User login
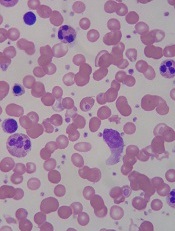
thalassemia
VIENNA—Data from a phase 2a trial suggest the activin receptor sotatercept can effectively treat patients with ß-thalassemia.
However, the companies developing the drug have decided not to advance sotatercept to phase 3 trials in this patient population.
Instead, the companies are initiating a phase 3 program with sotatercept’s “twin” activin receptor, luspatercept, in patients with ß-thalassemia or myelodysplastic syndromes.
Acceleron Pharma Inc. and Celgene Corporation are jointly developing both compounds. The companies plan to continue developing sotatercept for patients with chronic kidney disease.
Maria Domenica Cappellini, MD, of the University of Milan in Italy, presented results from the phase 2a study of sotatercept in ß-thalassemia at the 20th Congress of the European Hematology Association (abstract S137*).
Phase 2 results with luspatercept in ß-thalassemia were also presented at the meeting.
The dose-finding study of sotatercept had enrolled 46 patients at the time of Dr Cappellini’s presentation. The drug was given subcutaneously at doses ranging from 0.1 mg/kg to 1.0 mg/kg every 3 weeks.
The 30 non-transfusion-dependent (NTD) patients received 4 or fewer red blood cell (RBC) units in the 6 months prior to study enrollment. The 16 transfusion-dependent (TD) patients had received 2 or more RBC units every 30 days for 6 months or more prior to study enrollment.
Twenty-five of the 46 patients remain on treatment, with a median exposure time of 12.4 months.
NTD patients
The patients’ median age was 42, and 53% were female. Fifty-three percent had had a splenectomy, and the median baseline hemoglobin level was 8.4 g/dL.
Treatment with sotatercept produced a dose-dependent hemoglobin increase.
“[W]hat I found quite interesting is that the increase is consistent and persistent, [even] after 1 year,” Dr Cappellini said. “And they are still maintained on treatment, of course, but it is a sustained response.”
At the 0.75 mg/kg dose, 86% of patients had a hemoglobin increase of 1 g/dL for 12 weeks or more, and 71% had an increase of 1.5 g/dL.
TD patients
The patients’ median age was 36 years, and 38% were female. Three-quarters of patients had ß-thalassemia major, and a quarter had ß-thalassemia intermedia.
Nearly a third of patients had had a splenectomy, and their transfusion burden at baseline ranged from 8 RBC units to 35 RBC units every 24 weeks.
The mean reduction in transfusion burden among patients treated with sotatercept at doses of 0.5 mg/kg or higher was 32.25%. And the 1.0 mg/kg dose of sotatercept reduced one patient’s transfusion burden by 61.6%.
Dr Cappellini noted that the pharmacokinetic analysis showed a correlation with exposure. The investigators observed no apparent effects of weight, sex, age, or transfusion burden on drug clearance.
“So the relationship was probably more related to long-term exposure than to the real dosage,” she said.
Safety
Hypertension and bone pain were the most common grade 2-4, treatment-related adverse events.
Seven patients discontinued the study due to adverse events, one patient each with bone pain, superficial thrombophlebitis, ventricular extrasystole, spinal extramedullary erythropoietic tissue, and erythema at the injection site/allergic reaction. Two patients discontinued due to hypertension.
Dr Cappellini concluded that sotatercept and the related molecule, luspatercept, may provide a favorable risk-benefit profile for patients with ß-thalassemia.
“These 2 molecules are merging now for a phase 3 trial in either TD or NTD thalassemia cohorts,” she said. “The two drugs are actually very, very similar, and, in fact, for the trial, we decided to use only one. There is no way to go on with 2 molecules.”
In April, Acceleron and Celgene announced plans to initiate a phase 3 program with luspatercept in myelodysplastic syndromes and β-thalassemia by the end of this year. The companies said they will continue to develop sotatercept for patients with chronic kidney disease. ![]()
*Data in the abstract differ from the presentation.
