User login
The relationships among inflammation, Alzheimer disease, and depression have been the subject of recent research at several centers. Alzheimer disease and depression appear to be linked by several genetic and inflammatory processes, although the exact nature of the relationship is not clearly understood. The two disorders also share risk factors for vascular disease. This article reviews the current state of knowledge about inflammation and its implications for Alzheimer disease and depression, and it presents recent findings from the Texas Alzheimer’s Research Consortium, which assessed an array of inflammatory markers in a cohort of patients with Alzheimer disease.
INFLAMMATION MAY MEDIATE DEPRESSION, COGNITIVE DECLINE, AND DEMENTIA
Alzheimer disease and depression share several vascular disease risk factors and appear to be linked through complex and integrated processes. The link may be mediated by long-term inflammatory processes. Hypothalamic-pituitary-adrenal (HPA) axis dysfunction, chronic inflammation, and a deficit in neurotrophin signaling all may play roles in the pathogenesis of depression and Alzheimer disease.1 Excessive release of glucocorticoids subsequent to HPA-axis dysfunction in chronic depression appears to damage the hippocampus: hippocampal atrophy is a feature in both depression and dementia, and recurrent depression is associated with greater atrophy. The direction of influence—whether depression leads to the factors that increase the risk of Alzheimer disease or the other way around—remains a controversial topic.
Symptoms of depression tend to appear early in Alzheimer disease and increase as dementia progresses to moderate severity. In advanced dementia, depression symptoms tend to decline, although this may reflect the difficulty in assessing depression at advanced stages of dementia.2
Numerous reports have linked inflammation to cognitive dysfunction or decline, as well as to the development of Alzheimer disease.3–5 Evidence suggests that inflammation is a key mediator between cardiovascular risk factors and Alzheimer disease, although this is also still controversial.
FINDINGS FROM THE TEXAS ALZHEIMER’S RESEARCH CONSORTIUM
The Texas Alzheimer’s Research Consortium, composed of five medical centers, is pursuing a longitudinal, multi-institutional study of Alzheimer disease. The group recently published the results of a study assessing whether inflammatory markers were over- or underexpressed in patients with Alzheimer disease, and whether biomarkers could predict Alzheimer disease status and the age at onset of the disease.4 The analysis included 197 patients with Alzheimer disease and 203 control subjects. The evaluation consisted of cognitive assessment, DNA analysis for human genome-wide association studies, and protein microarray analysis from blood. Cardiovascular risk factors were also measured, including serum lipids and blood factors for diabetes risk. The goal was to better understand the pathophysiology of cognitive decline and predict conversion of mild cognitive impairment to Alzheimer disease.
Significant differences were found in the study groups. For example, the median age in the Alzheimer group was significantly higher than in controls (79 vs 70 years, P < .0001), an issue that is being addressed as subjects are replaced due to attrition. The median educational level was higher in the control group (14 vs 16 years, P < .0001) than in the Alzheimer group. Subjects in the Alzheimer group were significantly more likely (P < .001) to carry at least one copy of the APOE ε4 allele.
Inflammation is associated with Alzheimer disease
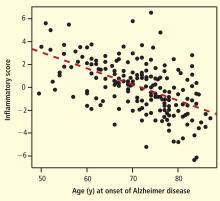
Degree of inflammation also correlated with Mini-Mental State Examination (MMSE) scores. Subjects with a high inflammatory score had a more accelerated decline in MMSE scores over a 3-year period than those with a low inflammatory score. The association was significant, although not as dramatic as the association between inflammation and age at onset of Alzheimer disease.
The investigators concluded that their findings, while considered preliminary, suggest the existence of an inflammatory endophenotype associated with Alzheimer disease. The findings need to be validated in other populations, including ethnic groups other than Caucasian. The Consortium also will evaluate whether inflammatory biomarkers are associated with progression of mild cognitive impairment to Alzheimer disease.
Inflammation has a mixed association with depression
In a study whose results are not yet published, the Texas Consortium also examined the association between inflammatory markers and depression. Four subscales of depression were used, derived from the Geriatric Depression Scale (GDS) 30: dysphoria (consisting of 11 items), meaninglessness (seven items), apathy and withdrawal (six items), and cognitive impairment (six items).5
The GDS30 results as a whole suggested a trend toward an association between depression and inflammatory biomarkers, but the association was not significant. When the results were examined by subscale, however, striking differences were found between Alzheimer patients and the control group. For example, apathy was significantly associated with the C-reactive protein level, and the assocation was much stronger in patients with Alzheimer disease than in controls. Further, the association of apathy with C-reactive protein level was more significant in women than in men.
