User login
Thrombocytopenia Reaction to Vancomycin
Von Drygalski A, Curtis BR, Bougie DW, et al. Vancomycin-induced immune thrombocytopenia. N Engl J Med. 2007 Mar 1;356(9):904-910
The use of vancomycin has grown exponentially in the past 20 years.1 Physicians have become increasingly aware of its major side effects, such as red man syndrome, hypersensitivity, neutropenia, and nephrotoxicity. But there have been only a few case reports of thrombocytopenia associated with this drug. This article looked at cases of thrombocytopenia in patients referred for clinical suspicion of vancomycin-induced thrombocytopenia.
From 2001-2005, serum samples were sent to the Platelet and Neutrophil Immunology Laboratory at the BloodCenter of Wisconsin in Milwaukee for testing for vancomycin-dependent antibodies from several sites. Clinical information regarding these patients was obtained from their referring physicians and one of the authors. Platelet reactive antibodies were detected by flow cytometry.
IgG and IgM vancomycin-dependent antibodies were detected in 34 patients. It was found that platelets dropped an average of 93% from pretreatment levels, and the average nadir occurred on day eight. The mean platelet count was 13,600. After vancomycin was discontinued, the platelet count returned to normal in all patients except for the three who died. The average time for resolution of thrombocytopenia was 7.5 days.
Unlike other drug-induced thrombocytopenia, these cases of thrombocytopenia associated with vancomycin appear to be more prone to significant hemorrhage. In this group 34% were found to have had severe hemorrhage defined in this study as florid petechial hemorrhages, ecchymoses, and oozing form the buccal mucosa. Three patients who had renal insufficiency were found to be profoundly thrombocytopenic for a longer duration, presumably due to delayed clearance of vancomycin in this setting.
Based on this study, it appears thrombocytopenia is a significant adverse reaction that can be attributed to vancomycin. Unlike other drug-induced thrombocytopenias, it appears to be associated with a higher likelihood of significant hemorrhage, as well.
Thrombocytopenia is a common occurrence in the acutely ill hospitalized patient and has been linked to increased hospital mortality and increased length of stay.2 Many drugs and diseases that hospitalists treat are associated with thrombocytopenia. The indications for usage of vancomycin continues to grow with the increasing number of patients with prosthetic devices and intravascular access, and the increasing prevalence of MRSA. This study raises awareness of a significant side effect that can be associated with vancomycin.
References
- Ena J, Dick RW, Jones RN, et al. The epidemiology of intravenous vancomycin usage in a university hospital: a 10-year study. JAMA. 1993 Feb 3;269(5):598-602. Comment in JAMA. 1993 Sep 22-29;270(12):1426.
- Crowther MA, Cook DJ, Meade M, et al. Thrombocytopenia in medical-surgical critically ill patients: prevalence, incidence, and risk factors. J Crit Care. 2005 Dec;20(4):248-253.
Can the mBRS Stratify Pts Admitted for Nonvariceal Upper GI Bleeds?
Romagnuolo J, Barkun AN, Enns R, et al. Simple clinical predictors may obviate urgent endoscopy in selected patients with nonvariceal upper gastrointestinal tract bleeding. Arch Intern Med. 2007 Feb 12;167(3):265-270.
Nonvariceal upper gastrointestinal bleeding is one of the top 10 admission diagnoses based on reviews of diagnosis-related groups. Patients with low-risk lesions on endoscopy, such as ulcers with a clean base, esophagitis, gastritis, duodenitis, or Mallory-Weiss tears, are felt to have less than a 5% chance of recurrent bleeding. In some instances, these patients can be treated successfully and discharged to home.1
Unfortunately, endoscopy is not always available—especially late at night and on weekends. It would be helpful to have a clinical prediction rule to identify patients at low risk for bleeding who could be safely discharged to get endoscopy within a few days.
In the study, 1,869 patients who had undergone upper endoscopy for upper gastrointestinal bleeding were entered into a Canadian national Registry for Upper GI Bleeding and Endoscopy (RUGBE). A modified Blatchford risk score (mBRS) was calculated to see if it could predict the presence of high-risk stigmata of bleeding, rebleeding rates, and mortality.
