User login
CASE 1: Short cervix in the middle trimester
During routine second-trimester ultrasonography, a 34-year-old primigravida at 22 weeks’ gestation is found to have a cervix 15 mm in length. She has no other risk factors for spontaneous preterm birth.
What steps do you take to ensure that her pregnancy progresses uneventfully to term?
Cervical length is not routinely measured in low-risk women—i.e., those without a history of spontaneous preterm birth—but a short cervix is sometimes detected during ultrasonographic imaging for other indications, as it was in this case. When a short cervix is detected incidentally, I educate the patient to watch for early warning signs of preterm labor. I also recommend pelvic rest and a sedentary lifestyle.
The rate of preterm birth declined slightly in 2007—the first decrease in more than 20 years—but the phenomenon remains the leading cause of perinatal morbidity and mortality in developed nations.1 In the United States, more than 500,000 babies each year, or 12% to 13% of all births, are delivered before 37 weeks’ gestation. Most of these births are spontaneous and involve preterm labor or premature rupture of membranes. Medical costs for a preterm newborn exceed those of a term infant by a multiple of more than 10, and the average hospitalization exceeds that of a term infant by a multiple of more than six.
In this article, I discuss the rationale and technique for ultrasonographic cervical measurement to determine the likelihood of preterm birth. I also examine the data on the short cervix in various settings, and describe strategies for cervical assessment and preterm birth prevention, including cerclage and progesterone, framing the discussion in terms of gestational age.
Accurate and reproducible measurement of cervical length depends on correct technique. Use of transvaginal ultrasonography (TVUS) limits variations between measurements to 5% to 10%, a marked improvement over digital examination and transabdominal US.
Here are the five steps involved, in the order performed:
- Ensure that the patient’s bladder is empty. This precaution is necessary to prevent dynamic, or spontaneous, lengthening or shortening of the cervix.
- Counsel and position the patient. Explain the procedure to the patient and have her assume the dorsal lithotomy position.
- Introduce the probe into the anterior vaginal fornix using real-time visualization, and obtain a mid-sagittal view of the cervix. Withdraw the probe just enough to allow the image to blur, then advance the probe just enough for the image to regain clarity. This sequence prevents the practitioner from exerting excessive pressure on the cervix, which can falsely elongate it.
- Place an electronic caliper (on-screen) at the notch that represents the internal cervical os, and another at the external os (FIGURE 1).
- Measure the distance between the notches and report the shortest of three separately obtained measurements.
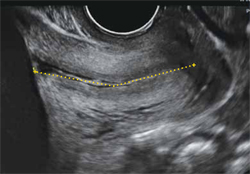
FIGURE 1 How to measure the cervix
Electronic calipers mark the internal and external os in this cervix measuring 42 mm via midsagittal transvaginal ultrasonography.
Watch for these pitfalls!
Before 20 weeks’ gestation, the lower uterine segment is not particularly well developed, making it difficult to reliably determine the location of the internal os (FIGURE 2). Moreover, focal myometrial contractions of the lower uterine segment, which are common, may give the false impression of increased cervical length or dilation of the internal os (FIGURE 2).24
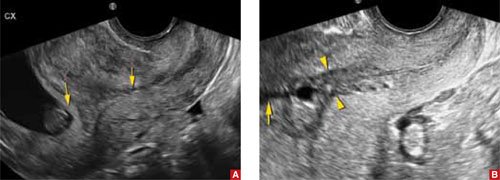
FIGURE 2 Measurement may be difficult in early pregnancy
A. This transvaginal sonogram demonstrates the difficulty of determining the location of the internal os when the lower uterine segment is undeveloped (arrows). B. When lower uterine contractions occur with the anterior and posterior walls in opposition (arrowheads), transvaginal imaging may give the false appearance of dilation with funneling (arrow).
Why we assess cervical length
In the past, the cervix was viewed as either competent—i.e., capable of maintaining a pregnancy until term—or as “incompetent.” More recent evidence has broadened our understanding of cervical function, which is now viewed along a continuum.
In landmark research in the mid-1990s, investigators compared cervical lengths, measured via transvaginal ultrasonography (TVUS), between two groups of pregnant women—those who had a history of preterm birth and those who did not.
The result? Gestational age at delivery in the first pregnancy correlated significantly—and continuously—with cervical length between 20 and 30 weeks’ gestation in the subsequent pregnancy.2 Investigators also observed that the risk of spontaneous preterm birth increased with decreasing cervical length. A length of 25 mm (10th percentile) offered a clinically appropriate threshold for identification of the risk of preterm delivery.3
The value of cervical-length measurement lies in its high negative predictive value for recurrent spontaneous preterm birth.4 As a general rule of thumb, routine assessment of cervical length in asymptomatic women who do not have a history of preterm birth is not recommended because of the high rate of false-positive results and the low positive predictive value for preterm delivery. We also lack an evidence-based consensus on how to manage an abnormally short cervix in these women.
CASE RESOLVED
The patient is counseled to watch for signs of preterm labor and to remain sedentary. Her pregnancy progresses without incident until 40 weeks, when she undergoes induction of labor for oligohydramnios and delivers a healthy infant weighing 3,855 g.
When a short cervix is detected at less than 20 weeks
If a woman has a history of spontaneous preterm birth, a short cervix this early in gestation raises the question of cervical insufficiency. No objective criteria have been devised to identify this condition. Nor is there a widely accepted definition. A reasonable description does exist, however:
- …a clinical diagnosis characterized by recurrent painless dilation and spontaneous midtrimester birth, generally in the absence of predisposing conditions such as spontaneous membrane rupture, bleeding, and infection, characteristics that shift the presumed underlying cause away from cervical incompetence and support other components of the preterm birth syndrome.5
A patient who fits this description may be a candidate for cervical cerclage. Alternatively, it is reasonable to reassess the patient in 3 to 7 days, after restricting physical activity, keeping in mind the pitfalls of TVUS assessment of the lower uterine segment in early gestation (see the box on imaging). If cervical length remains short, consider cerclage.6,7
Watch for inflammation
Occasionally, echogenic material is observed in the amniotic fluid at the level of a short cervix. This debris is an inflammatory exudate of fibrin, white blood cells, and bacteria. The presence of this sludge (FIGURE 3) signifies a risk of preterm birth much greater than that associated with a short cervix alone.8 Because cerclage in the presence of inflammation may further heighten the risk of spontaneous preterm birth, I recommend caution.

FIGURE 3 Watch for signs of inflammation
When inflammatory exudate (asterisk) is identified at the level of a short cervix, the risk of spontaneous preterm birth is elevated beyond the risk associated with a short cervix alone.
When a short cervix is detected between 20 and 24 weeks
CASE 2: Is recurrent preterm birth likely?
A 30-year-old woman 21 weeks pregnant with her second child reports for TVUS. Because her first child was delivered preterm at 30 weeks, she has been undergoing periodic measurement of her cervix. Until today, it has been longer than 25 mm, but now it is 20 mm. What is the best strategy to avert another preterm birth?
If a short cervix (<25 mm) is noted in a high-risk patient at this gestational age, consider the possibility of preterm labor and ruptured membranes. If these conditions are present, they should be managed according to existing guidelines.4,9 If they are absent, consider cerclage.
A recent meta-analysis of randomized trials of cerclage for the prevention of preterm birth in a singleton, high-risk pregnancy with a short cervix suggests that cerclage is associated with a significantly lower risk of delivery before 35 weeks’ gestation (relative risk [RR], 0.61; 95% confidence interval [CI], 0.40–0.92). Among singleton pregnancies involving both a short cervix and a history of midtrimester loss, cerclage is again associated with a reduced likelihood of delivery before 35 weeks (39% vs 23.4%; number needed to treat [NNT], 8; RR, 0.57; 95% CI, 0.33–0.99).10 A recent randomized trial of cerclage versus no cerclage in women who had a history of spontaneous preterm birth produced similar findings.11 This trial is described in detail in the box.
