User login
- An “internal orgasm” may be linked to sensory input from the cervix. Therefore, removal of the cervix may inhibit sexual satisfaction.
- In a study evaluating the sexual functioning of women prior to and following supracervical, or “subtotal,” hysterectomy, about half the women reported improved sexual function, one-third reported little change, and one-fifth noted deterioration.
- The more interested and sexually active a woman is preoperatively, the more likely she is to report satisfactory sexual function postoperatively.
Concerns about postoperative sexuality often top the list of questions when a woman contemplates hysterectomy.1 Unfortunately, data regarding the impact of hysterectomy on sexual function are conflicting. Further, as Grimes points out, the literature fails to elucidate the role of the cervix in sexual response.2 Thus, it is difficult to advise women which procedure is better: a total or supracervical (“subtotal”) hysterectomy. The decision must be individualized following a thorough discussion with the patient.
One factor hampering scientific evaluation of the subject is the complex and ambiguous nature of the physiologic and psychologic aspects of sexuality. Preoperative medical conditions, emotional well-being, and/or the pathologic process necessitating the hysterectomy itself may contribute to both pre- and postoperative sexual functioning, as may the nature of a woman’s personal relationships and her support system. Therefore, it is no surprise that various studies have shown improvement, stability, and deterioration in sexuality following hysterectomy.1
Technique and other factors
With approximately 600,000 procedures performed annually, hysterectomy is one of the most common operations in the United States. Indications for the procedure constitute a broad spectrum of benign and malignant gynecologic disease.
Most gynecologists in practice today were taught to remove the cervix at the time of hysterectomy. To do otherwise was a sign of surgical naiveté. Recently, however, employing a uniform and inflexible approach has been questioned. As new surgical devices and advances in minimally invasive technology make it possible to perform subtotal hysterectomy safely and expediently, the debate over the fate of the benign cervix has been rekindled. Not only are new data emerging, but patients themselves are beginning to question the physical, physiologic, and psychologic sequelae of various operative techniques and participating, to a greater extent, in the formation of a surgical plan.
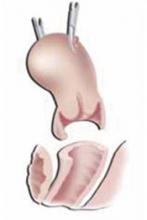
For the subtotal procedure, only the fundus is amputated from the cervix.
The total procedure. First, the uterus is separated from its surrounding and supporting tissues. The ligaments within the broad ligament, as well as the ovarian and uterine vessels, are clamped, divided, and ligated at their uterine attachments. Once the dissection has reached the level of the vaginal fornices, the bladder is mobilized anteriorly, the rectosigmoid colon posteriorly, and the ureters laterally with regard to the plane of resection. The uterus and cervix are then separated from their attachments to the vagina.
The subtotal procedure. For this technique, the uterine fundus is approached as described in the total hysterectomy. However, after the uterine blood supply is controlled, only the uterine fundus is amputated from the cervix. This procedure allows for varying amounts of the proximal cervix to be removed, depending on the extent of dissection. This is determined by the indications for the hysterectomy and the intraoperative anatomic findings. (A classification system in this regard has been proposed by Munro and Parker.3) The remaining cervical stump is cauterized and its edges coapted. At the conclusion of the procedure, the cervical stump appears similar to a vaginal cuff.
In my practice, after ligating the uterine vasculature, I remove a small portion of parametrial tissue at the level of the cervical isthmus to ensure the removal of all endometrial tissue. If some of it remains, menstrual flow may continue following the procedure.
While many gynecologic surgeons amputate the fundus from the cervix by transecting the tissue in a flat plane, I find that this hinders stump closure, especially when trying to coapt the tissue. Instead, I prefer to “core out” the proximal endocervical tissue. This technique—often described as a “reverse cone”—has several advantages. It effectively ensures excision of all endometrial tissue. In addition, some researchers have hypothesized that excision and cauterization of the endocervical canal can reduce the risk of adenocarcinomas of the cervical stump. Lastly, removal of this tissue allows for reapproximation of the wound edges without tension.
