User login
There is ample evidence in the medical literature, as well as clinical experience, that patients seeking help for chemical dependency benefit from pharmacotherapy. It is common, however, for physicians, patients, and family to balk at the idea. Even within the psychiatry community, where there should be better understanding of substance use disorders, many practitioners hesitate to employ medications, especially for alcohol use disorder (AUD).
Efficacy for such FDA-approved medications has been demonstrated in well-designed, randomized controlled trials, but many trainees, and even experienced professionals, have never seen these medications used effectively and appropriately. Medication-assisted treatment (MAT) is not an alternative to biopsychosocial approaches but is an augmentation that can (1) help stabilize the patient until he (she) can be educated in relapse prevention skills and (2) allow the brain to rewire and heal until he regains impulse control.
Diverse presentations
Do you remember that patient who often arrived for appointments intoxicated, promising that he plans to cut down? How about the man you saw in the emergency department with an elevated blood alcohol level, who was constantly endorsing suicidal thoughts that subsided when he reached clinical sobriety? What about the college student who often was treated for alcohol poisoning after binge drinking on weekends, but who never considered this behavior problematic? And, how about the elderly woman who was evaluated for anxiety, but had been drinking 4 beers nightly for the past 30 years?
Despite the diverse presentations, these patients all have a chronic disease and we fail them when we do not apply evidence-based medicine to their treatment.
As psychiatrists, we encounter many patients with AUD as a primary or comorbid diagnosis. This is a global problem associated with significant human and financial cost. With 80% of American adolescents having reported using alcohol in the past year, the problem will continue to grow.1 Furthermore, a greater prevalence of AUD is noted in clinical populations undergoing psychiatric treatment.2 Ongoing alcohol abuse complicates the course of medical and psychiatric conditions and incites significant societal exclusion.
Pharmacotherapy is underutilized
Despite an increase in the use of psychotropic medications for treating psychiatric illness, pharmacotherapy for AUD is underutilized: only 3% of patients have received an FDA-approved treatment.2,3 Nearly one-third of adults are affected by AUD during their lifetime, yet only 20% seek help.3 Management today remains limited to episodic, brief inpatient detoxification and psychosocial therapy.
Recovery rates are highest when addiction treatment that monitors abstinence is continuous; yet, for most part, alcohol addiction is treated in discrete episodes upon relapse. Although MAT is recommended by experts for “moderate” and “severe” substance use disorders, practitioners, in general, have demonstrated considerable resistance to using this modality as part of routine practice.4,5 This is regrettable: Regardless of terminology used to describe their condition, these people suffer a potentially fatal disease characterized by high post-treatment recidivism.
Neuroscience supports the brain disease model of addiction, with neuroplasticity changes being made during phases of drug use. Medications are shown to assist in preventing relapse while the brain is healing and normal emotional and decision-making capacities are being restored.6
Why hesitate to use pharmacotherapeutics?
There are diverse pharmacotherapeutic options that can be pursued for treating AUD with minimal disruption to home and work life. Alarmingly, many trainees have never prescribed or even considered such medications. Despite modest effect sizes in randomized controlled trials, efficacy has been demonstrated in reducing relapse rates and overall severity of drinking days.4,5 So, from where does the ambivalence of patients and providers about using these treatments to achieve lasting recovery stem?
Starting MAT certainly requires both parties to be in agreement. A patient might decline medication because of a fear of dependence or because he overestimates his ability to achieve remission on his own. There also may be financial barriers in a current alcohol treatment system that is traditionally non-medically oriented. Prescribers also fail to offer medications because of:
- lack of familiarity with available agents
- absence of guidelines for use
- disbelief that the condition is treatable.
Given that treatment often is based on a 12-step approach, such as Alcoholics Anonymous (AA), providers might hesitate to prescribe medication for an illness that is thought to be managed through psychosocial interventions, such as group and motivational therapy.
Therapeutic options
Choice of medication depends on the prescriber’s comfort level, reputation of the medication, potential side-effect profile, medical contraindications, and affordability; the most important consideration, however, should be the overall goals and expectations of the patient.