Another randomized trial compared the relative merits of ultrasound-indicated cerclage for a cervix shorter than 20 mm to a history-indicated cerclage among women with a prior spontaneous preterm birth between 16 and 34 weeks. Thirty-nine of 123 women randomized to the former group received a cerclage, as did 25 of 125 subjects in the latter group. There were no significant differences in the primary outcome of delivery before 34 weeks or secondary measures of loss before 24 weeks, preterm premature membrane rupture, mean gestational age at delivery, or neonatal outcomes. This study was not designed or powered to evaluate the efficacy of cerclage in preventing recurrent, spontaneous preterm birth. It simply compares two ways of selecting high-risk women for cerclage.12
We lack data supporting placement of cerclage for an incidentally detected short cervix in women who lack a history of spontaneous preterm birth or midtrimester loss.7
Other groups known to be at increased risk of spontaneous preterm birth include women carrying twins and women who have undergone cervical cone biopsy or loop electrosurgical excision procedure (LEEP). Among twin gestations, cerclage for a short cervix is associated with an increased rate of preterm birth (<35 weeks).10 Cerclage for a short cervix has not been evaluated among women who have a history of LEEP.6
CASE RESOLVED
After preterm labor is ruled out, the patient is counseled about her options and chooses cervical cerclage. Her pregnancy proceeds uneventfully until 36 weeks’ gestation, when she delivers a healthy infant weighing 2,950 g.
When a short cervix is detected between 24 and 34 weeks
CASE 3: Is it preterm labor?
A primigravida at 31 weeks’ gestation presents to the labor floor reporting regular contractions. She denies bleeding or rupture of membranes. Contractions are noted at 3-minute intervals, and digital cervical examination reveals that she is dilated 1 cm, with 70% effacement. TVUS determines cervical length to be 17 mm.
How should she be managed?
From 24 to 34 weeks’ gestation, the prevention, diagnosis, and treatment of preterm labor become the main concerns. Because our ability to predict and prevent preterm birth is limited, clinical management focuses on a reliable diagnosis of preterm labor to allow for selective, timely interventions to optimize neonatal outcomes. These interventions include tocolysis to permit maternal transport; antibiotic prophylaxis for group B strep; and steroid administration to accelerate fetal lung maturity. Equally important is the ability to reliably rule out preterm labor among symptomatic (contracting) women to avoid the potential morbidity, cost, and inconvenience of these interventions.
Before 37 weeks, a diagnosis of preterm labor requires the following findings:
- six or more contractions per hour
- cervical dilation, as identified by digital examination, of at least 3 cm and 80% effacement.
This diagnosis is more reliable when ruptured membranes or vaginal bleeding are present.
The significance of contractions without these findings is less clear. Therefore, we follow an algorithm that incorporates TVUS measurement of cervical length and evaluation of fetal fibronectin (fFN) (FIGURE 4).13
fFN is a glycoprotein that is normally confined to the extracellular matrix of the fetal membranes between 24 and 34 weeks’ gestation. Detection of fFN in cervicovaginal secretions during this window is associated with an increased risk of spontaneous preterm birth, whereas its absence demonstrates a negative predictive value for delivery within 7 days of testing of more than 97%.
During initial assessment of a regularly contracting preterm patient, perform a vaginal speculum examination. If the membranes are intact, use a vaginal swab to assess the patient for the presence of fFN, and set the specimen aside. Also obtain a culture for group B strep.
If a digital cervical examination and the contraction pattern establish a diagnosis of preterm labor, administer a tocolytic, When fetal prophylactic antibiotics, and steroids. If the diagnosis remains unclear, evaluate the cervix via TVUS. A cervical length above 30 mm effectively rules out preterm labor and obviates the need to send the fFN swab for assessment. As a result, the patient can be managed expectantly.
In contrast, a cervical length below 20 mm effectively confirms the diagnosis of preterm labor, and treatment can proceed. Again, the fFN swab may be discarded. The swab is sent for processing only if cervical length is 20 mm to 30 mm (FIGURE 4). A positive fFN result leads to the presumptive diagnosis of preterm labor, whereas a negative result permits expectant management.
We also recommend that women who display symptoms of preterm labor be screened for asymptomatic bacteriuria. Identification and treatment of this condition significantly reduce the risk of preterm delivery (RR, 0.56; 95% CI, 0.43–0.73).14 In addition, diagnosis and treatment of bacterial vaginosis in symptomatic women who have a history of spontaneous preterm birth can also reduce the risk of recurrent preterm delivery (RR, 0.42; 95% CI, 0.27–0.67).15
Not all obstetric care providers have the resources necessary for TVUS assessment of cervical length. When that is the case, fFN offers high sensitivity and negative predictive value and can help guide initial clinical decision-making. Keep in mind, however, that not all facilities offer fFN testing. In addition, in some cases, cervical manipulation may have occurred before fFN testing was performed, precluding its validity. In such cases, the incorporation of TVUS assessment of cervical length into clinical evaluation may help guide decision-making.

FIGURE 4 How to identify preterm labor at 24 to 34 weeks
CASE RESOLVED
The determination of short cervical length (17 mm) by TVUS confirms the diagnosis of preterm labor. The patient is admitted to the hospital and treated with a tocolytic, prophylactic antibiotics, and steroids. Three days later, preterm labor recurs, and she delivers an otherwise healthy infant. Future pregnancies will be managed according to the algorithm presented in FIGURE 5.
Cerclage may benefit women who have a history of spontaneous preterm birth
A recent multicenter randomized trial evaluated the efficacy of cerclage in preventing preterm birth among 302 women who had a history of spontaneous preterm birth before 34 weeks’ gestation.11 Any woman who had a cervix shorter than 25 mm between 16-0/7 and 22-6/7 weeks’ gestation was randomized to cerclage or no cerclage.
Cerclage did not significantly reduce preterm delivery before 35 weeks’ gestation, the primary outcome. Thirty-two percent of women who received cerclage and 42% of women who did not receive cerclage delivered before 35 weeks (P = .09). However, among women who had a cervix shorter than 15 mm at randomization, cerclage reduced the rate of delivery before 35 weeks by more than 75% (P = .006). Cerclage also reduced the rate of spontaneous birth before 37 weeks, compared with no cerclage (45% vs 60%; P = .01), as well as the rate of previable preterm birth before 24 weeks (6.1% vs 14%; P = .03) and the rate of perinatal death (8.8% vs 16%; P = .046).
As this study demonstrates, ultrasonographically indicated cerclage produces a number of highly clinically significant benefits in women who have a history of spontaneous preterm birth. Another important question is whether supplemental progesterone offers additional benefit beyond that conferred by cerclage in this population.
The role of progesterone in preventing preterm birth
CASE 4: History of preterm and term delivery
A woman in her third pregnancy is referred for placement of cervical cerclage, based on her obstetric history. Her first pregnancy was marked by preterm labor at 26 weeks, resulting in spontaneous preterm birth at 28 weeks. In her second pregnancy, she had cerclage placed electively at 13 weeks and delivered spontaneously at 40 weeks with no complications of pregnancy.
Is another cerclage indicated—or would progesterone be more effective?
Supplemental 17-hydroxyprogesterone caproate, given weekly in an intramuscular dosage of 250 mg, significantly reduced the rate of recurrent spontaneous preterm birth when it was administered from 16 to 36 weeks’ gestation in women carrying a singleton fetus.16 The protective effect of progesterone is most apparent in women who have a history of very preterm delivery (<32 weeks). No such benefit has been observed in twin and triplet gestations, however.17-19
Among women who do benefit from progesterone, the effect may vary. For this reason, researchers have explored the measurement of midtrimester cervical length as a means of stratifying response to progesterone.
For example, investigators randomized women who had a history of spontaneous preterm birth to daily treatment with 90 mg of vaginal progesterone gel or placebo, starting between 16 and 22-6/7 weeks and continuing until 37 weeks or delivery, whichever came first. No difference in the rate of delivery at or before 32 weeks was observed. However, a secondary analysis among progesterone-treated women who had a cervical length below 28 mm found significant declines in the rate of delivery at or before 32 weeks, admission to a NICU, and length of stay.20,21
In another trial, investigators assessed cervical length via TVUS between 20 and 25 weeks’ gestation in a general obstetric population that included women carrying twins. Women who had a cervical length below 15 mm were offered randomization to daily oral progesterone (200 mg) or placebo from 24 weeks to 33-6/7 weeks’ gestation. The rate of spontaneous preterm birth was significantly lower in the progesterone group (19% vs 34%).22
Because the ideal formulation of progesterone for the prevention of preterm birth is unknown, ACOG recommends restricting its use to women who have a documented history of spontaneous preterm birth at less than 37 weeks’ gestation.23 My practice follows the protocol of Meis and colleagues within the framework of an overall systematic algorithm (FIGURE 5).

FIGURE 5 Cervical length in the second trimester
*For a singleton gestation only.
CASE RESOLVED
The ObGyn reviews the patient’s obstetric history and determines that the first pregnancy was more suggestive of preterm labor than cervical insufficiency. Therefore, the ObGyn opts for progesterone rather than cerclage to prolong the gestation. The patient begins weekly injections of 17-hydroxyprogesterone caproate, starting at 16 weeks’ gestation, with TVUS measurement of cervical length every 2 weeks. The cervix remains longer than 25 mm through 24 weeks’ gestation, at which time TVUS assessment is stopped. Progesterone injections continue through 36 weeks, and the patient spontaneously delivers a healthy 3,700-g infant at term.
