User login
Negotiating salaries. Improving patient flow. Increasing patient satisfaction. Reducing readmissions. Championing quality improvement efforts. Planning strategically. Handling schedule issues. Dealing with coverage issues. Working on Ebola preparation. Being on call 24 hours a day for an urgent concern from hospital administration or a hospitalist.
Hospitalist group leaders often feel they are pulled in multiple directions all at once and find that a day off really is not a day off. Leaders often are asked to take on additional responsibilities and might wonder whether they are given sufficient protected time. Leaders of larger HM groups might ask whether adding an associate chief would help cover the administrative workload. Or they may be asking whether hospitalist group leaders should receive a premium in salary, above that of other hospitalists in the group.
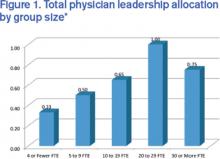
These are questions the State of Hospital Medicine Report (SOHM) attempts to answer. Although there is significant variation that is dependent on many factors (i.e., group size, academic status, and whether or not the practice is part of a larger multi-site group), the 2014 SOHM found that the median total full-time equivalent (FTE) allocation for physician administration/leadership for HMGs serving adults was just 0.60. The highest-ranking physician leader most commonly had 0.25 to 0.35 FTE protected for administrative responsibilities. And the median compensation premium for group leaders was 15%.
One leadership challenge is that administrative work never stops. Group leaders often find themselves having to come in for meetings before or after night shifts. Leaders sometimes feel that the 0.30 FTE allocated for administrative responsibilities actually requires the workload of a full-time position. Yet, like other hospitalists, leaders typically work a significant number of consecutive clinical shifts to ensure continuity of care for patients, which can make juggling administrative work challenging.
Additionally, group leaders often carry a significant clinical workload. (Read about Team Hospitalist’s newest member and her split leadership-clinical roles) I would argue that this is a good thing, important for many reasons, including maintaining clinical skills, understanding the nature of work and challenges on the front lines, and being able to facilitate quality improvement efforts. Further, group leaders often are perceived to be team players by other hospitalists when they work a wide variety of shifts on all days of the week. Many programs face staffing challenges, and leaders might work extra shifts when other hospitalists are unable to fill them.
Certainly group leaders face significant challenges, but the position also comes with many rewards. Satisfaction comes from improving the program for all hospitalists in a group, from gains in hospital efficiency or flow, from systems improvements to ensure patient safety or improve patient outcomes, and from being respected by hospital administration as well as other hospitalists in the group. With a good understanding of hospital finances and patient flow, some hospitalist group leaders advance to other roles in hospital administration, such as CMO or CEO.
Although there may be no one-size-fits-all answer for the right amount of protected time or salary for group leaders, leaders clearly play a challenging but essential role in bringing value to both hospitals and hospitalist groups.
For more data from the 2014 State of Hospital Medicine Report, visit www.hospitalmedicine.org/survey.

Dr. Huang is associate chief of the division of hospital medicine and associate clinical professor at the University of California San Diego. He is a member of SHM’s Practice Analysis Committee.
Negotiating salaries. Improving patient flow. Increasing patient satisfaction. Reducing readmissions. Championing quality improvement efforts. Planning strategically. Handling schedule issues. Dealing with coverage issues. Working on Ebola preparation. Being on call 24 hours a day for an urgent concern from hospital administration or a hospitalist.
Hospitalist group leaders often feel they are pulled in multiple directions all at once and find that a day off really is not a day off. Leaders often are asked to take on additional responsibilities and might wonder whether they are given sufficient protected time. Leaders of larger HM groups might ask whether adding an associate chief would help cover the administrative workload. Or they may be asking whether hospitalist group leaders should receive a premium in salary, above that of other hospitalists in the group.
These are questions the State of Hospital Medicine Report (SOHM) attempts to answer. Although there is significant variation that is dependent on many factors (i.e., group size, academic status, and whether or not the practice is part of a larger multi-site group), the 2014 SOHM found that the median total full-time equivalent (FTE) allocation for physician administration/leadership for HMGs serving adults was just 0.60. The highest-ranking physician leader most commonly had 0.25 to 0.35 FTE protected for administrative responsibilities. And the median compensation premium for group leaders was 15%.
One leadership challenge is that administrative work never stops. Group leaders often find themselves having to come in for meetings before or after night shifts. Leaders sometimes feel that the 0.30 FTE allocated for administrative responsibilities actually requires the workload of a full-time position. Yet, like other hospitalists, leaders typically work a significant number of consecutive clinical shifts to ensure continuity of care for patients, which can make juggling administrative work challenging.
Additionally, group leaders often carry a significant clinical workload. (Read about Team Hospitalist’s newest member and her split leadership-clinical roles) I would argue that this is a good thing, important for many reasons, including maintaining clinical skills, understanding the nature of work and challenges on the front lines, and being able to facilitate quality improvement efforts. Further, group leaders often are perceived to be team players by other hospitalists when they work a wide variety of shifts on all days of the week. Many programs face staffing challenges, and leaders might work extra shifts when other hospitalists are unable to fill them.
Certainly group leaders face significant challenges, but the position also comes with many rewards. Satisfaction comes from improving the program for all hospitalists in a group, from gains in hospital efficiency or flow, from systems improvements to ensure patient safety or improve patient outcomes, and from being respected by hospital administration as well as other hospitalists in the group. With a good understanding of hospital finances and patient flow, some hospitalist group leaders advance to other roles in hospital administration, such as CMO or CEO.
Although there may be no one-size-fits-all answer for the right amount of protected time or salary for group leaders, leaders clearly play a challenging but essential role in bringing value to both hospitals and hospitalist groups.
For more data from the 2014 State of Hospital Medicine Report, visit www.hospitalmedicine.org/survey.

