User login
Behaviors during seizures can mimic psychiatric disorders, and patients with epilepsy have higher-than-normal rates of many types of psychiatric illness. That’s why it is important for psychiatrists to be familiar with epilepsy and electroencephalography (EEG)—the key diagnostic tool for epileptic disorders.
As a neurologist who specializes in epilepsy treatment, I offer five case studies that highlight basic concepts about epilepsy and EEGs. My goal is to help psychiatrists answer common clinical questions such as:
- If a patient with bipolar illness has an abnormal EEG, should this guide the treatment choice?
- In a patient with episodes of fear, tachycardia, and other autonomic symptoms, how does one differentiate between panic attacks, complex partial seizures, and psychogenic nonepileptic seizures?
- When is EEG indicated in a patient with attention-deficit/hyperactivity disorder (ADHD)?
- Can complex partial status epilepticus present as a psychiatric disorder?
- In patients with epilepsy, why is it important to categorize psychiatric symptoms as ictal (occurring at the time of seizure), interictal (between seizures), or postictal (following seizures)?
How EEG is used today
EEG is used mainly to evaluate epilepsy and diffuse brain dysfunction (e.g., coma and confusional states). Modern brain imaging, including magnetic resonance imaging (MRI) and computerized tomography (CT), has replaced EEG for evaluating structural brain abnormalities.
Two basic EEG findings with which psychiatrists should be familiar are slowing and epileptiform activity:
Slowing is a nonspecific finding that indicates dysfunction of the underlying white matter, with or without gray matter involvement. Focal slowing indicates a focal area of cortical dysfunction usually caused by a focal structural lesion (tumor, stroke, trauma, etc.), although a lesion is not always found. Brain imaging, usually MRI, is indicated.
Epileptiform activity, which is seen as spikes or sharp waves, indicates potential for epileptic seizures (Box). EEG technologists may use activation procedures such as hyperventilation and photic stimulation to enhance the ability of EEG to detect epileptiform activity. Special electrodes (e.g., anterior temporal electrodes) may be used to improve recordings taken from the temporal lobe. In selected inpatients, epilepsy centers may use sphenoidal electrodes—wires inserted under the skin of the cheek to record temporal lobe activity.
Video/EEG monitoring has been used since the 1960s and is the gold standard in evaluating patients with seizures or episodes that resemble seizures. The technique involves simultaneously recording brain activity on an EEG and behavior on tape or digital video. Usually patients are admitted to a specialized hospital unit, medications are reduced or discontinued, and the seizures or other behaviors are recorded. Neurologists with special training in EEG and epilepsy evaluate the EEG for changes before, during, and after the behavioral event. Clinical characteristics of seizures and nonepileptic events detected on the video also help with the evaluation.
Video/EEG is most helpful in:
- determining whether the events are epileptic or nonepileptic
- determining—if epileptic—the precise seizure type for treatment decisions
- localizing the site of seizure onset in patients with medication-resistant epilepsy who may be candidates for epilepsy surgery
Normal variants occur frequently on EEG and may be misinterpreted because they resemble epileptiform activity. They include:
- benign epileptiform transients of sleep
- mu rhythm
- rhythmic midtemporal variant
- subclinical rhythmic epileptiform discharge in adults.
Experienced electroencephalographers can readily identify these normal variants, but some neurologists may misidentify or misinterpret these EEG findings, potentially leading to unnecessary treatment with antiepileptic drugs.
Hundreds of medications can alter an EEG, usually by increasing either slowing or beta activity. The most common change is excessive beta activity, which is seen in most patients taking benzodiazepines or barbiturates. Enhanced beta activity is an appropriate response of a normal brain to certain medications and does not indicate underlying brain pathology.
If a patient with psychiatric illness has seizure-like episodes, an abnormal EEG may help in diagnosis. A neurologist can help direct the patient evaluation. Whether or not interictal EEG abnormalities are present, video/EEG monitoring can often make the diagnosis by capturing the events.
Case 1: Does this patient have epilepsy?
For Mr. A, age 27, lithium has stabilized his bipolar I disorder for 2 years without significant adverse effects. An EEG ordered for unknown reasons by his primary care physician shows large amounts of beta activity and a single sharp wave from the right temporal region. Should you add an antiepileptic drug to his regimen?
In this patient, lithium probably caused the large amounts of beta activity. A rule of thumb says that if an EEG shows increased beta activity, a medication is almost certainly the cause. If an EEG finds increased generalized slowing, medication effect is one of many possible causes.
The single sharp wave from the right temporal lobe raises the possibility of increased susceptibility to seizures but is not diagnostic of epilepsy. There is no indication to change the patient’s treatment regimen if he is well controlled without adverse effects from his current medications and there is no clear history of clinical seizures. In short, treat the patient, not the EEG.
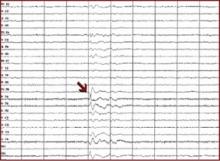
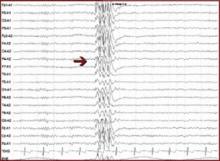
On an EEG, epileptiform activity is seen as spikes or sharp waves and indicates potential for epileptic seizures.
- Focal epileptiform activity is consistent with seizures of focal origin (e.g., simple partial, complex partial, or partial onset seizure with secondary generalization into tonic-clonic seizure).
- Generalized epileptiform activity is consistent with seizures of generalized onset (e.g., absence, myoclonic, or primary generalized tonic-clonic seizure).
Interictal spikes (between seizures) are consistent with, but not diagnostic of, seizures and epilepsy. An ictal discharge (rhythmic, persistent epileptiform activity) on an EEG accompanied by a clinical change in behavior is diagnostic of a seizure.
Focal epileptiform activity
Generalized epileptiform activity
Based on early studies, EEG results can show epileptiform activity in some normal brains.1 On the other hand, only about 50% of patients with epilepsy will show epileptiform activity on a single EEG. Thus, some EEG abnormalities in psychiatric patients may not be related to either epilepsy or the psychiatric disorder, and a normal EEG does not exclude the possibility of epileptic seizures.
