User login
- Read a related case in July’s Medical Verdicts
- “10 practical, evidence-based recommendations for the management of severe postpartum hemorrhage”
Baha M. Sibai, MD (June 2011) - “Postpartum hemorrhage: 11 critical questions, answered by an expert”
Q&A with Haywood L. Brown, MD (January 2011) - “What you can do to optimize blood conservation in ObGyn practice”
Eric J. Bieber, MD; Linda Scott, RN; Corinna Muller, DO; Nancy Nuss, RN; and Edie L. Derian, MD (February 2010) - “Planning reduces the risk of maternal death. This tool helps.”
Robert L. Barbieri, MD (Editorial; August 2009) - “Consider retroperitoneal packing for postpartum hemorrhage”
Maj. William R. Fulton, DO (July 2008)
Obstetricians know that postpartum hemorrhage (PPH) must be treated decisively and swiftly.1 To review:
Active management of the third stage after vaginal delivery, with a uterotonic such as oxytocin, helps to reduce the frequency of PPH2; in a recent randomized trial involving vaginal delivery, the rate of PPH was 10% in women who received postpartum oxytocin and 17% in those who did not (P<.001).3
When hemorrhage occurs despite oxytocin, having been given postpartum, the standard treatment algorithm (see the TABLE) calls for:
- uterine massage
- additional uterotonics
- identification and repair of vaginal and cervical lacerations
- removal of any retained products of conception.
Sequential interventions for managing postpartum hemorrhage
| This sequence of steps applies 1) after vaginal delivery (including the left hand-side interventions) and 2) after cesarean delivery, with the abdominal incision still open (including the right hand-side interventions). | |
| Hemorrhage after vaginal birth | Hemorrhage after cesarean delivery |
| Administer oxytocin | |
| Perform uterine massage | |
| Administer additional uterotonics (methergine, misoprostol, carboprost [Hemabate]) | |
| Bring 2 units of packed RBCs and 2 units of fresh frozen plasma (FFP) to point of care Transfuse based on the clinical condition Consider transfusing RBCs and FFP at a 1:1 ratio until clotting parameters are evaluated Obtain Stat clotting studies Start an additional intravenous line | |
| Move the patient to the operating room |
|
| Repair any tears |
|
| Place uterine compression suture(s), such as a B-Lynch suture |
| Place an intrauterine balloon | Consider bilateral ligation of the internal iliac artery |
| If indicated, call for additional specialists: second anesthesiologist, gyn surgeon, interventional radiologist, blood bank director | |
| Selective embolization by interventional radiology | Hysterectomy |
| Exploratory laparotomy—follow steps (along the right-hand side of this table) for treating hemorrhage after cesarean delivery | Pelvic packing |
| Adapted from: California Maternal Quality Care Collaborative (www.CMQCC.org). | |
Placing an intrauterine balloon, such as the Bakri Postpartum Balloon (Cook Medical) or the BT-Cath (Utah Medical Products), is strongly recommended if these steps do not control bleeding.
In this Editorial, I review tips and tricks for using the Bakri balloon, building on my earlier OBG Management Editorial (February 2009), in which I outlined a basic approach to intrauterine balloon tamponade.4
TIP: Place the Bakri balloon early in the PPH treatment algorithm
For postpartum hemorrhage after vaginal delivery, typical initial steps include, as noted, fundal massage, administration of uterotonics, and curettage to remove retained products of conception. If these steps are ineffective, don’t wait: Immediately consider placing a Bakri balloon. Time is precious, and wasting time with less effective interventions results in excessive blood loss and consumption of clotting factors and increases the risk of a coagulopathy.
I’ve found that clinicians often spend too much time trying to determine whether postpartum bleeding originates in the uterus or from a cervical or vaginal laceration. But heavy bleeding can obscure anatomic structures, making it difficult to identify the site of bleeding with precision. Fruitlessly perseverating to differentiate uterine, cervical, and upper vaginal sources of bleeding can waste valuable time and lead to unnecessary blood loss.
By placing a Bakri balloon and inflating it early in the PPH treatment algorithm, you will significantly reduce uterine bleeding. You will also be able to assess the cervix and upper vagina more effectively for lacerations.
