functioning clinic.2
Site Selection—First, determine whether you are opening a new standalone clinic, extending an existing practice, or creating a part-time satellite. Referral mapping with local primary care providers is essential, as is a scan of payer mix and dermatologist density in the region to ensure sustainability.
Employment and Licensing—Confirm state licensure and Drug Enforcement Administration registration and initiate hospital privileges early. These processes can stretch across the entire 90-day window, so starting immediately is critical.
Credentialing and Contracting—Applications with commercial and federal payers, along with Council for Affordable Quality Healthcare updates, often consume weeks if not months. If you plan to perform office microscopy or establish a dermatopathology laboratory, begin the Clinical Laboratory Improvement Amendments certification process in parallel.
Operations—Once the regulatory wheels are in motion, shift to building your practice infrastructure. Secure space, weigh lease vs purchase, and consider partnerships with local hospitals for shared clinic facilities. Recruit staff with dermatology-specific skills such as clinical photography and biopsy assistance. Implement an electronic health record, set up payroll and malpractice insurance, and establish supply chains for everything from liquid nitrogen to surgical trays. Decide whether revenue cycle management will be in-house or outsourced and finalize dermatopathology workflows including courier and transport agreements.
Compensation in rural dermatology mirrors that of other clinical settings: base salary with productivity bonuses, revenue pooling, or relative value unit structures. Financial planning is crucial. Develop a pro forma that models patient volume, expenses, and realistic growth. Risks exist, including payer mix, staffing, and competition, but the demand for care in underserved areas often offsets these, and communities may support practices with reduced overhead and strong loyalty. Hospital systems may add stipends for supervising advanced practitioners or outreach travel. Loan repayment programs, tax credits, and grants can further enhance packages. Consider checking with the state’s Office of Rural Health.
Career sustainability ultimately depends on more than finances. Geography, amenities, schedule flexibility, autonomy in medical decision-making, work-life balance, the value of being part of and serving a community, and other personal values will shape your “best-fit” practice model. Ask whether you can envision yourself thriving in the community you would be serving.
No one builds a rural dermatology practice alone. That is why one of the authors (M.E.L.) created the Rural Access to Dermatology Society (https://www.radsociety.org/), a nonprofit organization connecting dermatologists, residents, and medical students with a shared mission. The organization supports residents through scholarships, mentorship, and telementoring. Faculty can contribute through advocacy, residency track development, and outreach to uniquely underserved rural populations such as Native American reservations where access to dermatology care remains severely limited. Joining can be as simple as attending a webinar, finding a mentor, or volunteering at a free clinic. You do not need to launch your own clinic to get involved; you can begin by connecting with a network already laying the foundation.
Teledermatology and academic initiatives enhance rural care but do not replace in-person practice. Store-and-forward consultations extend reach but cannot match the continuity and trust of long-term patient relationships. Academic rural tracks prepare residents for unique challenges, but someone must staff the clinics. Private and hybrid models remain the backbone of rural access, where dermatologists take on the responsibility and the joy of being the local expert.
So here’s the invitation: bring one question to your mentor about rural practice and identify one rural site you could visit. The road less traveled in dermatology is closer than you think—and it might just be your path.
- Association of American Medical Colleges. ERAS Directory: Dermatology. Accessed December 11, 2025. https://systems.aamc.org/eras/erasstats/par/display.cfm?NAV_ROW=PAR&SPEC_CD=080
- Medical Group Management Association. Large group or organization practice startup checklist. Accessed December 11, 2025. https://www.mgma.com/member-tools/large-group-or-organization -practice-startup-checklist
- Association of American Medical Colleges. ERAS Directory: Dermatology. Accessed December 11, 2025. https://systems.aamc.org/eras/erasstats/par/display.cfm?NAV_ROW=PAR&SPEC_CD=080
- Medical Group Management Association. Large group or organization practice startup checklist. Accessed December 11, 2025. https://www.mgma.com/member-tools/large-group-or-organization -practice-startup-checklist
The Road Less Traveled: Why Rural Dermatology Could Be Your Path After Residency
The Road Less Traveled: Why Rural Dermatology Could Be Your Path After Residency
Office-Based Endoscopy Model Offers Way Forward for Outpatient GI
After decades of successful growth, the ambulatory surgery center (ASC) model may be turning a corner, opening up opportunity for office-based endoscopy models, according to a recent practice management editorial published in Clinical Gastroenterology and Hepatology.
