User login
The US Food and Drug Administration (FDA) has granted new clearance for Verax Biomedical’s Platelet PGD® Test.
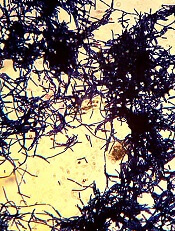
This qualitative immunoassay is designed to detect aerobic and anaerobic Gram-positive and Gram-negative bacteria in platelets.
The test is now cleared for use on single units of leukocyte-reduced or non-leukocyte-reduced whole blood-derived (WBD) platelets in plasma.
The Platelet PGD Test was previously cleared by the FDA as a safety measure to be used following testing with a growth-based, quality control (QC) test for platelet components that is cleared by the FDA.
For this indication, the Platelet PGD Test can be used within 24 hours of transfusion on:
- Leukocyte-reduced apheresis platelets suspended in plasma
- Leukocyte-reduced apheresis platelets suspended in platelet additive solution C and plasma
- Pre-storage pools of up to 6 leukocyte-reduced WBD platelets suspended in plasma.
When used as a safety measure, the Platelet PGD Test can extend the dating of apheresis platelets in plasma from 5 to 7 days.
The Platelet PGD Test also has FDA clearance as a QC test for use on pools of up to 6 units of leukocyte-reduced and non-leukocyte-reduced WBD platelets suspended in plasma that are pooled within 4 hours of transfusion.
The latest FDA clearance extends this use to individual units of WBD platelets in plasma.
“[The new clearance] has been requested by current users of PGD as well as being outlined as a need in pending FDA Draft Guidance to address the risk of bacterial contamination in platelets,” said Jim Lousararian, chief executive officer of Verax Biomedical.
According to the company, the new clearance is intended to help reduce the risk of bacterial contamination for pediatric patients receiving platelet transfusions.
“Pediatric patients pose unique challenges in transfusion medicine,” said Paul Mintz, MD, chief medical officer of Verax Biomedical.
“They require small platelet doses and possess fragile immune systems. PGD testing individual WBD units for transfusion makes it practical to provide bacterially tested platelets to this most vulnerable group of patients.”
Multicenter study
The Verax PGD® test was evaluated in a 2-year study including 18 US hospitals. The results were published in Transfusion in 2011.
The objective of the study was to evaluate the test’s ability to detect bacterially contaminated units in the US apheresis inventory that tested negative for contamination by existing growth-based QC tests.
A total of 9 contaminated units were detected by PGD and confirmed as bacterially contaminated in a population of 27,620 leukocyte-reduced apheresis units (1:3,069 doses tested).
All 9 units had previously tested negative by growth-based QC methods applied earlier in unit life in conformance with all applicable AABB and CAP standards for bacterial testing.
Researchers said the study clearly demonstrated the ability of the Platelet PGD Test to detect and interdict contaminated units missed by current QC testing methods. ![]()
The US Food and Drug Administration (FDA) has granted new clearance for Verax Biomedical’s Platelet PGD® Test.
This qualitative immunoassay is designed to detect aerobic and anaerobic Gram-positive and Gram-negative bacteria in platelets.
The test is now cleared for use on single units of leukocyte-reduced or non-leukocyte-reduced whole blood-derived (WBD) platelets in plasma.
The Platelet PGD Test was previously cleared by the FDA as a safety measure to be used following testing with a growth-based, quality control (QC) test for platelet components that is cleared by the FDA.
For this indication, the Platelet PGD Test can be used within 24 hours of transfusion on:
- Leukocyte-reduced apheresis platelets suspended in plasma
- Leukocyte-reduced apheresis platelets suspended in platelet additive solution C and plasma
- Pre-storage pools of up to 6 leukocyte-reduced WBD platelets suspended in plasma.
When used as a safety measure, the Platelet PGD Test can extend the dating of apheresis platelets in plasma from 5 to 7 days.
The Platelet PGD Test also has FDA clearance as a QC test for use on pools of up to 6 units of leukocyte-reduced and non-leukocyte-reduced WBD platelets suspended in plasma that are pooled within 4 hours of transfusion.
The latest FDA clearance extends this use to individual units of WBD platelets in plasma.