My recommendation. Place the Bakri balloon as soon as it is apparent that bleeding is so heavy that you are going to have difficulty assessing the cervix and upper vagina for lacerations. Note that this stands in contrast to the usual recommendation that you assess the cervix and vagina for lacerations before you place the Bakri balloon.
TIP: Have 3 clinicians place the balloon
Teamwork is a key to success here: The Bakri balloon is most quickly and elegantly inserted and inflated when three clinicians team up, as follows:
Clinician#1 scans the uterus, assessing for retained products of conception and providing real-time imaging as the balloon is placed and inflated. This team member provides feedback to the others about correct placement and filling of the balloon.
Clinician#2 inserts the balloon into the uterus by placing her hand into the vagina and guiding the balloon into the proper intrauterine position. (Most often, clinician#2 is the delivering clinician.) This technique is performed in a manner similar to how one places an intrauterine pressure catheter.5
Clinician #2 stabilizes the balloon in position by maintaining her hand in the vagina. She ensures that the balloon does not “pop” out of the lower uterus as the balloon is filled (FIGURE).
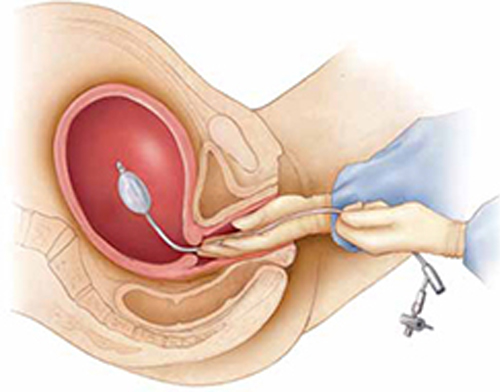
Manual insertion of a Bakri balloon
Insert the balloon into the uterus by 1) placing your hand into the vagina and guiding the balloon into the proper intrauterine position (similar to the manner in which an intrauterine pressure catheter is placed),5 2) stabilizing the balloon in position by maintaining the hand in the vagina, and 3) ensuring that the balloon does not “pop” out of the lower uterus as the balloon is filled.Clinician #3 simultaneously begins to instill sterile fluid into the balloon. This team member can be a nurse, medical assistant, or surgical technician.
My recommendation. Consider using simulation training to practice the team approach to placing the Bakri balloon. This is an effective method of improving team coordination.
TIP: Instill at least 150 mL of fluid
In short, use more fluid, not less. Although one study showed that most clinicians fill the balloon to a median volume of 300 mL,6 I’ve observed that some timidly instill the balloon with 80 to 120 mL of fluid. I think this is too little to maximize the effectiveness of the balloon for a postpartum patient who has massive hemorrhage.
Studies have shown that filling the balloon to at least 150 mL noticeably increases tamponade pressure.7
TIP: Place a pack in the upper vagina to stabilize the balloon in position
It usually takes only a few minutes after the Bakri balloon is filled to determine whether it is going to control uterine bleeding—what is called a tamponade test. If the balloon does control bleeding, you can place a vaginal pack of ribbon gauze to help ensure that the balloon does not slip down through the dilated postpartum cervix.
To avoid obscuring continued bleeding, however, do not place vaginal packing until you have obtained a positive tamponade test.
TIP: Check the hemoglobin concentration, platelet count, and coagulation status
The trauma literature demonstrates that optimal patient outcomes are realized when the following targets are maintained during resuscitation of patients who have massive hemorrhage8:
- hematocrit, ≥21%
- platelet count, ≥50 × 103/μL
- fibrinogen ≥100 mg/dL
- International Normalized Ratio (INR) ≤1.5.
These targets are achieved by appropriate transfusion of red blood cells, platelets, fresh frozen plasma, cryoprecipitate, and purified recombinant fibrinogen concentrate (RiaSTAP). Many trauma specialists recommend transfusion of a 1:1 ratio of RBCs and fresh frozen plasma in cases of major hemorrhage until coagulation status is normalized.
My recommendation. Often, it takes as long as 1 hour (sometimes, longer) to get results of Stat coagulation tests from the lab. While you are waiting, obtain clinical evidence of clotting function by filling a red-top tube with the patient’s blood. Adequate function is signaled by formation of a stable clot within 10 minutes.