Question the patient for a history of other factors that may predispose him or her to seizures, such as:
- family history of seizures
- previous traumatic brain injury
- structural brain abnormality.
In light of this EEG, brain MRI is indicated. In this case the patient could be counseled to avoid seizure triggers (e.g., sleep deprivation). Because a long list of medications can lower the seizure threshold, the clinician must weigh the risks and benefits of using any medication in patients with increased susceptibility for seizures.
Case 2: Seizures or panic attacks?
Mr. B, age 31, is referred by his primary care physician for “spells” that began several years ago and recently increased in frequency to three to four times per week. The episodes start with a feeling of fear, “butterflies” in his stomach, and hyperventilation. These feelings intensify within minutes; each episode lasts 10 to 30 minutes.
The patient is usually aware of his surroundings during the episodes but twice has lost consciousness for less than 1 minute. There is no evidence of incontinence or tongue biting. Four years ago, the patient was involved in a motor vehicle accident and lost consciousness for about 30 minutes.
An EEG shows intermittent slowing from the left temporal region, and brain MRI is normal. Treatment with a benzodiazepine shortens the attacks. Where do you proceed from here?
Mr. B presents a diagnostic dilemma. Characteristics of his episodes may be seen in panic attacks, temporal lobe complex partial seizures, and psychogenic nonepileptic seizures, which is the preferred term for pseudoseizures (Table).2
One option would be to see how he responds to an agent that would treat seizures but not panic attacks (e.g., carbamazepine) or one that would treat panic attacks but not seizures (e.g., a selective serotonin reuptake inhibitor). Because his episodes are frequent, however, a more appropriate option would be to admit him for video/EEG monitoring, which can distinguish among these possible diagnoses with almost 100% accuracy.
Case 3: Attention disorder or epilepsy?
Miss C, age 9, is referred for possible ADHD. Her teachers notice she has difficulty following lessons in class but is intelligent and usually motivated. Her grades have been dropping. Her family reports she has episodes during which she stares and is unable to answer questions for 3 to 5 seconds, but she exhibits no other seizure-like manifestations. A trial of methylphenidate has not improved the symptoms. What should you try next?
This patient presents with symptoms that could be consistent with absence seizures. EEG would be diagnostic if it showed generalized spike and wave. Absence seizures (sometimes called petit mal) usually present in childhood and are characterized by recurrent brief staring spells with no postictal confusion or other clinical manifestations.
Patients with childhood absence epilepsy are usually of normal intelligence and only rarely have other associated seizure types (e.g., myoclonus or tonic-clonic). Seizures of approximately 3 to 5 seconds may occur up to 100 times a day and thus may be mistaken for attention problems.
EEG shows characteristic generalized three-per-second spike and wave, which is often precipitated by hyperventilation or photic stimulation. Ethosuximide or valproate can completely control seizures in most cases.
Case 4: Emergency use of EEG
Ms. D, age 21, is brought to the emergency department by her mother with symptoms of confusion. Ms. D has a long history of temporal lobe complex partial seizures, and her mother thinks she may have missed some doses of her antiepileptic drugs (carbamazepine and valproate). Yesterday Ms. D had two complex partial seizures but returned to baseline. Today she had three complex partial seizures within 2 hours and has not returned to baseline.
When you interview Ms. D she is alert but only intermittently oriented to date and location. She makes a variety of paraphasic speech errors. She is talking about heaven and angels and several times asks if you are the devil. Evaluation by the emergency physician discloses no toxic, metabolic, or infectious cause for her symptoms. Other than mental status, her neurologic examination is normal and shows no evidence of motor seizure activity. What would you suggest next?
This patient presents with complex partial seizures occurring in sequence without return to normal between seizures, followed by a continuous state of altered consciousness. This cluster of symptoms and signs is consistent with complex partial status epilepticus.
Emergency EEG is diagnostic. If the EEG is positive for status epilepticus, recommended treatment is IV benzodiazepines along with other IV antiepileptic drugs.
Complex partial status epilepticus can have a variety of triggers, including drug overdose, hyperthyroidism, brain tumor, or carcinomatous meningitis.3 In this case, the most likely trigger is medication noncompliance.
Complex partial or other forms of nonconvulsive status epilepticus occur in up to 37% of hospitalized patients with altered consciousness of uncertain etiology.3 EEG is required to confirm the diagnosis, but many hospitals do not have EEG technologists on call nights and weekends.
Table
THE FEARFUL PATIENT: PANIC ATTACK, SEIZURE DISORDER, OR PSYCHOGENIC?
| Panic attacks |
|
| Temporal lobe complex partial seizures |
|
| Psychogenic nonepileptic seizures |
|
In my experience, a patient who later was referred to me for seizure control was once admitted to a psychiatry ward for 4 days because of unidentified complex partial status epilepticus. When someone finally restarted her carbamazepine, she returned to normal in a few days. Six months after she became my patient, she presented with identical symptoms. An EEG within hours of symptom onset showed continuous EEG ictal activity from the left temporal lobe. When we administered IV lorazepam, her EEG normalized within minutes and her confusion and delusional symptoms resolved in 20 minutes.
Case 5: Seizure clusters followed by agitation
Mr. E, 32, has had complex partial and tonic-clonic seizures since age 14. He presents with chronic depressive symptoms and independent episodes of agitated behavior with psychotic features lasting hours after seizure clusters. His seizures have continued despite trials of different antiepileptic drugs, and he currently is receiving phenytoin and valproate. He is referred to you to diagnose and treat the psychiatric symptoms.
He scores a 28 on the Beck Depression Inventory, which indicates moderate depression,4 but he is not suicidal. He reports that although his depression symptoms are constant, his psychotic features occur only after a series of closely-spaced seizures. How do you approach this problem?
