User login
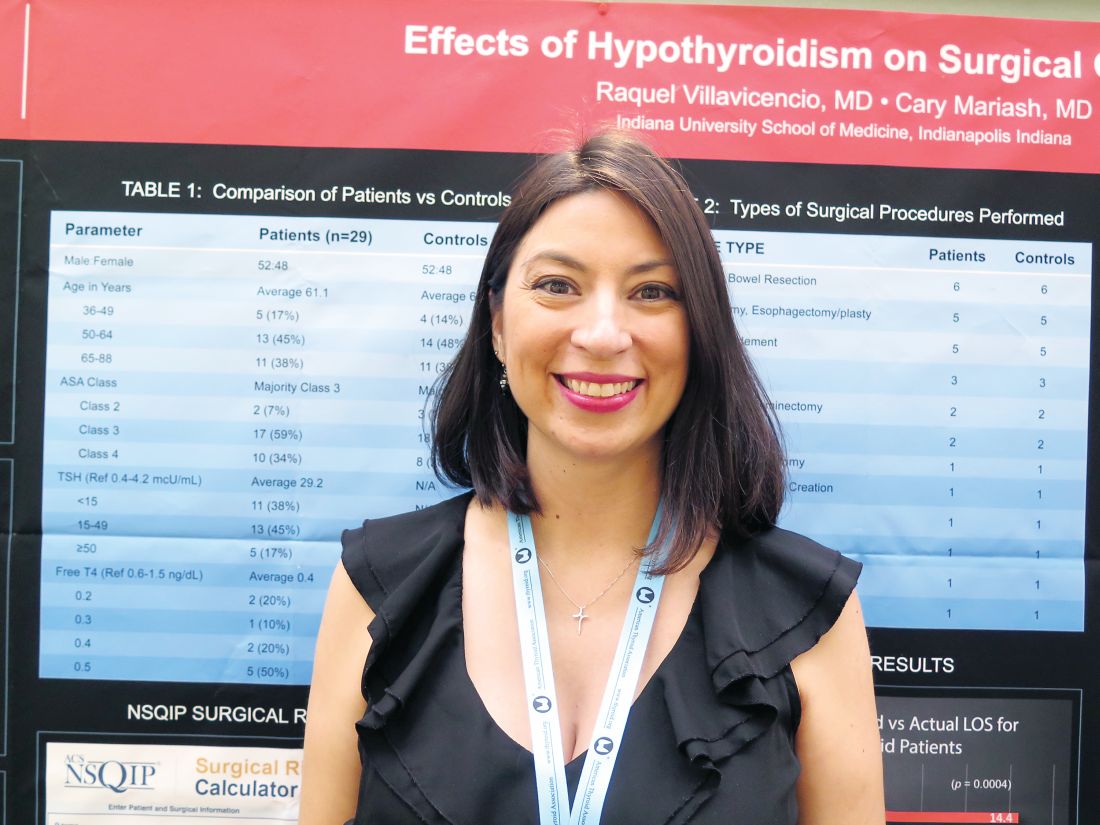
VICTORIA, B.C. – Even with contemporary anesthesia and surgical techniques, patients who are overtly hypothyroid at the time of major surgery have a rockier course, suggests a retrospective cohort study of 58 patients in a poster presentation at the annual meeting of the American Thyroid Association.
Actual length of stay for hypothyroid patients was twice that predicted by a commonly used risk calculator, whereas actual and predicted stays aligned well for euthyroid patients. The hypothyroid group had more cases of postoperative atrial fibrillation, ileus, reintubation, and death, although numbers were too small for statistical comparison.
“This will have an impact on how we look at patients, especially from a hospital standpoint and management. That’s quite a bit longer stay and quite a bit more cost. And the longer you stay, the more complications you have, too, so it could be riskier for the patient as well,” said first author Raquel Villavicencio, MD, a fellow at Indiana University at the time of the study, and now a clinical endocrinologist at Community Hospital in Indianapolis.
“Although we don’t consider hypothyroidism an absolute contraindication to surgery, especially if it’s necessary surgery, certainly anybody who is having elective surgery should have it postponed, in our opinion, until they are rendered euthyroid,” she said. “More studies are needed to look at this a little bit closer.”
Explaining the study’s rationale, Dr. Villavicencio noted, “This was a question that came up maybe three or four times a year, where we would get a hypothyroid patient and had to decide whether or not to clear them for surgery.”
Previous studies conducted at large institutions, the Mayo Clinic and Massachusetts General Hospital, had conflicting findings and were done about 30 years ago, she said. Anesthesia and surgical care have improved substantially since then, leading the investigators to hypothesize that hypothyroidism would not carry higher surgical risk today.
Dr. Villavicencio and her coinvestigator, Cary Mariash, MD, used their institutional database to identify 29 adult patients with a thyroid-stimulating hormone (TSH) level of greater than 10 mcU/mL alone or with a TSH level exceeding the upper limit of normal along with a free thyroxine (T4) level of less than 0.6 ng/dL who underwent surgery during 2010-2015. They matched each patient on age, sex, and surgical procedure with a control euthyroid patient.
