User login
October marks the start of a new fiscal year for the federal government and with it comes a host of new and revised regulatory requirements for hospitalists and hospitals.
Medicare officials are using some carrots – but mostly sticks – to get hospitals and doctors to improve quality and lower costs. Some of the programs levy financial penalties on hospitals but affect the day-to-day work of hospitalists, while others affect physicians at the individual level.
"There’s a lot of confusion and lack of knowledge about what’s occurring at the physician level and what’s occurring at the hospital level," said Dr. Patrick J. Torcson, a member of the board of directors of the Society of Hospital Medicine (SHM) and director of hospital medicine at St. Tammany Parish Hospital in Covington, La.
Carrots, sticks for hospitalists
Two programs will touch hospitalists – and their wallets – directly. Medicare’s Physician Quality Reporting System (PQRS), a voluntary pay-for-reporting program, has been around since 2007 offering small incentives for participation, but it will soon begin penalizing physicians who don’t report on quality. Officials at the Centers for Medicare and Medicaid Services (CMS) are also phasing in the physician value-based modifier, which will begin adjusting physician payments up or down depending on the quality and cost of the care they provide.
CMS will use PQRS reporting as the basis for the new modifier, making participation in the older program a top priority for all physicians, Dr. Torcson said.
This year, physicians who successfully report quality measures through PQRS can earn a 0.5% bonus on their total allowable Medicare Part B charges. The same bonus will be in place for 2014. But starting in 2015, Medicare will assess a 1.5% penalty on physicians who fail to report successfully. That payment penalty increases to 2% in 2016.
But the PQRS has been criticized as being cumbersome and not especially relevant for hospitalists.
"I think many physicians hoped it would go away," Dr. Torcson said. "It hasn’t. It has expanded."
Hospitalists are currently required to report on at least three quality measures through the program. But Medicare is proposing to require physicians to report on at least nine measures starting in 2014. CMS will issue a final regulation outlining changes to the PQRS in November.
The SHM has recommended instead that CMS limit the expansion to no more than six quality measures to keep from ramping up the program too fast.
In comments to the agency, SHM also noted that the PQRS quality measures, while improving, still do not accurately reflect the scope of care provided by hospitalists. For instance, about half of the measures that hospitalists can report on are related to stroke care, though stoke care is not a primary practice focus for many hospital medicine programs.
Many hospitalists have ignored the PQRS so far, Dr. Torcson said, because the added time and effort of reporting on quality measures outweighed the value of the 0.5% bonus, on average about $500 per physician. But he urged physicians to rethink participation in light of the rollout of the new value-based modifier program.
Value-based modifier coming soon
The physician value-based payment modifier was part of the 2008 Medicare Improvement for Patients and Providers Act and was expanded as part of the 2010 Affordable Care Act. The program seeks to pay physicians more for providing high-quality, low-cost care. But the budget-neutral program will pay less for low-quality, high-cost care. Physician groups could see payment cuts of between 1% and 2% in 2016, based on their performance. Physicians who don’t report on quality measures through the PQRS will get an automatic 1% pay cut under the value-based modifier program.
The value-based modifier already is affecting physicians who work in groups of 100 or more eligible providers. While payments won’t be affected until 2015, CMS will base its adjustments on the data reported to the PQRS in 2013. The program will expand to cover physician groups of 10 or more in 2016, though the measurement on cost and quality will occur in 2014. Payments for all physicians will be subject to the modifier by 2017, based on performance during 2015.
"Physician-level pay for reporting is well underway and now actual pay for performance is here," Dr. Torcson said. "Engagement, familiarity, and participation in the PQRS is really going to be the key for physicians. It’s not too late."
CMS is providing some tools to help physicians understand their performance on cost and quality. The agency is producing annual Quality and Resource Use Reports (QRURs) that will show the individual physician’s past performance on the measures chosen by CMS. The reports are scheduled to go out to groups of 25 or more eligible professionals this fall. All physicians should start receiving the reports sometime in 2014.