Based on the history, this patient has both mild interictal depression and postictal psychosis. In patients with epilepsy, psychiatric symptoms are categorized as:
- ictal (occur only during a seizure)
- interictal (may wax and wane but are present chronically, usually with no relation to seizure occurrence)
- or postictal (appear within 7 days after a lucid interval following a seizure or—more often—a series of seizures).5
Interictal psychiatric disorders include depression, bipolar disorder, and psychotic disorders. If the psychiatric disorder is truly interictal and has no clear relation to seizure occurrence, it should be treated like any other psychiatric illness with appropriate medications. One should not automatically add another antiepileptic drug (AED), because AEDs as a class have more adverse effects and more drug interactions than commonly used antidepressants.
Begin by examining the AEDs the patient is receiving. For example, phenobarbital and, to a lesser extent, phenytoin are associated with depression and should be used in patients with depression only when other AEDs have failed.
Ictal and postictal psychiatric symptoms should be treated acutely. Postictal symptoms may include psychosis, depression, mania, or anxiety. A short course of benzodiazepines is often helpful; the use of neuroleptics is dictated by the intensity and quality of the postictal symptoms.
Ictal depression-like symptoms can be seen with temporal lobe complex partial seizures. Many patients with these seizures have simple partial seizures (auras) that manifest as brief (usually less than 1 minute) intense feelings of fear or impending doom, or of “the life drained out” of them. These symptoms may arise from seizures involving mesial temporal regions. They do not usually require treatment besides AEDs.
The idea that patients with temporal lobe epilepsy may have a particular personality type is controversial. Retrospective data first suggested that certain traits (e.g., altered sexual behavior, anger, emotionality and obsessionalism, hypergraphia, and hyper-religiosity) could be found consistently in patients with temporal lobe epilepsy.6 This personality inventory was sometimes used to diagnose epilepsy. Subsequent studies have not validated the original data, although the cluster of personality traits can certainly occur in some patients.7-9
Related resources
- Epilepsy Foundation. www.epilepsyfoundation.org
- Engel J, Pedley TA (eds). Epilepsy: A comprehensive textbook. Philadelphia: Lippincott-Raven, 1998.
Drug brand names
- Carbamazepine • Tegretol
- Ethosuximide • Zarontin
- Lorazepam • Ativan
- Phenytoin • Dilantin
- Valproate • Depakote
Disclosure
The author reports that he receives research/grant support from, is a consultant to, and is on the speakers’ bureau of GlaxoSmithKline, UCBPharma, and Ortho-McNeil Pharmaceuticals; receives research/grant support from and is a consultant to Schwarz Pharma; is a consultant to Pfizer Inc., Elan Pharmaceuticals, and Shire Pharmaceuticals; and is on the speakers’ bureau of Abbott Laboratories, Cyberonics, and Shire Pharmaceuticals.
1. Zivin L, Ajmone-Marson C. Incidence and prognostic significance of epileptiform activity in the EEG of nonepileptic subjects. Brain 1969;91:751-78.
2. Arnold LM, Privitera MD. Psychopathology and trauma in epileptic and psychogenic seizures. Psychosomatics 1996;37(5):438-43.
3. Privitera M, Hoffman M, Moore JL, Jester D. EEG detection of nontonic-clonic status epilepticus in patients with altered consciousness. Epilepsy Res 1994;18(2):155-66.
4. Lambert MV, Robertson MM. Depression in epilepsy: etiology, phenomenology, and treatment. Epilepsia 1999;40(suppl 10):S21-47.
5. Logsdail SJ, Toone BK. Post-ictal psychoses: a clinical and phenomenological description. Br J Psychiatry 1988;152:246-52.
6. Bear DM, Fedio P. Quantitative analysis of interictal behavior in temporal lobe epilepsy. Arch Neurol 1977;34:454-67.
7. Devinsky O, Najjar S. Evidence against the existence of a temporal lobe epilepsy personality. Neurology 1999;53(5, suppl 2):S13-25.
8. Blumer D. Evidence supporting the temporal lobe epilepsy personality. Neurology 1999;53 (5, suppl 2):S9-12.
9. Mungas D. Interictal behavior abnormality in temporal lobe epilepsy. A specific syndrome or nonspecific psychopathology? Arch Gen Psychiatry 1982;39(1):108-11.
Behaviors during seizures can mimic psychiatric disorders, and patients with epilepsy have higher-than-normal rates of many types of psychiatric illness. That’s why it is important for psychiatrists to be familiar with epilepsy and electroencephalography (EEG)—the key diagnostic tool for epileptic disorders.
As a neurologist who specializes in epilepsy treatment, I offer five case studies that highlight basic concepts about epilepsy and EEGs. My goal is to help psychiatrists answer common clinical questions such as:
- If a patient with bipolar illness has an abnormal EEG, should this guide the treatment choice?
- In a patient with episodes of fear, tachycardia, and other autonomic symptoms, how does one differentiate between panic attacks, complex partial seizures, and psychogenic nonepileptic seizures?
- When is EEG indicated in a patient with attention-deficit/hyperactivity disorder (ADHD)?
- Can complex partial status epilepticus present as a psychiatric disorder?
- In patients with epilepsy, why is it important to categorize psychiatric symptoms as ictal (occurring at the time of seizure), interictal (between seizures), or postictal (following seizures)?
How EEG is used today
EEG is used mainly to evaluate epilepsy and diffuse brain dysfunction (e.g., coma and confusional states). Modern brain imaging, including magnetic resonance imaging (MRI) and computerized tomography (CT), has replaced EEG for evaluating structural brain abnormalities.
Two basic EEG findings with which psychiatrists should be familiar are slowing and epileptiform activity:
Slowing is a nonspecific finding that indicates dysfunction of the underlying white matter, with or without gray matter involvement. Focal slowing indicates a focal area of cortical dysfunction usually caused by a focal structural lesion (tumor, stroke, trauma, etc.), although a lesion is not always found. Brain imaging, usually MRI, is indicated.