TIP: Practice your team’s response to PPH with simulation
Last, I urge clinicians in every birthing unit to use simulation exercises to improve all facets of their response to severe postpartum hemorrhage.9
Summing up
Death following PPH remains a major cause of maternal mortality in developed and developing countries. The appropriateness of your response within 10 minutes of the onset of PPH is critical to ensuring a successful outcome and minimizing adverse events.10 To help, use the Bakri Postpartum Balloon often, and use it early.
What are your tips and tricks for effective use of intra-uterine balloon tamponade in postpartum hemorrhage?
To enter your response, click here or send your pearl to [email protected], with your name and location of practice.
We’ll publish a sampling of bylined contributions in an upcoming issue of OBG Management, with appreciation.
1. Sibai BM. 10 practical evidence-based recommendations for managing severe postpartum hemorrhage. OBG Manage. 2011;23(6):44-48.
2. Barbieri RL. Give a uterotonic routinely during the third stage of labor. OBG Manage. 2007;19(05):6-13.
3. Jangsten E, Mattsson LA, Lyckestam I, Hellstrom AL, Berg M. A comparison of active management and expectant management of the third stage of labour: a Swedish randomised controlled trial. BJOG. 2011;118(3):362-369.
4. Barbieri RL. You should add the Bakri balloon to your treatment for OB bleeds. OBG Manage. 2009;21(2):6-10.
5. Dabelea V, Schultze PM, McDuffie RS, Jr. Intrauterine balloon tamponade in the management of postpartum hemorrhage. Am J Perinatol. 2007;24(6):359-364.
6. Vitthala S, Tsoumpou I, Anjum ZK, Aziz NA. Use of Bakri balloon in post-partum hemorrhage: a series of 15 cases. Aust NZ J Obstet Gynecol. 2009;49(2):191-194.
7. Georgiou C. Intraluminal pressure readings during the establishment of a positive “tamponade test” in the management of postpartum hemorrhage. BJOG. 2010;117(3):295-303.
8. Barbieri RL. Control of massive hemorrhage: Lessons from Iraq reach the US labor and delivery suite. OBG Manage. 2007;19(7):8-16.
9. Skupski DW, Lowenwirt IP, Weinbaum FI, Brodsky D, Danek M, Eglinton GS. Improving hospital systems for the care of women with major obstetric hemorrhage. Obstet Gynecol. 2006;107(5):977-983.
10. Driessen M, Bouvier-Colle MH, Dupont C, et al. Pithagore6 Group Postpartum hemorrhage resulting from uterine atony after vaginal delivery: factors associated with severity. Obstet Gynecol. 2011;117(1):21-31.
- Read a related case in July’s Medical Verdicts
- “10 practical, evidence-based recommendations for the management of severe postpartum hemorrhage”
Baha M. Sibai, MD (June 2011) - “Postpartum hemorrhage: 11 critical questions, answered by an expert”
Q&A with Haywood L. Brown, MD (January 2011) - “What you can do to optimize blood conservation in ObGyn practice”
Eric J. Bieber, MD; Linda Scott, RN; Corinna Muller, DO; Nancy Nuss, RN; and Edie L. Derian, MD (February 2010) - “Planning reduces the risk of maternal death. This tool helps.”
Robert L. Barbieri, MD (Editorial; August 2009) - “Consider retroperitoneal packing for postpartum hemorrhage”
Maj. William R. Fulton, DO (July 2008)
Obstetricians know that postpartum hemorrhage (PPH) must be treated decisively and swiftly.1 To review:
Active management of the third stage after vaginal delivery, with a uterotonic such as oxytocin, helps to reduce the frequency of PPH2; in a recent randomized trial involving vaginal delivery, the rate of PPH was 10% in women who received postpartum oxytocin and 17% in those who did not (P<.001).3
When hemorrhage occurs despite oxytocin, having been given postpartum, the standard treatment algorithm (see the TABLE) calls for:
- uterine massage
- additional uterotonics
- identification and repair of vaginal and cervical lacerations
- removal of any retained products of conception.