But hospitalists should look closely at their reports, Dr. Torcson said. CMS is still figuring out how to classify the work done by hospitalists. Currently, CMS compares hospitalists’ cost and quality data to general internists even though hospitalized patients have a very different quality and cost profile.
"That’s something where there are still ongoing focused advocacy efforts by SHM to make sure that the attribution and the measurement methodology takes into account the hospitalist model," he said.
Hospitals under pressure, too
But hospitalists have more them just themselves to worry about. Often it’s the hospitalist who is the point person for quality and efficiency in their institution. And Medicare has an array of hospital-focused carrots and sticks, as well.
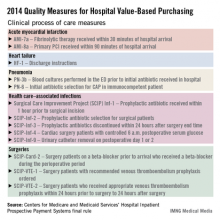
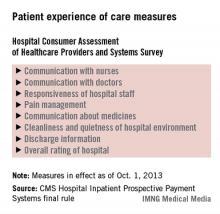
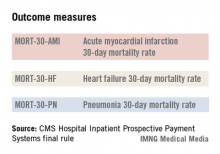
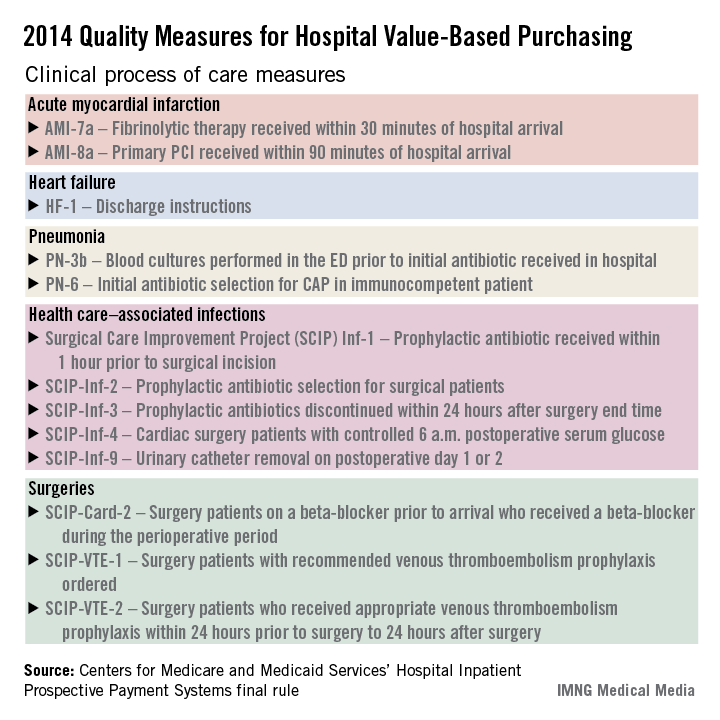
The hospital value-based purchasing program is already in full swing. For fiscal year 2014, which begins in October 2013, hospitals will have 1.25% of their base operating charges at risk in the program. The program bases payment on a group of clinical process measures, patient satisfaction, and selected mortality measures.
Additionally, Medicare is doubling the maximum penalties for its from 1% to 2% of base operating payments starting this month. The penalties apply to hospitals that have excess 30-day readmissions for pneumonia, heart failure, and acute myocardial infarction. CMS is also expected to add more conditions to the list. Total hip and Hospital Readmissions Reduction Program knee arthroplasty and chronic obstructive pulmonary disease will be added to the list of conditions in October 2014.
CMS is also launching a new Hospital-Acquired Condition (HAC) Reduction Program in October 2014. In this program, which was authorized under the Affordable Care Act, hospitals with the most HACs will see their payments reduced by 1%. During the first year, hospitals will be judged based on several indicators including:
• Pressure ulcer rate.
• Iatrogenic pneumothorax rate.
• Central venous catheter–related blood stream infection rate.
• Postoperative hip fracture rate.
• Postoperative pulmonary embolism or deep vein thrombosis rate.
• Postoperative sepsis rate.
• Wound dehiscence rate.