1. Hamilton BE, Martin JA, Ventura SJ. Births: Preliminary data for 2007. National vital statistics reports; 2009;57(12). National Center for Health Statistics Web site. http://www.cdc.gov/nchs/data/nvsr/nvsr57/nvsr57_12.pdf. March 18, 2009. Accessed March 30, 2010.
2. Iams JD, Johnson FF, Sonek J, et al. Cervical competence as a continuum: a study of ultrasonographic cervical length and obstetric performance. Am J Obstet Gynecol. 1995;172(4 pt 1):1097-1106.
3. Iams JD, Goldenberg RL, Meis PJ, et al. The length of the cervix and the risk of spontaneous premature delivery. National Institute of Child Health and Human Development Maternal Fetal Medicine Unit Network. N Engl J Med. 1996;334(9):567-572.
4. Clinical Management Guidelines for Obstetrician-Gynecologists. No. 43, May 2003: Management of Preterm Labor. Obstet Gynecol. 2003;101(5 pt 1):1039-1047.
5. Owen J, Iams JD, Hauth JC. Vaginal sonography and cervical incompetence. Am J Obstet Gynecol. 2003;188(2):586-596.
6. Harger JH. Cerclage and cervical insufficiency: an evidence-based analysis. Obstet Gynecol. 2002;100(6):1313-1327.
7. Clinical Management Guidelines for Obstetrician-Gynecologists. No. 48, Nov 2003: Cervical insufficiency. Obstet Gynecol. 2003;102(5 pt 1):1091-1099.
8. Kusanovic JP, Espinoza J, Romero R, et al. Clinical significance of the presence of amniotic fluid ‘sludge’ in asymptomatic patients at high risk for spontaneous preterm delivery. Ultrasound Obstet Gynecol. 2007;30(5):706-714.
9. ACOG Practice Bulletin No. 80. Premature rupture of membranes. Obstet Gynecol. 2007;109(4):1007-1020.DOI:10.1097/01.AOG.0000263888.69178.1f.
10. Berghella V, Odibo AO, To MS, Rust OA, Althuisius SM. Cerclage for short cervix on ultrasonography: meta-analysis of trials using individual patient-level data. Obstet Gynecol. 2005;106(1):181-189.
11. Owen J, Hankins G, Iams JD, et al. Multicenter randomized trial of cerclage for preterm birth prevention in high-risk women with shortened mid-trimester cervical length. Am J Obstet Gynecol. 2009;201(4):375.e1-e8.
12. Simcox R, Seed PT, Bennett P, Teoh TG, Poston L, Shennan AH. A randomized control trial of cervical scanning vs history to determine cerclage in women at high risk of preterm birth (CIRCLE trial). Am J Obstet Gynecol. 2009;200(6):623.e1-e6.
13. Iams JD. Prediction and early detection of preterm labor. Obstet Gynecol. 2003;101(2):402-412.
14. Romero R, Oyarzun E, Mazor M, Sirtori M, Hobbins JC, Bracken M. Meta-analysis of the relationship between asymptomatic bacteriuria and preterm delivery/low birth weight. Obstet Gynecol. 1989;73(4):576-582.
15. Leitich H, Brunbauer M, Bodnar-Aderl B, Kaider A, Egarter C, Husslein P. Antibiotic treatment of bacterial vaginosis in pregnancy: a meta-analysis. Am J Obstet Gynecol. 2003;188(3):752-758.
16. Meis PJ, Klebanoff M, Thom E, et al. For National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Prevention of recurrent preterm birth by 17 alpha-hydroxyprogesterone caproate. N Engl J Med. 2003;348(24):2379-2385.
17. Norman JE, Mackenzie F, Owen P, et al. Progesterone for the prevention of preterm birth in twin pregnancy (STOPPIT): a randomised, double-blind, placebo-controlled study and meta-analysis. Lancet. 2009;373(9680):2034-2040.
18. Rouse DJ, Caritis SN, Peaceman AM, et al. For National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. A trial of 17 alpha-hydroxyprogesterone caproate to prevent prematurity in twins. N Engl J Med. 2007;357(5):454-461.
19. Caritis SN, Rouse DJ, Peaceman AM, et al. for Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), Medicine Units Network (MFMU). Prevention of preterm birth in triplets using 17 alpha-hydroxyprogesterone caproate: a randomized controlled trial. Obstet Gynecol. 2009;113(2 pt 1):285-292.
20. O’Brien JM, Adair CD, Lewis DF, et al. Progesterone vaginal gel for the reduction of recurrent preterm birth: primary results from a randomized, double-blind, placebo-controlled trial. Ultrasound Obstet Gynecol. 2007;30(5):687-696.
21. DeFranco EA, O’Brien JM, Adair CD, et al. Vaginal progesterone is associated with a decrease in risk for early preterm birth and improved neonatal outcome in women with a short cervix: a secondary analysis from a randomized, double-blind, placebo-controlled trial. Ultrasound Obstet Gynecol. 2007;30(5):697-705.
22. Fonseca EB, Celik E, Parra M, et al. For Fetal Medicine Foundation Second Trimester Screening Group. Progesterone and the risk of preterm birth among women with a short cervix. N Engl J Med. 2007;357(5):462-469.
23. ACOG Committee Opinion No. 419: Use of progesterone to reduce preterm birth. Obstet Gynecol. 2008;112(4):963.-
24. Yost NP, Bloom SL, Twickler DM, Leveno KJ. Pitfalls in ultrasonic cervical length measurement for predicting preterm birth. Obstet Gynecol. 1999;93(4):510-516.
CASE 1: Short cervix in the middle trimester
During routine second-trimester ultrasonography, a 34-year-old primigravida at 22 weeks’ gestation is found to have a cervix 15 mm in length. She has no other risk factors for spontaneous preterm birth.
What steps do you take to ensure that her pregnancy progresses uneventfully to term?
Cervical length is not routinely measured in low-risk women—i.e., those without a history of spontaneous preterm birth—but a short cervix is sometimes detected during ultrasonographic imaging for other indications, as it was in this case. When a short cervix is detected incidentally, I educate the patient to watch for early warning signs of preterm labor. I also recommend pelvic rest and a sedentary lifestyle.
The rate of preterm birth declined slightly in 2007—the first decrease in more than 20 years—but the phenomenon remains the leading cause of perinatal morbidity and mortality in developed nations.1 In the United States, more than 500,000 babies each year, or 12% to 13% of all births, are delivered before 37 weeks’ gestation. Most of these births are spontaneous and involve preterm labor or premature rupture of membranes. Medical costs for a preterm newborn exceed those of a term infant by a multiple of more than 10, and the average hospitalization exceeds that of a term infant by a multiple of more than six.
In this article, I discuss the rationale and technique for ultrasonographic cervical measurement to determine the likelihood of preterm birth. I also examine the data on the short cervix in various settings, and describe strategies for cervical assessment and preterm birth prevention, including cerclage and progesterone, framing the discussion in terms of gestational age.
Accurate and reproducible measurement of cervical length depends on correct technique. Use of transvaginal ultrasonography (TVUS) limits variations between measurements to 5% to 10%, a marked improvement over digital examination and transabdominal US.
Here are the five steps involved, in the order performed:
- Ensure that the patient’s bladder is empty. This precaution is necessary to prevent dynamic, or spontaneous, lengthening or shortening of the cervix.
- Counsel and position the patient. Explain the procedure to the patient and have her assume the dorsal lithotomy position.
- Introduce the probe into the anterior vaginal fornix using real-time visualization, and obtain a mid-sagittal view of the cervix. Withdraw the probe just enough to allow the image to blur, then advance the probe just enough for the image to regain clarity. This sequence prevents the practitioner from exerting excessive pressure on the cervix, which can falsely elongate it.
- Place an electronic caliper (on-screen) at the notch that represents the internal cervical os, and another at the external os (FIGURE 1).
- Measure the distance between the notches and report the shortest of three separately obtained measurements.
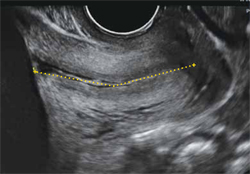
FIGURE 1 How to measure the cervix
Electronic calipers mark the internal and external os in this cervix measuring 42 mm via midsagittal transvaginal ultrasonography.
Watch for these pitfalls!
