User login
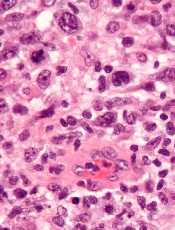
Researchers have discovered 3 subgroups of ALK-negative anaplastic large-cell lymphoma (ALCL) that have markedly different survival rates, according to a paper published in Blood.
They found that ALCL patients with TP63 rearrangements had a 17% chance of living 5 years beyond diagnosis, compared to 90% of patients who had DUSP22 rearrangements.
A third group of patients, those with neither rearrangement, had a 42% survival rate.
The researchers noted that these subgroups cannot be differentiated by routine pathology but can be identified via fluorescence in situ hybridization (FISH).
“This is the first study to demonstrate unequivocal genetic and clinical heterogeneity among systemic ALK-negative anaplastic large-cell lymphomas,” said study author Andrew L. Feldman, MD, of the Mayo Clinic in Rochester, Minnesota.
“Most strikingly, patients with DUSP22-rearranged ALCL had excellent overall survival rates, while patients with TP63-rearranged ALCL had dismal outcomes and nearly always failed standard therapy.”
Currently, all ALK-negative ALCLs are treated the same, using chemotherapy and, in some institutions, stem cell transplantation. But these new findings make a case for additional testing and possible changes to the standard of care.
“This is a great example of where individualized medicine can make a difference,” Dr Feldman said. “Patients whose chance of surviving is 1 in 6 are receiving the same therapy as patients whose odds are 9 in 10. Developing tests that identify how tumors are different is a critical step toward being able to tailor therapy to each individual patient.”
Therefore, Dr Feldman and his colleagues recommend performing FISH in all patients with ALK-negative ALCL.
To learn more about testing for DUSP22 and TP63:
- 6p25.3 FISH (DUSP22/IRF4): http://www.mayomedicallaboratories.com/test-catalog/Overview/60506
- 3q28 FISH (TP63): http://www.mayomedicallaboratories.com/test-catalog/Overview/70014.

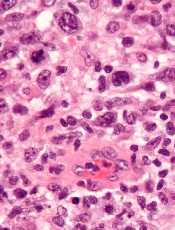
Researchers have discovered 3 subgroups of ALK-negative anaplastic large-cell lymphoma (ALCL) that have markedly different survival rates, according to a paper published in Blood.
They found that ALCL patients with TP63 rearrangements had a 17% chance of living 5 years beyond diagnosis, compared to 90% of patients who had DUSP22 rearrangements.
A third group of patients, those with neither rearrangement, had a 42% survival rate.
The researchers noted that these subgroups cannot be differentiated by routine pathology but can be identified via fluorescence in situ hybridization (FISH).
“This is the first study to demonstrate unequivocal genetic and clinical heterogeneity among systemic ALK-negative anaplastic large-cell lymphomas,” said study author Andrew L. Feldman, MD, of the Mayo Clinic in Rochester, Minnesota.
“Most strikingly, patients with DUSP22-rearranged ALCL had excellent overall survival rates, while patients with TP63-rearranged ALCL had dismal outcomes and nearly always failed standard therapy.”
Currently, all ALK-negative ALCLs are treated the same, using chemotherapy and, in some institutions, stem cell transplantation. But these new findings make a case for additional testing and possible changes to the standard of care.
“This is a great example of where individualized medicine can make a difference,” Dr Feldman said. “Patients whose chance of surviving is 1 in 6 are receiving the same therapy as patients whose odds are 9 in 10. Developing tests that identify how tumors are different is a critical step toward being able to tailor therapy to each individual patient.”
Therefore, Dr Feldman and his colleagues recommend performing FISH in all patients with ALK-negative ALCL.
To learn more about testing for DUSP22 and TP63:
- 6p25.3 FISH (DUSP22/IRF4): http://www.mayomedicallaboratories.com/test-catalog/Overview/60506
- 3q28 FISH (TP63): http://www.mayomedicallaboratories.com/test-catalog/Overview/70014.

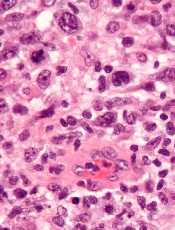
Researchers have discovered 3 subgroups of ALK-negative anaplastic large-cell lymphoma (ALCL) that have markedly different survival rates, according to a paper published in Blood.
They found that ALCL patients with TP63 rearrangements had a 17% chance of living 5 years beyond diagnosis, compared to 90% of patients who had DUSP22 rearrangements.
A third group of patients, those with neither rearrangement, had a 42% survival rate.
The researchers noted that these subgroups cannot be differentiated by routine pathology but can be identified via fluorescence in situ hybridization (FISH).
“This is the first study to demonstrate unequivocal genetic and clinical heterogeneity among systemic ALK-negative anaplastic large-cell lymphomas,” said study author Andrew L. Feldman, MD, of the Mayo Clinic in Rochester, Minnesota.
“Most strikingly, patients with DUSP22-rearranged ALCL had excellent overall survival rates, while patients with TP63-rearranged ALCL had dismal outcomes and nearly always failed standard therapy.”
Currently, all ALK-negative ALCLs are treated the same, using chemotherapy and, in some institutions, stem cell transplantation. But these new findings make a case for additional testing and possible changes to the standard of care.
“This is a great example of where individualized medicine can make a difference,” Dr Feldman said. “Patients whose chance of surviving is 1 in 6 are receiving the same therapy as patients whose odds are 9 in 10. Developing tests that identify how tumors are different is a critical step toward being able to tailor therapy to each individual patient.”
Therefore, Dr Feldman and his colleagues recommend performing FISH in all patients with ALK-negative ALCL.
To learn more about testing for DUSP22 and TP63:
- 6p25.3 FISH (DUSP22/IRF4): http://www.mayomedicallaboratories.com/test-catalog/Overview/60506
- 3q28 FISH (TP63): http://www.mayomedicallaboratories.com/test-catalog/Overview/70014.