• Accidental puncture and laceration rate.
• Central line–associated blood stream infection.
• Catheter-associated urinary tract infection.
• Hospitals’ scores will be risk adjusted based on age, sex, and comorbidities.
More regulatory changes
CMS is also making some changes that will impact how hospitalists admit patients. Over the summer, Medicare officials issued a regulation that changes the criteria for when to admit a patient to hospital, as covered under Medicare Part A, and when to place them under observation status under Part B. The new criteria are based on the amount of time the physician expects the patient to spend as an inpatient.
Starting on Oct. 1, 2013, Medicare contractors will assume that a hospital stay is covered under Part A if the physician expects the patient to stay as an inpatient in the hospital for at least 2 midnights. CMS also emphasized in the rule that the inpatient stay does not begin until the patient is formally admitted by a physician.
What can hospitalists do to prepare?
While new regulatory requirements continue to hit hospitals year after year, Dr. Torcson said hospitalists are well prepared to handle the changes.
"The whole purpose and success and value of hospitalists is being the physician champions for the hospital-level performance agenda around core measures, readmissions, hospital-acquired conditions, and medical necessity documentation," he said. "That’s something that hospitalists have been preparing for from day 1, going back to the ’90s."
He urged hospitalists to redouble their efforts as hospital champions for quality.
"Concentrating on the hospital-level performance agenda is really going to be the key for hospital medicine programs to continue to be successful," Dr. Torcson said.
On Twitter @MaryEllenNY
October marks the start of a new fiscal year for the federal government and with it comes a host of new and revised regulatory requirements for hospitalists and hospitals.
Medicare officials are using some carrots – but mostly sticks – to get hospitals and doctors to improve quality and lower costs. Some of the programs levy financial penalties on hospitals but affect the day-to-day work of hospitalists, while others affect physicians at the individual level.
"There’s a lot of confusion and lack of knowledge about what’s occurring at the physician level and what’s occurring at the hospital level," said Dr. Patrick J. Torcson, a member of the board of directors of the Society of Hospital Medicine (SHM) and director of hospital medicine at St. Tammany Parish Hospital in Covington, La.
Carrots, sticks for hospitalists
Two programs will touch hospitalists – and their wallets – directly. Medicare’s Physician Quality Reporting System (PQRS), a voluntary pay-for-reporting program, has been around since 2007 offering small incentives for participation, but it will soon begin penalizing physicians who don’t report on quality. Officials at the Centers for Medicare and Medicaid Services (CMS) are also phasing in the physician value-based modifier, which will begin adjusting physician payments up or down depending on the quality and cost of the care they provide.
CMS will use PQRS reporting as the basis for the new modifier, making participation in the older program a top priority for all physicians, Dr. Torcson said.
This year, physicians who successfully report quality measures through PQRS can earn a 0.5% bonus on their total allowable Medicare Part B charges. The same bonus will be in place for 2014. But starting in 2015, Medicare will assess a 1.5% penalty on physicians who fail to report successfully. That payment penalty increases to 2% in 2016.
But the PQRS has been criticized as being cumbersome and not especially relevant for hospitalists.
"I think many physicians hoped it would go away," Dr. Torcson said. "It hasn’t. It has expanded."
Hospitalists are currently required to report on at least three quality measures through the program. But Medicare is proposing to require physicians to report on at least nine measures starting in 2014. CMS will issue a final regulation outlining changes to the PQRS in November.
The SHM has recommended instead that CMS limit the expansion to no more than six quality measures to keep from ramping up the program too fast.
In comments to the agency, SHM also noted that the PQRS quality measures, while improving, still do not accurately reflect the scope of care provided by hospitalists. For instance, about half of the measures that hospitalists can report on are related to stroke care, though stoke care is not a primary practice focus for many hospital medicine programs.
Many hospitalists have ignored the PQRS so far, Dr. Torcson said, because the added time and effort of reporting on quality measures outweighed the value of the 0.5% bonus, on average about $500 per physician. But he urged physicians to rethink participation in light of the rollout of the new value-based modifier program.
