User login
- Provide an urgent ophthalmology referral for any patient with a sudden decrease in visual acuity. C
- Record bilateral pupil size as part of a comprehensive eye exam, and provide an urgent referral for a patient whose pupils are of unequal size. C
- Involve an ophthalmologist or other specialist in the management of eye conditions caused by systemic diseases such as stroke or giant cell arteritis. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Knowing how to respond when patients present with problems involving the eye is crucial for family physicians. Yet it is often difficult to know whether to treat or refer and which signs and symptoms are indicative of an ophthalmologic emergency with the potential to cause loss of sight.
Categorizing ophthalmologic conditions based on patients’ chief complaints, we have found, can help to narrow the differential diagnosis and home in on emergent signs and symptoms. Thus, we’ve used that approach in this review.
In the pages that follow, common complaints like “I can’t see,” “I’m seeing things,” and “My eye hurts” are used to highlight disorders—both benign and emergent—associated with each. You’ll also find an at-a-glance table listing the differential diagnosis for each presentation, and a mnemonic to guide you through the elements of a comprehensive eye exam.
1) "I can't see"
Patients may use words like “cloudy vision,“ “a veil over my eyes,” or “fuzziness” to describe diminished vision. Some will report black areas within their visual field; others will have a loss of peripheral vision or total vision loss in one eye, or possibly even both. Some causes of vision problems, such as cataracts, are not emergencies. Causes of more severe (but painless) vision loss include central retinal artery occlusion (CRAO) or vein occlusion (CRVO), giant cell arteritis (GCA), stroke or transient ischemic attack (TIA), nonarteritic anterior ischemic optic neuropathy (NAION), and nonorganic (functional) vision loss (TABLE).1-11
When the cause is ischemic
Patients with CRAO experience acute loss of vision in one eye, usually occurring within seconds to minutes. Most patients with CRVO will have a similar presentation, depending on the presence or absence of ischemia and involvement of the macula. Those with branch retinal vein occlusion may have no vision loss
at all.1-3
Risk factors for CRAO include cardiovascular disease, hypertension, diabetes, and other disorders associated with systemic inflammation. In patients older than 60 years, it is also important to consider GCA, which we’ll talk more about shortly, as a cause of CRAO.
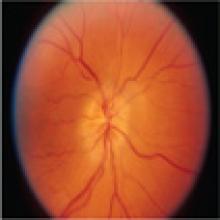
In patients with CRAO, an eye exam will show profoundly decreased visual acuity, and the swinging light test (see “Use this mnemonic to ensure a comprehensive eye exam” on page 348) will reveal a relative afferent pupillary defect (RAPD). Fundoscopy is diagnostic, revealing a pale retina due to decreased blood flow.4 Emergent referral to ophthalmology is indicated to establish a definitive diagnosis and initiate treatment based on the cause of the occlusion. If emergency care is not immediately available, massaging the eye globe through closed lids, then releasing, in 10- to 15-second cycles, may be helpful.5
Use this mnemonic to ensure a comprehensive eye exam. In a potential emergency, an eye exam needs to be quick and thorough. To ensure that all the key elements are included, use the mnemonic VVEEPP (Visual acuity, Visual fields, External exam, Extraocular movements, Pupillary exam, and Pressure) as a guide.1Visual acuity. Check distance vision, with the patient wearing his or her corrective lenses, if possible. If not, substitute pinhole testing, which can function like corrective lenses and eliminate refractive error.2
Begin with distance charts. If the patient can’t see the charts, hold up fingers and ask whether the patient is able to count them. If not, try hand motion—or, if the patient can’t see that, try testing the patient’s ability to see light. Swing a light between the eyes. Paradoxical dilation of the affected eye when directly exposed to the light is evidence of a relative afferent pupillary defect (RAPD).2
Visual fields. Examine visual fields by using the standard confrontation technique—ie, asking the patient to cover one eye at a time while you move your hand in and out of his or her visual field.
External exam and extraocular movements. Use a penlight to inspect the eyelids, conjunctiva, sclera, cornea, and anterior chamber of the eye and to assess extraocular movements.1
Pupillary examination and pressure. Observe bilateral pupil size and swing a light between the eyes to test pupillary response to direct and consensual light (and to rule out an RAPD).2 If available, measure eye pressure, as well.1
Fundoscopy should be performed to complete the examination—along with a slit lamp evaluation, if possible.1
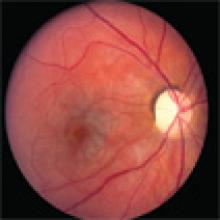
Risk factors for CRVO include age older than 65 and a number of chronic conditions. One analysis attributed 48% of cases to hypertension, 20% to hyperlipidemia, and 5% to diabetes.3 Fundoscopy will reveal dilated veins, retinal hemorrhages, and cotton wool spots, which look like puffy white patches on the retina.6
As with CRAO, an urgent ophthalmology referral is critical to establish the diagnosis and develop a treatment plan. Outcomes are poor in patients with visual acuity of 20/200 or worse at the time of diagnosis.7,8
GCA. Patients with GCA may develop arteritic ischemic optic neuropathy, resulting in vision loss in one or both eyes. Risk factors for GCA include age (>50 years), polymyalgia rheumatica, Caucasian race, and female sex. Systemic symptoms include fever, muscle aches, headache, jaw claudication, and scalp pain.6
The swinging light test will reveal an RAPD;1,2 fundoscopy findings typically include disk edema and disk hemorrhages, or a pale retina if GCA is associated with CRAO.6 Testing, including an erythrocyte sedimentation rate and a C-reactive protein, will provide supportive evidence, and biopsy of the temporal artery will confirm the diagnosis.4
Blindness from GCA is often profound. Bilateral disease is treated immediately with high-dose corticosteroids; when just one eye is affected, high-dose steroids should also be started right away to prevent vision loss in the other eye. Whenever GCA is suspected, initiate treatment and provide an urgent referral to an ophthalmologist for biopsy and further treatment.6
Strokes and TIAs that affect vision may be a result of ischemia of the visual cortex, or the eye itself. Visual cortex ischemia will present as a homonymous visual field cut between the eyes; TIAs that affect only one eye (known as amaurosis fugax) are associated with ischemia to the optic nerve or retina.
Patients with amaurosis fugax will experience unilateral loss of vision that extends like a dark shade from the top or bottom periphery to the center of vision. When a TIA is the cause, vision will return to normal within minutes. The underlying pathology is usually carotid artery atherosclerosis. If left untreated, evidence suggests that 30% to 50% of patients will have a stroke within a month.9
Visual acuity may or may not be decreased, depending on whether the ischemia involves the macula. Symptoms suggestive of amaurosis fugax should prompt an urgent ophthalmology referral, while patients with persistent vision loss or visual field deficit require urgent referral to a stroke treatment center.9
NAION is also associated with acute monocular vision loss, particularly in older patients.10 Visual acuity will be markedly decreased, and fundoscopic exam will show a swollen and hemorrhagic optic disc. The vision loss can be profound, and is usually permanent; neither medical nor surgical treatment has been shown to improve outcomes.10
When the cause is functional
Functional (nonorganic) visual disturbances should also be considered when sudden blindness is reported. Nonorganic vision loss has a number of causes, and patients present with a range of chief complaints, making diagnosis complex. Because some patients will have organic disease with a component of functional vision loss, it is best to refer individuals whom you suspect of having functional vision loss to an ophthalmologist for testing and a definitive diagnosis. Treatment includes psychological support and reassurance that vision will return.11
2) "I'm seeing things"
Patients with this problem often use words like “flashes,” “floaters” “worms,” or “lights,” and various colors and unusual shapes to describe what they see. When this phenomenon is accompanied by decreased visual acuity, emergent or urgent referral is required. Normal vision in a patient who reports “seeing things” calls for careful consideration of the etiology, and referral if the diagnosis is uncertain or the suspected disorder is sight-threatening (TABLE).4,12-14 Migraine and psychiatric disorders should be considered if suggested by history. (Patients with ocular migraine—which may or may not be associated with a headache—may also report seeing light patterns off to one side, typically lasting 20-45 minutes.)
Vitreous or retinal detachment
Patients with vitreous detachment, which is far more common and less serious than retinal detachment, report seeing new floaters or peripheral flashing lights in one eye. Risks for vitreous detachment include myopia, older age, eye trauma, and previous eye surgery.4 Physical examination and visual acuity will be normal unless there is an accompanying retinal detachment.12
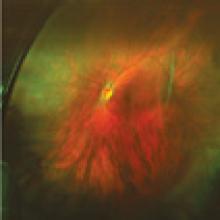
Patients who have decreased visual acuity or a visual field defect, or who describe a “curtain of darkness” are at risk for retinal detachment (shown above) and require a same-day referral.