Although office endoscopy has been an option, it hasn’t always felt practical or financially viable in the past. However, the paradigm appears to be shifting as ASC-based revenue streams show signs of stress and fail to keep pace with inflation. As healthcare regulatory and economic environments continue to change, gastroenterologists need a new model to support equity, efficiency, and growth in gastrointestinal (GI) care delivery, the authors wrote.
“Through the course of my 40-year career, I’ve been hit with a lot of changes related to regulations, insurance, and the market. You can’t stay entrenched in your old ways. You have to remain pivotable and come up with new strategic positions,” said Lawrence Kosinski, MD, AGAF, lead author and founder of SonarMD and VOCnomics.
During his private practice career, Kosinski built one of the largest GI practices in Illinois, which had seven ASCs and is now part of one of the largest GI groups in the country. Across 30 years of experience with ASCs, Kosinski has watched the reimbursement for professional services decline, as well as for added revenue streams such as pathology and anesthesia.
Looking for a better solution, Kosinski served on the governing board for the American Gastroenterological Association as the councilor for development and growth. During the past 3 years, he has spoken with GI practices and worked with a national anesthesia company — Ambulatory Anesthesia Care — to better understand the office endoscopy setting.
“In the ’90s, all I wanted was to have an ASC because that was in vogue,” he said. “But if you look critically at what has happened to the business of outpatient endoscopy in the past 25 years, you’ll see that professional fees haven’t kept up, and trying to replace that lost revenue is a losing battle.”
Considering Financial Shifts
Since 2001, professional reimbursement for colonoscopies has fallen by more than 40% while ASC revenue has risen, decreasing the percentage of revenue from professional fees (from 34% to 23%) and increasing the facility component (from 44% to 60%), Kosinski and colleagues wrote.
When looking at profit, compression of professional service fees appears even greater, especially with surging costs of anesthesia care due to high demand and provider shortages. Beyond that, about a third of ASCs are owned at least partially by national entities, as of 2024, leading to even lower realization of profit.
“The profit margins have really been crushed, so what is a GI doc to do? Go where there is opportunity,” Kosinski said. “The difference between hospitals and ASCs has been compressed, so what about the office?”
The proposed 2026 Medicare Physician Fee Schedule includes a 14% increase in reimbursement for office-based procedures, including endoscopy, as well as a 7% decrease for facility-based procedures.
In several states — such as Illinois, Oregon, Virginia, Washington, and Wisconsin — health plans are introducing programs to promote the transition of outpatient endoscopy to office settings rather than hospital-based or ASC-based settings due to costs, the authors wrote.
“The decision to start offering office-based endoscopy services was an easy one for our practice, as it provides a way for us to provide patients convenient, easy-to-access endoscopy that is high quality yet much more affordable than hospital-based settings,” said Neil Gupta, MD, managing partner at Midwest Digestive Health & Nutrition in Des Plaines, Illinois.
The practice has used office-based endoscopy for nearly 2 years, Gupta said, performing about 5000 GI endoscopy procedures per year.
“As we all try to find better ways to provide high-quality but affordable care for patients, office-based endoscopy is a great way to help achieve those goals,” he said. “Healthcare professionals and patients should all be asking, ‘What type of site am I getting my GI endoscopy scheduled at — hospital, surgery center, or physician’s office?’”
Regaining Autonomy and Time
Beyond the financial dynamics, , Kosinski and colleagues wrote.
Looking ahead, office-based models can also provide the agility and infrastructure to compete in value-based care models, they wrote. In turn, value-based models can create relevance and resilience in a continually changing healthcare environment.
Without the involvement of ASC managers, investors, or health system partners, physicians retain control of scheduling, clinical protocols, financial decisions, and operational workflows, the authors wrote. This could create better alignment with personal preferences, clinical judgment, and patient needs, they noted.
“GI physicians should no longer feel trapped in a hospital setting where they lack independence and influence over decision-making,” said Rock Rockett, PhD, owner and principal consultant of Rockett Healthcare Strategies, which partners with GI groups nationwide to help with development, accreditation, and payer contracting for office endoscopy.
“GI physicians should also no longer feel trapped in a ‘bad marriage’ with partners in an ASC or partners in a practice who create a difficult work environment,” he said. “The viability of office endoscopy allows them to strike out on their own or set up a new partnership on more equitable terms that are attractive for them.”