“[The new clearance] has been requested by current users of PGD as well as being outlined as a need in pending FDA Draft Guidance to address the risk of bacterial contamination in platelets,” said Jim Lousararian, chief executive officer of Verax Biomedical.
According to the company, the new clearance is intended to help reduce the risk of bacterial contamination for pediatric patients receiving platelet transfusions.
“Pediatric patients pose unique challenges in transfusion medicine,” said Paul Mintz, MD, chief medical officer of Verax Biomedical.
“They require small platelet doses and possess fragile immune systems. PGD testing individual WBD units for transfusion makes it practical to provide bacterially tested platelets to this most vulnerable group of patients.”
Multicenter study
The Verax PGD® test was evaluated in a 2-year study including 18 US hospitals. The results were published in Transfusion in 2011.
The objective of the study was to evaluate the test’s ability to detect bacterially contaminated units in the US apheresis inventory that tested negative for contamination by existing growth-based QC tests.
A total of 9 contaminated units were detected by PGD and confirmed as bacterially contaminated in a population of 27,620 leukocyte-reduced apheresis units (1:3,069 doses tested).
All 9 units had previously tested negative by growth-based QC methods applied earlier in unit life in conformance with all applicable AABB and CAP standards for bacterial testing.
Researchers said the study clearly demonstrated the ability of the Platelet PGD Test to detect and interdict contaminated units missed by current QC testing methods. ![]()
The US Food and Drug Administration (FDA) has granted new clearance for Verax Biomedical’s Platelet PGD® Test.
This qualitative immunoassay is designed to detect aerobic and anaerobic Gram-positive and Gram-negative bacteria in platelets.
The test is now cleared for use on single units of leukocyte-reduced or non-leukocyte-reduced whole blood-derived (WBD) platelets in plasma.
The Platelet PGD Test was previously cleared by the FDA as a safety measure to be used following testing with a growth-based, quality control (QC) test for platelet components that is cleared by the FDA.
For this indication, the Platelet PGD Test can be used within 24 hours of transfusion on:
- Leukocyte-reduced apheresis platelets suspended in plasma
- Leukocyte-reduced apheresis platelets suspended in platelet additive solution C and plasma
- Pre-storage pools of up to 6 leukocyte-reduced WBD platelets suspended in plasma.
When used as a safety measure, the Platelet PGD Test can extend the dating of apheresis platelets in plasma from 5 to 7 days.
The Platelet PGD Test also has FDA clearance as a QC test for use on pools of up to 6 units of leukocyte-reduced and non-leukocyte-reduced WBD platelets suspended in plasma that are pooled within 4 hours of transfusion.
The latest FDA clearance extends this use to individual units of WBD platelets in plasma.
“[The new clearance] has been requested by current users of PGD as well as being outlined as a need in pending FDA Draft Guidance to address the risk of bacterial contamination in platelets,” said Jim Lousararian, chief executive officer of Verax Biomedical.
According to the company, the new clearance is intended to help reduce the risk of bacterial contamination for pediatric patients receiving platelet transfusions.
“Pediatric patients pose unique challenges in transfusion medicine,” said Paul Mintz, MD, chief medical officer of Verax Biomedical.
“They require small platelet doses and possess fragile immune systems. PGD testing individual WBD units for transfusion makes it practical to provide bacterially tested platelets to this most vulnerable group of patients.”
Multicenter study
The Verax PGD® test was evaluated in a 2-year study including 18 US hospitals. The results were published in Transfusion in 2011.
The objective of the study was to evaluate the test’s ability to detect bacterially contaminated units in the US apheresis inventory that tested negative for contamination by existing growth-based QC tests.
A total of 9 contaminated units were detected by PGD and confirmed as bacterially contaminated in a population of 27,620 leukocyte-reduced apheresis units (1:3,069 doses tested).
All 9 units had previously tested negative by growth-based QC methods applied earlier in unit life in conformance with all applicable AABB and CAP standards for bacterial testing.
Researchers said the study clearly demonstrated the ability of the Platelet PGD Test to detect and interdict contaminated units missed by current QC testing methods. ![]()