Before 20 weeks’ gestation, the lower uterine segment is not particularly well developed, making it difficult to reliably determine the location of the internal os (FIGURE 2). Moreover, focal myometrial contractions of the lower uterine segment, which are common, may give the false impression of increased cervical length or dilation of the internal os (FIGURE 2).24
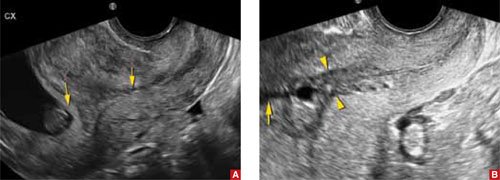
FIGURE 2 Measurement may be difficult in early pregnancy
A. This transvaginal sonogram demonstrates the difficulty of determining the location of the internal os when the lower uterine segment is undeveloped (arrows). B. When lower uterine contractions occur with the anterior and posterior walls in opposition (arrowheads), transvaginal imaging may give the false appearance of dilation with funneling (arrow).
Why we assess cervical length
In the past, the cervix was viewed as either competent—i.e., capable of maintaining a pregnancy until term—or as “incompetent.” More recent evidence has broadened our understanding of cervical function, which is now viewed along a continuum.
In landmark research in the mid-1990s, investigators compared cervical lengths, measured via transvaginal ultrasonography (TVUS), between two groups of pregnant women—those who had a history of preterm birth and those who did not.
The result? Gestational age at delivery in the first pregnancy correlated significantly—and continuously—with cervical length between 20 and 30 weeks’ gestation in the subsequent pregnancy.2 Investigators also observed that the risk of spontaneous preterm birth increased with decreasing cervical length. A length of 25 mm (10th percentile) offered a clinically appropriate threshold for identification of the risk of preterm delivery.3
The value of cervical-length measurement lies in its high negative predictive value for recurrent spontaneous preterm birth.4 As a general rule of thumb, routine assessment of cervical length in asymptomatic women who do not have a history of preterm birth is not recommended because of the high rate of false-positive results and the low positive predictive value for preterm delivery. We also lack an evidence-based consensus on how to manage an abnormally short cervix in these women.
CASE RESOLVED
The patient is counseled to watch for signs of preterm labor and to remain sedentary. Her pregnancy progresses without incident until 40 weeks, when she undergoes induction of labor for oligohydramnios and delivers a healthy infant weighing 3,855 g.
When a short cervix is detected at less than 20 weeks
If a woman has a history of spontaneous preterm birth, a short cervix this early in gestation raises the question of cervical insufficiency. No objective criteria have been devised to identify this condition. Nor is there a widely accepted definition. A reasonable description does exist, however:
- …a clinical diagnosis characterized by recurrent painless dilation and spontaneous midtrimester birth, generally in the absence of predisposing conditions such as spontaneous membrane rupture, bleeding, and infection, characteristics that shift the presumed underlying cause away from cervical incompetence and support other components of the preterm birth syndrome.5
A patient who fits this description may be a candidate for cervical cerclage. Alternatively, it is reasonable to reassess the patient in 3 to 7 days, after restricting physical activity, keeping in mind the pitfalls of TVUS assessment of the lower uterine segment in early gestation (see the box on imaging). If cervical length remains short, consider cerclage.6,7
Watch for inflammation
Occasionally, echogenic material is observed in the amniotic fluid at the level of a short cervix. This debris is an inflammatory exudate of fibrin, white blood cells, and bacteria. The presence of this sludge (FIGURE 3) signifies a risk of preterm birth much greater than that associated with a short cervix alone.8 Because cerclage in the presence of inflammation may further heighten the risk of spontaneous preterm birth, I recommend caution.

FIGURE 3 Watch for signs of inflammation
When inflammatory exudate (asterisk) is identified at the level of a short cervix, the risk of spontaneous preterm birth is elevated beyond the risk associated with a short cervix alone.
When a short cervix is detected between 20 and 24 weeks
CASE 2: Is recurrent preterm birth likely?
A 30-year-old woman 21 weeks pregnant with her second child reports for TVUS. Because her first child was delivered preterm at 30 weeks, she has been undergoing periodic measurement of her cervix. Until today, it has been longer than 25 mm, but now it is 20 mm. What is the best strategy to avert another preterm birth?
If a short cervix (<25 mm) is noted in a high-risk patient at this gestational age, consider the possibility of preterm labor and ruptured membranes. If these conditions are present, they should be managed according to existing guidelines.4,9 If they are absent, consider cerclage.
A recent meta-analysis of randomized trials of cerclage for the prevention of preterm birth in a singleton, high-risk pregnancy with a short cervix suggests that cerclage is associated with a significantly lower risk of delivery before 35 weeks’ gestation (relative risk [RR], 0.61; 95% confidence interval [CI], 0.40–0.92). Among singleton pregnancies involving both a short cervix and a history of midtrimester loss, cerclage is again associated with a reduced likelihood of delivery before 35 weeks (39% vs 23.4%; number needed to treat [NNT], 8; RR, 0.57; 95% CI, 0.33–0.99).10 A recent randomized trial of cerclage versus no cerclage in women who had a history of spontaneous preterm birth produced similar findings.11 This trial is described in detail in the box.
Another randomized trial compared the relative merits of ultrasound-indicated cerclage for a cervix shorter than 20 mm to a history-indicated cerclage among women with a prior spontaneous preterm birth between 16 and 34 weeks. Thirty-nine of 123 women randomized to the former group received a cerclage, as did 25 of 125 subjects in the latter group. There were no significant differences in the primary outcome of delivery before 34 weeks or secondary measures of loss before 24 weeks, preterm premature membrane rupture, mean gestational age at delivery, or neonatal outcomes. This study was not designed or powered to evaluate the efficacy of cerclage in preventing recurrent, spontaneous preterm birth. It simply compares two ways of selecting high-risk women for cerclage.12
We lack data supporting placement of cerclage for an incidentally detected short cervix in women who lack a history of spontaneous preterm birth or midtrimester loss.7
Other groups known to be at increased risk of spontaneous preterm birth include women carrying twins and women who have undergone cervical cone biopsy or loop electrosurgical excision procedure (LEEP). Among twin gestations, cerclage for a short cervix is associated with an increased rate of preterm birth (<35 weeks).10 Cerclage for a short cervix has not been evaluated among women who have a history of LEEP.6
CASE RESOLVED
After preterm labor is ruled out, the patient is counseled about her options and chooses cervical cerclage. Her pregnancy proceeds uneventfully until 36 weeks’ gestation, when she delivers a healthy infant weighing 2,950 g.
When a short cervix is detected between 24 and 34 weeks
CASE 3: Is it preterm labor?
A primigravida at 31 weeks’ gestation presents to the labor floor reporting regular contractions. She denies bleeding or rupture of membranes. Contractions are noted at 3-minute intervals, and digital cervical examination reveals that she is dilated 1 cm, with 70% effacement. TVUS determines cervical length to be 17 mm.
How should she be managed?
From 24 to 34 weeks’ gestation, the prevention, diagnosis, and treatment of preterm labor become the main concerns. Because our ability to predict and prevent preterm birth is limited, clinical management focuses on a reliable diagnosis of preterm labor to allow for selective, timely interventions to optimize neonatal outcomes. These interventions include tocolysis to permit maternal transport; antibiotic prophylaxis for group B strep; and steroid administration to accelerate fetal lung maturity. Equally important is the ability to reliably rule out preterm labor among symptomatic (contracting) women to avoid the potential morbidity, cost, and inconvenience of these interventions.
Before 37 weeks, a diagnosis of preterm labor requires the following findings:
- six or more contractions per hour
- cervical dilation, as identified by digital examination, of at least 3 cm and 80% effacement.
This diagnosis is more reliable when ruptured membranes or vaginal bleeding are present.
The significance of contractions without these findings is less clear. Therefore, we follow an algorithm that incorporates TVUS measurement of cervical length and evaluation of fetal fibronectin (fFN) (FIGURE 4).13
fFN is a glycoprotein that is normally confined to the extracellular matrix of the fetal membranes between 24 and 34 weeks’ gestation. Detection of fFN in cervicovaginal secretions during this window is associated with an increased risk of spontaneous preterm birth, whereas its absence demonstrates a negative predictive value for delivery within 7 days of testing of more than 97%.
During initial assessment of a regularly contracting preterm patient, perform a vaginal speculum examination. If the membranes are intact, use a vaginal swab to assess the patient for the presence of fFN, and set the specimen aside. Also obtain a culture for group B strep.
If a digital cervical examination and the contraction pattern establish a diagnosis of preterm labor, administer a tocolytic, When fetal prophylactic antibiotics, and steroids. If the diagnosis remains unclear, evaluate the cervix via TVUS. A cervical length above 30 mm effectively rules out preterm labor and obviates the need to send the fFN swab for assessment. As a result, the patient can be managed expectantly.