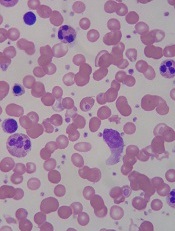
thalassemia
VIENNA—Data from a phase 2a trial suggest the activin receptor sotatercept can effectively treat patients with ß-thalassemia.
However, the companies developing the drug have decided not to advance sotatercept to phase 3 trials in this patient population.
Instead, the companies are initiating a phase 3 program with sotatercept’s “twin” activin receptor, luspatercept, in patients with ß-thalassemia or myelodysplastic syndromes.
Acceleron Pharma Inc. and Celgene Corporation are jointly developing both compounds. The companies plan to continue developing sotatercept for patients with chronic kidney disease.
Maria Domenica Cappellini, MD, of the University of Milan in Italy, presented results from the phase 2a study of sotatercept in ß-thalassemia at the 20th Congress of the European Hematology Association (abstract S137*).
Phase 2 results with luspatercept in ß-thalassemia were also presented at the meeting.
The dose-finding study of sotatercept had enrolled 46 patients at the time of Dr Cappellini’s presentation. The drug was given subcutaneously at doses ranging from 0.1 mg/kg to 1.0 mg/kg every 3 weeks.
The 30 non-transfusion-dependent (NTD) patients received 4 or fewer red blood cell (RBC) units in the 6 months prior to study enrollment. The 16 transfusion-dependent (TD) patients had received 2 or more RBC units every 30 days for 6 months or more prior to study enrollment.
Twenty-five of the 46 patients remain on treatment, with a median exposure time of 12.4 months.
NTD patients
The patients’ median age was 42, and 53% were female. Fifty-three percent had had a splenectomy, and the median baseline hemoglobin level was 8.4 g/dL.
Treatment with sotatercept produced a dose-dependent hemoglobin increase.
“[W]hat I found quite interesting is that the increase is consistent and persistent, [even] after 1 year,” Dr Cappellini said. “And they are still maintained on treatment, of course, but it is a sustained response.”
At the 0.75 mg/kg dose, 86% of patients had a hemoglobin increase of 1 g/dL for 12 weeks or more, and 71% had an increase of 1.5 g/dL.
TD patients
The patients’ median age was 36 years, and 38% were female. Three-quarters of patients had ß-thalassemia major, and a quarter had ß-thalassemia intermedia.
Nearly a third of patients had had a splenectomy, and their transfusion burden at baseline ranged from 8 RBC units to 35 RBC units every 24 weeks.
The mean reduction in transfusion burden among patients treated with sotatercept at doses of 0.5 mg/kg or higher was 32.25%. And the 1.0 mg/kg dose of sotatercept reduced one patient’s transfusion burden by 61.6%.
Dr Cappellini noted that the pharmacokinetic analysis showed a correlation with exposure. The investigators observed no apparent effects of weight, sex, age, or transfusion burden on drug clearance.
“So the relationship was probably more related to long-term exposure than to the real dosage,” she said.
Safety
Hypertension and bone pain were the most common grade 2-4, treatment-related adverse events.
Seven patients discontinued the study due to adverse events, one patient each with bone pain, superficial thrombophlebitis, ventricular extrasystole, spinal extramedullary erythropoietic tissue, and erythema at the injection site/allergic reaction. Two patients discontinued due to hypertension.
Dr Cappellini concluded that sotatercept and the related molecule, luspatercept, may provide a favorable risk-benefit profile for patients with ß-thalassemia.
“These 2 molecules are merging now for a phase 3 trial in either TD or NTD thalassemia cohorts,” she said. “The two drugs are actually very, very similar, and, in fact, for the trial, we decided to use only one. There is no way to go on with 2 molecules.”
In April, Acceleron and Celgene announced plans to initiate a phase 3 program with luspatercept in myelodysplastic syndromes and β-thalassemia by the end of this year. The companies said they will continue to develop sotatercept for patients with chronic kidney disease. ![]()
*Data in the abstract differ from the presentation.