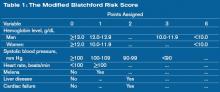
This mBRS was also compared with another scoring system—the Rockall score. The mBRS uses clinical and laboratory data to risk assess nonvariceal bleeding. The variables included in the scoring system include hemoglobin, systolic blood pressure, heart rate, melena, liver disease, and heart failure. High-risk endoscopic stigmata were defined as adherent clot after irrigation, a bleeding, oozing or spurting vessel, or a nonbleeding visible vessel. Rebleeding was defined as hematemesis, melena, or a bloody nasogastric aspirate in the presence of shock or a decrease in hemoglobin of 2 g/dL or more.
Patients who had a modified Blatchford risk score of <1 were found to have a lower likelihood of high-risk stigmata on endoscopy and were at a low risk for rebleeding (5%). Patients who had high-risk stigmata on endoscopy but an mBRS score of <1 were also found to have low rebleeding rates. The mBRS seemed to a better predictor than the Rockall score for high-risk stigmata and for rebleeding rates.
Patients with nonvariceal upper gastrointestinal tract bleeding may be identified as low risk for re-bleeding if they are normotensive, not tachycardic, not anemic, and do not have active melena, liver disease, or heart failure. It is conceivable that if endoscopy were not available, these patients could be sent home on high-dose proton pump inhibitor and asked to return for outpatient upper endoscopy within a few days.
The study certainly raises interesting questions. Whether it is acceptable practice to discharge a “low-risk” patient with an upper gastrointestinal hemorrhage on a high-dose proton pump inhibitor with good social support and close outpatient follow-up, but without diagnostic endoscopy is still unclear.
The study is limited by the fact that it is a retrospective analysis; however, it does examine a large cohort of patients. The authors acknowledge this, and this work could lead to a prospective randomized trial that would help answer this question. In the meantime, the mBRS may be a helpful tool to help risk stratify patients admitted for nonvariceal upper gastrointestinal bleeding.
References
- Cipolletta L, Bianco M, Rotondano G, et al. Outpatient management for low-risk nonvariceal upper GI bleeding: a randomized controlled trial. Gastrointest Endosc. 2002;55(1):1-5.
Lumbar Puncture to Reduce Adverse Events
Straus SE, Thorpe KE, Holroyd-Leduc J. How do I perform a lumbar puncture and analyze the results to diagnose bacterial meningitis? JAMA. 2006 Oct 25;296(16):2012-2022.
Lumbar punctures (LPs) remain a common diagnostic test performed by physicians to rule out meningitis. This procedure may be associated with adverse events, with headache and backache the most commonly reported. This systematic review and meta-analysis sought to review the evidence regarding diagnostic lumbar puncture techniques that might reduce the risk of adverse events, and to examine the accuracy of cerebrospinal fluid (CSF) analysis in the diagnosis of bacterial meningitis.
Studies were identified through searches of the Cochrane Library (www3.interscience.wiley.com/cgi-bin/mrwhome/106568753/AboutCochrane.html), MEDLINE from 1966 to January 2006, and EMBASE from 1980 to January 2006 (without language restrictions) to identify relevant studies. Bibliographies of retrieved articles were also used as data sources.
Randomized controlled trials of patients 18 or older undergoing lumbar puncture testing interventions to facilitate a successful diagnostic procedure or reduce adverse events were identified and selected. As a secondary outcome, trials that assessed the accuracy of CSF biochemical analysis for the diagnosis of bacterial meningitis were also identified and included. Trials that studied spinal anesthesia or myelography were excluded.
Study appraisals for quality (randomization, blinding, and outcome assessment) and data extraction were performed by two investigators independently. Fifteen randomized trials of interventions to reduce adverse events met criteria for inclusion, and four studies of the diagnostic test characteristics of CSF analysis met criteria and were included.
Meta-analysis with a random effects model of five studies (total of 587 patients) comparing atraumatic needles with standard needles yielded a nonsignificant decrease in the odds of headache with an atraumatic needle (absolute risk reduction [ARR], 12.3%; 95% confidence interval [CI], –1.72% to 26.2%). A single study of reinsertion of the stylet before needle removal (600 patients) showed a decreased risk of headache (ARR, 11.3%; 95% CI, 6.50%-16.2%). Meta-analysis of four studies (717 patients) revealed a nonsignificant decrease in headache in patients mobilized after LP (ARR 2.9%; 95% CI, –3.4 to 9.3%).