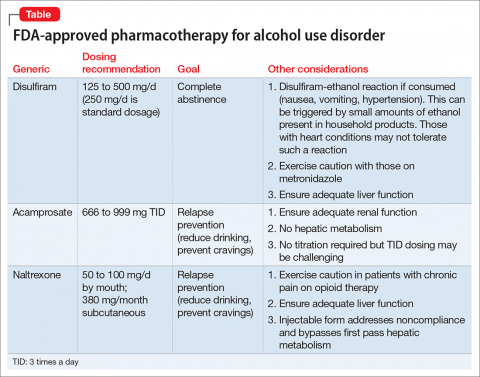
There are 4 FDA-approved medications for AUD (Table); many others are off-label. It is advisable to start with an FDA-approved medication such as disulfiram for the motivated patient who has a collaborator and desires complete abstinence; naltrexone for a patient who wants to cut down on intake (a long-acting formulation can be used for poorly adherent patients); and acamprosate for a patient with at least some established sobriety who needs help with post-withdrawal sleep disturbances.
With regard to off-label medications, topiramate has the highest evidence for efficacy. Gabapentin can augment naltrexone and also helps with sleep, anxiety, withdrawal, and cravings.4,5
Psychosocial interventions
Medications are just 1 tool in recovery; patients should be engaged in a program of counseling. Encourage attendance at AA meetings. An up-and-coming concept is the use of smartphone applications to prevent relapse (or even induce remission); apps that provide an accurate blood alcohol tracking systems and integrated psychosocial therapies are in the pipeline. The novel Reddit online forum r/StopDrinking is a 24-hour peer-support community that relies on
fellowship, accountability, monitoring, and anonymity; the forum can compete with
motivational interviewing for efficacy in increasing abstinence and preventing relapse.
1. Johnson L, O’Malley P, Miech RA, et al. Monitoring the Future national survey results on drug use, 1975-2015: overview, key findings on adolescent drug use. http://www.monitoringthefuture.org/pubs/monographs/mtf-overview2015.pdf. Published February 2016. Accessed January 20, 2016.
2. Substance Abuse and Mental Health Services Administration. Results from the 2013 national survey on drug use and health: mental health findings, NSDUH Series H-49, HHS Publication No. (SMA) 14-4887. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2014.
3. Grant BF, Goldstein RB, Saha TD, et al. Epidemiology of DSM-5 alcohol use disorder: results from the National Epidemiological Survey on Alcohol and Related Conditions III. JAMA Psychiatry. 2015;72(8):757-766.
4. Robinson S, Meeks TW, Geniza C. Medication for alcohol use disorder: which agents work best. Current Psychiatry. 2014;13(1):22-29.
5. Substance Abuse and Mental Health Services Administration and National Institute on Alcohol Abuse and Alcoholism. Medication for the treatment of alcohol use disorder: a brief guide. HHS Publication No. (SMA) 15-4907. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2015.
6. Volkow ND, Koob GF, McLellan AT. Neurobiological advances from the brain disease model of addiction. N Engl J Med. 2016;374(4):363-371.
Acknowledgment
The authors would like to thank Thomas M. Penders, MS, MD, Medical Director for Consultation-Liaison Psychiatry at Cape Cod Healthcare, Hyannis, Massachusetts, and Affiliate Professor at East Carolina University, Greenville, North Carolina, for all his guidance, support, and mentorship.
There is ample evidence in the medical literature, as well as clinical experience, that patients seeking help for chemical dependency benefit from pharmacotherapy. It is common, however, for physicians, patients, and family to balk at the idea. Even within the psychiatry community, where there should be better understanding of substance use disorders, many practitioners hesitate to employ medications, especially for alcohol use disorder (AUD).
Efficacy for such FDA-approved medications has been demonstrated in well-designed, randomized controlled trials, but many trainees, and even experienced professionals, have never seen these medications used effectively and appropriately. Medication-assisted treatment (MAT) is not an alternative to biopsychosocial approaches but is an augmentation that can (1) help stabilize the patient until he (she) can be educated in relapse prevention skills and (2) allow the brain to rewire and heal until he regains impulse control.