Dr. Huang is associate chief of the division of hospital medicine and associate clinical professor at the University of California San Diego. He is a member of SHM’s Practice Analysis Committee.
Negotiating salaries. Improving patient flow. Increasing patient satisfaction. Reducing readmissions. Championing quality improvement efforts. Planning strategically. Handling schedule issues. Dealing with coverage issues. Working on Ebola preparation. Being on call 24 hours a day for an urgent concern from hospital administration or a hospitalist.
Hospitalist group leaders often feel they are pulled in multiple directions all at once and find that a day off really is not a day off. Leaders often are asked to take on additional responsibilities and might wonder whether they are given sufficient protected time. Leaders of larger HM groups might ask whether adding an associate chief would help cover the administrative workload. Or they may be asking whether hospitalist group leaders should receive a premium in salary, above that of other hospitalists in the group.
These are questions the State of Hospital Medicine Report (SOHM) attempts to answer. Although there is significant variation that is dependent on many factors (i.e., group size, academic status, and whether or not the practice is part of a larger multi-site group), the 2014 SOHM found that the median total full-time equivalent (FTE) allocation for physician administration/leadership for HMGs serving adults was just 0.60. The highest-ranking physician leader most commonly had 0.25 to 0.35 FTE protected for administrative responsibilities. And the median compensation premium for group leaders was 15%.
One leadership challenge is that administrative work never stops. Group leaders often find themselves having to come in for meetings before or after night shifts. Leaders sometimes feel that the 0.30 FTE allocated for administrative responsibilities actually requires the workload of a full-time position. Yet, like other hospitalists, leaders typically work a significant number of consecutive clinical shifts to ensure continuity of care for patients, which can make juggling administrative work challenging.
Additionally, group leaders often carry a significant clinical workload. (Read about Team Hospitalist’s newest member and her split leadership-clinical roles) I would argue that this is a good thing, important for many reasons, including maintaining clinical skills, understanding the nature of work and challenges on the front lines, and being able to facilitate quality improvement efforts. Further, group leaders often are perceived to be team players by other hospitalists when they work a wide variety of shifts on all days of the week. Many programs face staffing challenges, and leaders might work extra shifts when other hospitalists are unable to fill them.
Certainly group leaders face significant challenges, but the position also comes with many rewards. Satisfaction comes from improving the program for all hospitalists in a group, from gains in hospital efficiency or flow, from systems improvements to ensure patient safety or improve patient outcomes, and from being respected by hospital administration as well as other hospitalists in the group. With a good understanding of hospital finances and patient flow, some hospitalist group leaders advance to other roles in hospital administration, such as CMO or CEO.
Although there may be no one-size-fits-all answer for the right amount of protected time or salary for group leaders, leaders clearly play a challenging but essential role in bringing value to both hospitals and hospitalist groups.
For more data from the 2014 State of Hospital Medicine Report, visit www.hospitalmedicine.org/survey.

Dr. Huang is associate chief of the division of hospital medicine and associate clinical professor at the University of California San Diego. He is a member of SHM’s Practice Analysis Committee.