Sequential interventions for managing postpartum hemorrhage
| This sequence of steps applies 1) after vaginal delivery (including the left hand-side interventions) and 2) after cesarean delivery, with the abdominal incision still open (including the right hand-side interventions). | |
| Hemorrhage after vaginal birth | Hemorrhage after cesarean delivery |
| Administer oxytocin | |
| Perform uterine massage | |
| Administer additional uterotonics (methergine, misoprostol, carboprost [Hemabate]) | |
| Bring 2 units of packed RBCs and 2 units of fresh frozen plasma (FFP) to point of care Transfuse based on the clinical condition Consider transfusing RBCs and FFP at a 1:1 ratio until clotting parameters are evaluated Obtain Stat clotting studies Start an additional intravenous line | |
| Move the patient to the operating room |
|
| Repair any tears |
|
| Place uterine compression suture(s), such as a B-Lynch suture |
| Place an intrauterine balloon | Consider bilateral ligation of the internal iliac artery |
| If indicated, call for additional specialists: second anesthesiologist, gyn surgeon, interventional radiologist, blood bank director | |
| Selective embolization by interventional radiology | Hysterectomy |
| Exploratory laparotomy—follow steps (along the right-hand side of this table) for treating hemorrhage after cesarean delivery | Pelvic packing |
| Adapted from: California Maternal Quality Care Collaborative (www.CMQCC.org). | |
Placing an intrauterine balloon, such as the Bakri Postpartum Balloon (Cook Medical) or the BT-Cath (Utah Medical Products), is strongly recommended if these steps do not control bleeding.
In this Editorial, I review tips and tricks for using the Bakri balloon, building on my earlier OBG Management Editorial (February 2009), in which I outlined a basic approach to intrauterine balloon tamponade.4
TIP: Place the Bakri balloon early in the PPH treatment algorithm
For postpartum hemorrhage after vaginal delivery, typical initial steps include, as noted, fundal massage, administration of uterotonics, and curettage to remove retained products of conception. If these steps are ineffective, don’t wait: Immediately consider placing a Bakri balloon. Time is precious, and wasting time with less effective interventions results in excessive blood loss and consumption of clotting factors and increases the risk of a coagulopathy.
I’ve found that clinicians often spend too much time trying to determine whether postpartum bleeding originates in the uterus or from a cervical or vaginal laceration. But heavy bleeding can obscure anatomic structures, making it difficult to identify the site of bleeding with precision. Fruitlessly perseverating to differentiate uterine, cervical, and upper vaginal sources of bleeding can waste valuable time and lead to unnecessary blood loss.
By placing a Bakri balloon and inflating it early in the PPH treatment algorithm, you will significantly reduce uterine bleeding. You will also be able to assess the cervix and upper vagina more effectively for lacerations.
My recommendation. Place the Bakri balloon as soon as it is apparent that bleeding is so heavy that you are going to have difficulty assessing the cervix and upper vagina for lacerations. Note that this stands in contrast to the usual recommendation that you assess the cervix and vagina for lacerations before you place the Bakri balloon.
TIP: Have 3 clinicians place the balloon
Teamwork is a key to success here: The Bakri balloon is most quickly and elegantly inserted and inflated when three clinicians team up, as follows:
Clinician#1 scans the uterus, assessing for retained products of conception and providing real-time imaging as the balloon is placed and inflated. This team member provides feedback to the others about correct placement and filling of the balloon.
Clinician#2 inserts the balloon into the uterus by placing her hand into the vagina and guiding the balloon into the proper intrauterine position. (Most often, clinician#2 is the delivering clinician.) This technique is performed in a manner similar to how one places an intrauterine pressure catheter.5
Clinician #2 stabilizes the balloon in position by maintaining her hand in the vagina. She ensures that the balloon does not “pop” out of the lower uterus as the balloon is filled (FIGURE).