The mean TSH level in the hypothyroid group was 29.2 mcU/mL. The majority of patients in each group – 59% of the hypothyroid group and 62% of the euthyroid group – had an American Surgical Association class of 3, denoting that this was a fairly sick population. The groups were generally similar on rates of comorbidity, except that the euthyroid patients had a slightly higher prevalence of obstructive sleep apnea.
In both groups, the majority of procedures were laparotomy and/or bowel resection; pharyngolaryngectomy and esophagectomy/esophagoplasty; and wound or bone debridement.
Main results showed that in the hypothyroid group, hospital length of stay predicted with the American College of Surgeons National Surgical Quality Improvement Program surgical risk calculator was 6.9 days, but actual length of stay was 14.4 days (P = .0004). In contrast, in the euthyroid group, predicted length of stay was a similar at 7.1 days, and actual length of stay was statistically indistinguishable at 9.2 days (P = .1).
“Hypothyroidism is not taken into account with this calculator,” Dr. Villavicencio noted, adding that she was unaware of any surgical calculators that do.
One patient in the hypothyroid group died, compared with none in the euthyroid group. In terms of postoperative cardiac complications, two patients in the hypothyroid group experienced atrial fibrillation, and there was one case of pulseless electrical–activity arrest in each group.
The groups did not differ on incidence of hypothermia, bradycardia, hyponatremia, time to extubation, and hypotension. However, mean arterial pressure tended to be lower in the hypothyroid group (51 mm Hg) than in the euthyroid group (56 mm Hg), and the former more often needed vasopressors. Furthermore, postoperative ileus and reintubation were more common in the hypothyroid group.
“I think that there are kind of a lot of little things that add up to explain [the longer stay],” said Dr. Villavicencio, who disclosed that she had no relevant conflicts of interest.
VICTORIA, B.C. – Even with contemporary anesthesia and surgical techniques, patients who are overtly hypothyroid at the time of major surgery have a rockier course, suggests a retrospective cohort study of 58 patients in a poster presentation at the annual meeting of the American Thyroid Association.
Actual length of stay for hypothyroid patients was twice that predicted by a commonly used risk calculator, whereas actual and predicted stays aligned well for euthyroid patients. The hypothyroid group had more cases of postoperative atrial fibrillation, ileus, reintubation, and death, although numbers were too small for statistical comparison.
“This will have an impact on how we look at patients, especially from a hospital standpoint and management. That’s quite a bit longer stay and quite a bit more cost. And the longer you stay, the more complications you have, too, so it could be riskier for the patient as well,” said first author Raquel Villavicencio, MD, a fellow at Indiana University at the time of the study, and now a clinical endocrinologist at Community Hospital in Indianapolis.
“Although we don’t consider hypothyroidism an absolute contraindication to surgery, especially if it’s necessary surgery, certainly anybody who is having elective surgery should have it postponed, in our opinion, until they are rendered euthyroid,” she said. “More studies are needed to look at this a little bit closer.”
Explaining the study’s rationale, Dr. Villavicencio noted, “This was a question that came up maybe three or four times a year, where we would get a hypothyroid patient and had to decide whether or not to clear them for surgery.”
Previous studies conducted at large institutions, the Mayo Clinic and Massachusetts General Hospital, had conflicting findings and were done about 30 years ago, she said. Anesthesia and surgical care have improved substantially since then, leading the investigators to hypothesize that hypothyroidism would not carry higher surgical risk today.
Dr. Villavicencio and her coinvestigator, Cary Mariash, MD, used their institutional database to identify 29 adult patients with a thyroid-stimulating hormone (TSH) level of greater than 10 mcU/mL alone or with a TSH level exceeding the upper limit of normal along with a free thyroxine (T4) level of less than 0.6 ng/dL who underwent surgery during 2010-2015. They matched each patient on age, sex, and surgical procedure with a control euthyroid patient.
The mean TSH level in the hypothyroid group was 29.2 mcU/mL. The majority of patients in each group – 59% of the hypothyroid group and 62% of the euthyroid group – had an American Surgical Association class of 3, denoting that this was a fairly sick population. The groups were generally similar on rates of comorbidity, except that the euthyroid patients had a slightly higher prevalence of obstructive sleep apnea.
In both groups, the majority of procedures were laparotomy and/or bowel resection; pharyngolaryngectomy and esophagectomy/esophagoplasty; and wound or bone debridement.
Main results showed that in the hypothyroid group, hospital length of stay predicted with the American College of Surgeons National Surgical Quality Improvement Program surgical risk calculator was 6.9 days, but actual length of stay was 14.4 days (P = .0004). In contrast, in the euthyroid group, predicted length of stay was a similar at 7.1 days, and actual length of stay was statistically indistinguishable at 9.2 days (P = .1).
“Hypothyroidism is not taken into account with this calculator,” Dr. Villavicencio noted, adding that she was unaware of any surgical calculators that do.