Complications and physiologic considerations
All surgical procedures carry some risk of adverse sequelae. In the case of hysterectomy, sites of potential injury include the bladder, rectosigmoid colon, and ureters. In fact, Harris found complication rates of 1% to 2% associated with the bladder, 0.25% to 0.4% for the bowel, and 0.2% for the ureters.4
Besides direct trauma to adjacent organs, hysterectomy also can cause neural damage to the visceral pelvic nerves surrounding the cervix and the autonomic nerves and ganglia in the uterine ligaments.5 Although total hysterectomy disrupts these neural tracts to a greater extent than subtotal hysterectomy, some degree of injury occurs even with the less extensive procedure. This disruption is thought to be the culprit of postoperative urinary, sphincteric, and sexual dysfunction.
For women whose sexual response includes an “internal orgasm”—thought to be linked to sensory input from the cervix—removal of the cervix may have marked negative effects on sexual satisfaction. Therefore, proponents of the subtotal hysterectomy claim that the more limited resection preserves the neural pathways and, thus, physiologic function. However, Grimes argues that the presence of neural tissue in and around the cervix does not necessarily mean that it is functional.2
Other potential deleterious effects of complete cervical excision include the development of scar or granulation tissue at the vaginal apex and the possible shortening of the vagina. It is not clear from the current literature whether complete cervical excision increases the risk of vaginal-vault or pelvic-floor prolapse.6
Effects on sexuality
Using data from the Maine Women’s Health Study, Carlson and colleagues found marked improvements in symptomatology, including reduced rates of sexual dysfunction, when hysterectomy was performed for fibroids, bleeding, or pain.7 They concluded that hysterectomy was associated with an overall improvement in the quality of life. New problems were limited, with only 7% of patients reporting a loss of interest in sex following surgery.
A report from the Maryland Women’s Health Study noted that rates of dyspareunia decreased following hysterectomy and that measures of sexual activity, libido, and orgasmic function increased.1 These improvements were thought to result from removal of the offending pathology and freedom from conception concerns.
Unfortunately, neither the Maine nor the Maryland studies assessed the effects of the type of hysterectomy on outcomes. However, a prospective study from Finland did. The result? Measures of sexual function, libido, and coital frequency did not differ statistically between women in the 2 groups—either preoperatively or 1 year postoperatively.8
However, the percentages of women reporting reduced orgasmic function did increase significantly over the year following surgery among women who had a total hysterectomy but did not change appreciably in the subtotal cohort. Dyspareunia occurred less often in both groups but to a greater extent in women who had a subtotal hysterectomy.
When Helström and colleagues from Sweden reported their evaluation of the sexual lives of women prior to and following subtotal hysterectomy, they found varied results.9 Approximately half the women surveyed reported improved sexuality after surgery, nearly one-third reported little change, and one-fifth noted deterioration. Researchers concluded that the best predictor of postoperative functioning was preoperative sexual activity: The more interested and active the woman was before surgery, the more likely she was to report satisfactory sexual function afterward. A recent decision analysis comparing the effects of total and subtotal hysterectomy echoes this finding: Sexuality before best predicts sexuality after surgery.10
The previously held belief that hysterectomy is strongly associated with depression does not appear to have been borne out. In the Finnish study, the percentage of women experiencing no postoperative symptoms of depression rose continuously during 3 years of follow-up.8 Women who reported depression before surgery also were likely to report the condition in the 2 years following surgery, although some improvement was noted 3 years after the total hysterectomy. In contrast, women with preoperative depression who underwent subtotal hysterectomy reported marked improvement in emotional well-being 6 weeks after surgery. This effect endured throughout the period of observation.8 Although it is difficult to determine the precise reason for these findings, they provide encouraging information for the patient and her physician.
Information is more limited on the effects of surgical menopause on postoperative sexual function. The impact of estrogen deficiency may be direct or indirect. Vaginal dryness and/or atrophy may make intercourse uncomfortable. Lubricants may not completely alleviate this problem, as they may be awkward and cumbersome.
Estrogen deficiency also may induce sleep disturbances, mood changes, and other factors that impair a woman’s libido and affect her enjoyment of sexual relations. And some women may experience a feeling of loss associated with organs so closely identified with femininity, resulting in an altered sense of self and sexuality.
Subtotal hysterectomy. Women who have benign disease, e.g., fibroids, endometriosis, and ovarian cysts, but do not have a history of abnormal Pap smears. Rule out the presence of malignancies in the uterus or cervix prior to surgery.
Total hysterectomy. Women who have malignant disease, including cervical, uterine, and ovarian cancers. (Note, however, if a total hysterectomy is planned and the surgeon encounters severe endometriosis or extensive cul-de-sac adhesions, switch to a subtotal hysterectomy.)