Epileptiform activity, which is seen as spikes or sharp waves, indicates potential for epileptic seizures (Box). EEG technologists may use activation procedures such as hyperventilation and photic stimulation to enhance the ability of EEG to detect epileptiform activity. Special electrodes (e.g., anterior temporal electrodes) may be used to improve recordings taken from the temporal lobe. In selected inpatients, epilepsy centers may use sphenoidal electrodes—wires inserted under the skin of the cheek to record temporal lobe activity.
Video/EEG monitoring has been used since the 1960s and is the gold standard in evaluating patients with seizures or episodes that resemble seizures. The technique involves simultaneously recording brain activity on an EEG and behavior on tape or digital video. Usually patients are admitted to a specialized hospital unit, medications are reduced or discontinued, and the seizures or other behaviors are recorded. Neurologists with special training in EEG and epilepsy evaluate the EEG for changes before, during, and after the behavioral event. Clinical characteristics of seizures and nonepileptic events detected on the video also help with the evaluation.
Video/EEG is most helpful in:
- determining whether the events are epileptic or nonepileptic
- determining—if epileptic—the precise seizure type for treatment decisions
- localizing the site of seizure onset in patients with medication-resistant epilepsy who may be candidates for epilepsy surgery
Normal variants occur frequently on EEG and may be misinterpreted because they resemble epileptiform activity. They include:
- benign epileptiform transients of sleep
- mu rhythm
- rhythmic midtemporal variant
- subclinical rhythmic epileptiform discharge in adults.
Experienced electroencephalographers can readily identify these normal variants, but some neurologists may misidentify or misinterpret these EEG findings, potentially leading to unnecessary treatment with antiepileptic drugs.
Hundreds of medications can alter an EEG, usually by increasing either slowing or beta activity. The most common change is excessive beta activity, which is seen in most patients taking benzodiazepines or barbiturates. Enhanced beta activity is an appropriate response of a normal brain to certain medications and does not indicate underlying brain pathology.
If a patient with psychiatric illness has seizure-like episodes, an abnormal EEG may help in diagnosis. A neurologist can help direct the patient evaluation. Whether or not interictal EEG abnormalities are present, video/EEG monitoring can often make the diagnosis by capturing the events.
Case 1: Does this patient have epilepsy?
For Mr. A, age 27, lithium has stabilized his bipolar I disorder for 2 years without significant adverse effects. An EEG ordered for unknown reasons by his primary care physician shows large amounts of beta activity and a single sharp wave from the right temporal region. Should you add an antiepileptic drug to his regimen?
In this patient, lithium probably caused the large amounts of beta activity. A rule of thumb says that if an EEG shows increased beta activity, a medication is almost certainly the cause. If an EEG finds increased generalized slowing, medication effect is one of many possible causes.
The single sharp wave from the right temporal lobe raises the possibility of increased susceptibility to seizures but is not diagnostic of epilepsy. There is no indication to change the patient’s treatment regimen if he is well controlled without adverse effects from his current medications and there is no clear history of clinical seizures. In short, treat the patient, not the EEG.
On an EEG, epileptiform activity is seen as spikes or sharp waves and indicates potential for epileptic seizures.
- Focal epileptiform activity is consistent with seizures of focal origin (e.g., simple partial, complex partial, or partial onset seizure with secondary generalization into tonic-clonic seizure).
- Generalized epileptiform activity is consistent with seizures of generalized onset (e.g., absence, myoclonic, or primary generalized tonic-clonic seizure).
Interictal spikes (between seizures) are consistent with, but not diagnostic of, seizures and epilepsy. An ictal discharge (rhythmic, persistent epileptiform activity) on an EEG accompanied by a clinical change in behavior is diagnostic of a seizure.
Focal epileptiform activity
Generalized epileptiform activity
Based on early studies, EEG results can show epileptiform activity in some normal brains.1 On the other hand, only about 50% of patients with epilepsy will show epileptiform activity on a single EEG. Thus, some EEG abnormalities in psychiatric patients may not be related to either epilepsy or the psychiatric disorder, and a normal EEG does not exclude the possibility of epileptic seizures.
Question the patient for a history of other factors that may predispose him or her to seizures, such as:
- family history of seizures
- previous traumatic brain injury
- structural brain abnormality.
In light of this EEG, brain MRI is indicated. In this case the patient could be counseled to avoid seizure triggers (e.g., sleep deprivation). Because a long list of medications can lower the seizure threshold, the clinician must weigh the risks and benefits of using any medication in patients with increased susceptibility for seizures.
Case 2: Seizures or panic attacks?
Mr. B, age 31, is referred by his primary care physician for “spells” that began several years ago and recently increased in frequency to three to four times per week. The episodes start with a feeling of fear, “butterflies” in his stomach, and hyperventilation. These feelings intensify within minutes; each episode lasts 10 to 30 minutes.
The patient is usually aware of his surroundings during the episodes but twice has lost consciousness for less than 1 minute. There is no evidence of incontinence or tongue biting. Four years ago, the patient was involved in a motor vehicle accident and lost consciousness for about 30 minutes.
An EEG shows intermittent slowing from the left temporal region, and brain MRI is normal. Treatment with a benzodiazepine shortens the attacks. Where do you proceed from here?
Mr. B presents a diagnostic dilemma. Characteristics of his episodes may be seen in panic attacks, temporal lobe complex partial seizures, and psychogenic nonepileptic seizures, which is the preferred term for pseudoseizures (Table).2
One option would be to see how he responds to an agent that would treat seizures but not panic attacks (e.g., carbamazepine) or one that would treat panic attacks but not seizures (e.g., a selective serotonin reuptake inhibitor). Because his episodes are frequent, however, a more appropriate option would be to admit him for video/EEG monitoring, which can distinguish among these possible diagnoses with almost 100% accuracy.
Case 3: Attention disorder or epilepsy?
Miss C, age 9, is referred for possible ADHD. Her teachers notice she has difficulty following lessons in class but is intelligent and usually motivated. Her grades have been dropping. Her family reports she has episodes during which she stares and is unable to answer questions for 3 to 5 seconds, but she exhibits no other seizure-like manifestations. A trial of methylphenidate has not improved the symptoms. What should you try next?