One patient in the hypothyroid group died, compared with none in the euthyroid group. In terms of postoperative cardiac complications, two patients in the hypothyroid group experienced atrial fibrillation, and there was one case of pulseless electrical–activity arrest in each group.
The groups did not differ on incidence of hypothermia, bradycardia, hyponatremia, time to extubation, and hypotension. However, mean arterial pressure tended to be lower in the hypothyroid group (51 mm Hg) than in the euthyroid group (56 mm Hg), and the former more often needed vasopressors. Furthermore, postoperative ileus and reintubation were more common in the hypothyroid group.
“I think that there are kind of a lot of little things that add up to explain [the longer stay],” said Dr. Villavicencio, who disclosed that she had no relevant conflicts of interest.
VICTORIA, B.C. – Even with contemporary anesthesia and surgical techniques, patients who are overtly hypothyroid at the time of major surgery have a rockier course, suggests a retrospective cohort study of 58 patients in a poster presentation at the annual meeting of the American Thyroid Association.
Actual length of stay for hypothyroid patients was twice that predicted by a commonly used risk calculator, whereas actual and predicted stays aligned well for euthyroid patients. The hypothyroid group had more cases of postoperative atrial fibrillation, ileus, reintubation, and death, although numbers were too small for statistical comparison.
“This will have an impact on how we look at patients, especially from a hospital standpoint and management. That’s quite a bit longer stay and quite a bit more cost. And the longer you stay, the more complications you have, too, so it could be riskier for the patient as well,” said first author Raquel Villavicencio, MD, a fellow at Indiana University at the time of the study, and now a clinical endocrinologist at Community Hospital in Indianapolis.
“Although we don’t consider hypothyroidism an absolute contraindication to surgery, especially if it’s necessary surgery, certainly anybody who is having elective surgery should have it postponed, in our opinion, until they are rendered euthyroid,” she said. “More studies are needed to look at this a little bit closer.”
Explaining the study’s rationale, Dr. Villavicencio noted, “This was a question that came up maybe three or four times a year, where we would get a hypothyroid patient and had to decide whether or not to clear them for surgery.”
Previous studies conducted at large institutions, the Mayo Clinic and Massachusetts General Hospital, had conflicting findings and were done about 30 years ago, she said. Anesthesia and surgical care have improved substantially since then, leading the investigators to hypothesize that hypothyroidism would not carry higher surgical risk today.
Dr. Villavicencio and her coinvestigator, Cary Mariash, MD, used their institutional database to identify 29 adult patients with a thyroid-stimulating hormone (TSH) level of greater than 10 mcU/mL alone or with a TSH level exceeding the upper limit of normal along with a free thyroxine (T4) level of less than 0.6 ng/dL who underwent surgery during 2010-2015. They matched each patient on age, sex, and surgical procedure with a control euthyroid patient.
The mean TSH level in the hypothyroid group was 29.2 mcU/mL. The majority of patients in each group – 59% of the hypothyroid group and 62% of the euthyroid group – had an American Surgical Association class of 3, denoting that this was a fairly sick population. The groups were generally similar on rates of comorbidity, except that the euthyroid patients had a slightly higher prevalence of obstructive sleep apnea.
In both groups, the majority of procedures were laparotomy and/or bowel resection; pharyngolaryngectomy and esophagectomy/esophagoplasty; and wound or bone debridement.
Main results showed that in the hypothyroid group, hospital length of stay predicted with the American College of Surgeons National Surgical Quality Improvement Program surgical risk calculator was 6.9 days, but actual length of stay was 14.4 days (P = .0004). In contrast, in the euthyroid group, predicted length of stay was a similar at 7.1 days, and actual length of stay was statistically indistinguishable at 9.2 days (P = .1).
“Hypothyroidism is not taken into account with this calculator,” Dr. Villavicencio noted, adding that she was unaware of any surgical calculators that do.
One patient in the hypothyroid group died, compared with none in the euthyroid group. In terms of postoperative cardiac complications, two patients in the hypothyroid group experienced atrial fibrillation, and there was one case of pulseless electrical–activity arrest in each group.
The groups did not differ on incidence of hypothermia, bradycardia, hyponatremia, time to extubation, and hypotension. However, mean arterial pressure tended to be lower in the hypothyroid group (51 mm Hg) than in the euthyroid group (56 mm Hg), and the former more often needed vasopressors. Furthermore, postoperative ileus and reintubation were more common in the hypothyroid group.
“I think that there are kind of a lot of little things that add up to explain [the longer stay],” said Dr. Villavicencio, who disclosed that she had no relevant conflicts of interest.
AT ATA 2017
Key clinical point:
Major finding: Actual length of stay was significantly longer than calculator-predicted length of stay among hypothyroid patients (14.4 vs. 6.9 days, P = .0004) but not among euthyroid patients (9.2 vs. 7.1 days; P = .1).
Data source: A retrospective cohort study of 29 hypothyroid patients and 29 matched euthyroid patients undergoing major surgery.
Disclosures: Dr. Villavicencio disclosed that she had no relevant conflicts of interest.