Patient safety and quality also appear to be similar or better in office-based settings, based on benchmarking data analyzed so far. Hospital transfers were lower, falls were similar, and patient experience was positive, the authors wrote.
At the same time, Kosinski and colleagues noted the difficulty in shifting to office-based models. Most practices have committed to ASCs, for instance, and adding an office-based room can be challenging. Otherwise, practices already use their available office space and don’t have extra rooms available. In that case, an office endoscopy suite may be best suited for expansion sites, allowing practices to grow into new service areas, they wrote.
“You can’t fight the market. You have to focus on what the market wants and needs,” Kosinski said. “To do that, you have to be able to pivot and change direction, looking for new ways to change your mission. This could be an option to do that.”
Kosinski, Gupta, and Rockett declared having no conflicts of interest other than their current employments.
A version of this article appeared on Medscape.com.
After decades of successful growth, the ambulatory surgery center (ASC) model may be turning a corner, opening up opportunity for office-based endoscopy models, according to a recent practice management editorial published in Clinical Gastroenterology and Hepatology.
Although office endoscopy has been an option, it hasn’t always felt practical or financially viable in the past. However, the paradigm appears to be shifting as ASC-based revenue streams show signs of stress and fail to keep pace with inflation. As healthcare regulatory and economic environments continue to change, gastroenterologists need a new model to support equity, efficiency, and growth in gastrointestinal (GI) care delivery, the authors wrote.
“Through the course of my 40-year career, I’ve been hit with a lot of changes related to regulations, insurance, and the market. You can’t stay entrenched in your old ways. You have to remain pivotable and come up with new strategic positions,” said Lawrence Kosinski, MD, AGAF, lead author and founder of SonarMD and VOCnomics.
During his private practice career, Kosinski built one of the largest GI practices in Illinois, which had seven ASCs and is now part of one of the largest GI groups in the country. Across 30 years of experience with ASCs, Kosinski has watched the reimbursement for professional services decline, as well as for added revenue streams such as pathology and anesthesia.
Looking for a better solution, Kosinski served on the governing board for the American Gastroenterological Association as the councilor for development and growth. During the past 3 years, he has spoken with GI practices and worked with a national anesthesia company — Ambulatory Anesthesia Care — to better understand the office endoscopy setting.
“In the ’90s, all I wanted was to have an ASC because that was in vogue,” he said. “But if you look critically at what has happened to the business of outpatient endoscopy in the past 25 years, you’ll see that professional fees haven’t kept up, and trying to replace that lost revenue is a losing battle.”
Considering Financial Shifts
Since 2001, professional reimbursement for colonoscopies has fallen by more than 40% while ASC revenue has risen, decreasing the percentage of revenue from professional fees (from 34% to 23%) and increasing the facility component (from 44% to 60%), Kosinski and colleagues wrote.
When looking at profit, compression of professional service fees appears even greater, especially with surging costs of anesthesia care due to high demand and provider shortages. Beyond that, about a third of ASCs are owned at least partially by national entities, as of 2024, leading to even lower realization of profit.
“The profit margins have really been crushed, so what is a GI doc to do? Go where there is opportunity,” Kosinski said. “The difference between hospitals and ASCs has been compressed, so what about the office?”
The proposed 2026 Medicare Physician Fee Schedule includes a 14% increase in reimbursement for office-based procedures, including endoscopy, as well as a 7% decrease for facility-based procedures.
In several states — such as Illinois, Oregon, Virginia, Washington, and Wisconsin — health plans are introducing programs to promote the transition of outpatient endoscopy to office settings rather than hospital-based or ASC-based settings due to costs, the authors wrote.
“The decision to start offering office-based endoscopy services was an easy one for our practice, as it provides a way for us to provide patients convenient, easy-to-access endoscopy that is high quality yet much more affordable than hospital-based settings,” said Neil Gupta, MD, managing partner at Midwest Digestive Health & Nutrition in Des Plaines, Illinois.
The practice has used office-based endoscopy for nearly 2 years, Gupta said, performing about 5000 GI endoscopy procedures per year.
“As we all try to find better ways to provide high-quality but affordable care for patients, office-based endoscopy is a great way to help achieve those goals,” he said. “Healthcare professionals and patients should all be asking, ‘What type of site am I getting my GI endoscopy scheduled at — hospital, surgery center, or physician’s office?’”
