User login
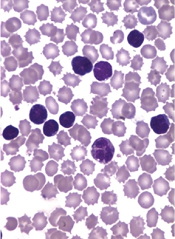
Researchers say lenalidomide exhibited clinically meaningful antitumor activity and an acceptable safety profile in a phase 2 study of patients with relapsed adult T-cell leukemia/lymphoma (ATLL).
Of the 26 patients enrolled in the trial, 42% responded to lenalidomide, and 35% experienced serious adverse events (AEs).
Results from this trial were published in the Journal of Clinical Oncology. Data were previously presented at the 8th Annual T-cell Lymphoma Forum. The study was sponsored by Celgene K.K.
Patients and treatment
All 26 patients had relapsed ATLL—15 with the acute subtype, 7 with the lymphoma subtype, and 4 with the unfavorable chronic subtype. The patients’ median age was 68.5 (range, 53-81), all were Japanese, and 54% were male.
The median number of prior treatment regimens was 2 (range, 1-4). Thirty-five percent of patients had prior mogamulizumab (n=9), 35% had received LSG15 (n=3) or modified LSG15 (n=6), and 27% had prior CHOP (n=7).
The patients received lenalidomide at 25 mg per day, given continuously until disease progression or intolerability.
Results
Five patients (19%) were still receiving lenalidomide at the data cutoff, which was November 20, 2014.
Thirteen patients (50%) stopped treatment due to progression, 6 (23%) because of AEs, 1 (4%) due to investigator decision, and 1 (4%) because of concerns about the increased possibility of disease recurrence.
The median follow-up was 3.9 months. Eleven patients (42%) responded to lenalidomide, including 4 complete responses and 1 unconfirmed complete response.
The median duration of response was not reached (range, 0.5 months to not reached), and the mean duration of response was 5.2 months (range, 0 to 16.6 months).
The median progression-free survival was 3.8 months (range, 1.9 months to not reached), and the median overall survival was 20.3 months (range, 9.1 months to not reached).
Nine patients (35%) experienced serious AEs. The only serious AE that occurred in more than 1 patient was thrombocytopenia, which occurred in 2 patients.
The most frequent AEs of any grade were thrombocytopenia (77%), neutropenia (73%), lymphopenia (69%), anemia (54%), and leukopenia (50%).
The most frequent grade 3 or higher AEs were neutropenia (65%), leukopenia (38%), lymphopenia (38%), and thrombocytopenia (23%). These events were all manageable and reversible, according to the researchers.
Based on these results, the team concluded that lenalidomide warrants further investigation as a treatment for ATLL. ![]()
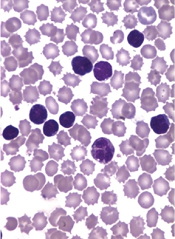
Researchers say lenalidomide exhibited clinically meaningful antitumor activity and an acceptable safety profile in a phase 2 study of patients with relapsed adult T-cell leukemia/lymphoma (ATLL).
Of the 26 patients enrolled in the trial, 42% responded to lenalidomide, and 35% experienced serious adverse events (AEs).
Results from this trial were published in the Journal of Clinical Oncology. Data were previously presented at the 8th Annual T-cell Lymphoma Forum. The study was sponsored by Celgene K.K.
Patients and treatment
All 26 patients had relapsed ATLL—15 with the acute subtype, 7 with the lymphoma subtype, and 4 with the unfavorable chronic subtype. The patients’ median age was 68.5 (range, 53-81), all were Japanese, and 54% were male.
The median number of prior treatment regimens was 2 (range, 1-4). Thirty-five percent of patients had prior mogamulizumab (n=9), 35% had received LSG15 (n=3) or modified LSG15 (n=6), and 27% had prior CHOP (n=7).
The patients received lenalidomide at 25 mg per day, given continuously until disease progression or intolerability.
Results
Five patients (19%) were still receiving lenalidomide at the data cutoff, which was November 20, 2014.
Thirteen patients (50%) stopped treatment due to progression, 6 (23%) because of AEs, 1 (4%) due to investigator decision, and 1 (4%) because of concerns about the increased possibility of disease recurrence.
The median follow-up was 3.9 months. Eleven patients (42%) responded to lenalidomide, including 4 complete responses and 1 unconfirmed complete response.
The median duration of response was not reached (range, 0.5 months to not reached), and the mean duration of response was 5.2 months (range, 0 to 16.6 months).
The median progression-free survival was 3.8 months (range, 1.9 months to not reached), and the median overall survival was 20.3 months (range, 9.1 months to not reached).
Nine patients (35%) experienced serious AEs. The only serious AE that occurred in more than 1 patient was thrombocytopenia, which occurred in 2 patients.
The most frequent AEs of any grade were thrombocytopenia (77%), neutropenia (73%), lymphopenia (69%), anemia (54%), and leukopenia (50%).
The most frequent grade 3 or higher AEs were neutropenia (65%), leukopenia (38%), lymphopenia (38%), and thrombocytopenia (23%). These events were all manageable and reversible, according to the researchers.
Based on these results, the team concluded that lenalidomide warrants further investigation as a treatment for ATLL. ![]()
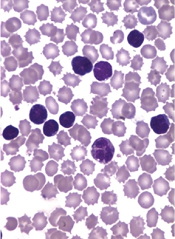
Researchers say lenalidomide exhibited clinically meaningful antitumor activity and an acceptable safety profile in a phase 2 study of patients with relapsed adult T-cell leukemia/lymphoma (ATLL).
Of the 26 patients enrolled in the trial, 42% responded to lenalidomide, and 35% experienced serious adverse events (AEs).
Results from this trial were published in the Journal of Clinical Oncology. Data were previously presented at the 8th Annual T-cell Lymphoma Forum. The study was sponsored by Celgene K.K.
Patients and treatment
All 26 patients had relapsed ATLL—15 with the acute subtype, 7 with the lymphoma subtype, and 4 with the unfavorable chronic subtype. The patients’ median age was 68.5 (range, 53-81), all were Japanese, and 54% were male.
The median number of prior treatment regimens was 2 (range, 1-4). Thirty-five percent of patients had prior mogamulizumab (n=9), 35% had received LSG15 (n=3) or modified LSG15 (n=6), and 27% had prior CHOP (n=7).
The patients received lenalidomide at 25 mg per day, given continuously until disease progression or intolerability.
Results
Five patients (19%) were still receiving lenalidomide at the data cutoff, which was November 20, 2014.
Thirteen patients (50%) stopped treatment due to progression, 6 (23%) because of AEs, 1 (4%) due to investigator decision, and 1 (4%) because of concerns about the increased possibility of disease recurrence.
The median follow-up was 3.9 months. Eleven patients (42%) responded to lenalidomide, including 4 complete responses and 1 unconfirmed complete response.
The median duration of response was not reached (range, 0.5 months to not reached), and the mean duration of response was 5.2 months (range, 0 to 16.6 months).
The median progression-free survival was 3.8 months (range, 1.9 months to not reached), and the median overall survival was 20.3 months (range, 9.1 months to not reached).
Nine patients (35%) experienced serious AEs. The only serious AE that occurred in more than 1 patient was thrombocytopenia, which occurred in 2 patients.
The most frequent AEs of any grade were thrombocytopenia (77%), neutropenia (73%), lymphopenia (69%), anemia (54%), and leukopenia (50%).
The most frequent grade 3 or higher AEs were neutropenia (65%), leukopenia (38%), lymphopenia (38%), and thrombocytopenia (23%). These events were all manageable and reversible, according to the researchers.
Based on these results, the team concluded that lenalidomide warrants further investigation as a treatment for ATLL. ![]()