A full ophthalmologic evaluation is indicated to detect or rule out a retinal detachment or tear—which has been found to co-occur with acute vitreous detachment in 14% of cases.13 Those who present with decreased visual acuity or a visual field defect or describe a “curtain of darkness” are at risk for retinal detachment and require a same-day referral.13
Like patients with vitreous detachment, those with a retinal detachment will report new floaters or peripheral flashing lights.12 The presence of vitreous hemorrhage or pigment, which can be seen in a slit lamp exam, is associated with increased risk for retinal detachment, as is a subjective report of vision loss.13
When retinal detachment is suspected, immediate referral to an ophthalmologist is needed.13 Reattachment surgery has good outcomes, especially if it is performed prior to macular involvement or within the first 3 days of macular detachment.14
3) "My eye hurts and is red"
Patients with painful, red eyes are at risk for a variety of sight-threatening conditions, iritis (anterior uveitis), keratitis, and acute angle closure glaucoma, as well as eye trauma, among them (TABLE).1,2,4,12,15-27 Decreased visual acuity in a patient with painful, red eyes warrants an urgent or emergent ophthalmologic referral.
When to suspect iritis
Patients with iritis will complain of vision loss, pain, photophobia, and redness. An eye exam will reveal injection of the conjunctiva around the cornea. Visual acuity is often decreased. Pupillary reaction may be sluggish, and the pupil may be smaller or larger than the other eye,4 but a normal pupil size does not exclude iritis in a patient with unilateral eye pain and ciliary injection.15
Iritis is often idiopathic, but risk factors include chronic inflammatory conditions such as ankylosing spondylitis, ulcerative colitis, and Crohn’s disease.16
Treatment with topical steroids is recommended.16 Urgent referral for long-term management of iritis is needed.17
Keratitis has varied causes
Patients with keratitis present with eye pain or foreign body sensation, redness, blurred vision, and photophobia. Examination of the eye will show injection of the conjunctiva surrounding the cornea, and possible corneal defects or opacities; visual acuity may be normal or decreased. The cause varies, based on whether keratitis is bacterial, viral, or noninfectious.
Risk factors for bacterial keratitis include extended wear of contact lenses, eye trauma, eye surgery, and systemic disease such as diabetes mellitus, while viral keratitis often follows a case of viral conjunctivitis and herpes simplex keratitis often involves reactivation of the virus. Causes of noninfectious keratitis include flash burns, dry eye or blepharitis, snow blindness, and sunburn.18
Treatment with topical antibiotics is effective for bacterial keratitis, but follow-up referral is needed because the infection could lead to loss of sight.19 Herpes simplex keratitis, which may appear as a mild corneal ulcer (a slit lamp examination will show the classic branching dendritic lesion), can be managed with topical antiviral medications,20 but here, too, an ophthalmologic referral is recommended to look for deeper corneal infiltrates that could lead to vision loss.20,21 Topical numbing medications should not be prescribed for patients with eye problems, as their extended use can lead to infection, corneal thinning, or even perforation of the cornea.22
Blurred vision, pain suggest acute angle closure glaucoma
Patients with acute angle closure glaucoma present with blurred vision, deep eye pain or brow ache, and frequently, nausea and vomiting.23 Some patients report seeing halos around lights, as well.
Risk factors for acute angle closure glaucoma include older age, Asian descent, farsightedness, family history, and female sex. Attacks are commonly idiopathic, but some are associated with routine pupillary dilation during eye exams.24
On examination, the cornea will be cloudy due to edema and the pupil will be mid-dilated and fixed.12 Typically, intraocular pressure in the affected eye will be elevated, an indication that the nausea and vomiting are associated with this disorder rather than a gastrointestinal condition.23 Emergent referral is needed to preserve vision.25
Eye trauma: What you’ll see, when to act Hyphema. In patients with a hyphema—typically the result of eye trauma—you’ll usually see a meniscus of blood in front of the iris in the anterior chamber. If the patient was supine before the evaluation, however, you’ll see red discoloration of the iris. Hyphemas can be a threat to vision, mostly due to potential elevated pressure. Because they are often associated with more extensive ocular injuries that are not always immediately evident, urgent referral is required.26
Hyphema—What you'll see
Courtesy of: Eye Teachers of America Foundation
More significant blunt trauma can cause globe rupture, resulting in both eye pain and loss of vision. Flooding the eye with fluorescein before examining it may make it possible to see a dark or green stream from the ruptured globe.
If you suspect a globe rupture, immediately stop your exam. Do not touch the eye. Instead, protect the eye—with a metal or plastic shield and an antiemetic to prevent pressure and Valsalva strain—and obtain an emergency ophthalmology consult.2,4
Chemical burns. Patients who incur chemical burns of the eye should irrigate the injured eye right away. The physical exam should be delayed until irrigation reaches an endpoint of neutral pH, as measured with Nitrazine paper.4,27 Alkali burns are particularly destructive to the eye and require longer irrigation.27
An emergent ophthalmology referral is needed for all alkali burns of the eye, as well as for any patient whose visual acuity does not return to baseline after irrigation. Slit lamp examination showing a deep corneal injury is also reason for an ophthalmology referral.1,2
4) "My eye is red" (but pain free)
When a patient seeks care for a red eye that’s not painful, the history and physical will help you determine whether the condition is benign or emergent. Orbital cellulitis, which we’ll discuss shortly, is the most dangerous condition related to this presentation (TABLE),4,9,28-32 requiring inpatient management and ophthalmology referral.
Conjunctivitis. The entire conjunctiva will be red and discharge will be present, but visual acuity will be normal.
Conjunctivitis can be viral or bacterial; office-based testing is now available for viral conjunctivitis caused by adenovirus. Treating bacterial conjunctivitis with antibiotic drops or ointment speeds recovery.29 When the cause is viral, standard treatment is supportive, with emphasis on preventing viral spread. Some antiviral preparations are being investigated as potential treatments for adenovirus conjunctivitis.28
Periorbital and orbital cellulitis. Redness surrounding the eye can be caused by preseptal (commonly called periorbital) or orbital cellulitis. The clinical presentation of these 2 conditions is similar, including redness, lid edema, and tenderness. However, periorbital cellulitis is more commonly seen after minor trauma to the eyelid skin or related to a stye or chalazion. Orbital cellulitis, which is considerably more serious, is typically associated with sinus disease or abscess.30
Patients with orbital cellulitis will present with restricted eye movements, decreased visual acuity, proptosis, and possibly an RAPD. These patients will often have pain as well. A fine-cut computed tomography of the orbits aids in diagnosis.31
Care for each is different. Oral antibiotics are usually sufficient for patients with periorbital cellulitis, but for orbital cellulitis, a same-day ophthalmology referral and hospitalization for treatment with parenteral antibiotics is required.9,32
Subconjunctival hemorrhage—dramatic but harmless
While dramatic in appearance, subconjunctival hemorrhage generally does not affect vision. It may be the result of trauma to the globe, but can also occur spontaneously.
On physical exam, you’ll see bleeding into the conjunctiva that stops at the edge of the cornea. Visual acuity will be normal, as will the remainder of the eye examination. Abnormal vision, pain, or significant or recurrent bleeding should prompt a search for an alternative diagnosis. No treatment is needed for a simple subconjunctival hemorrhage.4
5) "My eye hurts"
Patients complaining of eye pain with or without vision changes—and without redness—usually have a medical history that leads to the diagnosis (TABLE).1,2,4,33-38 Physical exam findings are compatible with the history.
Optic neuritis. Patients with optic neuritis have acute to subacute vision loss, usually in one eye but sometimes bilaterally, lasting hours to days. Optic neuritis is more common in women and in those ages 15 to 45 years, with an incidence of 5 in 100,000 among Caucasians.33 Pain with eye movement is present in more than 90% of adults with optic neuritis,34 and is also common in children.35
In addition to vision loss, patients will report decreased detection of light and color,6 and examination will reveal an RAPD.1,2 Vision returns without treatment to the same extent as with treatment, but treatment will speed recovery.36 Patients with optic neuritis require an urgent referral to an ophthalmologist or neurologist to evaluate for multiple sclerosis, which develops in about 30% of those with optic neuritis.4,33
Corneal abrasion. Pain, localized to the surface of the eye, will be the primary complaint of patients with a corneal abrasion, who may or may not have loss of vision. Larger and deeper abrasions are extremely painful, while smaller corneal abrasions may be experienced as a foreign body sensation. The typical patient with a corneal abrasion is likely to have had trauma to the eye.37
Fluorescein is used to examine the patient with a suspected abrasion to highlight the epithelial defect.1 Visual acuity needs to be tested, and checked using a pinhole if it is below baseline.37 Treatment protocols range from artificial tears to antibiotic drops or ointments. Topical steroids should be given to patients only by an ophthalmologist.4
Is patching necessary? In a systematic review comparing outcomes based on the use of patching vs not patching on the first day of injury, patients who were not given patches fared the same or better than those whose eyes were patched, both in terms of healing time and pain relief. Primary care physicians can treat most corneal abrasions, and symptoms typically resolve in 2 days.38
1. Wright JL, Wightman JM. Red and painful eye. In: Marx JA, Hockberger RS, Walls RM, et al, eds. Rosen’s Emergency Medicine: Concepts and Clinical Practice. 7th ed. Philadelphia, Pa: Mosby Elsevier; 2009:chap 32.