Regaining Autonomy and Time
Beyond the financial dynamics, , Kosinski and colleagues wrote.
Looking ahead, office-based models can also provide the agility and infrastructure to compete in value-based care models, they wrote. In turn, value-based models can create relevance and resilience in a continually changing healthcare environment.
Without the involvement of ASC managers, investors, or health system partners, physicians retain control of scheduling, clinical protocols, financial decisions, and operational workflows, the authors wrote. This could create better alignment with personal preferences, clinical judgment, and patient needs, they noted.
“GI physicians should no longer feel trapped in a hospital setting where they lack independence and influence over decision-making,” said Rock Rockett, PhD, owner and principal consultant of Rockett Healthcare Strategies, which partners with GI groups nationwide to help with development, accreditation, and payer contracting for office endoscopy.
“GI physicians should also no longer feel trapped in a ‘bad marriage’ with partners in an ASC or partners in a practice who create a difficult work environment,” he said. “The viability of office endoscopy allows them to strike out on their own or set up a new partnership on more equitable terms that are attractive for them.”
Patient safety and quality also appear to be similar or better in office-based settings, based on benchmarking data analyzed so far. Hospital transfers were lower, falls were similar, and patient experience was positive, the authors wrote.
At the same time, Kosinski and colleagues noted the difficulty in shifting to office-based models. Most practices have committed to ASCs, for instance, and adding an office-based room can be challenging. Otherwise, practices already use their available office space and don’t have extra rooms available. In that case, an office endoscopy suite may be best suited for expansion sites, allowing practices to grow into new service areas, they wrote.
“You can’t fight the market. You have to focus on what the market wants and needs,” Kosinski said. “To do that, you have to be able to pivot and change direction, looking for new ways to change your mission. This could be an option to do that.”
Kosinski, Gupta, and Rockett declared having no conflicts of interest other than their current employments.
A version of this article appeared on Medscape.com.
After decades of successful growth, the ambulatory surgery center (ASC) model may be turning a corner, opening up opportunity for office-based endoscopy models, according to a recent practice management editorial published in Clinical Gastroenterology and Hepatology.
Although office endoscopy has been an option, it hasn’t always felt practical or financially viable in the past. However, the paradigm appears to be shifting as ASC-based revenue streams show signs of stress and fail to keep pace with inflation. As healthcare regulatory and economic environments continue to change, gastroenterologists need a new model to support equity, efficiency, and growth in gastrointestinal (GI) care delivery, the authors wrote.
“Through the course of my 40-year career, I’ve been hit with a lot of changes related to regulations, insurance, and the market. You can’t stay entrenched in your old ways. You have to remain pivotable and come up with new strategic positions,” said Lawrence Kosinski, MD, AGAF, lead author and founder of SonarMD and VOCnomics.
During his private practice career, Kosinski built one of the largest GI practices in Illinois, which had seven ASCs and is now part of one of the largest GI groups in the country. Across 30 years of experience with ASCs, Kosinski has watched the reimbursement for professional services decline, as well as for added revenue streams such as pathology and anesthesia.
Looking for a better solution, Kosinski served on the governing board for the American Gastroenterological Association as the councilor for development and growth. During the past 3 years, he has spoken with GI practices and worked with a national anesthesia company — Ambulatory Anesthesia Care — to better understand the office endoscopy setting.
“In the ’90s, all I wanted was to have an ASC because that was in vogue,” he said. “But if you look critically at what has happened to the business of outpatient endoscopy in the past 25 years, you’ll see that professional fees haven’t kept up, and trying to replace that lost revenue is a losing battle.”
Considering Financial Shifts
Since 2001, professional reimbursement for colonoscopies has fallen by more than 40% while ASC revenue has risen, decreasing the percentage of revenue from professional fees (from 34% to 23%) and increasing the facility component (from 44% to 60%), Kosinski and colleagues wrote.
When looking at profit, compression of professional service fees appears even greater, especially with surging costs of anesthesia care due to high demand and provider shortages. Beyond that, about a third of ASCs are owned at least partially by national entities, as of 2024, leading to even lower realization of profit.
“The profit margins have really been crushed, so what is a GI doc to do? Go where there is opportunity,” Kosinski said. “The difference between hospitals and ASCs has been compressed, so what about the office?”