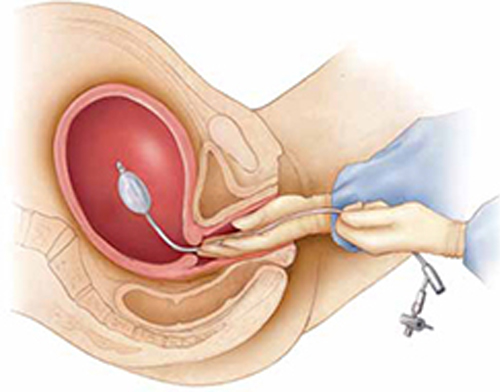
Manual insertion of a Bakri balloon
Insert the balloon into the uterus by 1) placing your hand into the vagina and guiding the balloon into the proper intrauterine position (similar to the manner in which an intrauterine pressure catheter is placed),5 2) stabilizing the balloon in position by maintaining the hand in the vagina, and 3) ensuring that the balloon does not “pop” out of the lower uterus as the balloon is filled.Clinician #3 simultaneously begins to instill sterile fluid into the balloon. This team member can be a nurse, medical assistant, or surgical technician.
My recommendation. Consider using simulation training to practice the team approach to placing the Bakri balloon. This is an effective method of improving team coordination.
TIP: Instill at least 150 mL of fluid
In short, use more fluid, not less. Although one study showed that most clinicians fill the balloon to a median volume of 300 mL,6 I’ve observed that some timidly instill the balloon with 80 to 120 mL of fluid. I think this is too little to maximize the effectiveness of the balloon for a postpartum patient who has massive hemorrhage.
Studies have shown that filling the balloon to at least 150 mL noticeably increases tamponade pressure.7
TIP: Place a pack in the upper vagina to stabilize the balloon in position
It usually takes only a few minutes after the Bakri balloon is filled to determine whether it is going to control uterine bleeding—what is called a tamponade test. If the balloon does control bleeding, you can place a vaginal pack of ribbon gauze to help ensure that the balloon does not slip down through the dilated postpartum cervix.
To avoid obscuring continued bleeding, however, do not place vaginal packing until you have obtained a positive tamponade test.
TIP: Check the hemoglobin concentration, platelet count, and coagulation status
The trauma literature demonstrates that optimal patient outcomes are realized when the following targets are maintained during resuscitation of patients who have massive hemorrhage8:
- hematocrit, ≥21%
- platelet count, ≥50 × 103/μL
- fibrinogen ≥100 mg/dL
- International Normalized Ratio (INR) ≤1.5.
These targets are achieved by appropriate transfusion of red blood cells, platelets, fresh frozen plasma, cryoprecipitate, and purified recombinant fibrinogen concentrate (RiaSTAP). Many trauma specialists recommend transfusion of a 1:1 ratio of RBCs and fresh frozen plasma in cases of major hemorrhage until coagulation status is normalized.
My recommendation. Often, it takes as long as 1 hour (sometimes, longer) to get results of Stat coagulation tests from the lab. While you are waiting, obtain clinical evidence of clotting function by filling a red-top tube with the patient’s blood. Adequate function is signaled by formation of a stable clot within 10 minutes.
TIP: Practice your team’s response to PPH with simulation
Last, I urge clinicians in every birthing unit to use simulation exercises to improve all facets of their response to severe postpartum hemorrhage.9
Summing up
Death following PPH remains a major cause of maternal mortality in developed and developing countries. The appropriateness of your response within 10 minutes of the onset of PPH is critical to ensuring a successful outcome and minimizing adverse events.10 To help, use the Bakri Postpartum Balloon often, and use it early.
What are your tips and tricks for effective use of intra-uterine balloon tamponade in postpartum hemorrhage?
To enter your response, click here or send your pearl to [email protected], with your name and location of practice.
We’ll publish a sampling of bylined contributions in an upcoming issue of OBG Management, with appreciation.
- Read a related case in July’s Medical Verdicts
- “10 practical, evidence-based recommendations for the management of severe postpartum hemorrhage”
Baha M. Sibai, MD (June 2011) - “Postpartum hemorrhage: 11 critical questions, answered by an expert”
Q&A with Haywood L. Brown, MD (January 2011) - “What you can do to optimize blood conservation in ObGyn practice”
Eric J. Bieber, MD; Linda Scott, RN; Corinna Muller, DO; Nancy Nuss, RN; and Edie L. Derian, MD (February 2010) - “Planning reduces the risk of maternal death. This tool helps.”
