User login
Airway fistula is a rare but life-threatening complication of esophageal surgery, but an innovative technique using two custom-made, Y-shaped metallic stents can preserve airway patency, researchers at Zhengzhou University in China reported in the August issue of the Journal of Thoracic and Cardiovascular Surgery (J Thorac Cardiovasc Surg. 2016;152:557-63).
The study involved 10 patients who received Y-shaped stents to treat gastrotracheal or gastrobronchial fistulas (GTFs and GBFs, respectively) after esophageal surgery from 2010 through 2014. “Our patients tolerated the stents well and had good palliation of their symptoms,” wrote Teng-Fei Li, MD, and colleagues.
Six patients died within 8 months for unrelated reasons – either tumors (four patients), or hemoptysis or pulmonary infection (one each). In one patient, the carinal fistula enlarged 4 months after stenting, but the researchers successfully placed an additional small Y-shaped stent. At the publication of the paper, this patient and three others had survived, Dr. Li and colleagues said.
After esophagectomy, fistulas can form between the tracheobronchial tree and stomach for a variety of reasons. A metallic stent would seem the logical choice after fistula formation, but it can be problematic, Dr. Li and colleagues pointed out. “Most often the clinician faces a situation in which the esophageal stent should have a larger diameter on the gastric side, making stenting the alimentary side of the fistula insufficient,” they said. The risk of stent migration is high, and the bifurcated structure of the trachea and main bronchi can cause leakage and stent displacement.
The researchers noted that Y-shaped self-expanding stents have been used for sealing airway fistulas, but they don’t always fully seal large GTFs and GBFs. Their primary objective in studying the combined-type Y-shaped covered metallic stent was to determine the safety and feasibility of the technique; the secondary aim was to evaluate long-term patency and complication rates.
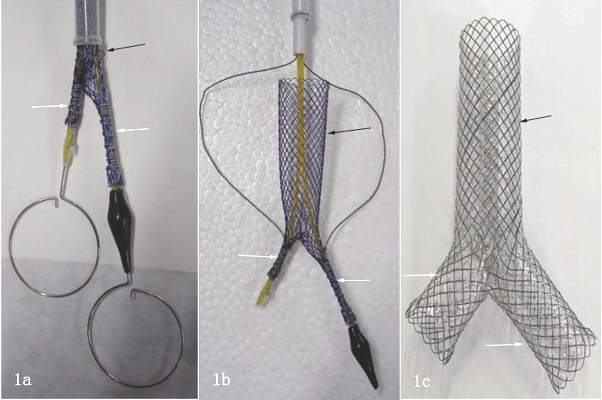
They designed a Y-shaped stent delivery system (Micro-Tech) and used a combined bundle-and-push to insert the main body of the stent. In all, they inserted 20 Y-shaped stents in the 10 patients, although two stents did not fully expand and were dilated with a balloon. The researchers reported resolution of coughing during eating, toleration of liquid or semiliquid diet, and no complications after insertion.
Dr. Li and colleagues also developed strategies to avoid complications of Y-shaped stents, which have been known to retain secretions because they hinder cilia function. “To avoid this, we provided sputum suction and administered continuous high-concentration oxygen during the procedure,” they noted. Also, speed and agility in placement are important. “The operation should be performed as rapidly and gently as possible to avoid irritation to the airway,” Dr. Li and colleagues wrote. The postoperative course involved IV expectorants and antiasthma agents and aerosol inhalation of terbutaline. Surveillance bronchoscopes and debridement of granulation tissue helped avoid stent obstruction.
Nonetheless, the researches acknowledged limitations of the retrospective study, namely its small sample size and lack of a control group.
Dr. Li and colleagues had no financial relationships to disclose.
The Zhengzhou University investigators provide an opportunity to “think outside the box” when managing complex airway fistulas, Waël C. Hanna, MDCM, of McMaster University and St. Joseph’s Healthcare in Hamilton, Ontario, said in his invited commentary (J Thorac Cardiovasc Surg. 2016;152:564).

|
Dr. Waël Hanna |
Dr. Hanna credited a couple of innovations in their technique to overcome the challenge of Y stents that “remain notoriously difficult to position”: eliminating rigid bronchoscopy and using angiography-guided oral delivery; and developing the hybrid deployment mechanism.
Dr. Hanna also noted two “important nuances” of the technique: The stents are custom-made based on the length and location of the fistula; and the routine placement of two stents, with a limb of the smaller Y stent projecting through a limb of the larger Y stent to seal the entire airway. “This Y-en-Y technique using perfectly fitted stents is likely what caused the excellent outcomes that are reported in this series,” Dr. Hanna said.