Data from the diagnostic test studies yielded the following likelihood ratios for diagnosing bacterial meningitis: A CSF–blood glucose ratio of 0.4 or less with a likelihood ratio of 18 (95% CI, 12-27); CSF white blood cell count of 500/µL or higher with a likelihood ratio of 15 (95% CI, 10-22); and CSF lactate level of >31.53 mg/dL with a likelihood ration of 21 (95% CI, 14-32) in accurately diagnosed bacterial meningitis.
These data support the reinsertion of the stylet before needle removal to reduce the risk of headache after lumbar puncture and that patients do not require bed rest after diagnostic lumbar puncture. Biochemical analyses, including CSF-blood glucose ratio, CSF leukocyte count and lactate level are useful in diagnosing bacterial meningitis.
This Rational Clinical Examination systematic review and meta-analysis provides a nice review of the available data on optimizing diagnostic lumbar puncture technique to reduce adverse events. It is somewhat remarkable so little has changed in our knowledge about this long-standing diagnostic procedure. Post-lumbar puncture headaches remain a challenge that may affect patient satisfaction as well as hospital (or observation unit) course particularly for patients who do not have evidence of bacterial meningitis once the analysis is complete.
This review seems to provide some useful answers for physicians performing lumbar puncture, who should consider selecting a small gauge needle and reinserting the stylet prior to removal. Future studies of other maneuvers to reduce post-procedure adverse events should be considered for the question of atraumatic needles, which may be technically more difficult to use. The review confirms and helps quantify the utility of CSF biochemical analysis in the diagnosis of bacterial meningitis.
Who’s Performing Procedures?
Wigton RS, Alguire P. The declining number and variety of procedures done by general internists: a resurvey of members of the American College of Physicians. Ann Intern Med. 2007 Mar 6;146(5):355-360. Comment in Ann Intern Med. 2007 Mar 6; 146(5):392-393.
Prior surveys of physicians documented that general internists performed a variety and significant number of procedures in their practice. Much has changed since those prior assessments, including physician training, practice settings, availability of subspecialists, and regulatory requirements that have altered physician’s practice with regard to procedures. This study sought to reassess the volume and variety of procedures performed by general internists compared with the prior survey of 1986. The final sample included 990 completed surveys from general internists from 1,389 returned questionnaires for a successful completion rate of 39.6%.
The median number of different procedures performed in practice decreased from 16 in 1986 to seven in 2004. Internists who practiced in smaller hospitals or smaller towns reported performing almost twice as many procedures as physicians in the largest hospitals and cities. Hours spent in the care of hospitalized patients were also associated with an increased number of different procedures—in particular mechanical ventilation, central venous catheter placement, and thoracentesis. For all but one of the 34 procedures common to both surveys, fewer general internists performed them in 2004 compared with 1986. Remarkably, for 22 of the 34 procedures, a greater than 50% reduction in the proportion of respondents who performed the procedure was noted.
In the 1986 survey, the majority of internists performed all but one of the six procedures required by the American Board of Internal Medicine (ABIM) for certification (abdominal paracentesis, arterial puncture for blood gases, central venous catheter placement, joint aspiration, lumbar puncture, and thoracentesis). Except for joint aspiration, in 2004 these required procedures were performed by 25% or fewer of the respondents.
The 2004 survey demonstrated a striking reduction in the number of different procedures performed by general internists, and a decrease in the proportion of internists who do most procedures. These reductions may stem from a variety of changes in physician practices, including the emergence of hospitalists, availability of subspecialty physicians and proceduralists, and changes in technology and regulatory environments.
Regardless of the forces behind these changes, internal medicine residents’ training in procedures should be re-examined.
Many of those in academic hospital medicine have noted a decline in procedures performed by general internists at large academic centers. This study affirms this trend overall and in particular for physicians in large urban settings or in the largest hospitals. The emergence of hospital medicine may have played a role in reducing the procedures performed by primary care (outpatient) physicians who now spend less time caring for medically ill hospitalized patients.
Residency programs now must consider how to incorporate procedure skills and training to align with the needs of internists. The rising interest in careers in hospital medicine (as opposed to outpatient primary care) necessitates a new approach and individualized plans for gaining procedural skills to match career goals and practice settings. The new ABIM policy acknowledges this greater variability in the procedures performed by internists in practice, and takes steps to more closely align procedure requirements and core manual skills with physician practice.