Subtotal hysterectomy
A “reverse cone”—removal of the proximal endocervical tissue—ensures excision of all endometrial tissue.
Total hysterectomy
Mobilize the bladder anteriorly, the colon posteriorly, and the ureters laterally prior to resecting the uterus and cervix.
Counseling the patient
As I mentioned at the beginning of this article, the physical and psychological make-up of each woman plays an important role in her sexuality. While surgery introduces additional factors, they are interrelated with this physical and psychological milieu. Depending on the indication for the hysterectomy and the type of procedure performed, specific outcomes can be anticipated but not predicted with any certainty.
It is my practice to discuss these issues with a woman before surgery. I review the difficulties involved in estimating her sexual functioning after surgery, emphasizing 2 important variables: her prior experiences and her expectations. I also reassure her that, with continued interest and activity, she has a very good chance of regaining or surpassing preoperative levels of sexual enjoyment. I make it a point to include her partner in these discussions, since providing the proper preoperative perspective is an invaluable part of their postoperative sexual recuperation.
Dr. Menzin reports that he is on the speakers’ bureaus for Wyeth, Ortho Biotech, and Cytyc.
1. Rhodes JC, Kjerulff KH, Langenberg PW, Guzinski GM. Hysterectomy and sexual functioning. JAMA. 1999;282:1934-1941.
2. Grimes DA. Role of the cervix in sexual response: evidence for and against. Clin Obstet Gynecol. 1999;42:972-978.
3. Munro MG, Parker WH. A classification system for laparoscopic hysterectomy. Obstet Gynecol. 1993;82:624-629.
4. Harris WJ. Complications of hysterectomy. Clin Obstet Gynecol. 1997;40:928-938.
5. Butler-Manuel SA, Buttery LDK, A’Hern RP, Polak JM, Barton DPJ. Pelvic nerve plexus trauma at radical hysterectomy and simple hysterectomy. Cancer. 2000;89:834-841.
6. Johns A. Supracervical versus total hysterectomy. Clin Obstet Gynecol. 1997;40:903-913.
7. Carlson KJ. Outcomes of hysterectomy. Clin Obstet Gynecol. 1997;40:939-946.
8. Kilkku PP. Total versus subtotal abdominal hysterectomy. In: Garcia CR, Mikuta JJ, Rosenblum NG, eds. Current Therapy in Surgical Gynecology. Toronto: BC Decker; 1987;58-61.
9. Helström L, Lundberg PO, Sörbom D, Bäckström T. Sexuality after hysterectomy: a factor analysis of women’s sexual lives before and after subtotal hysterectomy. Obstet Gynecol. 1993;81:357-362.
10. Scott JR, Sharp HT, Dodson MK, Norton PA, Warner HR. Subtotal hysterectomy in modern gynecology: a decision analysis. Am J Obstet Gynecol. 1997;176:1186-1191.
- An “internal orgasm” may be linked to sensory input from the cervix. Therefore, removal of the cervix may inhibit sexual satisfaction.
- In a study evaluating the sexual functioning of women prior to and following supracervical, or “subtotal,” hysterectomy, about half the women reported improved sexual function, one-third reported little change, and one-fifth noted deterioration.
- The more interested and sexually active a woman is preoperatively, the more likely she is to report satisfactory sexual function postoperatively.
Concerns about postoperative sexuality often top the list of questions when a woman contemplates hysterectomy.1 Unfortunately, data regarding the impact of hysterectomy on sexual function are conflicting. Further, as Grimes points out, the literature fails to elucidate the role of the cervix in sexual response.2 Thus, it is difficult to advise women which procedure is better: a total or supracervical (“subtotal”) hysterectomy. The decision must be individualized following a thorough discussion with the patient.
One factor hampering scientific evaluation of the subject is the complex and ambiguous nature of the physiologic and psychologic aspects of sexuality. Preoperative medical conditions, emotional well-being, and/or the pathologic process necessitating the hysterectomy itself may contribute to both pre- and postoperative sexual functioning, as may the nature of a woman’s personal relationships and her support system. Therefore, it is no surprise that various studies have shown improvement, stability, and deterioration in sexuality following hysterectomy.1
Technique and other factors
With approximately 600,000 procedures performed annually, hysterectomy is one of the most common operations in the United States. Indications for the procedure constitute a broad spectrum of benign and malignant gynecologic disease.