The proposed 2026 Medicare Physician Fee Schedule includes a 14% increase in reimbursement for office-based procedures, including endoscopy, as well as a 7% decrease for facility-based procedures.
In several states — such as Illinois, Oregon, Virginia, Washington, and Wisconsin — health plans are introducing programs to promote the transition of outpatient endoscopy to office settings rather than hospital-based or ASC-based settings due to costs, the authors wrote.
“The decision to start offering office-based endoscopy services was an easy one for our practice, as it provides a way for us to provide patients convenient, easy-to-access endoscopy that is high quality yet much more affordable than hospital-based settings,” said Neil Gupta, MD, managing partner at Midwest Digestive Health & Nutrition in Des Plaines, Illinois.
The practice has used office-based endoscopy for nearly 2 years, Gupta said, performing about 5000 GI endoscopy procedures per year.
“As we all try to find better ways to provide high-quality but affordable care for patients, office-based endoscopy is a great way to help achieve those goals,” he said. “Healthcare professionals and patients should all be asking, ‘What type of site am I getting my GI endoscopy scheduled at — hospital, surgery center, or physician’s office?’”
Regaining Autonomy and Time
Beyond the financial dynamics, , Kosinski and colleagues wrote.
Looking ahead, office-based models can also provide the agility and infrastructure to compete in value-based care models, they wrote. In turn, value-based models can create relevance and resilience in a continually changing healthcare environment.
Without the involvement of ASC managers, investors, or health system partners, physicians retain control of scheduling, clinical protocols, financial decisions, and operational workflows, the authors wrote. This could create better alignment with personal preferences, clinical judgment, and patient needs, they noted.
“GI physicians should no longer feel trapped in a hospital setting where they lack independence and influence over decision-making,” said Rock Rockett, PhD, owner and principal consultant of Rockett Healthcare Strategies, which partners with GI groups nationwide to help with development, accreditation, and payer contracting for office endoscopy.
“GI physicians should also no longer feel trapped in a ‘bad marriage’ with partners in an ASC or partners in a practice who create a difficult work environment,” he said. “The viability of office endoscopy allows them to strike out on their own or set up a new partnership on more equitable terms that are attractive for them.”
Patient safety and quality also appear to be similar or better in office-based settings, based on benchmarking data analyzed so far. Hospital transfers were lower, falls were similar, and patient experience was positive, the authors wrote.
At the same time, Kosinski and colleagues noted the difficulty in shifting to office-based models. Most practices have committed to ASCs, for instance, and adding an office-based room can be challenging. Otherwise, practices already use their available office space and don’t have extra rooms available. In that case, an office endoscopy suite may be best suited for expansion sites, allowing practices to grow into new service areas, they wrote.
“You can’t fight the market. You have to focus on what the market wants and needs,” Kosinski said. “To do that, you have to be able to pivot and change direction, looking for new ways to change your mission. This could be an option to do that.”
Kosinski, Gupta, and Rockett declared having no conflicts of interest other than their current employments.
A version of this article appeared on Medscape.com.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
‘So You Have an Idea…’: A Practical Guide to Tech and Device Development for the Early Career GI
You are in the middle of a busy clinic day and think, “there has to be a better way to do this.” Suddenly, a better way to do something becomes obvious. Maybe it’s a tool that simplifies documentation, a device that improves patient comfort, or an app that bridges a clinical gap. Many physicians, especially early career gastroenterologists, have ideas like this, but few know what to do next.
This article is for the curious innovator at the beginning of their clinical career. It offers practical, real-world guidance on developing a clinical product: whether that be hardware, software, or a hybrid. It outlines what questions to ask, who to consult, and how to protect your work, using personal insights and business principles learned through lived experience.
1. Understand Intellectual Property (IP): Know Its Value and Ownership
What is IP?
Intellectual property refers to your original creations: inventions, designs, software, and more. This is what you want to protect legally through patents, trademarks, or copyrights.
Who owns your idea?
This is the first and most important question to ask. If you are employed (especially by a hospital or academic center), your contract may already give your employer rights to any inventions you create, even those developed in your personal time.
What to ask:
- Does my employment contract include an “assignment of inventions” clause?
- Does the institution claim rights to anything developed with institutional resources?
- Are there moonlighting or external activity policies that affect this?