2. Knoop KJ, Dennis WR, Hedges JR. Ophthalmologic procedures. In: Roberts JR, Hedges JR, eds. Clinical Procedures in Emergency Medicine. 5th ed. Philadelphia, Pa: Saunders Elsevier;2009:chap 63.
3. Ehlers JP, Fekrat S. Retinal vein occlusion: beyond the acute event. Surv Ophthalmol. 2011;56:281-299.
4. Sharma R, Brunette DD. Ophthalmology. In: Marx JA, Hockberger RS, Walls RM, et al, eds. Rosen’s Emergency Medicine: Concepts and Clinical Practice. 7th ed. Philadelphia, Pa: Mosby Elsevier; 2009:chap 69.
5. Cugati S, Varma DD, Chen CS, et al. Treatment options for central retinal artery occlusion. Curr Treat Options Neurol. 2013;15:63-77.
6. Matson M, Fujimoto L. Bilateral arteritic anterior ischemic optic neuropathy. Optometry. 2011;82:622-631.
7. McIntosh RL, Rogers SL, Lim L, et al. Natural history of central retinal vein occlusion: an evidence-based systematic review. Ophthalmology. 2010;117:1113-1123.
8. Wong TY, Scott IU. Retinal-vein occlusion. N Engl J Med. 2010;363:2135-2144.
9. Crouch ER, Crouch ER, Grant T. Ophthalmology. In: Rakel RE, ed. Textbook of Family Medicine. 8th ed. Philadelphia, Pa: Saunders Elsevier; 2011:chap 41.
10. Dickersin K, Manheimer E, Li T. Surgery for nonarteritic anterior ischemic optic neuropathy. Cochrane Database Syst Rev. 2012;(1):CD001538.
11. Thurtell MJ, Tomsak RL. Neuro-ophthalmology: afferent visual system. In: Daroff RB, Fenichel GM, Jankovic J, et al, eds. Bradley’s Neurology in Clinical Practice. 6th ed. Los Angeles, Calif: Saunders Elsevier; 2012:chap 36.
12. Yanoff M, Cameron D. Diseases of the visual system. In: Goldman L, Schafer AI, eds. Cecil Medicine. 24th ed. Philadelphia, Pa: Saunders Elsevier; 2011:chap 431.
13. Hollands H, Johnson D, Brox A, et al. Acute-onset floaters and flashes: is this patient at risk for retinal detachment? JAMA. 2009;302:2243-2249.
14. D’Amico DJ. Primary retinal detachment. N Engl J Med. 2008;359:2346-2354.
15. Hunsley T, Lee C. Does a normal-shaped pupil exclude the diagnosis of iritis? Best evidence topic reports. Towards evidence-based emergency medicine: best BETs from the Manchester Royal Infirmary. Emerg Med J. 2006;23:872-877.
16. Islam N, Pavesio C. Uveitis (acute anterior). Clin Evid. 2010;4:705.
17. Grunwald L, Newcomb CW, Daniel E, et al. Risk of relapse in primary acute anterior uveitis. Ophthalmology. 2011;118:1911-1915.
18. Thomas PA, Geraldine P. Infectious keratitis. Curr Opin Infect Dis. 2007;20:129-141.
19. Suwan-Apichon O, Reyes JM, Herretes S, et al. Topical corticosteroids as adjunctive therapy for bacterial keratitis. Cochrane Database Syst Rev. 2007;(4):CD005430.
20. Morris D, Latham E. Ulcers in the eye. J Emerg Med. 2012;42:62-64.
21. Wilhelmus KR. Antiviral treatment and other therapeutic interventions for herpes simplex virus epithelial keratitis. Cochrane Database Syst Rev. 2010;(12):CD002898.
22. Yagci A, Bozkurt B, Egrilmez S, et al. Topical anesthetic abuse keratopathy: a commonly overlooked health care problem.Cornea. 2011;30:571-575.
23. Cholongitas E, Pipili C, Dasenaki M. Acute angle closure glaucoma presented with nausea and epigastric pain. Dig Dis Sci. 2008;53:1430-1431.
24. White J. Diagnosis and management of acute angle-closure glaucoma. Emerg Nurse. 2011;19:27.
25. Lama DSC, Thama CCY, Laia JSM, et al. Current approaches to the management of acute primary angle closure. Curr Opin Ophthalmol. 2007;18:146-151.
26. Gharaibeh A, Savage HI, Scherer RW, et al. Medical interventions for traumatic hyphema. Cochrane Database Syst Rev. 2011;(1):CD005431.
27. Connor AJ, Severn P. Use of a control test to aid pH assessment of chemical eye injuries. Emerg Med J. 2009;26:811-812.
28. Sambursky R, Trattler W, Tauber S, et al. Sensitivity and specificity of the AdenoPlus test for diagnosing adenoviral conjunctivitis. JAMA Ophthalmol. 2013;131:17-22.
29. Sheikh A, Hurwitz B. Antibiotics versus placebo for acute bacterial conjunctivitis. Cochrane Database Syst Rev. 2006;(2):CD001211.
30. Papier A, Tuttle DJ, Mahara TJ. Differential diagnosis of the swollen red eyelid. Am Fam Physician. 2007;76:1815-1824.
31. Howe L, Jones NS. Guidelines for the management of periorbital cellulitis/abscess. Clin Otolaryngol. 2004;29:725-728.
32. Mahalingam-Dhingra A, Lander L, Preciado DA, et al. Orbital and periorbital infections: a national perspective. Arch Otolaryngol Head Neck Surg. 2011;137:769-773.
33. Germann CA, Baumann MR, Hamzavi S. Ophthalmic diagnoses in the ED: optic neuritis. Am J Emerg Med. 2007;25:834-837.
34. Balcer LJ. Optic neuritis. N Engl J Med. 2006;354:1273-1280.
35. Olitsky SE, Hug D, Plummer L, et al. Abnormalities of the optic nerve. In: Kliegman RM, Behrman RE, Jenson HB, et al, eds.Nelson Textbook of Pediatrics. 19th ed. Philadelphia, Pa: Saunders Elsevier; 2011:chap 623.
36. Gal RL, Vedula SS, Beck R. Corticosteroids for treating optic neuritis. Cochrane Database Syst Rev. 2012;(4):CD001430.
37. Aslam SA, Sheth HG, Vaughan AJ. Emergency management of corneal injuries. Injury. 2007;38:594-597.
38. Turner A, Rabiu M. Patching for corneal abrasion. Cochrane Database Syst Rev. 2006;(2):CD004764.
- Provide an urgent ophthalmology referral for any patient with a sudden decrease in visual acuity. C
- Record bilateral pupil size as part of a comprehensive eye exam, and provide an urgent referral for a patient whose pupils are of unequal size. C
- Involve an ophthalmologist or other specialist in the management of eye conditions caused by systemic diseases such as stroke or giant cell arteritis. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Knowing how to respond when patients present with problems involving the eye is crucial for family physicians. Yet it is often difficult to know whether to treat or refer and which signs and symptoms are indicative of an ophthalmologic emergency with the potential to cause loss of sight.
Categorizing ophthalmologic conditions based on patients’ chief complaints, we have found, can help to narrow the differential diagnosis and home in on emergent signs and symptoms. Thus, we’ve used that approach in this review.
In the pages that follow, common complaints like “I can’t see,” “I’m seeing things,” and “My eye hurts” are used to highlight disorders—both benign and emergent—associated with each. You’ll also find an at-a-glance table listing the differential diagnosis for each presentation, and a mnemonic to guide you through the elements of a comprehensive eye exam.
1) "I can't see"
Patients may use words like “cloudy vision,“ “a veil over my eyes,” or “fuzziness” to describe diminished vision. Some will report black areas within their visual field; others will have a loss of peripheral vision or total vision loss in one eye, or possibly even both. Some causes of vision problems, such as cataracts, are not emergencies. Causes of more severe (but painless) vision loss include central retinal artery occlusion (CRAO) or vein occlusion (CRVO), giant cell arteritis (GCA), stroke or transient ischemic attack (TIA), nonarteritic anterior ischemic optic neuropathy (NAION), and nonorganic (functional) vision loss (TABLE).1-11
When the cause is ischemic
Patients with CRAO experience acute loss of vision in one eye, usually occurring within seconds to minutes. Most patients with CRVO will have a similar presentation, depending on the presence or absence of ischemia and involvement of the macula. Those with branch retinal vein occlusion may have no vision loss
at all.1-3
Risk factors for CRAO include cardiovascular disease, hypertension, diabetes, and other disorders associated with systemic inflammation. In patients older than 60 years, it is also important to consider GCA, which we’ll talk more about shortly, as a cause of CRAO.