Most gynecologists in practice today were taught to remove the cervix at the time of hysterectomy. To do otherwise was a sign of surgical naiveté. Recently, however, employing a uniform and inflexible approach has been questioned. As new surgical devices and advances in minimally invasive technology make it possible to perform subtotal hysterectomy safely and expediently, the debate over the fate of the benign cervix has been rekindled. Not only are new data emerging, but patients themselves are beginning to question the physical, physiologic, and psychologic sequelae of various operative techniques and participating, to a greater extent, in the formation of a surgical plan.
For the subtotal procedure, only the fundus is amputated from the cervix.
The total procedure. First, the uterus is separated from its surrounding and supporting tissues. The ligaments within the broad ligament, as well as the ovarian and uterine vessels, are clamped, divided, and ligated at their uterine attachments. Once the dissection has reached the level of the vaginal fornices, the bladder is mobilized anteriorly, the rectosigmoid colon posteriorly, and the ureters laterally with regard to the plane of resection. The uterus and cervix are then separated from their attachments to the vagina.
The subtotal procedure. For this technique, the uterine fundus is approached as described in the total hysterectomy. However, after the uterine blood supply is controlled, only the uterine fundus is amputated from the cervix. This procedure allows for varying amounts of the proximal cervix to be removed, depending on the extent of dissection. This is determined by the indications for the hysterectomy and the intraoperative anatomic findings. (A classification system in this regard has been proposed by Munro and Parker.3) The remaining cervical stump is cauterized and its edges coapted. At the conclusion of the procedure, the cervical stump appears similar to a vaginal cuff.
In my practice, after ligating the uterine vasculature, I remove a small portion of parametrial tissue at the level of the cervical isthmus to ensure the removal of all endometrial tissue. If some of it remains, menstrual flow may continue following the procedure.
While many gynecologic surgeons amputate the fundus from the cervix by transecting the tissue in a flat plane, I find that this hinders stump closure, especially when trying to coapt the tissue. Instead, I prefer to “core out” the proximal endocervical tissue. This technique—often described as a “reverse cone”—has several advantages. It effectively ensures excision of all endometrial tissue. In addition, some researchers have hypothesized that excision and cauterization of the endocervical canal can reduce the risk of adenocarcinomas of the cervical stump. Lastly, removal of this tissue allows for reapproximation of the wound edges without tension.
Complications and physiologic considerations
All surgical procedures carry some risk of adverse sequelae. In the case of hysterectomy, sites of potential injury include the bladder, rectosigmoid colon, and ureters. In fact, Harris found complication rates of 1% to 2% associated with the bladder, 0.25% to 0.4% for the bowel, and 0.2% for the ureters.4
Besides direct trauma to adjacent organs, hysterectomy also can cause neural damage to the visceral pelvic nerves surrounding the cervix and the autonomic nerves and ganglia in the uterine ligaments.5 Although total hysterectomy disrupts these neural tracts to a greater extent than subtotal hysterectomy, some degree of injury occurs even with the less extensive procedure. This disruption is thought to be the culprit of postoperative urinary, sphincteric, and sexual dysfunction.
For women whose sexual response includes an “internal orgasm”—thought to be linked to sensory input from the cervix—removal of the cervix may have marked negative effects on sexual satisfaction. Therefore, proponents of the subtotal hysterectomy claim that the more limited resection preserves the neural pathways and, thus, physiologic function. However, Grimes argues that the presence of neural tissue in and around the cervix does not necessarily mean that it is functional.2
Other potential deleterious effects of complete cervical excision include the development of scar or granulation tissue at the vaginal apex and the possible shortening of the vagina. It is not clear from the current literature whether complete cervical excision increases the risk of vaginal-vault or pelvic-floor prolapse.6
Effects on sexuality
Using data from the Maine Women’s Health Study, Carlson and colleagues found marked improvements in symptomatology, including reduced rates of sexual dysfunction, when hysterectomy was performed for fibroids, bleeding, or pain.7 They concluded that hysterectomy was associated with an overall improvement in the quality of life. New problems were limited, with only 7% of patients reporting a loss of interest in sex following surgery.