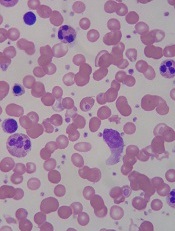
thalassemia
VIENNA—Data from a phase 2a trial suggest the activin receptor sotatercept can effectively treat patients with ß-thalassemia.
However, the companies developing the drug have decided not to advance sotatercept to phase 3 trials in this patient population.
Instead, the companies are initiating a phase 3 program with sotatercept’s “twin” activin receptor, luspatercept, in patients with ß-thalassemia or myelodysplastic syndromes.
Acceleron Pharma Inc. and Celgene Corporation are jointly developing both compounds. The companies plan to continue developing sotatercept for patients with chronic kidney disease.
Maria Domenica Cappellini, MD, of the University of Milan in Italy, presented results from the phase 2a study of sotatercept in ß-thalassemia at the 20th Congress of the European Hematology Association (abstract S137*).
Phase 2 results with luspatercept in ß-thalassemia were also presented at the meeting.
The dose-finding study of sotatercept had enrolled 46 patients at the time of Dr Cappellini’s presentation. The drug was given subcutaneously at doses ranging from 0.1 mg/kg to 1.0 mg/kg every 3 weeks.
The 30 non-transfusion-dependent (NTD) patients received 4 or fewer red blood cell (RBC) units in the 6 months prior to study enrollment. The 16 transfusion-dependent (TD) patients had received 2 or more RBC units every 30 days for 6 months or more prior to study enrollment.
Twenty-five of the 46 patients remain on treatment, with a median exposure time of 12.4 months.
NTD patients
The patients’ median age was 42, and 53% were female. Fifty-three percent had had a splenectomy, and the median baseline hemoglobin level was 8.4 g/dL.
Treatment with sotatercept produced a dose-dependent hemoglobin increase.
“[W]hat I found quite interesting is that the increase is consistent and persistent, [even] after 1 year,” Dr Cappellini said. “And they are still maintained on treatment, of course, but it is a sustained response.”
At the 0.75 mg/kg dose, 86% of patients had a hemoglobin increase of 1 g/dL for 12 weeks or more, and 71% had an increase of 1.5 g/dL.
TD patients
The patients’ median age was 36 years, and 38% were female. Three-quarters of patients had ß-thalassemia major, and a quarter had ß-thalassemia intermedia.
Nearly a third of patients had had a splenectomy, and their transfusion burden at baseline ranged from 8 RBC units to 35 RBC units every 24 weeks.
The mean reduction in transfusion burden among patients treated with sotatercept at doses of 0.5 mg/kg or higher was 32.25%. And the 1.0 mg/kg dose of sotatercept reduced one patient’s transfusion burden by 61.6%.
Dr Cappellini noted that the pharmacokinetic analysis showed a correlation with exposure. The investigators observed no apparent effects of weight, sex, age, or transfusion burden on drug clearance.
“So the relationship was probably more related to long-term exposure than to the real dosage,” she said.
Safety
Hypertension and bone pain were the most common grade 2-4, treatment-related adverse events.
Seven patients discontinued the study due to adverse events, one patient each with bone pain, superficial thrombophlebitis, ventricular extrasystole, spinal extramedullary erythropoietic tissue, and erythema at the injection site/allergic reaction. Two patients discontinued due to hypertension.
Dr Cappellini concluded that sotatercept and the related molecule, luspatercept, may provide a favorable risk-benefit profile for patients with ß-thalassemia.
“These 2 molecules are merging now for a phase 3 trial in either TD or NTD thalassemia cohorts,” she said. “The two drugs are actually very, very similar, and, in fact, for the trial, we decided to use only one. There is no way to go on with 2 molecules.”
In April, Acceleron and Celgene announced plans to initiate a phase 3 program with luspatercept in myelodysplastic syndromes and β-thalassemia by the end of this year. The companies said they will continue to develop sotatercept for patients with chronic kidney disease. ![]()
*Data in the abstract differ from the presentation.