But their approach may not be a practical solution to complex airway fistulas soon, he said. “Most of us who see the occasional case are unlikely to be able to commission custom-made Y stents,” he said. What’s more, the deployment mechanism is complicated, and the effect on patient quality of life is unclear.
Dr. Hanna had no financial relationships to disclose.
The Zhengzhou University investigators provide an opportunity to “think outside the box” when managing complex airway fistulas, Waël C. Hanna, MDCM, of McMaster University and St. Joseph’s Healthcare in Hamilton, Ontario, said in his invited commentary (J Thorac Cardiovasc Surg. 2016;152:564).

|
Dr. Waël Hanna |
Dr. Hanna credited a couple of innovations in their technique to overcome the challenge of Y stents that “remain notoriously difficult to position”: eliminating rigid bronchoscopy and using angiography-guided oral delivery; and developing the hybrid deployment mechanism.
Dr. Hanna also noted two “important nuances” of the technique: The stents are custom-made based on the length and location of the fistula; and the routine placement of two stents, with a limb of the smaller Y stent projecting through a limb of the larger Y stent to seal the entire airway. “This Y-en-Y technique using perfectly fitted stents is likely what caused the excellent outcomes that are reported in this series,” Dr. Hanna said.
But their approach may not be a practical solution to complex airway fistulas soon, he said. “Most of us who see the occasional case are unlikely to be able to commission custom-made Y stents,” he said. What’s more, the deployment mechanism is complicated, and the effect on patient quality of life is unclear.
Dr. Hanna had no financial relationships to disclose.
The Zhengzhou University investigators provide an opportunity to “think outside the box” when managing complex airway fistulas, Waël C. Hanna, MDCM, of McMaster University and St. Joseph’s Healthcare in Hamilton, Ontario, said in his invited commentary (J Thorac Cardiovasc Surg. 2016;152:564).

|
Dr. Waël Hanna |
Dr. Hanna credited a couple of innovations in their technique to overcome the challenge of Y stents that “remain notoriously difficult to position”: eliminating rigid bronchoscopy and using angiography-guided oral delivery; and developing the hybrid deployment mechanism.
Dr. Hanna also noted two “important nuances” of the technique: The stents are custom-made based on the length and location of the fistula; and the routine placement of two stents, with a limb of the smaller Y stent projecting through a limb of the larger Y stent to seal the entire airway. “This Y-en-Y technique using perfectly fitted stents is likely what caused the excellent outcomes that are reported in this series,” Dr. Hanna said.
But their approach may not be a practical solution to complex airway fistulas soon, he said. “Most of us who see the occasional case are unlikely to be able to commission custom-made Y stents,” he said. What’s more, the deployment mechanism is complicated, and the effect on patient quality of life is unclear.
Dr. Hanna had no financial relationships to disclose.
Airway fistula is a rare but life-threatening complication of esophageal surgery, but an innovative technique using two custom-made, Y-shaped metallic stents can preserve airway patency, researchers at Zhengzhou University in China reported in the August issue of the Journal of Thoracic and Cardiovascular Surgery (J Thorac Cardiovasc Surg. 2016;152:557-63).
The study involved 10 patients who received Y-shaped stents to treat gastrotracheal or gastrobronchial fistulas (GTFs and GBFs, respectively) after esophageal surgery from 2010 through 2014. “Our patients tolerated the stents well and had good palliation of their symptoms,” wrote Teng-Fei Li, MD, and colleagues.
Six patients died within 8 months for unrelated reasons – either tumors (four patients), or hemoptysis or pulmonary infection (one each). In one patient, the carinal fistula enlarged 4 months after stenting, but the researchers successfully placed an additional small Y-shaped stent. At the publication of the paper, this patient and three others had survived, Dr. Li and colleagues said.
After esophagectomy, fistulas can form between the tracheobronchial tree and stomach for a variety of reasons. A metallic stent would seem the logical choice after fistula formation, but it can be problematic, Dr. Li and colleagues pointed out. “Most often the clinician faces a situation in which the esophageal stent should have a larger diameter on the gastric side, making stenting the alimentary side of the fistula insufficient,” they said. The risk of stent migration is high, and the bifurcated structure of the trachea and main bronchi can cause leakage and stent displacement.
The researchers noted that Y-shaped self-expanding stents have been used for sealing airway fistulas, but they don’t always fully seal large GTFs and GBFs. Their primary objective in studying the combined-type Y-shaped covered metallic stent was to determine the safety and feasibility of the technique; the secondary aim was to evaluate long-term patency and complication rates.