Robert L. Barbieri, MD (Editorial; August 2009) - “Consider retroperitoneal packing for postpartum hemorrhage”
Maj. William R. Fulton, DO (July 2008)
Obstetricians know that postpartum hemorrhage (PPH) must be treated decisively and swiftly.1 To review:
Active management of the third stage after vaginal delivery, with a uterotonic such as oxytocin, helps to reduce the frequency of PPH2; in a recent randomized trial involving vaginal delivery, the rate of PPH was 10% in women who received postpartum oxytocin and 17% in those who did not (P<.001).3
When hemorrhage occurs despite oxytocin, having been given postpartum, the standard treatment algorithm (see the TABLE) calls for:
- uterine massage
- additional uterotonics
- identification and repair of vaginal and cervical lacerations
- removal of any retained products of conception.
Sequential interventions for managing postpartum hemorrhage
| This sequence of steps applies 1) after vaginal delivery (including the left hand-side interventions) and 2) after cesarean delivery, with the abdominal incision still open (including the right hand-side interventions). | |
| Hemorrhage after vaginal birth | Hemorrhage after cesarean delivery |
| Administer oxytocin | |
| Perform uterine massage | |
| Administer additional uterotonics (methergine, misoprostol, carboprost [Hemabate]) | |
| Bring 2 units of packed RBCs and 2 units of fresh frozen plasma (FFP) to point of care Transfuse based on the clinical condition Consider transfusing RBCs and FFP at a 1:1 ratio until clotting parameters are evaluated Obtain Stat clotting studies Start an additional intravenous line | |
| Move the patient to the operating room |
|
| Repair any tears |
|
| Place uterine compression suture(s), such as a B-Lynch suture |
| Place an intrauterine balloon | Consider bilateral ligation of the internal iliac artery |
| If indicated, call for additional specialists: second anesthesiologist, gyn surgeon, interventional radiologist, blood bank director | |
| Selective embolization by interventional radiology | Hysterectomy |
| Exploratory laparotomy—follow steps (along the right-hand side of this table) for treating hemorrhage after cesarean delivery | Pelvic packing |
| Adapted from: California Maternal Quality Care Collaborative (www.CMQCC.org). | |
Placing an intrauterine balloon, such as the Bakri Postpartum Balloon (Cook Medical) or the BT-Cath (Utah Medical Products), is strongly recommended if these steps do not control bleeding.
In this Editorial, I review tips and tricks for using the Bakri balloon, building on my earlier OBG Management Editorial (February 2009), in which I outlined a basic approach to intrauterine balloon tamponade.4
TIP: Place the Bakri balloon early in the PPH treatment algorithm
For postpartum hemorrhage after vaginal delivery, typical initial steps include, as noted, fundal massage, administration of uterotonics, and curettage to remove retained products of conception. If these steps are ineffective, don’t wait: Immediately consider placing a Bakri balloon. Time is precious, and wasting time with less effective interventions results in excessive blood loss and consumption of clotting factors and increases the risk of a coagulopathy.
I’ve found that clinicians often spend too much time trying to determine whether postpartum bleeding originates in the uterus or from a cervical or vaginal laceration. But heavy bleeding can obscure anatomic structures, making it difficult to identify the site of bleeding with precision. Fruitlessly perseverating to differentiate uterine, cervical, and upper vaginal sources of bleeding can waste valuable time and lead to unnecessary blood loss.
By placing a Bakri balloon and inflating it early in the PPH treatment algorithm, you will significantly reduce uterine bleeding. You will also be able to assess the cervix and upper vagina more effectively for lacerations.
My recommendation. Place the Bakri balloon as soon as it is apparent that bleeding is so heavy that you are going to have difficulty assessing the cervix and upper vagina for lacerations. Note that this stands in contrast to the usual recommendation that you assess the cervix and vagina for lacerations before you place the Bakri balloon.
TIP: Have 3 clinicians place the balloon
Teamwork is a key to success here: The Bakri balloon is most quickly and elegantly inserted and inflated when three clinicians team up, as follows:
Clinician#1 scans the uterus, assessing for retained products of conception and providing real-time imaging as the balloon is placed and inflated. This team member provides feedback to the others about correct placement and filling of the balloon.