Diverse presentations
Do you remember that patient who often arrived for appointments intoxicated, promising that he plans to cut down? How about the man you saw in the emergency department with an elevated blood alcohol level, who was constantly endorsing suicidal thoughts that subsided when he reached clinical sobriety? What about the college student who often was treated for alcohol poisoning after binge drinking on weekends, but who never considered this behavior problematic? And, how about the elderly woman who was evaluated for anxiety, but had been drinking 4 beers nightly for the past 30 years?
Despite the diverse presentations, these patients all have a chronic disease and we fail them when we do not apply evidence-based medicine to their treatment.
As psychiatrists, we encounter many patients with AUD as a primary or comorbid diagnosis. This is a global problem associated with significant human and financial cost. With 80% of American adolescents having reported using alcohol in the past year, the problem will continue to grow.1 Furthermore, a greater prevalence of AUD is noted in clinical populations undergoing psychiatric treatment.2 Ongoing alcohol abuse complicates the course of medical and psychiatric conditions and incites significant societal exclusion.
Pharmacotherapy is underutilized
Despite an increase in the use of psychotropic medications for treating psychiatric illness, pharmacotherapy for AUD is underutilized: only 3% of patients have received an FDA-approved treatment.2,3 Nearly one-third of adults are affected by AUD during their lifetime, yet only 20% seek help.3 Management today remains limited to episodic, brief inpatient detoxification and psychosocial therapy.
Recovery rates are highest when addiction treatment that monitors abstinence is continuous; yet, for most part, alcohol addiction is treated in discrete episodes upon relapse. Although MAT is recommended by experts for “moderate” and “severe” substance use disorders, practitioners, in general, have demonstrated considerable resistance to using this modality as part of routine practice.4,5 This is regrettable: Regardless of terminology used to describe their condition, these people suffer a potentially fatal disease characterized by high post-treatment recidivism.
Neuroscience supports the brain disease model of addiction, with neuroplasticity changes being made during phases of drug use. Medications are shown to assist in preventing relapse while the brain is healing and normal emotional and decision-making capacities are being restored.6
Why hesitate to use pharmacotherapeutics?
There are diverse pharmacotherapeutic options that can be pursued for treating AUD with minimal disruption to home and work life. Alarmingly, many trainees have never prescribed or even considered such medications. Despite modest effect sizes in randomized controlled trials, efficacy has been demonstrated in reducing relapse rates and overall severity of drinking days.4,5 So, from where does the ambivalence of patients and providers about using these treatments to achieve lasting recovery stem?
Starting MAT certainly requires both parties to be in agreement. A patient might decline medication because of a fear of dependence or because he overestimates his ability to achieve remission on his own. There also may be financial barriers in a current alcohol treatment system that is traditionally non-medically oriented. Prescribers also fail to offer medications because of:
- lack of familiarity with available agents
- absence of guidelines for use
- disbelief that the condition is treatable.
Given that treatment often is based on a 12-step approach, such as Alcoholics Anonymous (AA), providers might hesitate to prescribe medication for an illness that is thought to be managed through psychosocial interventions, such as group and motivational therapy.
Therapeutic options
Choice of medication depends on the prescriber’s comfort level, reputation of the medication, potential side-effect profile, medical contraindications, and affordability; the most important consideration, however, should be the overall goals and expectations of the patient.
There are 4 FDA-approved medications for AUD (Table); many others are off-label. It is advisable to start with an FDA-approved medication such as disulfiram for the motivated patient who has a collaborator and desires complete abstinence; naltrexone for a patient who wants to cut down on intake (a long-acting formulation can be used for poorly adherent patients); and acamprosate for a patient with at least some established sobriety who needs help with post-withdrawal sleep disturbances.
With regard to off-label medications, topiramate has the highest evidence for efficacy. Gabapentin can augment naltrexone and also helps with sleep, anxiety, withdrawal, and cravings.4,5
Psychosocial interventions
Medications are just 1 tool in recovery; patients should be engaged in a program of counseling. Encourage attendance at AA meetings. An up-and-coming concept is the use of smartphone applications to prevent relapse (or even induce remission); apps that provide an accurate blood alcohol tracking systems and integrated psychosocial therapies are in the pipeline. The novel Reddit online forum r/StopDrinking is a 24-hour peer-support community that relies on
fellowship, accountability, monitoring, and anonymity; the forum can compete with
motivational interviewing for efficacy in increasing abstinence and preventing relapse.