They designed a Y-shaped stent delivery system (Micro-Tech) and used a combined bundle-and-push to insert the main body of the stent. In all, they inserted 20 Y-shaped stents in the 10 patients, although two stents did not fully expand and were dilated with a balloon. The researchers reported resolution of coughing during eating, toleration of liquid or semiliquid diet, and no complications after insertion.
Dr. Li and colleagues also developed strategies to avoid complications of Y-shaped stents, which have been known to retain secretions because they hinder cilia function. “To avoid this, we provided sputum suction and administered continuous high-concentration oxygen during the procedure,” they noted. Also, speed and agility in placement are important. “The operation should be performed as rapidly and gently as possible to avoid irritation to the airway,” Dr. Li and colleagues wrote. The postoperative course involved IV expectorants and antiasthma agents and aerosol inhalation of terbutaline. Surveillance bronchoscopes and debridement of granulation tissue helped avoid stent obstruction.
Nonetheless, the researches acknowledged limitations of the retrospective study, namely its small sample size and lack of a control group.
Dr. Li and colleagues had no financial relationships to disclose.
Airway fistula is a rare but life-threatening complication of esophageal surgery, but an innovative technique using two custom-made, Y-shaped metallic stents can preserve airway patency, researchers at Zhengzhou University in China reported in the August issue of the Journal of Thoracic and Cardiovascular Surgery (J Thorac Cardiovasc Surg. 2016;152:557-63).
The study involved 10 patients who received Y-shaped stents to treat gastrotracheal or gastrobronchial fistulas (GTFs and GBFs, respectively) after esophageal surgery from 2010 through 2014. “Our patients tolerated the stents well and had good palliation of their symptoms,” wrote Teng-Fei Li, MD, and colleagues.
Six patients died within 8 months for unrelated reasons – either tumors (four patients), or hemoptysis or pulmonary infection (one each). In one patient, the carinal fistula enlarged 4 months after stenting, but the researchers successfully placed an additional small Y-shaped stent. At the publication of the paper, this patient and three others had survived, Dr. Li and colleagues said.
After esophagectomy, fistulas can form between the tracheobronchial tree and stomach for a variety of reasons. A metallic stent would seem the logical choice after fistula formation, but it can be problematic, Dr. Li and colleagues pointed out. “Most often the clinician faces a situation in which the esophageal stent should have a larger diameter on the gastric side, making stenting the alimentary side of the fistula insufficient,” they said. The risk of stent migration is high, and the bifurcated structure of the trachea and main bronchi can cause leakage and stent displacement.
The researchers noted that Y-shaped self-expanding stents have been used for sealing airway fistulas, but they don’t always fully seal large GTFs and GBFs. Their primary objective in studying the combined-type Y-shaped covered metallic stent was to determine the safety and feasibility of the technique; the secondary aim was to evaluate long-term patency and complication rates.
They designed a Y-shaped stent delivery system (Micro-Tech) and used a combined bundle-and-push to insert the main body of the stent. In all, they inserted 20 Y-shaped stents in the 10 patients, although two stents did not fully expand and were dilated with a balloon. The researchers reported resolution of coughing during eating, toleration of liquid or semiliquid diet, and no complications after insertion.
Dr. Li and colleagues also developed strategies to avoid complications of Y-shaped stents, which have been known to retain secretions because they hinder cilia function. “To avoid this, we provided sputum suction and administered continuous high-concentration oxygen during the procedure,” they noted. Also, speed and agility in placement are important. “The operation should be performed as rapidly and gently as possible to avoid irritation to the airway,” Dr. Li and colleagues wrote. The postoperative course involved IV expectorants and antiasthma agents and aerosol inhalation of terbutaline. Surveillance bronchoscopes and debridement of granulation tissue helped avoid stent obstruction.
Nonetheless, the researches acknowledged limitations of the retrospective study, namely its small sample size and lack of a control group.
Dr. Li and colleagues had no financial relationships to disclose.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: A combined type Y-shaped self-expandable coated metallic stent is a new approach for treatment of airway fistulas.
Major finding: Ten patients received the stents; all of them reported improved quality of life. Six died within 8 months because of unrelated factors.
Data source: Single-institution retrospective review of 10 patients with gastrotracheal or gastrobronchial fistulas who received the stent to reopen the airway.
Disclosures: Dr. Li and coauthors had no financial relationships to disclose. The study received support from the National High-Tech R&D Program of China.