In patients with CRAO, an eye exam will show profoundly decreased visual acuity, and the swinging light test (see “Use this mnemonic to ensure a comprehensive eye exam” on page 348) will reveal a relative afferent pupillary defect (RAPD). Fundoscopy is diagnostic, revealing a pale retina due to decreased blood flow.4 Emergent referral to ophthalmology is indicated to establish a definitive diagnosis and initiate treatment based on the cause of the occlusion. If emergency care is not immediately available, massaging the eye globe through closed lids, then releasing, in 10- to 15-second cycles, may be helpful.5
Use this mnemonic to ensure a comprehensive eye exam. In a potential emergency, an eye exam needs to be quick and thorough. To ensure that all the key elements are included, use the mnemonic VVEEPP (Visual acuity, Visual fields, External exam, Extraocular movements, Pupillary exam, and Pressure) as a guide.1Visual acuity. Check distance vision, with the patient wearing his or her corrective lenses, if possible. If not, substitute pinhole testing, which can function like corrective lenses and eliminate refractive error.2
Begin with distance charts. If the patient can’t see the charts, hold up fingers and ask whether the patient is able to count them. If not, try hand motion—or, if the patient can’t see that, try testing the patient’s ability to see light. Swing a light between the eyes. Paradoxical dilation of the affected eye when directly exposed to the light is evidence of a relative afferent pupillary defect (RAPD).2
Visual fields. Examine visual fields by using the standard confrontation technique—ie, asking the patient to cover one eye at a time while you move your hand in and out of his or her visual field.
External exam and extraocular movements. Use a penlight to inspect the eyelids, conjunctiva, sclera, cornea, and anterior chamber of the eye and to assess extraocular movements.1
Pupillary examination and pressure. Observe bilateral pupil size and swing a light between the eyes to test pupillary response to direct and consensual light (and to rule out an RAPD).2 If available, measure eye pressure, as well.1
Fundoscopy should be performed to complete the examination—along with a slit lamp evaluation, if possible.1
Risk factors for CRVO include age older than 65 and a number of chronic conditions. One analysis attributed 48% of cases to hypertension, 20% to hyperlipidemia, and 5% to diabetes.3 Fundoscopy will reveal dilated veins, retinal hemorrhages, and cotton wool spots, which look like puffy white patches on the retina.6
As with CRAO, an urgent ophthalmology referral is critical to establish the diagnosis and develop a treatment plan. Outcomes are poor in patients with visual acuity of 20/200 or worse at the time of diagnosis.7,8
GCA. Patients with GCA may develop arteritic ischemic optic neuropathy, resulting in vision loss in one or both eyes. Risk factors for GCA include age (>50 years), polymyalgia rheumatica, Caucasian race, and female sex. Systemic symptoms include fever, muscle aches, headache, jaw claudication, and scalp pain.6
The swinging light test will reveal an RAPD;1,2 fundoscopy findings typically include disk edema and disk hemorrhages, or a pale retina if GCA is associated with CRAO.6 Testing, including an erythrocyte sedimentation rate and a C-reactive protein, will provide supportive evidence, and biopsy of the temporal artery will confirm the diagnosis.4
Blindness from GCA is often profound. Bilateral disease is treated immediately with high-dose corticosteroids; when just one eye is affected, high-dose steroids should also be started right away to prevent vision loss in the other eye. Whenever GCA is suspected, initiate treatment and provide an urgent referral to an ophthalmologist for biopsy and further treatment.6
Strokes and TIAs that affect vision may be a result of ischemia of the visual cortex, or the eye itself. Visual cortex ischemia will present as a homonymous visual field cut between the eyes; TIAs that affect only one eye (known as amaurosis fugax) are associated with ischemia to the optic nerve or retina.
Patients with amaurosis fugax will experience unilateral loss of vision that extends like a dark shade from the top or bottom periphery to the center of vision. When a TIA is the cause, vision will return to normal within minutes. The underlying pathology is usually carotid artery atherosclerosis. If left untreated, evidence suggests that 30% to 50% of patients will have a stroke within a month.9
Visual acuity may or may not be decreased, depending on whether the ischemia involves the macula. Symptoms suggestive of amaurosis fugax should prompt an urgent ophthalmology referral, while patients with persistent vision loss or visual field deficit require urgent referral to a stroke treatment center.9
NAION is also associated with acute monocular vision loss, particularly in older patients.10 Visual acuity will be markedly decreased, and fundoscopic exam will show a swollen and hemorrhagic optic disc. The vision loss can be profound, and is usually permanent; neither medical nor surgical treatment has been shown to improve outcomes.10
When the cause is functional
Functional (nonorganic) visual disturbances should also be considered when sudden blindness is reported. Nonorganic vision loss has a number of causes, and patients present with a range of chief complaints, making diagnosis complex. Because some patients will have organic disease with a component of functional vision loss, it is best to refer individuals whom you suspect of having functional vision loss to an ophthalmologist for testing and a definitive diagnosis. Treatment includes psychological support and reassurance that vision will return.11
2) "I'm seeing things"
Patients with this problem often use words like “flashes,” “floaters” “worms,” or “lights,” and various colors and unusual shapes to describe what they see. When this phenomenon is accompanied by decreased visual acuity, emergent or urgent referral is required. Normal vision in a patient who reports “seeing things” calls for careful consideration of the etiology, and referral if the diagnosis is uncertain or the suspected disorder is sight-threatening (TABLE).4,12-14 Migraine and psychiatric disorders should be considered if suggested by history. (Patients with ocular migraine—which may or may not be associated with a headache—may also report seeing light patterns off to one side, typically lasting 20-45 minutes.)
Vitreous or retinal detachment
Patients with vitreous detachment, which is far more common and less serious than retinal detachment, report seeing new floaters or peripheral flashing lights in one eye. Risks for vitreous detachment include myopia, older age, eye trauma, and previous eye surgery.4 Physical examination and visual acuity will be normal unless there is an accompanying retinal detachment.12
Patients who have decreased visual acuity or a visual field defect, or who describe a “curtain of darkness” are at risk for retinal detachment (shown above) and require a same-day referral.
A full ophthalmologic evaluation is indicated to detect or rule out a retinal detachment or tear—which has been found to co-occur with acute vitreous detachment in 14% of cases.13 Those who present with decreased visual acuity or a visual field defect or describe a “curtain of darkness” are at risk for retinal detachment and require a same-day referral.13
Like patients with vitreous detachment, those with a retinal detachment will report new floaters or peripheral flashing lights.12 The presence of vitreous hemorrhage or pigment, which can be seen in a slit lamp exam, is associated with increased risk for retinal detachment, as is a subjective report of vision loss.13
When retinal detachment is suspected, immediate referral to an ophthalmologist is needed.13 Reattachment surgery has good outcomes, especially if it is performed prior to macular involvement or within the first 3 days of macular detachment.14
3) "My eye hurts and is red"
Patients with painful, red eyes are at risk for a variety of sight-threatening conditions, iritis (anterior uveitis), keratitis, and acute angle closure glaucoma, as well as eye trauma, among them (TABLE).1,2,4,12,15-27 Decreased visual acuity in a patient with painful, red eyes warrants an urgent or emergent ophthalmologic referral.
When to suspect iritis
Patients with iritis will complain of vision loss, pain, photophobia, and redness. An eye exam will reveal injection of the conjunctiva around the cornea. Visual acuity is often decreased. Pupillary reaction may be sluggish, and the pupil may be smaller or larger than the other eye,4 but a normal pupil size does not exclude iritis in a patient with unilateral eye pain and ciliary injection.15
Iritis is often idiopathic, but risk factors include chronic inflammatory conditions such as ankylosing spondylitis, ulcerative colitis, and Crohn’s disease.16
Treatment with topical steroids is recommended.16 Urgent referral for long-term management of iritis is needed.17
Keratitis has varied causes
Patients with keratitis present with eye pain or foreign body sensation, redness, blurred vision, and photophobia. Examination of the eye will show injection of the conjunctiva surrounding the cornea, and possible corneal defects or opacities; visual acuity may be normal or decreased. The cause varies, based on whether keratitis is bacterial, viral, or noninfectious.
Risk factors for bacterial keratitis include extended wear of contact lenses, eye trauma, eye surgery, and systemic disease such as diabetes mellitus, while viral keratitis often follows a case of viral conjunctivitis and herpes simplex keratitis often involves reactivation of the virus. Causes of noninfectious keratitis include flash burns, dry eye or blepharitis, snow blindness, and sunburn.18
Treatment with topical antibiotics is effective for bacterial keratitis, but follow-up referral is needed because the infection could lead to loss of sight.19 Herpes simplex keratitis, which may appear as a mild corneal ulcer (a slit lamp examination will show the classic branching dendritic lesion), can be managed with topical antiviral medications,20 but here, too, an ophthalmologic referral is recommended to look for deeper corneal infiltrates that could lead to vision loss.20,21 Topical numbing medications should not be prescribed for patients with eye problems, as their extended use can lead to infection, corneal thinning, or even perforation of the cornea.22
Blurred vision, pain suggest acute angle closure glaucoma
Patients with acute angle closure glaucoma present with blurred vision, deep eye pain or brow ache, and frequently, nausea and vomiting.23 Some patients report seeing halos around lights, as well.