Clinician#2 inserts the balloon into the uterus by placing her hand into the vagina and guiding the balloon into the proper intrauterine position. (Most often, clinician#2 is the delivering clinician.) This technique is performed in a manner similar to how one places an intrauterine pressure catheter.5
Clinician #2 stabilizes the balloon in position by maintaining her hand in the vagina. She ensures that the balloon does not “pop” out of the lower uterus as the balloon is filled (FIGURE).
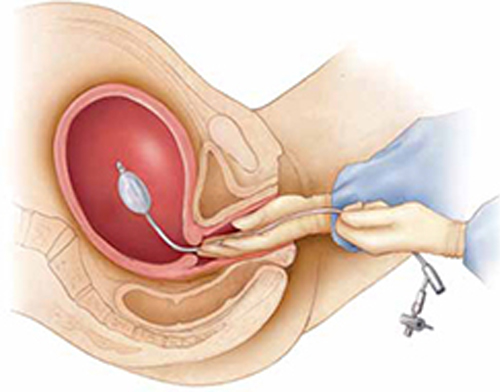
Manual insertion of a Bakri balloon
Insert the balloon into the uterus by 1) placing your hand into the vagina and guiding the balloon into the proper intrauterine position (similar to the manner in which an intrauterine pressure catheter is placed),5 2) stabilizing the balloon in position by maintaining the hand in the vagina, and 3) ensuring that the balloon does not “pop” out of the lower uterus as the balloon is filled.Clinician #3 simultaneously begins to instill sterile fluid into the balloon. This team member can be a nurse, medical assistant, or surgical technician.
My recommendation. Consider using simulation training to practice the team approach to placing the Bakri balloon. This is an effective method of improving team coordination.
TIP: Instill at least 150 mL of fluid
In short, use more fluid, not less. Although one study showed that most clinicians fill the balloon to a median volume of 300 mL,6 I’ve observed that some timidly instill the balloon with 80 to 120 mL of fluid. I think this is too little to maximize the effectiveness of the balloon for a postpartum patient who has massive hemorrhage.
Studies have shown that filling the balloon to at least 150 mL noticeably increases tamponade pressure.7
TIP: Place a pack in the upper vagina to stabilize the balloon in position
It usually takes only a few minutes after the Bakri balloon is filled to determine whether it is going to control uterine bleeding—what is called a tamponade test. If the balloon does control bleeding, you can place a vaginal pack of ribbon gauze to help ensure that the balloon does not slip down through the dilated postpartum cervix.
To avoid obscuring continued bleeding, however, do not place vaginal packing until you have obtained a positive tamponade test.
TIP: Check the hemoglobin concentration, platelet count, and coagulation status
The trauma literature demonstrates that optimal patient outcomes are realized when the following targets are maintained during resuscitation of patients who have massive hemorrhage8:
- hematocrit, ≥21%
- platelet count, ≥50 × 103/μL
- fibrinogen ≥100 mg/dL
- International Normalized Ratio (INR) ≤1.5.
These targets are achieved by appropriate transfusion of red blood cells, platelets, fresh frozen plasma, cryoprecipitate, and purified recombinant fibrinogen concentrate (RiaSTAP). Many trauma specialists recommend transfusion of a 1:1 ratio of RBCs and fresh frozen plasma in cases of major hemorrhage until coagulation status is normalized.
My recommendation. Often, it takes as long as 1 hour (sometimes, longer) to get results of Stat coagulation tests from the lab. While you are waiting, obtain clinical evidence of clotting function by filling a red-top tube with the patient’s blood. Adequate function is signaled by formation of a stable clot within 10 minutes.
TIP: Practice your team’s response to PPH with simulation
Last, I urge clinicians in every birthing unit to use simulation exercises to improve all facets of their response to severe postpartum hemorrhage.9
Summing up
Death following PPH remains a major cause of maternal mortality in developed and developing countries. The appropriateness of your response within 10 minutes of the onset of PPH is critical to ensuring a successful outcome and minimizing adverse events.10 To help, use the Bakri Postpartum Balloon often, and use it early.