If you are developing an idea on your personal time, with your own resources, and outside your scope of clinical duties, it might still be considered “theirs” under some contracts. Early legal consultation is critical. A specialized IP attorney can help you understand what you own and how to protect it. This should be done early, ideally before you start building anything.
2. Lawyers Aren’t Optional: They’re Essential Early Partners
You do not need a full legal team, but you do need a lawyer early. An early consultation with an IP attorney can clarify your rights, guide your filing process (e.g. provisional patents), and help you avoid costly missteps.
Do this before sharing your idea publicly, including in academic presentations, pitch competitions, or even on social media. Public disclosure can start a clock ticking for application to protect your IP.
3. Build a Founding Team with Intent
Think of your startup team like a long-term relationship: you’re committing to build something together through uncertainty, tension, and change.
Strong early-stage teams often include:
- The Visionary – understands the clinical need and vision
- The Builder – engineer, developer, or designer
- The Doer – project manager or operations lead
Before forming a company, clearly define:
- Ownership (equity percentages)
- Roles and responsibilities
- Time commitments
- What happens if someone exits
Have these discussions early and document your agreements. Avoid informal “handshake” deals that can lead to serious disputes later.
4. You Don’t Need to Know Everything on Day One
You do not need to know how to write code, build a prototype, or get FDA clearance on day one. Successful innovators are humble learners. Use a Minimum Viable Product (MVP), a simple, functional version of your idea, to test assumptions and gather feedback. Iterate based on what you learn. Do not chase perfection; pursue progress. Consider using online accelerators like Y Combinator’s startup school or AGA’s Center for GI Innovation and Technology.
5. Incubators: Use them Strategically
Incubators can offer mentorship, seed funding, legal support, and technical resources, but they vary widely in value (see Table 1). Many may want equity, and not all offer when you truly need.
Ask Yourself:
- Do I need technical help, business mentorship, or just accountability?
- What does this incubator offer in terms of IP protection, exposure, and connections?
- Do I understand the equity trade-off?
- What services and funding do they provide?
- Do they take equity? How much and when?
- What’s their track record with similar ventures?
- Are their incentives aligned with your vision?
6. Academic Institutions: Partners or Pitfalls?
Universities can provide credibility, resources, and early funding through their tech transfer office (TTO).
Key Questions to Ask:
- Will my IP be managed by the TTO?
- How much say do I have in licensing decisions?
- Are there royalty-sharing agreements in place?
- Can I form a startup while employed here?
You may need to negotiate if you want to commercialize your idea independently.
7. Do it for Purpose, Not Payday
Most founders end up owning only a small percentage of their company by the time a product reaches the market. Do not expect to get rich. Do it because it solves a problem you care about. If it happens to come with a nice paycheck, then that is an added bonus.
Your clinical training and insight give you a unique edge. You already know what’s broken. Use that as your compass.
Conclusion
Innovation isn’t about brilliance, it’s about curiosity, structure, and tenacity (see Table 2). Start small. Protect your work. Choose the right partners. Most importantly, stay anchored in your mission to make GI care better.
Dr. Muratore is based at UNC Rex Digestive Health, Raleigh, North Carolina. She has no conflicts related to this article. Dr. Wechsler is based at the University of North Carolina at Chapel Hill, Chapel Hill, North Carolina. She holds a patent assigned to Trustees of Dartmouth College. Dr. Shah is based at the University of Michigan, Ann Arbor, Michigan. He consults for Ardelyx, Laborie, Neuraxis, Salix, Sanofi, and Takeda and holds a patent with the Regents of the University of Michigan.
You are in the middle of a busy clinic day and think, “there has to be a better way to do this.” Suddenly, a better way to do something becomes obvious. Maybe it’s a tool that simplifies documentation, a device that improves patient comfort, or an app that bridges a clinical gap. Many physicians, especially early career gastroenterologists, have ideas like this, but few know what to do next.
This article is for the curious innovator at the beginning of their clinical career. It offers practical, real-world guidance on developing a clinical product: whether that be hardware, software, or a hybrid. It outlines what questions to ask, who to consult, and how to protect your work, using personal insights and business principles learned through lived experience.
1. Understand Intellectual Property (IP): Know Its Value and Ownership
What is IP?
Intellectual property refers to your original creations: inventions, designs, software, and more. This is what you want to protect legally through patents, trademarks, or copyrights.