This patient presents with symptoms that could be consistent with absence seizures. EEG would be diagnostic if it showed generalized spike and wave. Absence seizures (sometimes called petit mal) usually present in childhood and are characterized by recurrent brief staring spells with no postictal confusion or other clinical manifestations.
Patients with childhood absence epilepsy are usually of normal intelligence and only rarely have other associated seizure types (e.g., myoclonus or tonic-clonic). Seizures of approximately 3 to 5 seconds may occur up to 100 times a day and thus may be mistaken for attention problems.
EEG shows characteristic generalized three-per-second spike and wave, which is often precipitated by hyperventilation or photic stimulation. Ethosuximide or valproate can completely control seizures in most cases.
Case 4: Emergency use of EEG
Ms. D, age 21, is brought to the emergency department by her mother with symptoms of confusion. Ms. D has a long history of temporal lobe complex partial seizures, and her mother thinks she may have missed some doses of her antiepileptic drugs (carbamazepine and valproate). Yesterday Ms. D had two complex partial seizures but returned to baseline. Today she had three complex partial seizures within 2 hours and has not returned to baseline.
When you interview Ms. D she is alert but only intermittently oriented to date and location. She makes a variety of paraphasic speech errors. She is talking about heaven and angels and several times asks if you are the devil. Evaluation by the emergency physician discloses no toxic, metabolic, or infectious cause for her symptoms. Other than mental status, her neurologic examination is normal and shows no evidence of motor seizure activity. What would you suggest next?
This patient presents with complex partial seizures occurring in sequence without return to normal between seizures, followed by a continuous state of altered consciousness. This cluster of symptoms and signs is consistent with complex partial status epilepticus.
Emergency EEG is diagnostic. If the EEG is positive for status epilepticus, recommended treatment is IV benzodiazepines along with other IV antiepileptic drugs.
Complex partial status epilepticus can have a variety of triggers, including drug overdose, hyperthyroidism, brain tumor, or carcinomatous meningitis.3 In this case, the most likely trigger is medication noncompliance.
Complex partial or other forms of nonconvulsive status epilepticus occur in up to 37% of hospitalized patients with altered consciousness of uncertain etiology.3 EEG is required to confirm the diagnosis, but many hospitals do not have EEG technologists on call nights and weekends.
Table
THE FEARFUL PATIENT: PANIC ATTACK, SEIZURE DISORDER, OR PSYCHOGENIC?
| Panic attacks |
|
| Temporal lobe complex partial seizures |
|
| Psychogenic nonepileptic seizures |
|
In my experience, a patient who later was referred to me for seizure control was once admitted to a psychiatry ward for 4 days because of unidentified complex partial status epilepticus. When someone finally restarted her carbamazepine, she returned to normal in a few days. Six months after she became my patient, she presented with identical symptoms. An EEG within hours of symptom onset showed continuous EEG ictal activity from the left temporal lobe. When we administered IV lorazepam, her EEG normalized within minutes and her confusion and delusional symptoms resolved in 20 minutes.
Case 5: Seizure clusters followed by agitation
Mr. E, 32, has had complex partial and tonic-clonic seizures since age 14. He presents with chronic depressive symptoms and independent episodes of agitated behavior with psychotic features lasting hours after seizure clusters. His seizures have continued despite trials of different antiepileptic drugs, and he currently is receiving phenytoin and valproate. He is referred to you to diagnose and treat the psychiatric symptoms.
He scores a 28 on the Beck Depression Inventory, which indicates moderate depression,4 but he is not suicidal. He reports that although his depression symptoms are constant, his psychotic features occur only after a series of closely-spaced seizures. How do you approach this problem?
Based on the history, this patient has both mild interictal depression and postictal psychosis. In patients with epilepsy, psychiatric symptoms are categorized as:
- ictal (occur only during a seizure)
- interictal (may wax and wane but are present chronically, usually with no relation to seizure occurrence)
- or postictal (appear within 7 days after a lucid interval following a seizure or—more often—a series of seizures).5
Interictal psychiatric disorders include depression, bipolar disorder, and psychotic disorders. If the psychiatric disorder is truly interictal and has no clear relation to seizure occurrence, it should be treated like any other psychiatric illness with appropriate medications. One should not automatically add another antiepileptic drug (AED), because AEDs as a class have more adverse effects and more drug interactions than commonly used antidepressants.
Begin by examining the AEDs the patient is receiving. For example, phenobarbital and, to a lesser extent, phenytoin are associated with depression and should be used in patients with depression only when other AEDs have failed.
Ictal and postictal psychiatric symptoms should be treated acutely. Postictal symptoms may include psychosis, depression, mania, or anxiety. A short course of benzodiazepines is often helpful; the use of neuroleptics is dictated by the intensity and quality of the postictal symptoms.
Ictal depression-like symptoms can be seen with temporal lobe complex partial seizures. Many patients with these seizures have simple partial seizures (auras) that manifest as brief (usually less than 1 minute) intense feelings of fear or impending doom, or of “the life drained out” of them. These symptoms may arise from seizures involving mesial temporal regions. They do not usually require treatment besides AEDs.
The idea that patients with temporal lobe epilepsy may have a particular personality type is controversial. Retrospective data first suggested that certain traits (e.g., altered sexual behavior, anger, emotionality and obsessionalism, hypergraphia, and hyper-religiosity) could be found consistently in patients with temporal lobe epilepsy.6 This personality inventory was sometimes used to diagnose epilepsy. Subsequent studies have not validated the original data, although the cluster of personality traits can certainly occur in some patients.7-9
Related resources
- Epilepsy Foundation. www.epilepsyfoundation.org
- Engel J, Pedley TA (eds). Epilepsy: A comprehensive textbook. Philadelphia: Lippincott-Raven, 1998.