In contrast, a cervical length below 20 mm effectively confirms the diagnosis of preterm labor, and treatment can proceed. Again, the fFN swab may be discarded. The swab is sent for processing only if cervical length is 20 mm to 30 mm (FIGURE 4). A positive fFN result leads to the presumptive diagnosis of preterm labor, whereas a negative result permits expectant management.
We also recommend that women who display symptoms of preterm labor be screened for asymptomatic bacteriuria. Identification and treatment of this condition significantly reduce the risk of preterm delivery (RR, 0.56; 95% CI, 0.43–0.73).14 In addition, diagnosis and treatment of bacterial vaginosis in symptomatic women who have a history of spontaneous preterm birth can also reduce the risk of recurrent preterm delivery (RR, 0.42; 95% CI, 0.27–0.67).15
Not all obstetric care providers have the resources necessary for TVUS assessment of cervical length. When that is the case, fFN offers high sensitivity and negative predictive value and can help guide initial clinical decision-making. Keep in mind, however, that not all facilities offer fFN testing. In addition, in some cases, cervical manipulation may have occurred before fFN testing was performed, precluding its validity. In such cases, the incorporation of TVUS assessment of cervical length into clinical evaluation may help guide decision-making.

FIGURE 4 How to identify preterm labor at 24 to 34 weeks
CASE RESOLVED
The determination of short cervical length (17 mm) by TVUS confirms the diagnosis of preterm labor. The patient is admitted to the hospital and treated with a tocolytic, prophylactic antibiotics, and steroids. Three days later, preterm labor recurs, and she delivers an otherwise healthy infant. Future pregnancies will be managed according to the algorithm presented in FIGURE 5.
Cerclage may benefit women who have a history of spontaneous preterm birth
A recent multicenter randomized trial evaluated the efficacy of cerclage in preventing preterm birth among 302 women who had a history of spontaneous preterm birth before 34 weeks’ gestation.11 Any woman who had a cervix shorter than 25 mm between 16-0/7 and 22-6/7 weeks’ gestation was randomized to cerclage or no cerclage.
Cerclage did not significantly reduce preterm delivery before 35 weeks’ gestation, the primary outcome. Thirty-two percent of women who received cerclage and 42% of women who did not receive cerclage delivered before 35 weeks (P = .09). However, among women who had a cervix shorter than 15 mm at randomization, cerclage reduced the rate of delivery before 35 weeks by more than 75% (P = .006). Cerclage also reduced the rate of spontaneous birth before 37 weeks, compared with no cerclage (45% vs 60%; P = .01), as well as the rate of previable preterm birth before 24 weeks (6.1% vs 14%; P = .03) and the rate of perinatal death (8.8% vs 16%; P = .046).
As this study demonstrates, ultrasonographically indicated cerclage produces a number of highly clinically significant benefits in women who have a history of spontaneous preterm birth. Another important question is whether supplemental progesterone offers additional benefit beyond that conferred by cerclage in this population.
The role of progesterone in preventing preterm birth
CASE 4: History of preterm and term delivery
A woman in her third pregnancy is referred for placement of cervical cerclage, based on her obstetric history. Her first pregnancy was marked by preterm labor at 26 weeks, resulting in spontaneous preterm birth at 28 weeks. In her second pregnancy, she had cerclage placed electively at 13 weeks and delivered spontaneously at 40 weeks with no complications of pregnancy.
Is another cerclage indicated—or would progesterone be more effective?
Supplemental 17-hydroxyprogesterone caproate, given weekly in an intramuscular dosage of 250 mg, significantly reduced the rate of recurrent spontaneous preterm birth when it was administered from 16 to 36 weeks’ gestation in women carrying a singleton fetus.16 The protective effect of progesterone is most apparent in women who have a history of very preterm delivery (<32 weeks). No such benefit has been observed in twin and triplet gestations, however.17-19
Among women who do benefit from progesterone, the effect may vary. For this reason, researchers have explored the measurement of midtrimester cervical length as a means of stratifying response to progesterone.
For example, investigators randomized women who had a history of spontaneous preterm birth to daily treatment with 90 mg of vaginal progesterone gel or placebo, starting between 16 and 22-6/7 weeks and continuing until 37 weeks or delivery, whichever came first. No difference in the rate of delivery at or before 32 weeks was observed. However, a secondary analysis among progesterone-treated women who had a cervical length below 28 mm found significant declines in the rate of delivery at or before 32 weeks, admission to a NICU, and length of stay.20,21
In another trial, investigators assessed cervical length via TVUS between 20 and 25 weeks’ gestation in a general obstetric population that included women carrying twins. Women who had a cervical length below 15 mm were offered randomization to daily oral progesterone (200 mg) or placebo from 24 weeks to 33-6/7 weeks’ gestation. The rate of spontaneous preterm birth was significantly lower in the progesterone group (19% vs 34%).22
Because the ideal formulation of progesterone for the prevention of preterm birth is unknown, ACOG recommends restricting its use to women who have a documented history of spontaneous preterm birth at less than 37 weeks’ gestation.23 My practice follows the protocol of Meis and colleagues within the framework of an overall systematic algorithm (FIGURE 5).

FIGURE 5 Cervical length in the second trimester
*For a singleton gestation only.
CASE RESOLVED
The ObGyn reviews the patient’s obstetric history and determines that the first pregnancy was more suggestive of preterm labor than cervical insufficiency. Therefore, the ObGyn opts for progesterone rather than cerclage to prolong the gestation. The patient begins weekly injections of 17-hydroxyprogesterone caproate, starting at 16 weeks’ gestation, with TVUS measurement of cervical length every 2 weeks. The cervix remains longer than 25 mm through 24 weeks’ gestation, at which time TVUS assessment is stopped. Progesterone injections continue through 36 weeks, and the patient spontaneously delivers a healthy 3,700-g infant at term.
CASE 1: Short cervix in the middle trimester
During routine second-trimester ultrasonography, a 34-year-old primigravida at 22 weeks’ gestation is found to have a cervix 15 mm in length. She has no other risk factors for spontaneous preterm birth.
What steps do you take to ensure that her pregnancy progresses uneventfully to term?
Cervical length is not routinely measured in low-risk women—i.e., those without a history of spontaneous preterm birth—but a short cervix is sometimes detected during ultrasonographic imaging for other indications, as it was in this case. When a short cervix is detected incidentally, I educate the patient to watch for early warning signs of preterm labor. I also recommend pelvic rest and a sedentary lifestyle.
The rate of preterm birth declined slightly in 2007—the first decrease in more than 20 years—but the phenomenon remains the leading cause of perinatal morbidity and mortality in developed nations.1 In the United States, more than 500,000 babies each year, or 12% to 13% of all births, are delivered before 37 weeks’ gestation. Most of these births are spontaneous and involve preterm labor or premature rupture of membranes. Medical costs for a preterm newborn exceed those of a term infant by a multiple of more than 10, and the average hospitalization exceeds that of a term infant by a multiple of more than six.
In this article, I discuss the rationale and technique for ultrasonographic cervical measurement to determine the likelihood of preterm birth. I also examine the data on the short cervix in various settings, and describe strategies for cervical assessment and preterm birth prevention, including cerclage and progesterone, framing the discussion in terms of gestational age.
Accurate and reproducible measurement of cervical length depends on correct technique. Use of transvaginal ultrasonography (TVUS) limits variations between measurements to 5% to 10%, a marked improvement over digital examination and transabdominal US.
Here are the five steps involved, in the order performed:
- Ensure that the patient’s bladder is empty. This precaution is necessary to prevent dynamic, or spontaneous, lengthening or shortening of the cervix.
- Counsel and position the patient. Explain the procedure to the patient and have her assume the dorsal lithotomy position.
- Introduce the probe into the anterior vaginal fornix using real-time visualization, and obtain a mid-sagittal view of the cervix. Withdraw the probe just enough to allow the image to blur, then advance the probe just enough for the image to regain clarity. This sequence prevents the practitioner from exerting excessive pressure on the cervix, which can falsely elongate it.
- Place an electronic caliper (on-screen) at the notch that represents the internal cervical os, and another at the external os (FIGURE 1).
- Measure the distance between the notches and report the shortest of three separately obtained measurements.
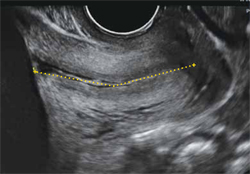
FIGURE 1 How to measure the cervix
Electronic calipers mark the internal and external os in this cervix measuring 42 mm via midsagittal transvaginal ultrasonography.