A report from the Maryland Women’s Health Study noted that rates of dyspareunia decreased following hysterectomy and that measures of sexual activity, libido, and orgasmic function increased.1 These improvements were thought to result from removal of the offending pathology and freedom from conception concerns.
Unfortunately, neither the Maine nor the Maryland studies assessed the effects of the type of hysterectomy on outcomes. However, a prospective study from Finland did. The result? Measures of sexual function, libido, and coital frequency did not differ statistically between women in the 2 groups—either preoperatively or 1 year postoperatively.8
However, the percentages of women reporting reduced orgasmic function did increase significantly over the year following surgery among women who had a total hysterectomy but did not change appreciably in the subtotal cohort. Dyspareunia occurred less often in both groups but to a greater extent in women who had a subtotal hysterectomy.
When Helström and colleagues from Sweden reported their evaluation of the sexual lives of women prior to and following subtotal hysterectomy, they found varied results.9 Approximately half the women surveyed reported improved sexuality after surgery, nearly one-third reported little change, and one-fifth noted deterioration. Researchers concluded that the best predictor of postoperative functioning was preoperative sexual activity: The more interested and active the woman was before surgery, the more likely she was to report satisfactory sexual function afterward. A recent decision analysis comparing the effects of total and subtotal hysterectomy echoes this finding: Sexuality before best predicts sexuality after surgery.10
The previously held belief that hysterectomy is strongly associated with depression does not appear to have been borne out. In the Finnish study, the percentage of women experiencing no postoperative symptoms of depression rose continuously during 3 years of follow-up.8 Women who reported depression before surgery also were likely to report the condition in the 2 years following surgery, although some improvement was noted 3 years after the total hysterectomy. In contrast, women with preoperative depression who underwent subtotal hysterectomy reported marked improvement in emotional well-being 6 weeks after surgery. This effect endured throughout the period of observation.8 Although it is difficult to determine the precise reason for these findings, they provide encouraging information for the patient and her physician.
Information is more limited on the effects of surgical menopause on postoperative sexual function. The impact of estrogen deficiency may be direct or indirect. Vaginal dryness and/or atrophy may make intercourse uncomfortable. Lubricants may not completely alleviate this problem, as they may be awkward and cumbersome.
Estrogen deficiency also may induce sleep disturbances, mood changes, and other factors that impair a woman’s libido and affect her enjoyment of sexual relations. And some women may experience a feeling of loss associated with organs so closely identified with femininity, resulting in an altered sense of self and sexuality.
Subtotal hysterectomy. Women who have benign disease, e.g., fibroids, endometriosis, and ovarian cysts, but do not have a history of abnormal Pap smears. Rule out the presence of malignancies in the uterus or cervix prior to surgery.
Total hysterectomy. Women who have malignant disease, including cervical, uterine, and ovarian cancers. (Note, however, if a total hysterectomy is planned and the surgeon encounters severe endometriosis or extensive cul-de-sac adhesions, switch to a subtotal hysterectomy.)
Subtotal hysterectomy
A “reverse cone”—removal of the proximal endocervical tissue—ensures excision of all endometrial tissue.
Total hysterectomy
Mobilize the bladder anteriorly, the colon posteriorly, and the ureters laterally prior to resecting the uterus and cervix.
Counseling the patient
As I mentioned at the beginning of this article, the physical and psychological make-up of each woman plays an important role in her sexuality. While surgery introduces additional factors, they are interrelated with this physical and psychological milieu. Depending on the indication for the hysterectomy and the type of procedure performed, specific outcomes can be anticipated but not predicted with any certainty.
It is my practice to discuss these issues with a woman before surgery. I review the difficulties involved in estimating her sexual functioning after surgery, emphasizing 2 important variables: her prior experiences and her expectations. I also reassure her that, with continued interest and activity, she has a very good chance of regaining or surpassing preoperative levels of sexual enjoyment. I make it a point to include her partner in these discussions, since providing the proper preoperative perspective is an invaluable part of their postoperative sexual recuperation.
Dr. Menzin reports that he is on the speakers’ bureaus for Wyeth, Ortho Biotech, and Cytyc.
- An “internal orgasm” may be linked to sensory input from the cervix. Therefore, removal of the cervix may inhibit sexual satisfaction.