Risk factors for acute angle closure glaucoma include older age, Asian descent, farsightedness, family history, and female sex. Attacks are commonly idiopathic, but some are associated with routine pupillary dilation during eye exams.24
On examination, the cornea will be cloudy due to edema and the pupil will be mid-dilated and fixed.12 Typically, intraocular pressure in the affected eye will be elevated, an indication that the nausea and vomiting are associated with this disorder rather than a gastrointestinal condition.23 Emergent referral is needed to preserve vision.25
Eye trauma: What you’ll see, when to act Hyphema. In patients with a hyphema—typically the result of eye trauma—you’ll usually see a meniscus of blood in front of the iris in the anterior chamber. If the patient was supine before the evaluation, however, you’ll see red discoloration of the iris. Hyphemas can be a threat to vision, mostly due to potential elevated pressure. Because they are often associated with more extensive ocular injuries that are not always immediately evident, urgent referral is required.26
Hyphema—What you'll see
Courtesy of: Eye Teachers of America Foundation
More significant blunt trauma can cause globe rupture, resulting in both eye pain and loss of vision. Flooding the eye with fluorescein before examining it may make it possible to see a dark or green stream from the ruptured globe.
If you suspect a globe rupture, immediately stop your exam. Do not touch the eye. Instead, protect the eye—with a metal or plastic shield and an antiemetic to prevent pressure and Valsalva strain—and obtain an emergency ophthalmology consult.2,4
Chemical burns. Patients who incur chemical burns of the eye should irrigate the injured eye right away. The physical exam should be delayed until irrigation reaches an endpoint of neutral pH, as measured with Nitrazine paper.4,27 Alkali burns are particularly destructive to the eye and require longer irrigation.27
An emergent ophthalmology referral is needed for all alkali burns of the eye, as well as for any patient whose visual acuity does not return to baseline after irrigation. Slit lamp examination showing a deep corneal injury is also reason for an ophthalmology referral.1,2
4) "My eye is red" (but pain free)
When a patient seeks care for a red eye that’s not painful, the history and physical will help you determine whether the condition is benign or emergent. Orbital cellulitis, which we’ll discuss shortly, is the most dangerous condition related to this presentation (TABLE),4,9,28-32 requiring inpatient management and ophthalmology referral.
Conjunctivitis. The entire conjunctiva will be red and discharge will be present, but visual acuity will be normal.
Conjunctivitis can be viral or bacterial; office-based testing is now available for viral conjunctivitis caused by adenovirus. Treating bacterial conjunctivitis with antibiotic drops or ointment speeds recovery.29 When the cause is viral, standard treatment is supportive, with emphasis on preventing viral spread. Some antiviral preparations are being investigated as potential treatments for adenovirus conjunctivitis.28
Periorbital and orbital cellulitis. Redness surrounding the eye can be caused by preseptal (commonly called periorbital) or orbital cellulitis. The clinical presentation of these 2 conditions is similar, including redness, lid edema, and tenderness. However, periorbital cellulitis is more commonly seen after minor trauma to the eyelid skin or related to a stye or chalazion. Orbital cellulitis, which is considerably more serious, is typically associated with sinus disease or abscess.30
Patients with orbital cellulitis will present with restricted eye movements, decreased visual acuity, proptosis, and possibly an RAPD. These patients will often have pain as well. A fine-cut computed tomography of the orbits aids in diagnosis.31
Care for each is different. Oral antibiotics are usually sufficient for patients with periorbital cellulitis, but for orbital cellulitis, a same-day ophthalmology referral and hospitalization for treatment with parenteral antibiotics is required.9,32
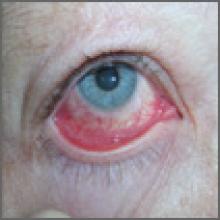
Subconjunctival hemorrhage—dramatic but harmless
While dramatic in appearance, subconjunctival hemorrhage generally does not affect vision. It may be the result of trauma to the globe, but can also occur spontaneously.
On physical exam, you’ll see bleeding into the conjunctiva that stops at the edge of the cornea. Visual acuity will be normal, as will the remainder of the eye examination. Abnormal vision, pain, or significant or recurrent bleeding should prompt a search for an alternative diagnosis. No treatment is needed for a simple subconjunctival hemorrhage.4
5) "My eye hurts"
Patients complaining of eye pain with or without vision changes—and without redness—usually have a medical history that leads to the diagnosis (TABLE).1,2,4,33-38 Physical exam findings are compatible with the history.
Optic neuritis. Patients with optic neuritis have acute to subacute vision loss, usually in one eye but sometimes bilaterally, lasting hours to days. Optic neuritis is more common in women and in those ages 15 to 45 years, with an incidence of 5 in 100,000 among Caucasians.33 Pain with eye movement is present in more than 90% of adults with optic neuritis,34 and is also common in children.35
In addition to vision loss, patients will report decreased detection of light and color,6 and examination will reveal an RAPD.1,2 Vision returns without treatment to the same extent as with treatment, but treatment will speed recovery.36 Patients with optic neuritis require an urgent referral to an ophthalmologist or neurologist to evaluate for multiple sclerosis, which develops in about 30% of those with optic neuritis.4,33
Corneal abrasion. Pain, localized to the surface of the eye, will be the primary complaint of patients with a corneal abrasion, who may or may not have loss of vision. Larger and deeper abrasions are extremely painful, while smaller corneal abrasions may be experienced as a foreign body sensation. The typical patient with a corneal abrasion is likely to have had trauma to the eye.37
Fluorescein is used to examine the patient with a suspected abrasion to highlight the epithelial defect.1 Visual acuity needs to be tested, and checked using a pinhole if it is below baseline.37 Treatment protocols range from artificial tears to antibiotic drops or ointments. Topical steroids should be given to patients only by an ophthalmologist.4
Is patching necessary? In a systematic review comparing outcomes based on the use of patching vs not patching on the first day of injury, patients who were not given patches fared the same or better than those whose eyes were patched, both in terms of healing time and pain relief. Primary care physicians can treat most corneal abrasions, and symptoms typically resolve in 2 days.38
- Provide an urgent ophthalmology referral for any patient with a sudden decrease in visual acuity. C
- Record bilateral pupil size as part of a comprehensive eye exam, and provide an urgent referral for a patient whose pupils are of unequal size. C
- Involve an ophthalmologist or other specialist in the management of eye conditions caused by systemic diseases such as stroke or giant cell arteritis. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Knowing how to respond when patients present with problems involving the eye is crucial for family physicians. Yet it is often difficult to know whether to treat or refer and which signs and symptoms are indicative of an ophthalmologic emergency with the potential to cause loss of sight.
Categorizing ophthalmologic conditions based on patients’ chief complaints, we have found, can help to narrow the differential diagnosis and home in on emergent signs and symptoms. Thus, we’ve used that approach in this review.
In the pages that follow, common complaints like “I can’t see,” “I’m seeing things,” and “My eye hurts” are used to highlight disorders—both benign and emergent—associated with each. You’ll also find an at-a-glance table listing the differential diagnosis for each presentation, and a mnemonic to guide you through the elements of a comprehensive eye exam.
1) "I can't see"
Patients may use words like “cloudy vision,“ “a veil over my eyes,” or “fuzziness” to describe diminished vision. Some will report black areas within their visual field; others will have a loss of peripheral vision or total vision loss in one eye, or possibly even both. Some causes of vision problems, such as cataracts, are not emergencies. Causes of more severe (but painless) vision loss include central retinal artery occlusion (CRAO) or vein occlusion (CRVO), giant cell arteritis (GCA), stroke or transient ischemic attack (TIA), nonarteritic anterior ischemic optic neuropathy (NAION), and nonorganic (functional) vision loss (TABLE).1-11
When the cause is ischemic
Patients with CRAO experience acute loss of vision in one eye, usually occurring within seconds to minutes. Most patients with CRVO will have a similar presentation, depending on the presence or absence of ischemia and involvement of the macula. Those with branch retinal vein occlusion may have no vision loss
at all.1-3
Risk factors for CRAO include cardiovascular disease, hypertension, diabetes, and other disorders associated with systemic inflammation. In patients older than 60 years, it is also important to consider GCA, which we’ll talk more about shortly, as a cause of CRAO.
In patients with CRAO, an eye exam will show profoundly decreased visual acuity, and the swinging light test (see “Use this mnemonic to ensure a comprehensive eye exam” on page 348) will reveal a relative afferent pupillary defect (RAPD). Fundoscopy is diagnostic, revealing a pale retina due to decreased blood flow.4 Emergent referral to ophthalmology is indicated to establish a definitive diagnosis and initiate treatment based on the cause of the occlusion. If emergency care is not immediately available, massaging the eye globe through closed lids, then releasing, in 10- to 15-second cycles, may be helpful.5
Use this mnemonic to ensure a comprehensive eye exam. In a potential emergency, an eye exam needs to be quick and thorough. To ensure that all the key elements are included, use the mnemonic VVEEPP (Visual acuity, Visual fields, External exam, Extraocular movements, Pupillary exam, and Pressure) as a guide.1Visual acuity. Check distance vision, with the patient wearing his or her corrective lenses, if possible. If not, substitute pinhole testing, which can function like corrective lenses and eliminate refractive error.2
Begin with distance charts. If the patient can’t see the charts, hold up fingers and ask whether the patient is able to count them. If not, try hand motion—or, if the patient can’t see that, try testing the patient’s ability to see light. Swing a light between the eyes. Paradoxical dilation of the affected eye when directly exposed to the light is evidence of a relative afferent pupillary defect (RAPD).2
Visual fields. Examine visual fields by using the standard confrontation technique—ie, asking the patient to cover one eye at a time while you move your hand in and out of his or her visual field.