Watch for these pitfalls!
Before 20 weeks’ gestation, the lower uterine segment is not particularly well developed, making it difficult to reliably determine the location of the internal os (FIGURE 2). Moreover, focal myometrial contractions of the lower uterine segment, which are common, may give the false impression of increased cervical length or dilation of the internal os (FIGURE 2).24
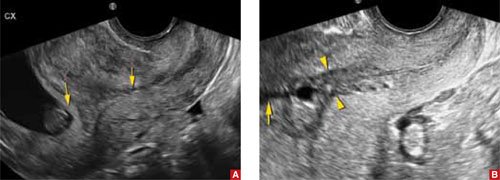
FIGURE 2 Measurement may be difficult in early pregnancy
A. This transvaginal sonogram demonstrates the difficulty of determining the location of the internal os when the lower uterine segment is undeveloped (arrows). B. When lower uterine contractions occur with the anterior and posterior walls in opposition (arrowheads), transvaginal imaging may give the false appearance of dilation with funneling (arrow).
Why we assess cervical length
In the past, the cervix was viewed as either competent—i.e., capable of maintaining a pregnancy until term—or as “incompetent.” More recent evidence has broadened our understanding of cervical function, which is now viewed along a continuum.
In landmark research in the mid-1990s, investigators compared cervical lengths, measured via transvaginal ultrasonography (TVUS), between two groups of pregnant women—those who had a history of preterm birth and those who did not.
The result? Gestational age at delivery in the first pregnancy correlated significantly—and continuously—with cervical length between 20 and 30 weeks’ gestation in the subsequent pregnancy.2 Investigators also observed that the risk of spontaneous preterm birth increased with decreasing cervical length. A length of 25 mm (10th percentile) offered a clinically appropriate threshold for identification of the risk of preterm delivery.3
The value of cervical-length measurement lies in its high negative predictive value for recurrent spontaneous preterm birth.4 As a general rule of thumb, routine assessment of cervical length in asymptomatic women who do not have a history of preterm birth is not recommended because of the high rate of false-positive results and the low positive predictive value for preterm delivery. We also lack an evidence-based consensus on how to manage an abnormally short cervix in these women.
CASE RESOLVED
The patient is counseled to watch for signs of preterm labor and to remain sedentary. Her pregnancy progresses without incident until 40 weeks, when she undergoes induction of labor for oligohydramnios and delivers a healthy infant weighing 3,855 g.
When a short cervix is detected at less than 20 weeks
If a woman has a history of spontaneous preterm birth, a short cervix this early in gestation raises the question of cervical insufficiency. No objective criteria have been devised to identify this condition. Nor is there a widely accepted definition. A reasonable description does exist, however:
- …a clinical diagnosis characterized by recurrent painless dilation and spontaneous midtrimester birth, generally in the absence of predisposing conditions such as spontaneous membrane rupture, bleeding, and infection, characteristics that shift the presumed underlying cause away from cervical incompetence and support other components of the preterm birth syndrome.5
A patient who fits this description may be a candidate for cervical cerclage. Alternatively, it is reasonable to reassess the patient in 3 to 7 days, after restricting physical activity, keeping in mind the pitfalls of TVUS assessment of the lower uterine segment in early gestation (see the box on imaging). If cervical length remains short, consider cerclage.6,7
Watch for inflammation
Occasionally, echogenic material is observed in the amniotic fluid at the level of a short cervix. This debris is an inflammatory exudate of fibrin, white blood cells, and bacteria. The presence of this sludge (FIGURE 3) signifies a risk of preterm birth much greater than that associated with a short cervix alone.8 Because cerclage in the presence of inflammation may further heighten the risk of spontaneous preterm birth, I recommend caution.

FIGURE 3 Watch for signs of inflammation
When inflammatory exudate (asterisk) is identified at the level of a short cervix, the risk of spontaneous preterm birth is elevated beyond the risk associated with a short cervix alone.
When a short cervix is detected between 20 and 24 weeks
CASE 2: Is recurrent preterm birth likely?
A 30-year-old woman 21 weeks pregnant with her second child reports for TVUS. Because her first child was delivered preterm at 30 weeks, she has been undergoing periodic measurement of her cervix. Until today, it has been longer than 25 mm, but now it is 20 mm. What is the best strategy to avert another preterm birth?
If a short cervix (<25 mm) is noted in a high-risk patient at this gestational age, consider the possibility of preterm labor and ruptured membranes. If these conditions are present, they should be managed according to existing guidelines.4,9 If they are absent, consider cerclage.
A recent meta-analysis of randomized trials of cerclage for the prevention of preterm birth in a singleton, high-risk pregnancy with a short cervix suggests that cerclage is associated with a significantly lower risk of delivery before 35 weeks’ gestation (relative risk [RR], 0.61; 95% confidence interval [CI], 0.40–0.92). Among singleton pregnancies involving both a short cervix and a history of midtrimester loss, cerclage is again associated with a reduced likelihood of delivery before 35 weeks (39% vs 23.4%; number needed to treat [NNT], 8; RR, 0.57; 95% CI, 0.33–0.99).10 A recent randomized trial of cerclage versus no cerclage in women who had a history of spontaneous preterm birth produced similar findings.11 This trial is described in detail in the box.
Another randomized trial compared the relative merits of ultrasound-indicated cerclage for a cervix shorter than 20 mm to a history-indicated cerclage among women with a prior spontaneous preterm birth between 16 and 34 weeks. Thirty-nine of 123 women randomized to the former group received a cerclage, as did 25 of 125 subjects in the latter group. There were no significant differences in the primary outcome of delivery before 34 weeks or secondary measures of loss before 24 weeks, preterm premature membrane rupture, mean gestational age at delivery, or neonatal outcomes. This study was not designed or powered to evaluate the efficacy of cerclage in preventing recurrent, spontaneous preterm birth. It simply compares two ways of selecting high-risk women for cerclage.12
We lack data supporting placement of cerclage for an incidentally detected short cervix in women who lack a history of spontaneous preterm birth or midtrimester loss.7
Other groups known to be at increased risk of spontaneous preterm birth include women carrying twins and women who have undergone cervical cone biopsy or loop electrosurgical excision procedure (LEEP). Among twin gestations, cerclage for a short cervix is associated with an increased rate of preterm birth (<35 weeks).10 Cerclage for a short cervix has not been evaluated among women who have a history of LEEP.6
CASE RESOLVED
After preterm labor is ruled out, the patient is counseled about her options and chooses cervical cerclage. Her pregnancy proceeds uneventfully until 36 weeks’ gestation, when she delivers a healthy infant weighing 2,950 g.
When a short cervix is detected between 24 and 34 weeks
CASE 3: Is it preterm labor?
A primigravida at 31 weeks’ gestation presents to the labor floor reporting regular contractions. She denies bleeding or rupture of membranes. Contractions are noted at 3-minute intervals, and digital cervical examination reveals that she is dilated 1 cm, with 70% effacement. TVUS determines cervical length to be 17 mm.
How should she be managed?
From 24 to 34 weeks’ gestation, the prevention, diagnosis, and treatment of preterm labor become the main concerns. Because our ability to predict and prevent preterm birth is limited, clinical management focuses on a reliable diagnosis of preterm labor to allow for selective, timely interventions to optimize neonatal outcomes. These interventions include tocolysis to permit maternal transport; antibiotic prophylaxis for group B strep; and steroid administration to accelerate fetal lung maturity. Equally important is the ability to reliably rule out preterm labor among symptomatic (contracting) women to avoid the potential morbidity, cost, and inconvenience of these interventions.
Before 37 weeks, a diagnosis of preterm labor requires the following findings:
- six or more contractions per hour
- cervical dilation, as identified by digital examination, of at least 3 cm and 80% effacement.
This diagnosis is more reliable when ruptured membranes or vaginal bleeding are present.
The significance of contractions without these findings is less clear. Therefore, we follow an algorithm that incorporates TVUS measurement of cervical length and evaluation of fetal fibronectin (fFN) (FIGURE 4).13
fFN is a glycoprotein that is normally confined to the extracellular matrix of the fetal membranes between 24 and 34 weeks’ gestation. Detection of fFN in cervicovaginal secretions during this window is associated with an increased risk of spontaneous preterm birth, whereas its absence demonstrates a negative predictive value for delivery within 7 days of testing of more than 97%.
During initial assessment of a regularly contracting preterm patient, perform a vaginal speculum examination. If the membranes are intact, use a vaginal swab to assess the patient for the presence of fFN, and set the specimen aside. Also obtain a culture for group B strep.