- In a study evaluating the sexual functioning of women prior to and following supracervical, or “subtotal,” hysterectomy, about half the women reported improved sexual function, one-third reported little change, and one-fifth noted deterioration.
- The more interested and sexually active a woman is preoperatively, the more likely she is to report satisfactory sexual function postoperatively.
Concerns about postoperative sexuality often top the list of questions when a woman contemplates hysterectomy.1 Unfortunately, data regarding the impact of hysterectomy on sexual function are conflicting. Further, as Grimes points out, the literature fails to elucidate the role of the cervix in sexual response.2 Thus, it is difficult to advise women which procedure is better: a total or supracervical (“subtotal”) hysterectomy. The decision must be individualized following a thorough discussion with the patient.
One factor hampering scientific evaluation of the subject is the complex and ambiguous nature of the physiologic and psychologic aspects of sexuality. Preoperative medical conditions, emotional well-being, and/or the pathologic process necessitating the hysterectomy itself may contribute to both pre- and postoperative sexual functioning, as may the nature of a woman’s personal relationships and her support system. Therefore, it is no surprise that various studies have shown improvement, stability, and deterioration in sexuality following hysterectomy.1
Technique and other factors
With approximately 600,000 procedures performed annually, hysterectomy is one of the most common operations in the United States. Indications for the procedure constitute a broad spectrum of benign and malignant gynecologic disease.
Most gynecologists in practice today were taught to remove the cervix at the time of hysterectomy. To do otherwise was a sign of surgical naiveté. Recently, however, employing a uniform and inflexible approach has been questioned. As new surgical devices and advances in minimally invasive technology make it possible to perform subtotal hysterectomy safely and expediently, the debate over the fate of the benign cervix has been rekindled. Not only are new data emerging, but patients themselves are beginning to question the physical, physiologic, and psychologic sequelae of various operative techniques and participating, to a greater extent, in the formation of a surgical plan.
For the subtotal procedure, only the fundus is amputated from the cervix.
The total procedure. First, the uterus is separated from its surrounding and supporting tissues. The ligaments within the broad ligament, as well as the ovarian and uterine vessels, are clamped, divided, and ligated at their uterine attachments. Once the dissection has reached the level of the vaginal fornices, the bladder is mobilized anteriorly, the rectosigmoid colon posteriorly, and the ureters laterally with regard to the plane of resection. The uterus and cervix are then separated from their attachments to the vagina.
The subtotal procedure. For this technique, the uterine fundus is approached as described in the total hysterectomy. However, after the uterine blood supply is controlled, only the uterine fundus is amputated from the cervix. This procedure allows for varying amounts of the proximal cervix to be removed, depending on the extent of dissection. This is determined by the indications for the hysterectomy and the intraoperative anatomic findings. (A classification system in this regard has been proposed by Munro and Parker.3) The remaining cervical stump is cauterized and its edges coapted. At the conclusion of the procedure, the cervical stump appears similar to a vaginal cuff.
In my practice, after ligating the uterine vasculature, I remove a small portion of parametrial tissue at the level of the cervical isthmus to ensure the removal of all endometrial tissue. If some of it remains, menstrual flow may continue following the procedure.
While many gynecologic surgeons amputate the fundus from the cervix by transecting the tissue in a flat plane, I find that this hinders stump closure, especially when trying to coapt the tissue. Instead, I prefer to “core out” the proximal endocervical tissue. This technique—often described as a “reverse cone”—has several advantages. It effectively ensures excision of all endometrial tissue. In addition, some researchers have hypothesized that excision and cauterization of the endocervical canal can reduce the risk of adenocarcinomas of the cervical stump. Lastly, removal of this tissue allows for reapproximation of the wound edges without tension.
Complications and physiologic considerations
All surgical procedures carry some risk of adverse sequelae. In the case of hysterectomy, sites of potential injury include the bladder, rectosigmoid colon, and ureters. In fact, Harris found complication rates of 1% to 2% associated with the bladder, 0.25% to 0.4% for the bowel, and 0.2% for the ureters.4
Besides direct trauma to adjacent organs, hysterectomy also can cause neural damage to the visceral pelvic nerves surrounding the cervix and the autonomic nerves and ganglia in the uterine ligaments.5 Although total hysterectomy disrupts these neural tracts to a greater extent than subtotal hysterectomy, some degree of injury occurs even with the less extensive procedure. This disruption is thought to be the culprit of postoperative urinary, sphincteric, and sexual dysfunction.