Other associations were found between several of the inflammatory and antiinflammatory cytokines and the various subscales; the relationship between inflammatory factors and depression appears to be complex and often gender-specific.
Inflammation-depression link is suggestive, not linear
Despite the relationships suggested by the data, no simple linear relationship was identified to indicate that more inflammation leads to more depression in Alzheimer disease. The relationship between inflammation and depression in Alzheimer disease appears to involve a complex interplay between many physiologic processes.
The effect of inflammation also varies with gender and with cognitive impairment. The mechanism that underlies these relationships remains to be determined and will be the focus of further studies with the Texas Alzheimer’s Research Consortium.
- Caraci F, Copani A, Nicoletti F, Drago F. Depression and Alzheimer’s disease: neurobiological links and common pharmacological targets. Eur J Pharmacol 2010; 626:64–71.
- Amore M, Tagariello P, Laterza C, Savoia EM. Subtypes of depression in dementia. Arch Gerontol Geriatr 2007; 44( suppl 1):23–33.
- O’Bryant SE, Xiao G, Barber R, et al., Texas Alzheimer’s Research Consortium. A serum protein-based algorithm for the detection of Alzheimer disease. Arch Neurol 2010; 67:1077–1081.
- Barber R, Xiao G, O’Bryant S, et al., Texas Alzheimer’s Research Consortium. An inflammatory endophenotype of Alzheimer’s disease. Alzheim Dement 2010; 6( suppl):S530.
- Hall JR, Davis TE. Factor structure of the Geriatric Depression Scale in cognitively impaired older adults. Clin Gerontol 2010; 33:39–48.
The relationships among inflammation, Alzheimer disease, and depression have been the subject of recent research at several centers. Alzheimer disease and depression appear to be linked by several genetic and inflammatory processes, although the exact nature of the relationship is not clearly understood. The two disorders also share risk factors for vascular disease. This article reviews the current state of knowledge about inflammation and its implications for Alzheimer disease and depression, and it presents recent findings from the Texas Alzheimer’s Research Consortium, which assessed an array of inflammatory markers in a cohort of patients with Alzheimer disease.
INFLAMMATION MAY MEDIATE DEPRESSION, COGNITIVE DECLINE, AND DEMENTIA
Alzheimer disease and depression share several vascular disease risk factors and appear to be linked through complex and integrated processes. The link may be mediated by long-term inflammatory processes. Hypothalamic-pituitary-adrenal (HPA) axis dysfunction, chronic inflammation, and a deficit in neurotrophin signaling all may play roles in the pathogenesis of depression and Alzheimer disease.1 Excessive release of glucocorticoids subsequent to HPA-axis dysfunction in chronic depression appears to damage the hippocampus: hippocampal atrophy is a feature in both depression and dementia, and recurrent depression is associated with greater atrophy. The direction of influence—whether depression leads to the factors that increase the risk of Alzheimer disease or the other way around—remains a controversial topic.
Symptoms of depression tend to appear early in Alzheimer disease and increase as dementia progresses to moderate severity. In advanced dementia, depression symptoms tend to decline, although this may reflect the difficulty in assessing depression at advanced stages of dementia.2
Numerous reports have linked inflammation to cognitive dysfunction or decline, as well as to the development of Alzheimer disease.3–5 Evidence suggests that inflammation is a key mediator between cardiovascular risk factors and Alzheimer disease, although this is also still controversial.
FINDINGS FROM THE TEXAS ALZHEIMER’S RESEARCH CONSORTIUM
The Texas Alzheimer’s Research Consortium, composed of five medical centers, is pursuing a longitudinal, multi-institutional study of Alzheimer disease. The group recently published the results of a study assessing whether inflammatory markers were over- or underexpressed in patients with Alzheimer disease, and whether biomarkers could predict Alzheimer disease status and the age at onset of the disease.4 The analysis included 197 patients with Alzheimer disease and 203 control subjects. The evaluation consisted of cognitive assessment, DNA analysis for human genome-wide association studies, and protein microarray analysis from blood. Cardiovascular risk factors were also measured, including serum lipids and blood factors for diabetes risk. The goal was to better understand the pathophysiology of cognitive decline and predict conversion of mild cognitive impairment to Alzheimer disease.
Significant differences were found in the study groups. For example, the median age in the Alzheimer group was significantly higher than in controls (79 vs 70 years, P < .0001), an issue that is being addressed as subjects are replaced due to attrition. The median educational level was higher in the control group (14 vs 16 years, P < .0001) than in the Alzheimer group. Subjects in the Alzheimer group were significantly more likely (P < .001) to carry at least one copy of the APOE ε4 allele.