If a digital cervical examination and the contraction pattern establish a diagnosis of preterm labor, administer a tocolytic, When fetal prophylactic antibiotics, and steroids. If the diagnosis remains unclear, evaluate the cervix via TVUS. A cervical length above 30 mm effectively rules out preterm labor and obviates the need to send the fFN swab for assessment. As a result, the patient can be managed expectantly.
In contrast, a cervical length below 20 mm effectively confirms the diagnosis of preterm labor, and treatment can proceed. Again, the fFN swab may be discarded. The swab is sent for processing only if cervical length is 20 mm to 30 mm (FIGURE 4). A positive fFN result leads to the presumptive diagnosis of preterm labor, whereas a negative result permits expectant management.
We also recommend that women who display symptoms of preterm labor be screened for asymptomatic bacteriuria. Identification and treatment of this condition significantly reduce the risk of preterm delivery (RR, 0.56; 95% CI, 0.43–0.73).14 In addition, diagnosis and treatment of bacterial vaginosis in symptomatic women who have a history of spontaneous preterm birth can also reduce the risk of recurrent preterm delivery (RR, 0.42; 95% CI, 0.27–0.67).15
Not all obstetric care providers have the resources necessary for TVUS assessment of cervical length. When that is the case, fFN offers high sensitivity and negative predictive value and can help guide initial clinical decision-making. Keep in mind, however, that not all facilities offer fFN testing. In addition, in some cases, cervical manipulation may have occurred before fFN testing was performed, precluding its validity. In such cases, the incorporation of TVUS assessment of cervical length into clinical evaluation may help guide decision-making.

FIGURE 4 How to identify preterm labor at 24 to 34 weeks
CASE RESOLVED
The determination of short cervical length (17 mm) by TVUS confirms the diagnosis of preterm labor. The patient is admitted to the hospital and treated with a tocolytic, prophylactic antibiotics, and steroids. Three days later, preterm labor recurs, and she delivers an otherwise healthy infant. Future pregnancies will be managed according to the algorithm presented in FIGURE 5.
Cerclage may benefit women who have a history of spontaneous preterm birth
A recent multicenter randomized trial evaluated the efficacy of cerclage in preventing preterm birth among 302 women who had a history of spontaneous preterm birth before 34 weeks’ gestation.11 Any woman who had a cervix shorter than 25 mm between 16-0/7 and 22-6/7 weeks’ gestation was randomized to cerclage or no cerclage.
Cerclage did not significantly reduce preterm delivery before 35 weeks’ gestation, the primary outcome. Thirty-two percent of women who received cerclage and 42% of women who did not receive cerclage delivered before 35 weeks (P = .09). However, among women who had a cervix shorter than 15 mm at randomization, cerclage reduced the rate of delivery before 35 weeks by more than 75% (P = .006). Cerclage also reduced the rate of spontaneous birth before 37 weeks, compared with no cerclage (45% vs 60%; P = .01), as well as the rate of previable preterm birth before 24 weeks (6.1% vs 14%; P = .03) and the rate of perinatal death (8.8% vs 16%; P = .046).
As this study demonstrates, ultrasonographically indicated cerclage produces a number of highly clinically significant benefits in women who have a history of spontaneous preterm birth. Another important question is whether supplemental progesterone offers additional benefit beyond that conferred by cerclage in this population.
The role of progesterone in preventing preterm birth
CASE 4: History of preterm and term delivery
A woman in her third pregnancy is referred for placement of cervical cerclage, based on her obstetric history. Her first pregnancy was marked by preterm labor at 26 weeks, resulting in spontaneous preterm birth at 28 weeks. In her second pregnancy, she had cerclage placed electively at 13 weeks and delivered spontaneously at 40 weeks with no complications of pregnancy.
Is another cerclage indicated—or would progesterone be more effective?
Supplemental 17-hydroxyprogesterone caproate, given weekly in an intramuscular dosage of 250 mg, significantly reduced the rate of recurrent spontaneous preterm birth when it was administered from 16 to 36 weeks’ gestation in women carrying a singleton fetus.16 The protective effect of progesterone is most apparent in women who have a history of very preterm delivery (<32 weeks). No such benefit has been observed in twin and triplet gestations, however.17-19
Among women who do benefit from progesterone, the effect may vary. For this reason, researchers have explored the measurement of midtrimester cervical length as a means of stratifying response to progesterone.
For example, investigators randomized women who had a history of spontaneous preterm birth to daily treatment with 90 mg of vaginal progesterone gel or placebo, starting between 16 and 22-6/7 weeks and continuing until 37 weeks or delivery, whichever came first. No difference in the rate of delivery at or before 32 weeks was observed. However, a secondary analysis among progesterone-treated women who had a cervical length below 28 mm found significant declines in the rate of delivery at or before 32 weeks, admission to a NICU, and length of stay.20,21
In another trial, investigators assessed cervical length via TVUS between 20 and 25 weeks’ gestation in a general obstetric population that included women carrying twins. Women who had a cervical length below 15 mm were offered randomization to daily oral progesterone (200 mg) or placebo from 24 weeks to 33-6/7 weeks’ gestation. The rate of spontaneous preterm birth was significantly lower in the progesterone group (19% vs 34%).22
Because the ideal formulation of progesterone for the prevention of preterm birth is unknown, ACOG recommends restricting its use to women who have a documented history of spontaneous preterm birth at less than 37 weeks’ gestation.23 My practice follows the protocol of Meis and colleagues within the framework of an overall systematic algorithm (FIGURE 5).

FIGURE 5 Cervical length in the second trimester
*For a singleton gestation only.
CASE RESOLVED
The ObGyn reviews the patient’s obstetric history and determines that the first pregnancy was more suggestive of preterm labor than cervical insufficiency. Therefore, the ObGyn opts for progesterone rather than cerclage to prolong the gestation. The patient begins weekly injections of 17-hydroxyprogesterone caproate, starting at 16 weeks’ gestation, with TVUS measurement of cervical length every 2 weeks. The cervix remains longer than 25 mm through 24 weeks’ gestation, at which time TVUS assessment is stopped. Progesterone injections continue through 36 weeks, and the patient spontaneously delivers a healthy 3,700-g infant at term.
1. Hamilton BE, Martin JA, Ventura SJ. Births: Preliminary data for 2007. National vital statistics reports; 2009;57(12). National Center for Health Statistics Web site. http://www.cdc.gov/nchs/data/nvsr/nvsr57/nvsr57_12.pdf. March 18, 2009. Accessed March 30, 2010.
2. Iams JD, Johnson FF, Sonek J, et al. Cervical competence as a continuum: a study of ultrasonographic cervical length and obstetric performance. Am J Obstet Gynecol. 1995;172(4 pt 1):1097-1106.
3. Iams JD, Goldenberg RL, Meis PJ, et al. The length of the cervix and the risk of spontaneous premature delivery. National Institute of Child Health and Human Development Maternal Fetal Medicine Unit Network. N Engl J Med. 1996;334(9):567-572.
4. Clinical Management Guidelines for Obstetrician-Gynecologists. No. 43, May 2003: Management of Preterm Labor. Obstet Gynecol. 2003;101(5 pt 1):1039-1047.
5. Owen J, Iams JD, Hauth JC. Vaginal sonography and cervical incompetence. Am J Obstet Gynecol. 2003;188(2):586-596.
6. Harger JH. Cerclage and cervical insufficiency: an evidence-based analysis. Obstet Gynecol. 2002;100(6):1313-1327.
7. Clinical Management Guidelines for Obstetrician-Gynecologists. No. 48, Nov 2003: Cervical insufficiency. Obstet Gynecol. 2003;102(5 pt 1):1091-1099.
8. Kusanovic JP, Espinoza J, Romero R, et al. Clinical significance of the presence of amniotic fluid ‘sludge’ in asymptomatic patients at high risk for spontaneous preterm delivery. Ultrasound Obstet Gynecol. 2007;30(5):706-714.
9. ACOG Practice Bulletin No. 80. Premature rupture of membranes. Obstet Gynecol. 2007;109(4):1007-1020.DOI:10.1097/01.AOG.0000263888.69178.1f.
10. Berghella V, Odibo AO, To MS, Rust OA, Althuisius SM. Cerclage for short cervix on ultrasonography: meta-analysis of trials using individual patient-level data. Obstet Gynecol. 2005;106(1):181-189.
11. Owen J, Hankins G, Iams JD, et al. Multicenter randomized trial of cerclage for preterm birth prevention in high-risk women with shortened mid-trimester cervical length. Am J Obstet Gynecol. 2009;201(4):375.e1-e8.