For women whose sexual response includes an “internal orgasm”—thought to be linked to sensory input from the cervix—removal of the cervix may have marked negative effects on sexual satisfaction. Therefore, proponents of the subtotal hysterectomy claim that the more limited resection preserves the neural pathways and, thus, physiologic function. However, Grimes argues that the presence of neural tissue in and around the cervix does not necessarily mean that it is functional.2
Other potential deleterious effects of complete cervical excision include the development of scar or granulation tissue at the vaginal apex and the possible shortening of the vagina. It is not clear from the current literature whether complete cervical excision increases the risk of vaginal-vault or pelvic-floor prolapse.6
Effects on sexuality
Using data from the Maine Women’s Health Study, Carlson and colleagues found marked improvements in symptomatology, including reduced rates of sexual dysfunction, when hysterectomy was performed for fibroids, bleeding, or pain.7 They concluded that hysterectomy was associated with an overall improvement in the quality of life. New problems were limited, with only 7% of patients reporting a loss of interest in sex following surgery.
A report from the Maryland Women’s Health Study noted that rates of dyspareunia decreased following hysterectomy and that measures of sexual activity, libido, and orgasmic function increased.1 These improvements were thought to result from removal of the offending pathology and freedom from conception concerns.
Unfortunately, neither the Maine nor the Maryland studies assessed the effects of the type of hysterectomy on outcomes. However, a prospective study from Finland did. The result? Measures of sexual function, libido, and coital frequency did not differ statistically between women in the 2 groups—either preoperatively or 1 year postoperatively.8
However, the percentages of women reporting reduced orgasmic function did increase significantly over the year following surgery among women who had a total hysterectomy but did not change appreciably in the subtotal cohort. Dyspareunia occurred less often in both groups but to a greater extent in women who had a subtotal hysterectomy.
When Helström and colleagues from Sweden reported their evaluation of the sexual lives of women prior to and following subtotal hysterectomy, they found varied results.9 Approximately half the women surveyed reported improved sexuality after surgery, nearly one-third reported little change, and one-fifth noted deterioration. Researchers concluded that the best predictor of postoperative functioning was preoperative sexual activity: The more interested and active the woman was before surgery, the more likely she was to report satisfactory sexual function afterward. A recent decision analysis comparing the effects of total and subtotal hysterectomy echoes this finding: Sexuality before best predicts sexuality after surgery.10
The previously held belief that hysterectomy is strongly associated with depression does not appear to have been borne out. In the Finnish study, the percentage of women experiencing no postoperative symptoms of depression rose continuously during 3 years of follow-up.8 Women who reported depression before surgery also were likely to report the condition in the 2 years following surgery, although some improvement was noted 3 years after the total hysterectomy. In contrast, women with preoperative depression who underwent subtotal hysterectomy reported marked improvement in emotional well-being 6 weeks after surgery. This effect endured throughout the period of observation.8 Although it is difficult to determine the precise reason for these findings, they provide encouraging information for the patient and her physician.
Information is more limited on the effects of surgical menopause on postoperative sexual function. The impact of estrogen deficiency may be direct or indirect. Vaginal dryness and/or atrophy may make intercourse uncomfortable. Lubricants may not completely alleviate this problem, as they may be awkward and cumbersome.
Estrogen deficiency also may induce sleep disturbances, mood changes, and other factors that impair a woman’s libido and affect her enjoyment of sexual relations. And some women may experience a feeling of loss associated with organs so closely identified with femininity, resulting in an altered sense of self and sexuality.
Subtotal hysterectomy. Women who have benign disease, e.g., fibroids, endometriosis, and ovarian cysts, but do not have a history of abnormal Pap smears. Rule out the presence of malignancies in the uterus or cervix prior to surgery.
Total hysterectomy. Women who have malignant disease, including cervical, uterine, and ovarian cancers. (Note, however, if a total hysterectomy is planned and the surgeon encounters severe endometriosis or extensive cul-de-sac adhesions, switch to a subtotal hysterectomy.)
Subtotal hysterectomy
A “reverse cone”—removal of the proximal endocervical tissue—ensures excision of all endometrial tissue.
Total hysterectomy
Mobilize the bladder anteriorly, the colon posteriorly, and the ureters laterally prior to resecting the uterus and cervix.