Value-based modifier coming soon
The physician value-based payment modifier was part of the 2008 Medicare Improvement for Patients and Providers Act and was expanded as part of the 2010 Affordable Care Act. The program seeks to pay physicians more for providing high-quality, low-cost care. But the budget-neutral program will pay less for low-quality, high-cost care. Physician groups could see payment cuts of between 1% and 2% in 2016, based on their performance. Physicians who don’t report on quality measures through the PQRS will get an automatic 1% pay cut under the value-based modifier program.
The value-based modifier already is affecting physicians who work in groups of 100 or more eligible providers. While payments won’t be affected until 2015, CMS will base its adjustments on the data reported to the PQRS in 2013. The program will expand to cover physician groups of 10 or more in 2016, though the measurement on cost and quality will occur in 2014. Payments for all physicians will be subject to the modifier by 2017, based on performance during 2015.
"Physician-level pay for reporting is well underway and now actual pay for performance is here," Dr. Torcson said. "Engagement, familiarity, and participation in the PQRS is really going to be the key for physicians. It’s not too late."
CMS is providing some tools to help physicians understand their performance on cost and quality. The agency is producing annual Quality and Resource Use Reports (QRURs) that will show the individual physician’s past performance on the measures chosen by CMS. The reports are scheduled to go out to groups of 25 or more eligible professionals this fall. All physicians should start receiving the reports sometime in 2014.
But hospitalists should look closely at their reports, Dr. Torcson said. CMS is still figuring out how to classify the work done by hospitalists. Currently, CMS compares hospitalists’ cost and quality data to general internists even though hospitalized patients have a very different quality and cost profile.
"That’s something where there are still ongoing focused advocacy efforts by SHM to make sure that the attribution and the measurement methodology takes into account the hospitalist model," he said.
Hospitals under pressure, too
But hospitalists have more them just themselves to worry about. Often it’s the hospitalist who is the point person for quality and efficiency in their institution. And Medicare has an array of hospital-focused carrots and sticks, as well.
The hospital value-based purchasing program is already in full swing. For fiscal year 2014, which begins in October 2013, hospitals will have 1.25% of their base operating charges at risk in the program. The program bases payment on a group of clinical process measures, patient satisfaction, and selected mortality measures.
Additionally, Medicare is doubling the maximum penalties for its from 1% to 2% of base operating payments starting this month. The penalties apply to hospitals that have excess 30-day readmissions for pneumonia, heart failure, and acute myocardial infarction. CMS is also expected to add more conditions to the list. Total hip and Hospital Readmissions Reduction Program knee arthroplasty and chronic obstructive pulmonary disease will be added to the list of conditions in October 2014.
CMS is also launching a new Hospital-Acquired Condition (HAC) Reduction Program in October 2014. In this program, which was authorized under the Affordable Care Act, hospitals with the most HACs will see their payments reduced by 1%. During the first year, hospitals will be judged based on several indicators including:
• Pressure ulcer rate.
• Iatrogenic pneumothorax rate.
• Central venous catheter–related blood stream infection rate.
• Postoperative hip fracture rate.
• Postoperative pulmonary embolism or deep vein thrombosis rate.
• Postoperative sepsis rate.
• Wound dehiscence rate.
• Accidental puncture and laceration rate.
• Central line–associated blood stream infection.
• Catheter-associated urinary tract infection.
• Hospitals’ scores will be risk adjusted based on age, sex, and comorbidities.
More regulatory changes
CMS is also making some changes that will impact how hospitalists admit patients. Over the summer, Medicare officials issued a regulation that changes the criteria for when to admit a patient to hospital, as covered under Medicare Part A, and when to place them under observation status under Part B. The new criteria are based on the amount of time the physician expects the patient to spend as an inpatient.
Starting on Oct. 1, 2013, Medicare contractors will assume that a hospital stay is covered under Part A if the physician expects the patient to stay as an inpatient in the hospital for at least 2 midnights. CMS also emphasized in the rule that the inpatient stay does not begin until the patient is formally admitted by a physician.
