User login
ANNAPOLIS, MD – Numerous suicide risk-assessment tools are available, but because none are perfect, the ability to prevent inpatient suicide hinges on a single factor, according to Dr. Robert P. Roca.
"It all comes down to clinical judgment. How do we guide clinical judgment?" Dr. Roca, vice president of medical affairs at Sheppard and Enoch Pratt Hospital, Towson, Md., asked at the annual meeting of the Southern Psychiatric Association. Basically, "it’s a synthetic clinical judgment that involves taking into account a whole lot of factors, and there’s really no test that tells us reliably what the answer is to this person’s risk."
About 5 years ago, Dr. Roca said, the Sheppard Pratt Health System looked retrospectively at its experience with inpatient suicide in its family and inpatient programs.
They found that men and women are equally likely to make serious attempts. Interestingly, the elderly were not disproportionately at risk. Nearly half of attempts occurred in the first 3 days; however, some attempts occurred when a patient appeared ready for discharge. Most patients who made serious attempts at suicide had unipolar or bipolar depression. Importantly, patients usually attempted hanging from a bedroom or bathroom door using bed linens or clothing.
Because attempts occur most often in bedrooms and bathrooms, careful design is needed to eliminate many hazards, such as using breakaway fixtures or down-sloping fixtures and avoiding breakable glass materials. "But a door is a potential gallows ... that was the vivid message that came across," he said. However, self-asphyxiation does not require hanging, and practically anything can become an instrument of self-harm.
"The most important message for me was that people who attempted suicide didn’t warn you in advance that they were going to do that," Dr. Roca said. "Certainly, a safety contract is no guarantee of safety."
Based on careful review of the records of patients who succeeded in committing suicide as an inpatient, the researchers identified several salient features of the mental status of these patients. These included intense psychological pain or anguish, intense self-loathing, delusions of guilt, agitation or perturbation, hopelessness, and a feeling that death would bring relief.
Universal precautions for these patients might include a physical environment that is safe yet therapeutically warm and a clinical milieu that inspires hope and rapidly relieves psychological distress, he said.
"You also need to be able to identify people who are at very, very high risk" and require special risk assessment. Early scales were simply inventories of demographic risk factors with limited evidence of reliability or validity. Subsequent scales were better researched, and included scales –such as the Beck Scale for Suicidal Ideation – with good reliability and validity but poor predictive value. Other scales were lengthy research tools that were impractical for clinical use and not designed to evaluate immediate risk.
More practical tools are available, but these are not perfect, either. The Nurses’ Global Assessment of Suicide Risk is a 15-item nurse-rated checklist. Scoring gives special weight to hopelessness, anhedonia, recent bereavement, and prior attempts. On this assessment, greater scores call for higher levels of engagement.
The Positive and Negative Suicidal Ideation Inventory (J. of Clin. Psychol. 2005;61:431-45) includes 14 items: eight "risk factors" and six "protective factors." Scoring uses a 5-point Likert scale. It has been validated in the adolescent and young adult populations in the Midwest, though it hasn’t been more broadly validated.
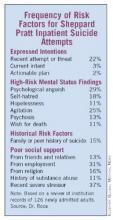
The clinicians at Sheppard Pratt have developed and are using their own assessment – the Sheppard Pratt Suicide Risk Assessment (SPSRA) – which includes 13 questions and three domains of risk: expressed intentions regarding suicide, mental status findings pertinent to risk, and aspects of history pertinent to risk. However, it is not a quantitative scale. The answers prompt clinicians to consider all three domains – not just expressed intentions – in their estimates of risk. The presence of any of these may increase suicide risk.
"The most important message for me was that people who attempted suicide didn’t warn you in advance that they were going to do that."
In terms of expressed intentions, these are important questions: Has there been a recent suicide attempt? Is there imminent suicide intent? Is there an actionable plan (a patient could realistically act upon this while in hospital)? If the answer to any of these three questions is yes, a high level of observation should be considered. If the patient’s answers demonstrate imminent intent and an actionable plan, an intensive level of observation should be ordered.