Who owns your idea?
This is the first and most important question to ask. If you are employed (especially by a hospital or academic center), your contract may already give your employer rights to any inventions you create, even those developed in your personal time.
What to ask:
- Does my employment contract include an “assignment of inventions” clause?
- Does the institution claim rights to anything developed with institutional resources?
- Are there moonlighting or external activity policies that affect this?
If you are developing an idea on your personal time, with your own resources, and outside your scope of clinical duties, it might still be considered “theirs” under some contracts. Early legal consultation is critical. A specialized IP attorney can help you understand what you own and how to protect it. This should be done early, ideally before you start building anything.
2. Lawyers Aren’t Optional: They’re Essential Early Partners
You do not need a full legal team, but you do need a lawyer early. An early consultation with an IP attorney can clarify your rights, guide your filing process (e.g. provisional patents), and help you avoid costly missteps.
Do this before sharing your idea publicly, including in academic presentations, pitch competitions, or even on social media. Public disclosure can start a clock ticking for application to protect your IP.
3. Build a Founding Team with Intent
Think of your startup team like a long-term relationship: you’re committing to build something together through uncertainty, tension, and change.
Strong early-stage teams often include:
- The Visionary – understands the clinical need and vision
- The Builder – engineer, developer, or designer
- The Doer – project manager or operations lead
Before forming a company, clearly define:
- Ownership (equity percentages)
- Roles and responsibilities
- Time commitments
- What happens if someone exits
Have these discussions early and document your agreements. Avoid informal “handshake” deals that can lead to serious disputes later.
4. You Don’t Need to Know Everything on Day One
You do not need to know how to write code, build a prototype, or get FDA clearance on day one. Successful innovators are humble learners. Use a Minimum Viable Product (MVP), a simple, functional version of your idea, to test assumptions and gather feedback. Iterate based on what you learn. Do not chase perfection; pursue progress. Consider using online accelerators like Y Combinator’s startup school or AGA’s Center for GI Innovation and Technology.
5. Incubators: Use them Strategically
Incubators can offer mentorship, seed funding, legal support, and technical resources, but they vary widely in value (see Table 1). Many may want equity, and not all offer when you truly need.
Ask Yourself:
- Do I need technical help, business mentorship, or just accountability?
- What does this incubator offer in terms of IP protection, exposure, and connections?
- Do I understand the equity trade-off?
- What services and funding do they provide?
- Do they take equity? How much and when?
- What’s their track record with similar ventures?
- Are their incentives aligned with your vision?
6. Academic Institutions: Partners or Pitfalls?
Universities can provide credibility, resources, and early funding through their tech transfer office (TTO).
Key Questions to Ask:
- Will my IP be managed by the TTO?
- How much say do I have in licensing decisions?
- Are there royalty-sharing agreements in place?
- Can I form a startup while employed here?
You may need to negotiate if you want to commercialize your idea independently.
7. Do it for Purpose, Not Payday
Most founders end up owning only a small percentage of their company by the time a product reaches the market. Do not expect to get rich. Do it because it solves a problem you care about. If it happens to come with a nice paycheck, then that is an added bonus.
Your clinical training and insight give you a unique edge. You already know what’s broken. Use that as your compass.
Conclusion
Innovation isn’t about brilliance, it’s about curiosity, structure, and tenacity (see Table 2). Start small. Protect your work. Choose the right partners. Most importantly, stay anchored in your mission to make GI care better.
Dr. Muratore is based at UNC Rex Digestive Health, Raleigh, North Carolina. She has no conflicts related to this article. Dr. Wechsler is based at the University of North Carolina at Chapel Hill, Chapel Hill, North Carolina. She holds a patent assigned to Trustees of Dartmouth College. Dr. Shah is based at the University of Michigan, Ann Arbor, Michigan. He consults for Ardelyx, Laborie, Neuraxis, Salix, Sanofi, and Takeda and holds a patent with the Regents of the University of Michigan.
You are in the middle of a busy clinic day and think, “there has to be a better way to do this.” Suddenly, a better way to do something becomes obvious. Maybe it’s a tool that simplifies documentation, a device that improves patient comfort, or an app that bridges a clinical gap. Many physicians, especially early career gastroenterologists, have ideas like this, but few know what to do next.