What can hospitalists do to prepare?
While new regulatory requirements continue to hit hospitals year after year, Dr. Torcson said hospitalists are well prepared to handle the changes.
"The whole purpose and success and value of hospitalists is being the physician champions for the hospital-level performance agenda around core measures, readmissions, hospital-acquired conditions, and medical necessity documentation," he said. "That’s something that hospitalists have been preparing for from day 1, going back to the ’90s."
He urged hospitalists to redouble their efforts as hospital champions for quality.
"Concentrating on the hospital-level performance agenda is really going to be the key for hospital medicine programs to continue to be successful," Dr. Torcson said.
On Twitter @MaryEllenNY
October marks the start of a new fiscal year for the federal government and with it comes a host of new and revised regulatory requirements for hospitalists and hospitals.
Medicare officials are using some carrots – but mostly sticks – to get hospitals and doctors to improve quality and lower costs. Some of the programs levy financial penalties on hospitals but affect the day-to-day work of hospitalists, while others affect physicians at the individual level.
"There’s a lot of confusion and lack of knowledge about what’s occurring at the physician level and what’s occurring at the hospital level," said Dr. Patrick J. Torcson, a member of the board of directors of the Society of Hospital Medicine (SHM) and director of hospital medicine at St. Tammany Parish Hospital in Covington, La.
Carrots, sticks for hospitalists
Two programs will touch hospitalists – and their wallets – directly. Medicare’s Physician Quality Reporting System (PQRS), a voluntary pay-for-reporting program, has been around since 2007 offering small incentives for participation, but it will soon begin penalizing physicians who don’t report on quality. Officials at the Centers for Medicare and Medicaid Services (CMS) are also phasing in the physician value-based modifier, which will begin adjusting physician payments up or down depending on the quality and cost of the care they provide.
CMS will use PQRS reporting as the basis for the new modifier, making participation in the older program a top priority for all physicians, Dr. Torcson said.
This year, physicians who successfully report quality measures through PQRS can earn a 0.5% bonus on their total allowable Medicare Part B charges. The same bonus will be in place for 2014. But starting in 2015, Medicare will assess a 1.5% penalty on physicians who fail to report successfully. That payment penalty increases to 2% in 2016.
But the PQRS has been criticized as being cumbersome and not especially relevant for hospitalists.
"I think many physicians hoped it would go away," Dr. Torcson said. "It hasn’t. It has expanded."
Hospitalists are currently required to report on at least three quality measures through the program. But Medicare is proposing to require physicians to report on at least nine measures starting in 2014. CMS will issue a final regulation outlining changes to the PQRS in November.
The SHM has recommended instead that CMS limit the expansion to no more than six quality measures to keep from ramping up the program too fast.
In comments to the agency, SHM also noted that the PQRS quality measures, while improving, still do not accurately reflect the scope of care provided by hospitalists. For instance, about half of the measures that hospitalists can report on are related to stroke care, though stoke care is not a primary practice focus for many hospital medicine programs.
Many hospitalists have ignored the PQRS so far, Dr. Torcson said, because the added time and effort of reporting on quality measures outweighed the value of the 0.5% bonus, on average about $500 per physician. But he urged physicians to rethink participation in light of the rollout of the new value-based modifier program.
Value-based modifier coming soon
The physician value-based payment modifier was part of the 2008 Medicare Improvement for Patients and Providers Act and was expanded as part of the 2010 Affordable Care Act. The program seeks to pay physicians more for providing high-quality, low-cost care. But the budget-neutral program will pay less for low-quality, high-cost care. Physician groups could see payment cuts of between 1% and 2% in 2016, based on their performance. Physicians who don’t report on quality measures through the PQRS will get an automatic 1% pay cut under the value-based modifier program.
The value-based modifier already is affecting physicians who work in groups of 100 or more eligible providers. While payments won’t be affected until 2015, CMS will base its adjustments on the data reported to the PQRS in 2013. The program will expand to cover physician groups of 10 or more in 2016, though the measurement on cost and quality will occur in 2014. Payments for all physicians will be subject to the modifier by 2017, based on performance during 2015.