Drug brand names
- Carbamazepine • Tegretol
- Ethosuximide • Zarontin
- Lorazepam • Ativan
- Phenytoin • Dilantin
- Valproate • Depakote
Disclosure
The author reports that he receives research/grant support from, is a consultant to, and is on the speakers’ bureau of GlaxoSmithKline, UCBPharma, and Ortho-McNeil Pharmaceuticals; receives research/grant support from and is a consultant to Schwarz Pharma; is a consultant to Pfizer Inc., Elan Pharmaceuticals, and Shire Pharmaceuticals; and is on the speakers’ bureau of Abbott Laboratories, Cyberonics, and Shire Pharmaceuticals.
Behaviors during seizures can mimic psychiatric disorders, and patients with epilepsy have higher-than-normal rates of many types of psychiatric illness. That’s why it is important for psychiatrists to be familiar with epilepsy and electroencephalography (EEG)—the key diagnostic tool for epileptic disorders.
As a neurologist who specializes in epilepsy treatment, I offer five case studies that highlight basic concepts about epilepsy and EEGs. My goal is to help psychiatrists answer common clinical questions such as:
- If a patient with bipolar illness has an abnormal EEG, should this guide the treatment choice?
- In a patient with episodes of fear, tachycardia, and other autonomic symptoms, how does one differentiate between panic attacks, complex partial seizures, and psychogenic nonepileptic seizures?
- When is EEG indicated in a patient with attention-deficit/hyperactivity disorder (ADHD)?
- Can complex partial status epilepticus present as a psychiatric disorder?
- In patients with epilepsy, why is it important to categorize psychiatric symptoms as ictal (occurring at the time of seizure), interictal (between seizures), or postictal (following seizures)?
How EEG is used today
EEG is used mainly to evaluate epilepsy and diffuse brain dysfunction (e.g., coma and confusional states). Modern brain imaging, including magnetic resonance imaging (MRI) and computerized tomography (CT), has replaced EEG for evaluating structural brain abnormalities.
Two basic EEG findings with which psychiatrists should be familiar are slowing and epileptiform activity:
Slowing is a nonspecific finding that indicates dysfunction of the underlying white matter, with or without gray matter involvement. Focal slowing indicates a focal area of cortical dysfunction usually caused by a focal structural lesion (tumor, stroke, trauma, etc.), although a lesion is not always found. Brain imaging, usually MRI, is indicated.
Epileptiform activity, which is seen as spikes or sharp waves, indicates potential for epileptic seizures (Box). EEG technologists may use activation procedures such as hyperventilation and photic stimulation to enhance the ability of EEG to detect epileptiform activity. Special electrodes (e.g., anterior temporal electrodes) may be used to improve recordings taken from the temporal lobe. In selected inpatients, epilepsy centers may use sphenoidal electrodes—wires inserted under the skin of the cheek to record temporal lobe activity.
Video/EEG monitoring has been used since the 1960s and is the gold standard in evaluating patients with seizures or episodes that resemble seizures. The technique involves simultaneously recording brain activity on an EEG and behavior on tape or digital video. Usually patients are admitted to a specialized hospital unit, medications are reduced or discontinued, and the seizures or other behaviors are recorded. Neurologists with special training in EEG and epilepsy evaluate the EEG for changes before, during, and after the behavioral event. Clinical characteristics of seizures and nonepileptic events detected on the video also help with the evaluation.
Video/EEG is most helpful in:
- determining whether the events are epileptic or nonepileptic
- determining—if epileptic—the precise seizure type for treatment decisions
- localizing the site of seizure onset in patients with medication-resistant epilepsy who may be candidates for epilepsy surgery
Normal variants occur frequently on EEG and may be misinterpreted because they resemble epileptiform activity. They include:
- benign epileptiform transients of sleep
- mu rhythm
- rhythmic midtemporal variant
- subclinical rhythmic epileptiform discharge in adults.
Experienced electroencephalographers can readily identify these normal variants, but some neurologists may misidentify or misinterpret these EEG findings, potentially leading to unnecessary treatment with antiepileptic drugs.
Hundreds of medications can alter an EEG, usually by increasing either slowing or beta activity. The most common change is excessive beta activity, which is seen in most patients taking benzodiazepines or barbiturates. Enhanced beta activity is an appropriate response of a normal brain to certain medications and does not indicate underlying brain pathology.
If a patient with psychiatric illness has seizure-like episodes, an abnormal EEG may help in diagnosis. A neurologist can help direct the patient evaluation. Whether or not interictal EEG abnormalities are present, video/EEG monitoring can often make the diagnosis by capturing the events.
Case 1: Does this patient have epilepsy?
For Mr. A, age 27, lithium has stabilized his bipolar I disorder for 2 years without significant adverse effects. An EEG ordered for unknown reasons by his primary care physician shows large amounts of beta activity and a single sharp wave from the right temporal region. Should you add an antiepileptic drug to his regimen?
In this patient, lithium probably caused the large amounts of beta activity. A rule of thumb says that if an EEG shows increased beta activity, a medication is almost certainly the cause. If an EEG finds increased generalized slowing, medication effect is one of many possible causes.
The single sharp wave from the right temporal lobe raises the possibility of increased susceptibility to seizures but is not diagnostic of epilepsy. There is no indication to change the patient’s treatment regimen if he is well controlled without adverse effects from his current medications and there is no clear history of clinical seizures. In short, treat the patient, not the EEG.
On an EEG, epileptiform activity is seen as spikes or sharp waves and indicates potential for epileptic seizures.
- Focal epileptiform activity is consistent with seizures of focal origin (e.g., simple partial, complex partial, or partial onset seizure with secondary generalization into tonic-clonic seizure).
- Generalized epileptiform activity is consistent with seizures of generalized onset (e.g., absence, myoclonic, or primary generalized tonic-clonic seizure).
Interictal spikes (between seizures) are consistent with, but not diagnostic of, seizures and epilepsy. An ictal discharge (rhythmic, persistent epileptiform activity) on an EEG accompanied by a clinical change in behavior is diagnostic of a seizure.