There is ample evidence in the medical literature, as well as clinical experience, that patients seeking help for chemical dependency benefit from pharmacotherapy. It is common, however, for physicians, patients, and family to balk at the idea. Even within the psychiatry community, where there should be better understanding of substance use disorders, many practitioners hesitate to employ medications, especially for alcohol use disorder (AUD).
Efficacy for such FDA-approved medications has been demonstrated in well-designed, randomized controlled trials, but many trainees, and even experienced professionals, have never seen these medications used effectively and appropriately. Medication-assisted treatment (MAT) is not an alternative to biopsychosocial approaches but is an augmentation that can (1) help stabilize the patient until he (she) can be educated in relapse prevention skills and (2) allow the brain to rewire and heal until he regains impulse control.
Diverse presentations
Do you remember that patient who often arrived for appointments intoxicated, promising that he plans to cut down? How about the man you saw in the emergency department with an elevated blood alcohol level, who was constantly endorsing suicidal thoughts that subsided when he reached clinical sobriety? What about the college student who often was treated for alcohol poisoning after binge drinking on weekends, but who never considered this behavior problematic? And, how about the elderly woman who was evaluated for anxiety, but had been drinking 4 beers nightly for the past 30 years?
Despite the diverse presentations, these patients all have a chronic disease and we fail them when we do not apply evidence-based medicine to their treatment.
As psychiatrists, we encounter many patients with AUD as a primary or comorbid diagnosis. This is a global problem associated with significant human and financial cost. With 80% of American adolescents having reported using alcohol in the past year, the problem will continue to grow.1 Furthermore, a greater prevalence of AUD is noted in clinical populations undergoing psychiatric treatment.2 Ongoing alcohol abuse complicates the course of medical and psychiatric conditions and incites significant societal exclusion.
Pharmacotherapy is underutilized
Despite an increase in the use of psychotropic medications for treating psychiatric illness, pharmacotherapy for AUD is underutilized: only 3% of patients have received an FDA-approved treatment.2,3 Nearly one-third of adults are affected by AUD during their lifetime, yet only 20% seek help.3 Management today remains limited to episodic, brief inpatient detoxification and psychosocial therapy.
Recovery rates are highest when addiction treatment that monitors abstinence is continuous; yet, for most part, alcohol addiction is treated in discrete episodes upon relapse. Although MAT is recommended by experts for “moderate” and “severe” substance use disorders, practitioners, in general, have demonstrated considerable resistance to using this modality as part of routine practice.4,5 This is regrettable: Regardless of terminology used to describe their condition, these people suffer a potentially fatal disease characterized by high post-treatment recidivism.
Neuroscience supports the brain disease model of addiction, with neuroplasticity changes being made during phases of drug use. Medications are shown to assist in preventing relapse while the brain is healing and normal emotional and decision-making capacities are being restored.6
Why hesitate to use pharmacotherapeutics?
There are diverse pharmacotherapeutic options that can be pursued for treating AUD with minimal disruption to home and work life. Alarmingly, many trainees have never prescribed or even considered such medications. Despite modest effect sizes in randomized controlled trials, efficacy has been demonstrated in reducing relapse rates and overall severity of drinking days.4,5 So, from where does the ambivalence of patients and providers about using these treatments to achieve lasting recovery stem?
Starting MAT certainly requires both parties to be in agreement. A patient might decline medication because of a fear of dependence or because he overestimates his ability to achieve remission on his own. There also may be financial barriers in a current alcohol treatment system that is traditionally non-medically oriented. Prescribers also fail to offer medications because of:
- lack of familiarity with available agents
- absence of guidelines for use
- disbelief that the condition is treatable.
Given that treatment often is based on a 12-step approach, such as Alcoholics Anonymous (AA), providers might hesitate to prescribe medication for an illness that is thought to be managed through psychosocial interventions, such as group and motivational therapy.
Therapeutic options
Choice of medication depends on the prescriber’s comfort level, reputation of the medication, potential side-effect profile, medical contraindications, and affordability; the most important consideration, however, should be the overall goals and expectations of the patient.