Inflammation is associated with Alzheimer disease
Degree of inflammation also correlated with Mini-Mental State Examination (MMSE) scores. Subjects with a high inflammatory score had a more accelerated decline in MMSE scores over a 3-year period than those with a low inflammatory score. The association was significant, although not as dramatic as the association between inflammation and age at onset of Alzheimer disease.
The investigators concluded that their findings, while considered preliminary, suggest the existence of an inflammatory endophenotype associated with Alzheimer disease. The findings need to be validated in other populations, including ethnic groups other than Caucasian. The Consortium also will evaluate whether inflammatory biomarkers are associated with progression of mild cognitive impairment to Alzheimer disease.
Inflammation has a mixed association with depression
In a study whose results are not yet published, the Texas Consortium also examined the association between inflammatory markers and depression. Four subscales of depression were used, derived from the Geriatric Depression Scale (GDS) 30: dysphoria (consisting of 11 items), meaninglessness (seven items), apathy and withdrawal (six items), and cognitive impairment (six items).5
The GDS30 results as a whole suggested a trend toward an association between depression and inflammatory biomarkers, but the association was not significant. When the results were examined by subscale, however, striking differences were found between Alzheimer patients and the control group. For example, apathy was significantly associated with the C-reactive protein level, and the assocation was much stronger in patients with Alzheimer disease than in controls. Further, the association of apathy with C-reactive protein level was more significant in women than in men.
Other associations were found between several of the inflammatory and antiinflammatory cytokines and the various subscales; the relationship between inflammatory factors and depression appears to be complex and often gender-specific.
Inflammation-depression link is suggestive, not linear
Despite the relationships suggested by the data, no simple linear relationship was identified to indicate that more inflammation leads to more depression in Alzheimer disease. The relationship between inflammation and depression in Alzheimer disease appears to involve a complex interplay between many physiologic processes.
The effect of inflammation also varies with gender and with cognitive impairment. The mechanism that underlies these relationships remains to be determined and will be the focus of further studies with the Texas Alzheimer’s Research Consortium.
The relationships among inflammation, Alzheimer disease, and depression have been the subject of recent research at several centers. Alzheimer disease and depression appear to be linked by several genetic and inflammatory processes, although the exact nature of the relationship is not clearly understood. The two disorders also share risk factors for vascular disease. This article reviews the current state of knowledge about inflammation and its implications for Alzheimer disease and depression, and it presents recent findings from the Texas Alzheimer’s Research Consortium, which assessed an array of inflammatory markers in a cohort of patients with Alzheimer disease.
INFLAMMATION MAY MEDIATE DEPRESSION, COGNITIVE DECLINE, AND DEMENTIA
Alzheimer disease and depression share several vascular disease risk factors and appear to be linked through complex and integrated processes. The link may be mediated by long-term inflammatory processes. Hypothalamic-pituitary-adrenal (HPA) axis dysfunction, chronic inflammation, and a deficit in neurotrophin signaling all may play roles in the pathogenesis of depression and Alzheimer disease.1 Excessive release of glucocorticoids subsequent to HPA-axis dysfunction in chronic depression appears to damage the hippocampus: hippocampal atrophy is a feature in both depression and dementia, and recurrent depression is associated with greater atrophy. The direction of influence—whether depression leads to the factors that increase the risk of Alzheimer disease or the other way around—remains a controversial topic.
Symptoms of depression tend to appear early in Alzheimer disease and increase as dementia progresses to moderate severity. In advanced dementia, depression symptoms tend to decline, although this may reflect the difficulty in assessing depression at advanced stages of dementia.2
Numerous reports have linked inflammation to cognitive dysfunction or decline, as well as to the development of Alzheimer disease.3–5 Evidence suggests that inflammation is a key mediator between cardiovascular risk factors and Alzheimer disease, although this is also still controversial.
FINDINGS FROM THE TEXAS ALZHEIMER’S RESEARCH CONSORTIUM
The Texas Alzheimer’s Research Consortium, composed of five medical centers, is pursuing a longitudinal, multi-institutional study of Alzheimer disease. The group recently published the results of a study assessing whether inflammatory markers were over- or underexpressed in patients with Alzheimer disease, and whether biomarkers could predict Alzheimer disease status and the age at onset of the disease.4 The analysis included 197 patients with Alzheimer disease and 203 control subjects. The evaluation consisted of cognitive assessment, DNA analysis for human genome-wide association studies, and protein microarray analysis from blood. Cardiovascular risk factors were also measured, including serum lipids and blood factors for diabetes risk. The goal was to better understand the pathophysiology of cognitive decline and predict conversion of mild cognitive impairment to Alzheimer disease.