Counseling the patient
As I mentioned at the beginning of this article, the physical and psychological make-up of each woman plays an important role in her sexuality. While surgery introduces additional factors, they are interrelated with this physical and psychological milieu. Depending on the indication for the hysterectomy and the type of procedure performed, specific outcomes can be anticipated but not predicted with any certainty.
It is my practice to discuss these issues with a woman before surgery. I review the difficulties involved in estimating her sexual functioning after surgery, emphasizing 2 important variables: her prior experiences and her expectations. I also reassure her that, with continued interest and activity, she has a very good chance of regaining or surpassing preoperative levels of sexual enjoyment. I make it a point to include her partner in these discussions, since providing the proper preoperative perspective is an invaluable part of their postoperative sexual recuperation.
Dr. Menzin reports that he is on the speakers’ bureaus for Wyeth, Ortho Biotech, and Cytyc.
1. Rhodes JC, Kjerulff KH, Langenberg PW, Guzinski GM. Hysterectomy and sexual functioning. JAMA. 1999;282:1934-1941.
2. Grimes DA. Role of the cervix in sexual response: evidence for and against. Clin Obstet Gynecol. 1999;42:972-978.
3. Munro MG, Parker WH. A classification system for laparoscopic hysterectomy. Obstet Gynecol. 1993;82:624-629.
4. Harris WJ. Complications of hysterectomy. Clin Obstet Gynecol. 1997;40:928-938.
5. Butler-Manuel SA, Buttery LDK, A’Hern RP, Polak JM, Barton DPJ. Pelvic nerve plexus trauma at radical hysterectomy and simple hysterectomy. Cancer. 2000;89:834-841.
6. Johns A. Supracervical versus total hysterectomy. Clin Obstet Gynecol. 1997;40:903-913.
7. Carlson KJ. Outcomes of hysterectomy. Clin Obstet Gynecol. 1997;40:939-946.
8. Kilkku PP. Total versus subtotal abdominal hysterectomy. In: Garcia CR, Mikuta JJ, Rosenblum NG, eds. Current Therapy in Surgical Gynecology. Toronto: BC Decker; 1987;58-61.
9. Helström L, Lundberg PO, Sörbom D, Bäckström T. Sexuality after hysterectomy: a factor analysis of women’s sexual lives before and after subtotal hysterectomy. Obstet Gynecol. 1993;81:357-362.
10. Scott JR, Sharp HT, Dodson MK, Norton PA, Warner HR. Subtotal hysterectomy in modern gynecology: a decision analysis. Am J Obstet Gynecol. 1997;176:1186-1191.
1. Rhodes JC, Kjerulff KH, Langenberg PW, Guzinski GM. Hysterectomy and sexual functioning. JAMA. 1999;282:1934-1941.
2. Grimes DA. Role of the cervix in sexual response: evidence for and against. Clin Obstet Gynecol. 1999;42:972-978.
3. Munro MG, Parker WH. A classification system for laparoscopic hysterectomy. Obstet Gynecol. 1993;82:624-629.
4. Harris WJ. Complications of hysterectomy. Clin Obstet Gynecol. 1997;40:928-938.
5. Butler-Manuel SA, Buttery LDK, A’Hern RP, Polak JM, Barton DPJ. Pelvic nerve plexus trauma at radical hysterectomy and simple hysterectomy. Cancer. 2000;89:834-841.
6. Johns A. Supracervical versus total hysterectomy. Clin Obstet Gynecol. 1997;40:903-913.
7. Carlson KJ. Outcomes of hysterectomy. Clin Obstet Gynecol. 1997;40:939-946.
8. Kilkku PP. Total versus subtotal abdominal hysterectomy. In: Garcia CR, Mikuta JJ, Rosenblum NG, eds. Current Therapy in Surgical Gynecology. Toronto: BC Decker; 1987;58-61.
9. Helström L, Lundberg PO, Sörbom D, Bäckström T. Sexuality after hysterectomy: a factor analysis of women’s sexual lives before and after subtotal hysterectomy. Obstet Gynecol. 1993;81:357-362.
10. Scott JR, Sharp HT, Dodson MK, Norton PA, Warner HR. Subtotal hysterectomy in modern gynecology: a decision analysis. Am J Obstet Gynecol. 1997;176:1186-1191.