External exam and extraocular movements. Use a penlight to inspect the eyelids, conjunctiva, sclera, cornea, and anterior chamber of the eye and to assess extraocular movements.1
Pupillary examination and pressure. Observe bilateral pupil size and swing a light between the eyes to test pupillary response to direct and consensual light (and to rule out an RAPD).2 If available, measure eye pressure, as well.1
Fundoscopy should be performed to complete the examination—along with a slit lamp evaluation, if possible.1
Risk factors for CRVO include age older than 65 and a number of chronic conditions. One analysis attributed 48% of cases to hypertension, 20% to hyperlipidemia, and 5% to diabetes.3 Fundoscopy will reveal dilated veins, retinal hemorrhages, and cotton wool spots, which look like puffy white patches on the retina.6
As with CRAO, an urgent ophthalmology referral is critical to establish the diagnosis and develop a treatment plan. Outcomes are poor in patients with visual acuity of 20/200 or worse at the time of diagnosis.7,8
GCA. Patients with GCA may develop arteritic ischemic optic neuropathy, resulting in vision loss in one or both eyes. Risk factors for GCA include age (>50 years), polymyalgia rheumatica, Caucasian race, and female sex. Systemic symptoms include fever, muscle aches, headache, jaw claudication, and scalp pain.6
The swinging light test will reveal an RAPD;1,2 fundoscopy findings typically include disk edema and disk hemorrhages, or a pale retina if GCA is associated with CRAO.6 Testing, including an erythrocyte sedimentation rate and a C-reactive protein, will provide supportive evidence, and biopsy of the temporal artery will confirm the diagnosis.4
Blindness from GCA is often profound. Bilateral disease is treated immediately with high-dose corticosteroids; when just one eye is affected, high-dose steroids should also be started right away to prevent vision loss in the other eye. Whenever GCA is suspected, initiate treatment and provide an urgent referral to an ophthalmologist for biopsy and further treatment.6
Strokes and TIAs that affect vision may be a result of ischemia of the visual cortex, or the eye itself. Visual cortex ischemia will present as a homonymous visual field cut between the eyes; TIAs that affect only one eye (known as amaurosis fugax) are associated with ischemia to the optic nerve or retina.
Patients with amaurosis fugax will experience unilateral loss of vision that extends like a dark shade from the top or bottom periphery to the center of vision. When a TIA is the cause, vision will return to normal within minutes. The underlying pathology is usually carotid artery atherosclerosis. If left untreated, evidence suggests that 30% to 50% of patients will have a stroke within a month.9
Visual acuity may or may not be decreased, depending on whether the ischemia involves the macula. Symptoms suggestive of amaurosis fugax should prompt an urgent ophthalmology referral, while patients with persistent vision loss or visual field deficit require urgent referral to a stroke treatment center.9
NAION is also associated with acute monocular vision loss, particularly in older patients.10 Visual acuity will be markedly decreased, and fundoscopic exam will show a swollen and hemorrhagic optic disc. The vision loss can be profound, and is usually permanent; neither medical nor surgical treatment has been shown to improve outcomes.10
When the cause is functional
Functional (nonorganic) visual disturbances should also be considered when sudden blindness is reported. Nonorganic vision loss has a number of causes, and patients present with a range of chief complaints, making diagnosis complex. Because some patients will have organic disease with a component of functional vision loss, it is best to refer individuals whom you suspect of having functional vision loss to an ophthalmologist for testing and a definitive diagnosis. Treatment includes psychological support and reassurance that vision will return.11
2) "I'm seeing things"
Patients with this problem often use words like “flashes,” “floaters” “worms,” or “lights,” and various colors and unusual shapes to describe what they see. When this phenomenon is accompanied by decreased visual acuity, emergent or urgent referral is required. Normal vision in a patient who reports “seeing things” calls for careful consideration of the etiology, and referral if the diagnosis is uncertain or the suspected disorder is sight-threatening (TABLE).4,12-14 Migraine and psychiatric disorders should be considered if suggested by history. (Patients with ocular migraine—which may or may not be associated with a headache—may also report seeing light patterns off to one side, typically lasting 20-45 minutes.)
Vitreous or retinal detachment
Patients with vitreous detachment, which is far more common and less serious than retinal detachment, report seeing new floaters or peripheral flashing lights in one eye. Risks for vitreous detachment include myopia, older age, eye trauma, and previous eye surgery.4 Physical examination and visual acuity will be normal unless there is an accompanying retinal detachment.12
Patients who have decreased visual acuity or a visual field defect, or who describe a “curtain of darkness” are at risk for retinal detachment (shown above) and require a same-day referral.
A full ophthalmologic evaluation is indicated to detect or rule out a retinal detachment or tear—which has been found to co-occur with acute vitreous detachment in 14% of cases.13 Those who present with decreased visual acuity or a visual field defect or describe a “curtain of darkness” are at risk for retinal detachment and require a same-day referral.13
Like patients with vitreous detachment, those with a retinal detachment will report new floaters or peripheral flashing lights.12 The presence of vitreous hemorrhage or pigment, which can be seen in a slit lamp exam, is associated with increased risk for retinal detachment, as is a subjective report of vision loss.13
When retinal detachment is suspected, immediate referral to an ophthalmologist is needed.13 Reattachment surgery has good outcomes, especially if it is performed prior to macular involvement or within the first 3 days of macular detachment.14
3) "My eye hurts and is red"
Patients with painful, red eyes are at risk for a variety of sight-threatening conditions, iritis (anterior uveitis), keratitis, and acute angle closure glaucoma, as well as eye trauma, among them (TABLE).1,2,4,12,15-27 Decreased visual acuity in a patient with painful, red eyes warrants an urgent or emergent ophthalmologic referral.
When to suspect iritis
Patients with iritis will complain of vision loss, pain, photophobia, and redness. An eye exam will reveal injection of the conjunctiva around the cornea. Visual acuity is often decreased. Pupillary reaction may be sluggish, and the pupil may be smaller or larger than the other eye,4 but a normal pupil size does not exclude iritis in a patient with unilateral eye pain and ciliary injection.15
Iritis is often idiopathic, but risk factors include chronic inflammatory conditions such as ankylosing spondylitis, ulcerative colitis, and Crohn’s disease.16
Treatment with topical steroids is recommended.16 Urgent referral for long-term management of iritis is needed.17
Keratitis has varied causes
Patients with keratitis present with eye pain or foreign body sensation, redness, blurred vision, and photophobia. Examination of the eye will show injection of the conjunctiva surrounding the cornea, and possible corneal defects or opacities; visual acuity may be normal or decreased. The cause varies, based on whether keratitis is bacterial, viral, or noninfectious.
Risk factors for bacterial keratitis include extended wear of contact lenses, eye trauma, eye surgery, and systemic disease such as diabetes mellitus, while viral keratitis often follows a case of viral conjunctivitis and herpes simplex keratitis often involves reactivation of the virus. Causes of noninfectious keratitis include flash burns, dry eye or blepharitis, snow blindness, and sunburn.18
Treatment with topical antibiotics is effective for bacterial keratitis, but follow-up referral is needed because the infection could lead to loss of sight.19 Herpes simplex keratitis, which may appear as a mild corneal ulcer (a slit lamp examination will show the classic branching dendritic lesion), can be managed with topical antiviral medications,20 but here, too, an ophthalmologic referral is recommended to look for deeper corneal infiltrates that could lead to vision loss.20,21 Topical numbing medications should not be prescribed for patients with eye problems, as their extended use can lead to infection, corneal thinning, or even perforation of the cornea.22
Blurred vision, pain suggest acute angle closure glaucoma
Patients with acute angle closure glaucoma present with blurred vision, deep eye pain or brow ache, and frequently, nausea and vomiting.23 Some patients report seeing halos around lights, as well.
Risk factors for acute angle closure glaucoma include older age, Asian descent, farsightedness, family history, and female sex. Attacks are commonly idiopathic, but some are associated with routine pupillary dilation during eye exams.24
On examination, the cornea will be cloudy due to edema and the pupil will be mid-dilated and fixed.12 Typically, intraocular pressure in the affected eye will be elevated, an indication that the nausea and vomiting are associated with this disorder rather than a gastrointestinal condition.23 Emergent referral is needed to preserve vision.25
Eye trauma: What you’ll see, when to act Hyphema. In patients with a hyphema—typically the result of eye trauma—you’ll usually see a meniscus of blood in front of the iris in the anterior chamber. If the patient was supine before the evaluation, however, you’ll see red discoloration of the iris. Hyphemas can be a threat to vision, mostly due to potential elevated pressure. Because they are often associated with more extensive ocular injuries that are not always immediately evident, urgent referral is required.26
Hyphema—What you'll see
Courtesy of: Eye Teachers of America Foundation
More significant blunt trauma can cause globe rupture, resulting in both eye pain and loss of vision. Flooding the eye with fluorescein before examining it may make it possible to see a dark or green stream from the ruptured globe.