Focal epileptiform activity
Generalized epileptiform activity
Based on early studies, EEG results can show epileptiform activity in some normal brains.1 On the other hand, only about 50% of patients with epilepsy will show epileptiform activity on a single EEG. Thus, some EEG abnormalities in psychiatric patients may not be related to either epilepsy or the psychiatric disorder, and a normal EEG does not exclude the possibility of epileptic seizures.
Question the patient for a history of other factors that may predispose him or her to seizures, such as:
- family history of seizures
- previous traumatic brain injury
- structural brain abnormality.
In light of this EEG, brain MRI is indicated. In this case the patient could be counseled to avoid seizure triggers (e.g., sleep deprivation). Because a long list of medications can lower the seizure threshold, the clinician must weigh the risks and benefits of using any medication in patients with increased susceptibility for seizures.
Case 2: Seizures or panic attacks?
Mr. B, age 31, is referred by his primary care physician for “spells” that began several years ago and recently increased in frequency to three to four times per week. The episodes start with a feeling of fear, “butterflies” in his stomach, and hyperventilation. These feelings intensify within minutes; each episode lasts 10 to 30 minutes.
The patient is usually aware of his surroundings during the episodes but twice has lost consciousness for less than 1 minute. There is no evidence of incontinence or tongue biting. Four years ago, the patient was involved in a motor vehicle accident and lost consciousness for about 30 minutes.
An EEG shows intermittent slowing from the left temporal region, and brain MRI is normal. Treatment with a benzodiazepine shortens the attacks. Where do you proceed from here?
Mr. B presents a diagnostic dilemma. Characteristics of his episodes may be seen in panic attacks, temporal lobe complex partial seizures, and psychogenic nonepileptic seizures, which is the preferred term for pseudoseizures (Table).2
One option would be to see how he responds to an agent that would treat seizures but not panic attacks (e.g., carbamazepine) or one that would treat panic attacks but not seizures (e.g., a selective serotonin reuptake inhibitor). Because his episodes are frequent, however, a more appropriate option would be to admit him for video/EEG monitoring, which can distinguish among these possible diagnoses with almost 100% accuracy.
Case 3: Attention disorder or epilepsy?
Miss C, age 9, is referred for possible ADHD. Her teachers notice she has difficulty following lessons in class but is intelligent and usually motivated. Her grades have been dropping. Her family reports she has episodes during which she stares and is unable to answer questions for 3 to 5 seconds, but she exhibits no other seizure-like manifestations. A trial of methylphenidate has not improved the symptoms. What should you try next?
This patient presents with symptoms that could be consistent with absence seizures. EEG would be diagnostic if it showed generalized spike and wave. Absence seizures (sometimes called petit mal) usually present in childhood and are characterized by recurrent brief staring spells with no postictal confusion or other clinical manifestations.
Patients with childhood absence epilepsy are usually of normal intelligence and only rarely have other associated seizure types (e.g., myoclonus or tonic-clonic). Seizures of approximately 3 to 5 seconds may occur up to 100 times a day and thus may be mistaken for attention problems.
EEG shows characteristic generalized three-per-second spike and wave, which is often precipitated by hyperventilation or photic stimulation. Ethosuximide or valproate can completely control seizures in most cases.
Case 4: Emergency use of EEG
Ms. D, age 21, is brought to the emergency department by her mother with symptoms of confusion. Ms. D has a long history of temporal lobe complex partial seizures, and her mother thinks she may have missed some doses of her antiepileptic drugs (carbamazepine and valproate). Yesterday Ms. D had two complex partial seizures but returned to baseline. Today she had three complex partial seizures within 2 hours and has not returned to baseline.
When you interview Ms. D she is alert but only intermittently oriented to date and location. She makes a variety of paraphasic speech errors. She is talking about heaven and angels and several times asks if you are the devil. Evaluation by the emergency physician discloses no toxic, metabolic, or infectious cause for her symptoms. Other than mental status, her neurologic examination is normal and shows no evidence of motor seizure activity. What would you suggest next?
This patient presents with complex partial seizures occurring in sequence without return to normal between seizures, followed by a continuous state of altered consciousness. This cluster of symptoms and signs is consistent with complex partial status epilepticus.
Emergency EEG is diagnostic. If the EEG is positive for status epilepticus, recommended treatment is IV benzodiazepines along with other IV antiepileptic drugs.
Complex partial status epilepticus can have a variety of triggers, including drug overdose, hyperthyroidism, brain tumor, or carcinomatous meningitis.3 In this case, the most likely trigger is medication noncompliance.
Complex partial or other forms of nonconvulsive status epilepticus occur in up to 37% of hospitalized patients with altered consciousness of uncertain etiology.3 EEG is required to confirm the diagnosis, but many hospitals do not have EEG technologists on call nights and weekends.
Table
THE FEARFUL PATIENT: PANIC ATTACK, SEIZURE DISORDER, OR PSYCHOGENIC?
| Panic attacks |
|
| Temporal lobe complex partial seizures |
|
| Psychogenic nonepileptic seizures |
|
In my experience, a patient who later was referred to me for seizure control was once admitted to a psychiatry ward for 4 days because of unidentified complex partial status epilepticus. When someone finally restarted her carbamazepine, she returned to normal in a few days. Six months after she became my patient, she presented with identical symptoms. An EEG within hours of symptom onset showed continuous EEG ictal activity from the left temporal lobe. When we administered IV lorazepam, her EEG normalized within minutes and her confusion and delusional symptoms resolved in 20 minutes.
Case 5: Seizure clusters followed by agitation
Mr. E, 32, has had complex partial and tonic-clonic seizures since age 14. He presents with chronic depressive symptoms and independent episodes of agitated behavior with psychotic features lasting hours after seizure clusters. His seizures have continued despite trials of different antiepileptic drugs, and he currently is receiving phenytoin and valproate. He is referred to you to diagnose and treat the psychiatric symptoms.