This article is for the curious innovator at the beginning of their clinical career. It offers practical, real-world guidance on developing a clinical product: whether that be hardware, software, or a hybrid. It outlines what questions to ask, who to consult, and how to protect your work, using personal insights and business principles learned through lived experience.
1. Understand Intellectual Property (IP): Know Its Value and Ownership
What is IP?
Intellectual property refers to your original creations: inventions, designs, software, and more. This is what you want to protect legally through patents, trademarks, or copyrights.
Who owns your idea?
This is the first and most important question to ask. If you are employed (especially by a hospital or academic center), your contract may already give your employer rights to any inventions you create, even those developed in your personal time.
What to ask:
- Does my employment contract include an “assignment of inventions” clause?
- Does the institution claim rights to anything developed with institutional resources?
- Are there moonlighting or external activity policies that affect this?
If you are developing an idea on your personal time, with your own resources, and outside your scope of clinical duties, it might still be considered “theirs” under some contracts. Early legal consultation is critical. A specialized IP attorney can help you understand what you own and how to protect it. This should be done early, ideally before you start building anything.
2. Lawyers Aren’t Optional: They’re Essential Early Partners
You do not need a full legal team, but you do need a lawyer early. An early consultation with an IP attorney can clarify your rights, guide your filing process (e.g. provisional patents), and help you avoid costly missteps.
Do this before sharing your idea publicly, including in academic presentations, pitch competitions, or even on social media. Public disclosure can start a clock ticking for application to protect your IP.
3. Build a Founding Team with Intent
Think of your startup team like a long-term relationship: you’re committing to build something together through uncertainty, tension, and change.
Strong early-stage teams often include:
- The Visionary – understands the clinical need and vision
- The Builder – engineer, developer, or designer
- The Doer – project manager or operations lead
Before forming a company, clearly define:
- Ownership (equity percentages)
- Roles and responsibilities
- Time commitments
- What happens if someone exits
Have these discussions early and document your agreements. Avoid informal “handshake” deals that can lead to serious disputes later.
4. You Don’t Need to Know Everything on Day One
You do not need to know how to write code, build a prototype, or get FDA clearance on day one. Successful innovators are humble learners. Use a Minimum Viable Product (MVP), a simple, functional version of your idea, to test assumptions and gather feedback. Iterate based on what you learn. Do not chase perfection; pursue progress. Consider using online accelerators like Y Combinator’s startup school or AGA’s Center for GI Innovation and Technology.
5. Incubators: Use them Strategically
Incubators can offer mentorship, seed funding, legal support, and technical resources, but they vary widely in value (see Table 1). Many may want equity, and not all offer when you truly need.
Ask Yourself:
- Do I need technical help, business mentorship, or just accountability?
- What does this incubator offer in terms of IP protection, exposure, and connections?
- Do I understand the equity trade-off?
- What services and funding do they provide?
- Do they take equity? How much and when?
- What’s their track record with similar ventures?
- Are their incentives aligned with your vision?
6. Academic Institutions: Partners or Pitfalls?
Universities can provide credibility, resources, and early funding through their tech transfer office (TTO).
Key Questions to Ask:
- Will my IP be managed by the TTO?
- How much say do I have in licensing decisions?
- Are there royalty-sharing agreements in place?
- Can I form a startup while employed here?
You may need to negotiate if you want to commercialize your idea independently.
7. Do it for Purpose, Not Payday
Most founders end up owning only a small percentage of their company by the time a product reaches the market. Do not expect to get rich. Do it because it solves a problem you care about. If it happens to come with a nice paycheck, then that is an added bonus.
Your clinical training and insight give you a unique edge. You already know what’s broken. Use that as your compass.
Conclusion
Innovation isn’t about brilliance, it’s about curiosity, structure, and tenacity (see Table 2). Start small. Protect your work. Choose the right partners. Most importantly, stay anchored in your mission to make GI care better.
Dr. Muratore is based at UNC Rex Digestive Health, Raleigh, North Carolina. She has no conflicts related to this article. Dr. Wechsler is based at the University of North Carolina at Chapel Hill, Chapel Hill, North Carolina. She holds a patent assigned to Trustees of Dartmouth College. Dr. Shah is based at the University of Michigan, Ann Arbor, Michigan. He consults for Ardelyx, Laborie, Neuraxis, Salix, Sanofi, and Takeda and holds a patent with the Regents of the University of Michigan.