In terms of mental status findings, consider this question: Does the patient show extreme psychological pain or anguish, intense self-hatred, hopelessness, agitation or perturbation, psychosis (especially delusional guilt), or a wish for death? The presence of one or several of these might call for a high level of observation, even if the patient denies suicidal thoughts.
In terms of worrisome aspects of history, these are key questions: Has there been a recent severely distressing loss, disappointment, or threat? Does the patient lack social support from family, friends, church, and/or work? Is there an active substance abuse problem?
In bivariate analysis, imminent intent, an actionable plan, hopelessness, psychological pain, agitation, and wish for death were all significantly correlated with staff recommending suicidal observation or intense suicidal observation. On multivariate analysis, expressed intentions, wish for death, and hopelessness remained significant, Dr. Roca said.
Among hospitalized patients who attempted suicide, 17% had expressed imminent attempt or actionable plan; psychological anguish, hopelessness, and/or family history of suicide were each present in 58%; and 75% had three or more risk factors that were identified by the admitting clinician.
Lastly, it’s important to continuously perform risk assessment on vulnerable patients throughout the course of treatment.
Dr. Roca reported that he had no disclosures.
ANNAPOLIS, MD – Numerous suicide risk-assessment tools are available, but because none are perfect, the ability to prevent inpatient suicide hinges on a single factor, according to Dr. Robert P. Roca.
"It all comes down to clinical judgment. How do we guide clinical judgment?" Dr. Roca, vice president of medical affairs at Sheppard and Enoch Pratt Hospital, Towson, Md., asked at the annual meeting of the Southern Psychiatric Association. Basically, "it’s a synthetic clinical judgment that involves taking into account a whole lot of factors, and there’s really no test that tells us reliably what the answer is to this person’s risk."
About 5 years ago, Dr. Roca said, the Sheppard Pratt Health System looked retrospectively at its experience with inpatient suicide in its family and inpatient programs.
They found that men and women are equally likely to make serious attempts. Interestingly, the elderly were not disproportionately at risk. Nearly half of attempts occurred in the first 3 days; however, some attempts occurred when a patient appeared ready for discharge. Most patients who made serious attempts at suicide had unipolar or bipolar depression. Importantly, patients usually attempted hanging from a bedroom or bathroom door using bed linens or clothing.
Because attempts occur most often in bedrooms and bathrooms, careful design is needed to eliminate many hazards, such as using breakaway fixtures or down-sloping fixtures and avoiding breakable glass materials. "But a door is a potential gallows ... that was the vivid message that came across," he said. However, self-asphyxiation does not require hanging, and practically anything can become an instrument of self-harm.
"The most important message for me was that people who attempted suicide didn’t warn you in advance that they were going to do that," Dr. Roca said. "Certainly, a safety contract is no guarantee of safety."
Based on careful review of the records of patients who succeeded in committing suicide as an inpatient, the researchers identified several salient features of the mental status of these patients. These included intense psychological pain or anguish, intense self-loathing, delusions of guilt, agitation or perturbation, hopelessness, and a feeling that death would bring relief.
Universal precautions for these patients might include a physical environment that is safe yet therapeutically warm and a clinical milieu that inspires hope and rapidly relieves psychological distress, he said.
"You also need to be able to identify people who are at very, very high risk" and require special risk assessment. Early scales were simply inventories of demographic risk factors with limited evidence of reliability or validity. Subsequent scales were better researched, and included scales –such as the Beck Scale for Suicidal Ideation – with good reliability and validity but poor predictive value. Other scales were lengthy research tools that were impractical for clinical use and not designed to evaluate immediate risk.