He scores a 28 on the Beck Depression Inventory, which indicates moderate depression,4 but he is not suicidal. He reports that although his depression symptoms are constant, his psychotic features occur only after a series of closely-spaced seizures. How do you approach this problem?
Based on the history, this patient has both mild interictal depression and postictal psychosis. In patients with epilepsy, psychiatric symptoms are categorized as:
- ictal (occur only during a seizure)
- interictal (may wax and wane but are present chronically, usually with no relation to seizure occurrence)
- or postictal (appear within 7 days after a lucid interval following a seizure or—more often—a series of seizures).5
Interictal psychiatric disorders include depression, bipolar disorder, and psychotic disorders. If the psychiatric disorder is truly interictal and has no clear relation to seizure occurrence, it should be treated like any other psychiatric illness with appropriate medications. One should not automatically add another antiepileptic drug (AED), because AEDs as a class have more adverse effects and more drug interactions than commonly used antidepressants.
Begin by examining the AEDs the patient is receiving. For example, phenobarbital and, to a lesser extent, phenytoin are associated with depression and should be used in patients with depression only when other AEDs have failed.
Ictal and postictal psychiatric symptoms should be treated acutely. Postictal symptoms may include psychosis, depression, mania, or anxiety. A short course of benzodiazepines is often helpful; the use of neuroleptics is dictated by the intensity and quality of the postictal symptoms.
Ictal depression-like symptoms can be seen with temporal lobe complex partial seizures. Many patients with these seizures have simple partial seizures (auras) that manifest as brief (usually less than 1 minute) intense feelings of fear or impending doom, or of “the life drained out” of them. These symptoms may arise from seizures involving mesial temporal regions. They do not usually require treatment besides AEDs.
The idea that patients with temporal lobe epilepsy may have a particular personality type is controversial. Retrospective data first suggested that certain traits (e.g., altered sexual behavior, anger, emotionality and obsessionalism, hypergraphia, and hyper-religiosity) could be found consistently in patients with temporal lobe epilepsy.6 This personality inventory was sometimes used to diagnose epilepsy. Subsequent studies have not validated the original data, although the cluster of personality traits can certainly occur in some patients.7-9
Related resources
- Epilepsy Foundation. www.epilepsyfoundation.org
- Engel J, Pedley TA (eds). Epilepsy: A comprehensive textbook. Philadelphia: Lippincott-Raven, 1998.
Drug brand names
- Carbamazepine • Tegretol
- Ethosuximide • Zarontin
- Lorazepam • Ativan
- Phenytoin • Dilantin
- Valproate • Depakote
Disclosure
The author reports that he receives research/grant support from, is a consultant to, and is on the speakers’ bureau of GlaxoSmithKline, UCBPharma, and Ortho-McNeil Pharmaceuticals; receives research/grant support from and is a consultant to Schwarz Pharma; is a consultant to Pfizer Inc., Elan Pharmaceuticals, and Shire Pharmaceuticals; and is on the speakers’ bureau of Abbott Laboratories, Cyberonics, and Shire Pharmaceuticals.
1. Zivin L, Ajmone-Marson C. Incidence and prognostic significance of epileptiform activity in the EEG of nonepileptic subjects. Brain 1969;91:751-78.
2. Arnold LM, Privitera MD. Psychopathology and trauma in epileptic and psychogenic seizures. Psychosomatics 1996;37(5):438-43.
3. Privitera M, Hoffman M, Moore JL, Jester D. EEG detection of nontonic-clonic status epilepticus in patients with altered consciousness. Epilepsy Res 1994;18(2):155-66.
4. Lambert MV, Robertson MM. Depression in epilepsy: etiology, phenomenology, and treatment. Epilepsia 1999;40(suppl 10):S21-47.
5. Logsdail SJ, Toone BK. Post-ictal psychoses: a clinical and phenomenological description. Br J Psychiatry 1988;152:246-52.
6. Bear DM, Fedio P. Quantitative analysis of interictal behavior in temporal lobe epilepsy. Arch Neurol 1977;34:454-67.
7. Devinsky O, Najjar S. Evidence against the existence of a temporal lobe epilepsy personality. Neurology 1999;53(5, suppl 2):S13-25.
8. Blumer D. Evidence supporting the temporal lobe epilepsy personality. Neurology 1999;53 (5, suppl 2):S9-12.
9. Mungas D. Interictal behavior abnormality in temporal lobe epilepsy. A specific syndrome or nonspecific psychopathology? Arch Gen Psychiatry 1982;39(1):108-11.
1. Zivin L, Ajmone-Marson C. Incidence and prognostic significance of epileptiform activity in the EEG of nonepileptic subjects. Brain 1969;91:751-78.
2. Arnold LM, Privitera MD. Psychopathology and trauma in epileptic and psychogenic seizures. Psychosomatics 1996;37(5):438-43.
3. Privitera M, Hoffman M, Moore JL, Jester D. EEG detection of nontonic-clonic status epilepticus in patients with altered consciousness. Epilepsy Res 1994;18(2):155-66.
4. Lambert MV, Robertson MM. Depression in epilepsy: etiology, phenomenology, and treatment. Epilepsia 1999;40(suppl 10):S21-47.
5. Logsdail SJ, Toone BK. Post-ictal psychoses: a clinical and phenomenological description. Br J Psychiatry 1988;152:246-52.
6. Bear DM, Fedio P. Quantitative analysis of interictal behavior in temporal lobe epilepsy. Arch Neurol 1977;34:454-67.
7. Devinsky O, Najjar S. Evidence against the existence of a temporal lobe epilepsy personality. Neurology 1999;53(5, suppl 2):S13-25.
8. Blumer D. Evidence supporting the temporal lobe epilepsy personality. Neurology 1999;53 (5, suppl 2):S9-12.
9. Mungas D. Interictal behavior abnormality in temporal lobe epilepsy. A specific syndrome or nonspecific psychopathology? Arch Gen Psychiatry 1982;39(1):108-11.