If you suspect a globe rupture, immediately stop your exam. Do not touch the eye. Instead, protect the eye—with a metal or plastic shield and an antiemetic to prevent pressure and Valsalva strain—and obtain an emergency ophthalmology consult.2,4
Chemical burns. Patients who incur chemical burns of the eye should irrigate the injured eye right away. The physical exam should be delayed until irrigation reaches an endpoint of neutral pH, as measured with Nitrazine paper.4,27 Alkali burns are particularly destructive to the eye and require longer irrigation.27
An emergent ophthalmology referral is needed for all alkali burns of the eye, as well as for any patient whose visual acuity does not return to baseline after irrigation. Slit lamp examination showing a deep corneal injury is also reason for an ophthalmology referral.1,2
4) "My eye is red" (but pain free)
When a patient seeks care for a red eye that’s not painful, the history and physical will help you determine whether the condition is benign or emergent. Orbital cellulitis, which we’ll discuss shortly, is the most dangerous condition related to this presentation (TABLE),4,9,28-32 requiring inpatient management and ophthalmology referral.
Conjunctivitis. The entire conjunctiva will be red and discharge will be present, but visual acuity will be normal.
Conjunctivitis can be viral or bacterial; office-based testing is now available for viral conjunctivitis caused by adenovirus. Treating bacterial conjunctivitis with antibiotic drops or ointment speeds recovery.29 When the cause is viral, standard treatment is supportive, with emphasis on preventing viral spread. Some antiviral preparations are being investigated as potential treatments for adenovirus conjunctivitis.28
Periorbital and orbital cellulitis. Redness surrounding the eye can be caused by preseptal (commonly called periorbital) or orbital cellulitis. The clinical presentation of these 2 conditions is similar, including redness, lid edema, and tenderness. However, periorbital cellulitis is more commonly seen after minor trauma to the eyelid skin or related to a stye or chalazion. Orbital cellulitis, which is considerably more serious, is typically associated with sinus disease or abscess.30
Patients with orbital cellulitis will present with restricted eye movements, decreased visual acuity, proptosis, and possibly an RAPD. These patients will often have pain as well. A fine-cut computed tomography of the orbits aids in diagnosis.31
Care for each is different. Oral antibiotics are usually sufficient for patients with periorbital cellulitis, but for orbital cellulitis, a same-day ophthalmology referral and hospitalization for treatment with parenteral antibiotics is required.9,32
Subconjunctival hemorrhage—dramatic but harmless
While dramatic in appearance, subconjunctival hemorrhage generally does not affect vision. It may be the result of trauma to the globe, but can also occur spontaneously.
On physical exam, you’ll see bleeding into the conjunctiva that stops at the edge of the cornea. Visual acuity will be normal, as will the remainder of the eye examination. Abnormal vision, pain, or significant or recurrent bleeding should prompt a search for an alternative diagnosis. No treatment is needed for a simple subconjunctival hemorrhage.4
5) "My eye hurts"
Patients complaining of eye pain with or without vision changes—and without redness—usually have a medical history that leads to the diagnosis (TABLE).1,2,4,33-38 Physical exam findings are compatible with the history.
Optic neuritis. Patients with optic neuritis have acute to subacute vision loss, usually in one eye but sometimes bilaterally, lasting hours to days. Optic neuritis is more common in women and in those ages 15 to 45 years, with an incidence of 5 in 100,000 among Caucasians.33 Pain with eye movement is present in more than 90% of adults with optic neuritis,34 and is also common in children.35
In addition to vision loss, patients will report decreased detection of light and color,6 and examination will reveal an RAPD.1,2 Vision returns without treatment to the same extent as with treatment, but treatment will speed recovery.36 Patients with optic neuritis require an urgent referral to an ophthalmologist or neurologist to evaluate for multiple sclerosis, which develops in about 30% of those with optic neuritis.4,33
Corneal abrasion. Pain, localized to the surface of the eye, will be the primary complaint of patients with a corneal abrasion, who may or may not have loss of vision. Larger and deeper abrasions are extremely painful, while smaller corneal abrasions may be experienced as a foreign body sensation. The typical patient with a corneal abrasion is likely to have had trauma to the eye.37
Fluorescein is used to examine the patient with a suspected abrasion to highlight the epithelial defect.1 Visual acuity needs to be tested, and checked using a pinhole if it is below baseline.37 Treatment protocols range from artificial tears to antibiotic drops or ointments. Topical steroids should be given to patients only by an ophthalmologist.4
Is patching necessary? In a systematic review comparing outcomes based on the use of patching vs not patching on the first day of injury, patients who were not given patches fared the same or better than those whose eyes were patched, both in terms of healing time and pain relief. Primary care physicians can treat most corneal abrasions, and symptoms typically resolve in 2 days.38
1. Wright JL, Wightman JM. Red and painful eye. In: Marx JA, Hockberger RS, Walls RM, et al, eds. Rosen’s Emergency Medicine: Concepts and Clinical Practice. 7th ed. Philadelphia, Pa: Mosby Elsevier; 2009:chap 32.
2. Knoop KJ, Dennis WR, Hedges JR. Ophthalmologic procedures. In: Roberts JR, Hedges JR, eds. Clinical Procedures in Emergency Medicine. 5th ed. Philadelphia, Pa: Saunders Elsevier;2009:chap 63.
3. Ehlers JP, Fekrat S. Retinal vein occlusion: beyond the acute event. Surv Ophthalmol. 2011;56:281-299.
4. Sharma R, Brunette DD. Ophthalmology. In: Marx JA, Hockberger RS, Walls RM, et al, eds. Rosen’s Emergency Medicine: Concepts and Clinical Practice. 7th ed. Philadelphia, Pa: Mosby Elsevier; 2009:chap 69.
5. Cugati S, Varma DD, Chen CS, et al. Treatment options for central retinal artery occlusion. Curr Treat Options Neurol. 2013;15:63-77.
6. Matson M, Fujimoto L. Bilateral arteritic anterior ischemic optic neuropathy. Optometry. 2011;82:622-631.
7. McIntosh RL, Rogers SL, Lim L, et al. Natural history of central retinal vein occlusion: an evidence-based systematic review. Ophthalmology. 2010;117:1113-1123.
8. Wong TY, Scott IU. Retinal-vein occlusion. N Engl J Med. 2010;363:2135-2144.
9. Crouch ER, Crouch ER, Grant T. Ophthalmology. In: Rakel RE, ed. Textbook of Family Medicine. 8th ed. Philadelphia, Pa: Saunders Elsevier; 2011:chap 41.
10. Dickersin K, Manheimer E, Li T. Surgery for nonarteritic anterior ischemic optic neuropathy. Cochrane Database Syst Rev. 2012;(1):CD001538.
11. Thurtell MJ, Tomsak RL. Neuro-ophthalmology: afferent visual system. In: Daroff RB, Fenichel GM, Jankovic J, et al, eds. Bradley’s Neurology in Clinical Practice. 6th ed. Los Angeles, Calif: Saunders Elsevier; 2012:chap 36.
12. Yanoff M, Cameron D. Diseases of the visual system. In: Goldman L, Schafer AI, eds. Cecil Medicine. 24th ed. Philadelphia, Pa: Saunders Elsevier; 2011:chap 431.
13. Hollands H, Johnson D, Brox A, et al. Acute-onset floaters and flashes: is this patient at risk for retinal detachment? JAMA. 2009;302:2243-2249.
14. D’Amico DJ. Primary retinal detachment. N Engl J Med. 2008;359:2346-2354.
15. Hunsley T, Lee C. Does a normal-shaped pupil exclude the diagnosis of iritis? Best evidence topic reports. Towards evidence-based emergency medicine: best BETs from the Manchester Royal Infirmary. Emerg Med J. 2006;23:872-877.
16. Islam N, Pavesio C. Uveitis (acute anterior). Clin Evid. 2010;4:705.
17. Grunwald L, Newcomb CW, Daniel E, et al. Risk of relapse in primary acute anterior uveitis. Ophthalmology. 2011;118:1911-1915.
18. Thomas PA, Geraldine P. Infectious keratitis. Curr Opin Infect Dis. 2007;20:129-141.
19. Suwan-Apichon O, Reyes JM, Herretes S, et al. Topical corticosteroids as adjunctive therapy for bacterial keratitis. Cochrane Database Syst Rev. 2007;(4):CD005430.
20. Morris D, Latham E. Ulcers in the eye. J Emerg Med. 2012;42:62-64.
21. Wilhelmus KR. Antiviral treatment and other therapeutic interventions for herpes simplex virus epithelial keratitis. Cochrane Database Syst Rev. 2010;(12):CD002898.
22. Yagci A, Bozkurt B, Egrilmez S, et al. Topical anesthetic abuse keratopathy: a commonly overlooked health care problem.Cornea. 2011;30:571-575.
23. Cholongitas E, Pipili C, Dasenaki M. Acute angle closure glaucoma presented with nausea and epigastric pain. Dig Dis Sci. 2008;53:1430-1431.