More practical tools are available, but these are not perfect, either. The Nurses’ Global Assessment of Suicide Risk is a 15-item nurse-rated checklist. Scoring gives special weight to hopelessness, anhedonia, recent bereavement, and prior attempts. On this assessment, greater scores call for higher levels of engagement.
The Positive and Negative Suicidal Ideation Inventory (J. of Clin. Psychol. 2005;61:431-45) includes 14 items: eight "risk factors" and six "protective factors." Scoring uses a 5-point Likert scale. It has been validated in the adolescent and young adult populations in the Midwest, though it hasn’t been more broadly validated.
The clinicians at Sheppard Pratt have developed and are using their own assessment – the Sheppard Pratt Suicide Risk Assessment (SPSRA) – which includes 13 questions and three domains of risk: expressed intentions regarding suicide, mental status findings pertinent to risk, and aspects of history pertinent to risk. However, it is not a quantitative scale. The answers prompt clinicians to consider all three domains – not just expressed intentions – in their estimates of risk. The presence of any of these may increase suicide risk.
"The most important message for me was that people who attempted suicide didn’t warn you in advance that they were going to do that."
In terms of expressed intentions, these are important questions: Has there been a recent suicide attempt? Is there imminent suicide intent? Is there an actionable plan (a patient could realistically act upon this while in hospital)? If the answer to any of these three questions is yes, a high level of observation should be considered. If the patient’s answers demonstrate imminent intent and an actionable plan, an intensive level of observation should be ordered.
In terms of mental status findings, consider this question: Does the patient show extreme psychological pain or anguish, intense self-hatred, hopelessness, agitation or perturbation, psychosis (especially delusional guilt), or a wish for death? The presence of one or several of these might call for a high level of observation, even if the patient denies suicidal thoughts.
In terms of worrisome aspects of history, these are key questions: Has there been a recent severely distressing loss, disappointment, or threat? Does the patient lack social support from family, friends, church, and/or work? Is there an active substance abuse problem?
In bivariate analysis, imminent intent, an actionable plan, hopelessness, psychological pain, agitation, and wish for death were all significantly correlated with staff recommending suicidal observation or intense suicidal observation. On multivariate analysis, expressed intentions, wish for death, and hopelessness remained significant, Dr. Roca said.
Among hospitalized patients who attempted suicide, 17% had expressed imminent attempt or actionable plan; psychological anguish, hopelessness, and/or family history of suicide were each present in 58%; and 75% had three or more risk factors that were identified by the admitting clinician.
Lastly, it’s important to continuously perform risk assessment on vulnerable patients throughout the course of treatment.
Dr. Roca reported that he had no disclosures.
ANNAPOLIS, MD – Numerous suicide risk-assessment tools are available, but because none are perfect, the ability to prevent inpatient suicide hinges on a single factor, according to Dr. Robert P. Roca.
"It all comes down to clinical judgment. How do we guide clinical judgment?" Dr. Roca, vice president of medical affairs at Sheppard and Enoch Pratt Hospital, Towson, Md., asked at the annual meeting of the Southern Psychiatric Association. Basically, "it’s a synthetic clinical judgment that involves taking into account a whole lot of factors, and there’s really no test that tells us reliably what the answer is to this person’s risk."
About 5 years ago, Dr. Roca said, the Sheppard Pratt Health System looked retrospectively at its experience with inpatient suicide in its family and inpatient programs.
They found that men and women are equally likely to make serious attempts. Interestingly, the elderly were not disproportionately at risk. Nearly half of attempts occurred in the first 3 days; however, some attempts occurred when a patient appeared ready for discharge. Most patients who made serious attempts at suicide had unipolar or bipolar depression. Importantly, patients usually attempted hanging from a bedroom or bathroom door using bed linens or clothing.
Because attempts occur most often in bedrooms and bathrooms, careful design is needed to eliminate many hazards, such as using breakaway fixtures or down-sloping fixtures and avoiding breakable glass materials. "But a door is a potential gallows ... that was the vivid message that came across," he said. However, self-asphyxiation does not require hanging, and practically anything can become an instrument of self-harm.