"Physician-level pay for reporting is well underway and now actual pay for performance is here," Dr. Torcson said. "Engagement, familiarity, and participation in the PQRS is really going to be the key for physicians. It’s not too late."
CMS is providing some tools to help physicians understand their performance on cost and quality. The agency is producing annual Quality and Resource Use Reports (QRURs) that will show the individual physician’s past performance on the measures chosen by CMS. The reports are scheduled to go out to groups of 25 or more eligible professionals this fall. All physicians should start receiving the reports sometime in 2014.
But hospitalists should look closely at their reports, Dr. Torcson said. CMS is still figuring out how to classify the work done by hospitalists. Currently, CMS compares hospitalists’ cost and quality data to general internists even though hospitalized patients have a very different quality and cost profile.
"That’s something where there are still ongoing focused advocacy efforts by SHM to make sure that the attribution and the measurement methodology takes into account the hospitalist model," he said.
Hospitals under pressure, too
But hospitalists have more them just themselves to worry about. Often it’s the hospitalist who is the point person for quality and efficiency in their institution. And Medicare has an array of hospital-focused carrots and sticks, as well.
The hospital value-based purchasing program is already in full swing. For fiscal year 2014, which begins in October 2013, hospitals will have 1.25% of their base operating charges at risk in the program. The program bases payment on a group of clinical process measures, patient satisfaction, and selected mortality measures.
Additionally, Medicare is doubling the maximum penalties for its from 1% to 2% of base operating payments starting this month. The penalties apply to hospitals that have excess 30-day readmissions for pneumonia, heart failure, and acute myocardial infarction. CMS is also expected to add more conditions to the list. Total hip and Hospital Readmissions Reduction Program knee arthroplasty and chronic obstructive pulmonary disease will be added to the list of conditions in October 2014.
CMS is also launching a new Hospital-Acquired Condition (HAC) Reduction Program in October 2014. In this program, which was authorized under the Affordable Care Act, hospitals with the most HACs will see their payments reduced by 1%. During the first year, hospitals will be judged based on several indicators including:
• Pressure ulcer rate.
• Iatrogenic pneumothorax rate.
• Central venous catheter–related blood stream infection rate.
• Postoperative hip fracture rate.
• Postoperative pulmonary embolism or deep vein thrombosis rate.
• Postoperative sepsis rate.
• Wound dehiscence rate.
• Accidental puncture and laceration rate.
• Central line–associated blood stream infection.
• Catheter-associated urinary tract infection.
• Hospitals’ scores will be risk adjusted based on age, sex, and comorbidities.
More regulatory changes
CMS is also making some changes that will impact how hospitalists admit patients. Over the summer, Medicare officials issued a regulation that changes the criteria for when to admit a patient to hospital, as covered under Medicare Part A, and when to place them under observation status under Part B. The new criteria are based on the amount of time the physician expects the patient to spend as an inpatient.
Starting on Oct. 1, 2013, Medicare contractors will assume that a hospital stay is covered under Part A if the physician expects the patient to stay as an inpatient in the hospital for at least 2 midnights. CMS also emphasized in the rule that the inpatient stay does not begin until the patient is formally admitted by a physician.
What can hospitalists do to prepare?
While new regulatory requirements continue to hit hospitals year after year, Dr. Torcson said hospitalists are well prepared to handle the changes.
"The whole purpose and success and value of hospitalists is being the physician champions for the hospital-level performance agenda around core measures, readmissions, hospital-acquired conditions, and medical necessity documentation," he said. "That’s something that hospitalists have been preparing for from day 1, going back to the ’90s."
He urged hospitalists to redouble their efforts as hospital champions for quality.
"Concentrating on the hospital-level performance agenda is really going to be the key for hospital medicine programs to continue to be successful," Dr. Torcson said.
On Twitter @MaryEllenNY