24. White J. Diagnosis and management of acute angle-closure glaucoma. Emerg Nurse. 2011;19:27.
25. Lama DSC, Thama CCY, Laia JSM, et al. Current approaches to the management of acute primary angle closure. Curr Opin Ophthalmol. 2007;18:146-151.
26. Gharaibeh A, Savage HI, Scherer RW, et al. Medical interventions for traumatic hyphema. Cochrane Database Syst Rev. 2011;(1):CD005431.
27. Connor AJ, Severn P. Use of a control test to aid pH assessment of chemical eye injuries. Emerg Med J. 2009;26:811-812.
28. Sambursky R, Trattler W, Tauber S, et al. Sensitivity and specificity of the AdenoPlus test for diagnosing adenoviral conjunctivitis. JAMA Ophthalmol. 2013;131:17-22.
29. Sheikh A, Hurwitz B. Antibiotics versus placebo for acute bacterial conjunctivitis. Cochrane Database Syst Rev. 2006;(2):CD001211.
30. Papier A, Tuttle DJ, Mahara TJ. Differential diagnosis of the swollen red eyelid. Am Fam Physician. 2007;76:1815-1824.
31. Howe L, Jones NS. Guidelines for the management of periorbital cellulitis/abscess. Clin Otolaryngol. 2004;29:725-728.
32. Mahalingam-Dhingra A, Lander L, Preciado DA, et al. Orbital and periorbital infections: a national perspective. Arch Otolaryngol Head Neck Surg. 2011;137:769-773.
33. Germann CA, Baumann MR, Hamzavi S. Ophthalmic diagnoses in the ED: optic neuritis. Am J Emerg Med. 2007;25:834-837.
34. Balcer LJ. Optic neuritis. N Engl J Med. 2006;354:1273-1280.
35. Olitsky SE, Hug D, Plummer L, et al. Abnormalities of the optic nerve. In: Kliegman RM, Behrman RE, Jenson HB, et al, eds.Nelson Textbook of Pediatrics. 19th ed. Philadelphia, Pa: Saunders Elsevier; 2011:chap 623.
36. Gal RL, Vedula SS, Beck R. Corticosteroids for treating optic neuritis. Cochrane Database Syst Rev. 2012;(4):CD001430.
37. Aslam SA, Sheth HG, Vaughan AJ. Emergency management of corneal injuries. Injury. 2007;38:594-597.
38. Turner A, Rabiu M. Patching for corneal abrasion. Cochrane Database Syst Rev. 2006;(2):CD004764.
1. Wright JL, Wightman JM. Red and painful eye. In: Marx JA, Hockberger RS, Walls RM, et al, eds. Rosen’s Emergency Medicine: Concepts and Clinical Practice. 7th ed. Philadelphia, Pa: Mosby Elsevier; 2009:chap 32.
2. Knoop KJ, Dennis WR, Hedges JR. Ophthalmologic procedures. In: Roberts JR, Hedges JR, eds. Clinical Procedures in Emergency Medicine. 5th ed. Philadelphia, Pa: Saunders Elsevier;2009:chap 63.
3. Ehlers JP, Fekrat S. Retinal vein occlusion: beyond the acute event. Surv Ophthalmol. 2011;56:281-299.
4. Sharma R, Brunette DD. Ophthalmology. In: Marx JA, Hockberger RS, Walls RM, et al, eds. Rosen’s Emergency Medicine: Concepts and Clinical Practice. 7th ed. Philadelphia, Pa: Mosby Elsevier; 2009:chap 69.
5. Cugati S, Varma DD, Chen CS, et al. Treatment options for central retinal artery occlusion. Curr Treat Options Neurol. 2013;15:63-77.
6. Matson M, Fujimoto L. Bilateral arteritic anterior ischemic optic neuropathy. Optometry. 2011;82:622-631.
7. McIntosh RL, Rogers SL, Lim L, et al. Natural history of central retinal vein occlusion: an evidence-based systematic review. Ophthalmology. 2010;117:1113-1123.
8. Wong TY, Scott IU. Retinal-vein occlusion. N Engl J Med. 2010;363:2135-2144.
9. Crouch ER, Crouch ER, Grant T. Ophthalmology. In: Rakel RE, ed. Textbook of Family Medicine. 8th ed. Philadelphia, Pa: Saunders Elsevier; 2011:chap 41.
10. Dickersin K, Manheimer E, Li T. Surgery for nonarteritic anterior ischemic optic neuropathy. Cochrane Database Syst Rev. 2012;(1):CD001538.
11. Thurtell MJ, Tomsak RL. Neuro-ophthalmology: afferent visual system. In: Daroff RB, Fenichel GM, Jankovic J, et al, eds. Bradley’s Neurology in Clinical Practice. 6th ed. Los Angeles, Calif: Saunders Elsevier; 2012:chap 36.
12. Yanoff M, Cameron D. Diseases of the visual system. In: Goldman L, Schafer AI, eds. Cecil Medicine. 24th ed. Philadelphia, Pa: Saunders Elsevier; 2011:chap 431.
13. Hollands H, Johnson D, Brox A, et al. Acute-onset floaters and flashes: is this patient at risk for retinal detachment? JAMA. 2009;302:2243-2249.
14. D’Amico DJ. Primary retinal detachment. N Engl J Med. 2008;359:2346-2354.
15. Hunsley T, Lee C. Does a normal-shaped pupil exclude the diagnosis of iritis? Best evidence topic reports. Towards evidence-based emergency medicine: best BETs from the Manchester Royal Infirmary. Emerg Med J. 2006;23:872-877.
16. Islam N, Pavesio C. Uveitis (acute anterior). Clin Evid. 2010;4:705.
17. Grunwald L, Newcomb CW, Daniel E, et al. Risk of relapse in primary acute anterior uveitis. Ophthalmology. 2011;118:1911-1915.
18. Thomas PA, Geraldine P. Infectious keratitis. Curr Opin Infect Dis. 2007;20:129-141.
19. Suwan-Apichon O, Reyes JM, Herretes S, et al. Topical corticosteroids as adjunctive therapy for bacterial keratitis. Cochrane Database Syst Rev. 2007;(4):CD005430.
20. Morris D, Latham E. Ulcers in the eye. J Emerg Med. 2012;42:62-64.
21. Wilhelmus KR. Antiviral treatment and other therapeutic interventions for herpes simplex virus epithelial keratitis. Cochrane Database Syst Rev. 2010;(12):CD002898.
22. Yagci A, Bozkurt B, Egrilmez S, et al. Topical anesthetic abuse keratopathy: a commonly overlooked health care problem.Cornea. 2011;30:571-575.
23. Cholongitas E, Pipili C, Dasenaki M. Acute angle closure glaucoma presented with nausea and epigastric pain. Dig Dis Sci. 2008;53:1430-1431.
24. White J. Diagnosis and management of acute angle-closure glaucoma. Emerg Nurse. 2011;19:27.
25. Lama DSC, Thama CCY, Laia JSM, et al. Current approaches to the management of acute primary angle closure. Curr Opin Ophthalmol. 2007;18:146-151.
26. Gharaibeh A, Savage HI, Scherer RW, et al. Medical interventions for traumatic hyphema. Cochrane Database Syst Rev. 2011;(1):CD005431.
27. Connor AJ, Severn P. Use of a control test to aid pH assessment of chemical eye injuries. Emerg Med J. 2009;26:811-812.
28. Sambursky R, Trattler W, Tauber S, et al. Sensitivity and specificity of the AdenoPlus test for diagnosing adenoviral conjunctivitis. JAMA Ophthalmol. 2013;131:17-22.
29. Sheikh A, Hurwitz B. Antibiotics versus placebo for acute bacterial conjunctivitis. Cochrane Database Syst Rev. 2006;(2):CD001211.
30. Papier A, Tuttle DJ, Mahara TJ. Differential diagnosis of the swollen red eyelid. Am Fam Physician. 2007;76:1815-1824.
31. Howe L, Jones NS. Guidelines for the management of periorbital cellulitis/abscess. Clin Otolaryngol. 2004;29:725-728.
32. Mahalingam-Dhingra A, Lander L, Preciado DA, et al. Orbital and periorbital infections: a national perspective. Arch Otolaryngol Head Neck Surg. 2011;137:769-773.
33. Germann CA, Baumann MR, Hamzavi S. Ophthalmic diagnoses in the ED: optic neuritis. Am J Emerg Med. 2007;25:834-837.
34. Balcer LJ. Optic neuritis. N Engl J Med. 2006;354:1273-1280.
35. Olitsky SE, Hug D, Plummer L, et al. Abnormalities of the optic nerve. In: Kliegman RM, Behrman RE, Jenson HB, et al, eds.Nelson Textbook of Pediatrics. 19th ed. Philadelphia, Pa: Saunders Elsevier; 2011:chap 623.
36. Gal RL, Vedula SS, Beck R. Corticosteroids for treating optic neuritis. Cochrane Database Syst Rev. 2012;(4):CD001430.
37. Aslam SA, Sheth HG, Vaughan AJ. Emergency management of corneal injuries. Injury. 2007;38:594-597.
38. Turner A, Rabiu M. Patching for corneal abrasion. Cochrane Database Syst Rev. 2006;(2):CD004764.