What are your tips and tricks for effective use of intra-uterine balloon tamponade in postpartum hemorrhage?
To enter your response, click here or send your pearl to [email protected], with your name and location of practice.
We’ll publish a sampling of bylined contributions in an upcoming issue of OBG Management, with appreciation.
1. Sibai BM. 10 practical evidence-based recommendations for managing severe postpartum hemorrhage. OBG Manage. 2011;23(6):44-48.
2. Barbieri RL. Give a uterotonic routinely during the third stage of labor. OBG Manage. 2007;19(05):6-13.
3. Jangsten E, Mattsson LA, Lyckestam I, Hellstrom AL, Berg M. A comparison of active management and expectant management of the third stage of labour: a Swedish randomised controlled trial. BJOG. 2011;118(3):362-369.
4. Barbieri RL. You should add the Bakri balloon to your treatment for OB bleeds. OBG Manage. 2009;21(2):6-10.
5. Dabelea V, Schultze PM, McDuffie RS, Jr. Intrauterine balloon tamponade in the management of postpartum hemorrhage. Am J Perinatol. 2007;24(6):359-364.
6. Vitthala S, Tsoumpou I, Anjum ZK, Aziz NA. Use of Bakri balloon in post-partum hemorrhage: a series of 15 cases. Aust NZ J Obstet Gynecol. 2009;49(2):191-194.
7. Georgiou C. Intraluminal pressure readings during the establishment of a positive “tamponade test” in the management of postpartum hemorrhage. BJOG. 2010;117(3):295-303.
8. Barbieri RL. Control of massive hemorrhage: Lessons from Iraq reach the US labor and delivery suite. OBG Manage. 2007;19(7):8-16.
9. Skupski DW, Lowenwirt IP, Weinbaum FI, Brodsky D, Danek M, Eglinton GS. Improving hospital systems for the care of women with major obstetric hemorrhage. Obstet Gynecol. 2006;107(5):977-983.
10. Driessen M, Bouvier-Colle MH, Dupont C, et al. Pithagore6 Group Postpartum hemorrhage resulting from uterine atony after vaginal delivery: factors associated with severity. Obstet Gynecol. 2011;117(1):21-31.
1. Sibai BM. 10 practical evidence-based recommendations for managing severe postpartum hemorrhage. OBG Manage. 2011;23(6):44-48.
2. Barbieri RL. Give a uterotonic routinely during the third stage of labor. OBG Manage. 2007;19(05):6-13.
3. Jangsten E, Mattsson LA, Lyckestam I, Hellstrom AL, Berg M. A comparison of active management and expectant management of the third stage of labour: a Swedish randomised controlled trial. BJOG. 2011;118(3):362-369.
4. Barbieri RL. You should add the Bakri balloon to your treatment for OB bleeds. OBG Manage. 2009;21(2):6-10.
5. Dabelea V, Schultze PM, McDuffie RS, Jr. Intrauterine balloon tamponade in the management of postpartum hemorrhage. Am J Perinatol. 2007;24(6):359-364.
6. Vitthala S, Tsoumpou I, Anjum ZK, Aziz NA. Use of Bakri balloon in post-partum hemorrhage: a series of 15 cases. Aust NZ J Obstet Gynecol. 2009;49(2):191-194.
7. Georgiou C. Intraluminal pressure readings during the establishment of a positive “tamponade test” in the management of postpartum hemorrhage. BJOG. 2010;117(3):295-303.
8. Barbieri RL. Control of massive hemorrhage: Lessons from Iraq reach the US labor and delivery suite. OBG Manage. 2007;19(7):8-16.
9. Skupski DW, Lowenwirt IP, Weinbaum FI, Brodsky D, Danek M, Eglinton GS. Improving hospital systems for the care of women with major obstetric hemorrhage. Obstet Gynecol. 2006;107(5):977-983.
10. Driessen M, Bouvier-Colle MH, Dupont C, et al. Pithagore6 Group Postpartum hemorrhage resulting from uterine atony after vaginal delivery: factors associated with severity. Obstet Gynecol. 2011;117(1):21-31.