Significant differences were found in the study groups. For example, the median age in the Alzheimer group was significantly higher than in controls (79 vs 70 years, P < .0001), an issue that is being addressed as subjects are replaced due to attrition. The median educational level was higher in the control group (14 vs 16 years, P < .0001) than in the Alzheimer group. Subjects in the Alzheimer group were significantly more likely (P < .001) to carry at least one copy of the APOE ε4 allele.
Inflammation is associated with Alzheimer disease
Degree of inflammation also correlated with Mini-Mental State Examination (MMSE) scores. Subjects with a high inflammatory score had a more accelerated decline in MMSE scores over a 3-year period than those with a low inflammatory score. The association was significant, although not as dramatic as the association between inflammation and age at onset of Alzheimer disease.
The investigators concluded that their findings, while considered preliminary, suggest the existence of an inflammatory endophenotype associated with Alzheimer disease. The findings need to be validated in other populations, including ethnic groups other than Caucasian. The Consortium also will evaluate whether inflammatory biomarkers are associated with progression of mild cognitive impairment to Alzheimer disease.
Inflammation has a mixed association with depression
In a study whose results are not yet published, the Texas Consortium also examined the association between inflammatory markers and depression. Four subscales of depression were used, derived from the Geriatric Depression Scale (GDS) 30: dysphoria (consisting of 11 items), meaninglessness (seven items), apathy and withdrawal (six items), and cognitive impairment (six items).5
The GDS30 results as a whole suggested a trend toward an association between depression and inflammatory biomarkers, but the association was not significant. When the results were examined by subscale, however, striking differences were found between Alzheimer patients and the control group. For example, apathy was significantly associated with the C-reactive protein level, and the assocation was much stronger in patients with Alzheimer disease than in controls. Further, the association of apathy with C-reactive protein level was more significant in women than in men.
Other associations were found between several of the inflammatory and antiinflammatory cytokines and the various subscales; the relationship between inflammatory factors and depression appears to be complex and often gender-specific.
Inflammation-depression link is suggestive, not linear
Despite the relationships suggested by the data, no simple linear relationship was identified to indicate that more inflammation leads to more depression in Alzheimer disease. The relationship between inflammation and depression in Alzheimer disease appears to involve a complex interplay between many physiologic processes.
The effect of inflammation also varies with gender and with cognitive impairment. The mechanism that underlies these relationships remains to be determined and will be the focus of further studies with the Texas Alzheimer’s Research Consortium.
- Caraci F, Copani A, Nicoletti F, Drago F. Depression and Alzheimer’s disease: neurobiological links and common pharmacological targets. Eur J Pharmacol 2010; 626:64–71.
- Amore M, Tagariello P, Laterza C, Savoia EM. Subtypes of depression in dementia. Arch Gerontol Geriatr 2007; 44( suppl 1):23–33.
- O’Bryant SE, Xiao G, Barber R, et al., Texas Alzheimer’s Research Consortium. A serum protein-based algorithm for the detection of Alzheimer disease. Arch Neurol 2010; 67:1077–1081.
- Barber R, Xiao G, O’Bryant S, et al., Texas Alzheimer’s Research Consortium. An inflammatory endophenotype of Alzheimer’s disease. Alzheim Dement 2010; 6( suppl):S530.
- Hall JR, Davis TE. Factor structure of the Geriatric Depression Scale in cognitively impaired older adults. Clin Gerontol 2010; 33:39–48.
- Caraci F, Copani A, Nicoletti F, Drago F. Depression and Alzheimer’s disease: neurobiological links and common pharmacological targets. Eur J Pharmacol 2010; 626:64–71.
- Amore M, Tagariello P, Laterza C, Savoia EM. Subtypes of depression in dementia. Arch Gerontol Geriatr 2007; 44( suppl 1):23–33.
- O’Bryant SE, Xiao G, Barber R, et al., Texas Alzheimer’s Research Consortium. A serum protein-based algorithm for the detection of Alzheimer disease. Arch Neurol 2010; 67:1077–1081.
- Barber R, Xiao G, O’Bryant S, et al., Texas Alzheimer’s Research Consortium. An inflammatory endophenotype of Alzheimer’s disease. Alzheim Dement 2010; 6( suppl):S530.
- Hall JR, Davis TE. Factor structure of the Geriatric Depression Scale in cognitively impaired older adults. Clin Gerontol 2010; 33:39–48.