There are 4 FDA-approved medications for AUD (Table); many others are off-label. It is advisable to start with an FDA-approved medication such as disulfiram for the motivated patient who has a collaborator and desires complete abstinence; naltrexone for a patient who wants to cut down on intake (a long-acting formulation can be used for poorly adherent patients); and acamprosate for a patient with at least some established sobriety who needs help with post-withdrawal sleep disturbances.
With regard to off-label medications, topiramate has the highest evidence for efficacy. Gabapentin can augment naltrexone and also helps with sleep, anxiety, withdrawal, and cravings.4,5
Psychosocial interventions
Medications are just 1 tool in recovery; patients should be engaged in a program of counseling. Encourage attendance at AA meetings. An up-and-coming concept is the use of smartphone applications to prevent relapse (or even induce remission); apps that provide an accurate blood alcohol tracking systems and integrated psychosocial therapies are in the pipeline. The novel Reddit online forum r/StopDrinking is a 24-hour peer-support community that relies on
fellowship, accountability, monitoring, and anonymity; the forum can compete with
motivational interviewing for efficacy in increasing abstinence and preventing relapse.
1. Johnson L, O’Malley P, Miech RA, et al. Monitoring the Future national survey results on drug use, 1975-2015: overview, key findings on adolescent drug use. http://www.monitoringthefuture.org/pubs/monographs/mtf-overview2015.pdf. Published February 2016. Accessed January 20, 2016.
2. Substance Abuse and Mental Health Services Administration. Results from the 2013 national survey on drug use and health: mental health findings, NSDUH Series H-49, HHS Publication No. (SMA) 14-4887. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2014.
3. Grant BF, Goldstein RB, Saha TD, et al. Epidemiology of DSM-5 alcohol use disorder: results from the National Epidemiological Survey on Alcohol and Related Conditions III. JAMA Psychiatry. 2015;72(8):757-766.
4. Robinson S, Meeks TW, Geniza C. Medication for alcohol use disorder: which agents work best. Current Psychiatry. 2014;13(1):22-29.
5. Substance Abuse and Mental Health Services Administration and National Institute on Alcohol Abuse and Alcoholism. Medication for the treatment of alcohol use disorder: a brief guide. HHS Publication No. (SMA) 15-4907. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2015.
6. Volkow ND, Koob GF, McLellan AT. Neurobiological advances from the brain disease model of addiction. N Engl J Med. 2016;374(4):363-371.
Acknowledgment
The authors would like to thank Thomas M. Penders, MS, MD, Medical Director for Consultation-Liaison Psychiatry at Cape Cod Healthcare, Hyannis, Massachusetts, and Affiliate Professor at East Carolina University, Greenville, North Carolina, for all his guidance, support, and mentorship.
1. Johnson L, O’Malley P, Miech RA, et al. Monitoring the Future national survey results on drug use, 1975-2015: overview, key findings on adolescent drug use. http://www.monitoringthefuture.org/pubs/monographs/mtf-overview2015.pdf. Published February 2016. Accessed January 20, 2016.
2. Substance Abuse and Mental Health Services Administration. Results from the 2013 national survey on drug use and health: mental health findings, NSDUH Series H-49, HHS Publication No. (SMA) 14-4887. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2014.
3. Grant BF, Goldstein RB, Saha TD, et al. Epidemiology of DSM-5 alcohol use disorder: results from the National Epidemiological Survey on Alcohol and Related Conditions III. JAMA Psychiatry. 2015;72(8):757-766.
4. Robinson S, Meeks TW, Geniza C. Medication for alcohol use disorder: which agents work best. Current Psychiatry. 2014;13(1):22-29.
5. Substance Abuse and Mental Health Services Administration and National Institute on Alcohol Abuse and Alcoholism. Medication for the treatment of alcohol use disorder: a brief guide. HHS Publication No. (SMA) 15-4907. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2015.
6. Volkow ND, Koob GF, McLellan AT. Neurobiological advances from the brain disease model of addiction. N Engl J Med. 2016;374(4):363-371.
Acknowledgment
The authors would like to thank Thomas M. Penders, MS, MD, Medical Director for Consultation-Liaison Psychiatry at Cape Cod Healthcare, Hyannis, Massachusetts, and Affiliate Professor at East Carolina University, Greenville, North Carolina, for all his guidance, support, and mentorship.