"The most important message for me was that people who attempted suicide didn’t warn you in advance that they were going to do that," Dr. Roca said. "Certainly, a safety contract is no guarantee of safety."
Based on careful review of the records of patients who succeeded in committing suicide as an inpatient, the researchers identified several salient features of the mental status of these patients. These included intense psychological pain or anguish, intense self-loathing, delusions of guilt, agitation or perturbation, hopelessness, and a feeling that death would bring relief.
Universal precautions for these patients might include a physical environment that is safe yet therapeutically warm and a clinical milieu that inspires hope and rapidly relieves psychological distress, he said.
"You also need to be able to identify people who are at very, very high risk" and require special risk assessment. Early scales were simply inventories of demographic risk factors with limited evidence of reliability or validity. Subsequent scales were better researched, and included scales –such as the Beck Scale for Suicidal Ideation – with good reliability and validity but poor predictive value. Other scales were lengthy research tools that were impractical for clinical use and not designed to evaluate immediate risk.
More practical tools are available, but these are not perfect, either. The Nurses’ Global Assessment of Suicide Risk is a 15-item nurse-rated checklist. Scoring gives special weight to hopelessness, anhedonia, recent bereavement, and prior attempts. On this assessment, greater scores call for higher levels of engagement.
The Positive and Negative Suicidal Ideation Inventory (J. of Clin. Psychol. 2005;61:431-45) includes 14 items: eight "risk factors" and six "protective factors." Scoring uses a 5-point Likert scale. It has been validated in the adolescent and young adult populations in the Midwest, though it hasn’t been more broadly validated.
The clinicians at Sheppard Pratt have developed and are using their own assessment – the Sheppard Pratt Suicide Risk Assessment (SPSRA) – which includes 13 questions and three domains of risk: expressed intentions regarding suicide, mental status findings pertinent to risk, and aspects of history pertinent to risk. However, it is not a quantitative scale. The answers prompt clinicians to consider all three domains – not just expressed intentions – in their estimates of risk. The presence of any of these may increase suicide risk.
"The most important message for me was that people who attempted suicide didn’t warn you in advance that they were going to do that."
In terms of expressed intentions, these are important questions: Has there been a recent suicide attempt? Is there imminent suicide intent? Is there an actionable plan (a patient could realistically act upon this while in hospital)? If the answer to any of these three questions is yes, a high level of observation should be considered. If the patient’s answers demonstrate imminent intent and an actionable plan, an intensive level of observation should be ordered.
In terms of mental status findings, consider this question: Does the patient show extreme psychological pain or anguish, intense self-hatred, hopelessness, agitation or perturbation, psychosis (especially delusional guilt), or a wish for death? The presence of one or several of these might call for a high level of observation, even if the patient denies suicidal thoughts.
In terms of worrisome aspects of history, these are key questions: Has there been a recent severely distressing loss, disappointment, or threat? Does the patient lack social support from family, friends, church, and/or work? Is there an active substance abuse problem?
In bivariate analysis, imminent intent, an actionable plan, hopelessness, psychological pain, agitation, and wish for death were all significantly correlated with staff recommending suicidal observation or intense suicidal observation. On multivariate analysis, expressed intentions, wish for death, and hopelessness remained significant, Dr. Roca said.
Among hospitalized patients who attempted suicide, 17% had expressed imminent attempt or actionable plan; psychological anguish, hopelessness, and/or family history of suicide were each present in 58%; and 75% had three or more risk factors that were identified by the admitting clinician.
Lastly, it’s important to continuously perform risk assessment on vulnerable patients throughout the course of treatment.
Dr. Roca reported that he had no disclosures.
EXPERT ANALYSIS FROM THE ANNUAL MEETING OF THE SOUTHERN PSYCHIATRY ASSOCIATION