12. Simcox R, Seed PT, Bennett P, Teoh TG, Poston L, Shennan AH. A randomized control trial of cervical scanning vs history to determine cerclage in women at high risk of preterm birth (CIRCLE trial). Am J Obstet Gynecol. 2009;200(6):623.e1-e6.
13. Iams JD. Prediction and early detection of preterm labor. Obstet Gynecol. 2003;101(2):402-412.
14. Romero R, Oyarzun E, Mazor M, Sirtori M, Hobbins JC, Bracken M. Meta-analysis of the relationship between asymptomatic bacteriuria and preterm delivery/low birth weight. Obstet Gynecol. 1989;73(4):576-582.
15. Leitich H, Brunbauer M, Bodnar-Aderl B, Kaider A, Egarter C, Husslein P. Antibiotic treatment of bacterial vaginosis in pregnancy: a meta-analysis. Am J Obstet Gynecol. 2003;188(3):752-758.
16. Meis PJ, Klebanoff M, Thom E, et al. For National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Prevention of recurrent preterm birth by 17 alpha-hydroxyprogesterone caproate. N Engl J Med. 2003;348(24):2379-2385.
17. Norman JE, Mackenzie F, Owen P, et al. Progesterone for the prevention of preterm birth in twin pregnancy (STOPPIT): a randomised, double-blind, placebo-controlled study and meta-analysis. Lancet. 2009;373(9680):2034-2040.
18. Rouse DJ, Caritis SN, Peaceman AM, et al. For National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. A trial of 17 alpha-hydroxyprogesterone caproate to prevent prematurity in twins. N Engl J Med. 2007;357(5):454-461.
19. Caritis SN, Rouse DJ, Peaceman AM, et al. for Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), Medicine Units Network (MFMU). Prevention of preterm birth in triplets using 17 alpha-hydroxyprogesterone caproate: a randomized controlled trial. Obstet Gynecol. 2009;113(2 pt 1):285-292.
20. O’Brien JM, Adair CD, Lewis DF, et al. Progesterone vaginal gel for the reduction of recurrent preterm birth: primary results from a randomized, double-blind, placebo-controlled trial. Ultrasound Obstet Gynecol. 2007;30(5):687-696.
21. DeFranco EA, O’Brien JM, Adair CD, et al. Vaginal progesterone is associated with a decrease in risk for early preterm birth and improved neonatal outcome in women with a short cervix: a secondary analysis from a randomized, double-blind, placebo-controlled trial. Ultrasound Obstet Gynecol. 2007;30(5):697-705.
22. Fonseca EB, Celik E, Parra M, et al. For Fetal Medicine Foundation Second Trimester Screening Group. Progesterone and the risk of preterm birth among women with a short cervix. N Engl J Med. 2007;357(5):462-469.
23. ACOG Committee Opinion No. 419: Use of progesterone to reduce preterm birth. Obstet Gynecol. 2008;112(4):963.-
24. Yost NP, Bloom SL, Twickler DM, Leveno KJ. Pitfalls in ultrasonic cervical length measurement for predicting preterm birth. Obstet Gynecol. 1999;93(4):510-516.
1. Hamilton BE, Martin JA, Ventura SJ. Births: Preliminary data for 2007. National vital statistics reports; 2009;57(12). National Center for Health Statistics Web site. http://www.cdc.gov/nchs/data/nvsr/nvsr57/nvsr57_12.pdf. March 18, 2009. Accessed March 30, 2010.
2. Iams JD, Johnson FF, Sonek J, et al. Cervical competence as a continuum: a study of ultrasonographic cervical length and obstetric performance. Am J Obstet Gynecol. 1995;172(4 pt 1):1097-1106.
3. Iams JD, Goldenberg RL, Meis PJ, et al. The length of the cervix and the risk of spontaneous premature delivery. National Institute of Child Health and Human Development Maternal Fetal Medicine Unit Network. N Engl J Med. 1996;334(9):567-572.
4. Clinical Management Guidelines for Obstetrician-Gynecologists. No. 43, May 2003: Management of Preterm Labor. Obstet Gynecol. 2003;101(5 pt 1):1039-1047.
5. Owen J, Iams JD, Hauth JC. Vaginal sonography and cervical incompetence. Am J Obstet Gynecol. 2003;188(2):586-596.
6. Harger JH. Cerclage and cervical insufficiency: an evidence-based analysis. Obstet Gynecol. 2002;100(6):1313-1327.
7. Clinical Management Guidelines for Obstetrician-Gynecologists. No. 48, Nov 2003: Cervical insufficiency. Obstet Gynecol. 2003;102(5 pt 1):1091-1099.
8. Kusanovic JP, Espinoza J, Romero R, et al. Clinical significance of the presence of amniotic fluid ‘sludge’ in asymptomatic patients at high risk for spontaneous preterm delivery. Ultrasound Obstet Gynecol. 2007;30(5):706-714.
9. ACOG Practice Bulletin No. 80. Premature rupture of membranes. Obstet Gynecol. 2007;109(4):1007-1020.DOI:10.1097/01.AOG.0000263888.69178.1f.
10. Berghella V, Odibo AO, To MS, Rust OA, Althuisius SM. Cerclage for short cervix on ultrasonography: meta-analysis of trials using individual patient-level data. Obstet Gynecol. 2005;106(1):181-189.
11. Owen J, Hankins G, Iams JD, et al. Multicenter randomized trial of cerclage for preterm birth prevention in high-risk women with shortened mid-trimester cervical length. Am J Obstet Gynecol. 2009;201(4):375.e1-e8.
12. Simcox R, Seed PT, Bennett P, Teoh TG, Poston L, Shennan AH. A randomized control trial of cervical scanning vs history to determine cerclage in women at high risk of preterm birth (CIRCLE trial). Am J Obstet Gynecol. 2009;200(6):623.e1-e6.
13. Iams JD. Prediction and early detection of preterm labor. Obstet Gynecol. 2003;101(2):402-412.
14. Romero R, Oyarzun E, Mazor M, Sirtori M, Hobbins JC, Bracken M. Meta-analysis of the relationship between asymptomatic bacteriuria and preterm delivery/low birth weight. Obstet Gynecol. 1989;73(4):576-582.
15. Leitich H, Brunbauer M, Bodnar-Aderl B, Kaider A, Egarter C, Husslein P. Antibiotic treatment of bacterial vaginosis in pregnancy: a meta-analysis. Am J Obstet Gynecol. 2003;188(3):752-758.
16. Meis PJ, Klebanoff M, Thom E, et al. For National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Prevention of recurrent preterm birth by 17 alpha-hydroxyprogesterone caproate. N Engl J Med. 2003;348(24):2379-2385.
17. Norman JE, Mackenzie F, Owen P, et al. Progesterone for the prevention of preterm birth in twin pregnancy (STOPPIT): a randomised, double-blind, placebo-controlled study and meta-analysis. Lancet. 2009;373(9680):2034-2040.
18. Rouse DJ, Caritis SN, Peaceman AM, et al. For National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. A trial of 17 alpha-hydroxyprogesterone caproate to prevent prematurity in twins. N Engl J Med. 2007;357(5):454-461.
19. Caritis SN, Rouse DJ, Peaceman AM, et al. for Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), Medicine Units Network (MFMU). Prevention of preterm birth in triplets using 17 alpha-hydroxyprogesterone caproate: a randomized controlled trial. Obstet Gynecol. 2009;113(2 pt 1):285-292.
20. O’Brien JM, Adair CD, Lewis DF, et al. Progesterone vaginal gel for the reduction of recurrent preterm birth: primary results from a randomized, double-blind, placebo-controlled trial. Ultrasound Obstet Gynecol. 2007;30(5):687-696.
21. DeFranco EA, O’Brien JM, Adair CD, et al. Vaginal progesterone is associated with a decrease in risk for early preterm birth and improved neonatal outcome in women with a short cervix: a secondary analysis from a randomized, double-blind, placebo-controlled trial. Ultrasound Obstet Gynecol. 2007;30(5):697-705.
22. Fonseca EB, Celik E, Parra M, et al. For Fetal Medicine Foundation Second Trimester Screening Group. Progesterone and the risk of preterm birth among women with a short cervix. N Engl J Med. 2007;357(5):462-469.
23. ACOG Committee Opinion No. 419: Use of progesterone to reduce preterm birth. Obstet Gynecol. 2008;112(4):963.-
24. Yost NP, Bloom SL, Twickler DM, Leveno KJ. Pitfalls in ultrasonic cervical length measurement for predicting preterm birth. Obstet Gynecol. 1999;93(4):510-516.