These changes and new flexibility in requirements provide another opportunity for academic hospital medicine programs to provide leadership, and help shape the training of inpatient physicians. TH
Thrombocytopenia Reaction to Vancomycin
Von Drygalski A, Curtis BR, Bougie DW, et al. Vancomycin-induced immune thrombocytopenia. N Engl J Med. 2007 Mar 1;356(9):904-910
The use of vancomycin has grown exponentially in the past 20 years.1 Physicians have become increasingly aware of its major side effects, such as red man syndrome, hypersensitivity, neutropenia, and nephrotoxicity. But there have been only a few case reports of thrombocytopenia associated with this drug. This article looked at cases of thrombocytopenia in patients referred for clinical suspicion of vancomycin-induced thrombocytopenia.
From 2001-2005, serum samples were sent to the Platelet and Neutrophil Immunology Laboratory at the BloodCenter of Wisconsin in Milwaukee for testing for vancomycin-dependent antibodies from several sites. Clinical information regarding these patients was obtained from their referring physicians and one of the authors. Platelet reactive antibodies were detected by flow cytometry.
IgG and IgM vancomycin-dependent antibodies were detected in 34 patients. It was found that platelets dropped an average of 93% from pretreatment levels, and the average nadir occurred on day eight. The mean platelet count was 13,600. After vancomycin was discontinued, the platelet count returned to normal in all patients except for the three who died. The average time for resolution of thrombocytopenia was 7.5 days.
Unlike other drug-induced thrombocytopenia, these cases of thrombocytopenia associated with vancomycin appear to be more prone to significant hemorrhage. In this group 34% were found to have had severe hemorrhage defined in this study as florid petechial hemorrhages, ecchymoses, and oozing form the buccal mucosa. Three patients who had renal insufficiency were found to be profoundly thrombocytopenic for a longer duration, presumably due to delayed clearance of vancomycin in this setting.
Based on this study, it appears thrombocytopenia is a significant adverse reaction that can be attributed to vancomycin. Unlike other drug-induced thrombocytopenias, it appears to be associated with a higher likelihood of significant hemorrhage, as well.
Thrombocytopenia is a common occurrence in the acutely ill hospitalized patient and has been linked to increased hospital mortality and increased length of stay.2 Many drugs and diseases that hospitalists treat are associated with thrombocytopenia. The indications for usage of vancomycin continues to grow with the increasing number of patients with prosthetic devices and intravascular access, and the increasing prevalence of MRSA. This study raises awareness of a significant side effect that can be associated with vancomycin.
References
- Ena J, Dick RW, Jones RN, et al. The epidemiology of intravenous vancomycin usage in a university hospital: a 10-year study. JAMA. 1993 Feb 3;269(5):598-602. Comment in JAMA. 1993 Sep 22-29;270(12):1426.
- Crowther MA, Cook DJ, Meade M, et al. Thrombocytopenia in medical-surgical critically ill patients: prevalence, incidence, and risk factors. J Crit Care. 2005 Dec;20(4):248-253.
Can the mBRS Stratify Pts Admitted for Nonvariceal Upper GI Bleeds?
Romagnuolo J, Barkun AN, Enns R, et al. Simple clinical predictors may obviate urgent endoscopy in selected patients with nonvariceal upper gastrointestinal tract bleeding. Arch Intern Med. 2007 Feb 12;167(3):265-270.
Nonvariceal upper gastrointestinal bleeding is one of the top 10 admission diagnoses based on reviews of diagnosis-related groups. Patients with low-risk lesions on endoscopy, such as ulcers with a clean base, esophagitis, gastritis, duodenitis, or Mallory-Weiss tears, are felt to have less than a 5% chance of recurrent bleeding. In some instances, these patients can be treated successfully and discharged to home.1
Unfortunately, endoscopy is not always available—especially late at night and on weekends. It would be helpful to have a clinical prediction rule to identify patients at low risk for bleeding who could be safely discharged to get endoscopy within a few days.
In the study, 1,869 patients who had undergone upper endoscopy for upper gastrointestinal bleeding were entered into a Canadian national Registry for Upper GI Bleeding and Endoscopy (RUGBE). A modified Blatchford risk score (mBRS) was calculated to see if it could predict the presence of high-risk stigmata of bleeding, rebleeding rates, and mortality.
This mBRS was also compared with another scoring system—the Rockall score. The mBRS uses clinical and laboratory data to risk assess nonvariceal bleeding. The variables included in the scoring system include hemoglobin, systolic blood pressure, heart rate, melena, liver disease, and heart failure. High-risk endoscopic stigmata were defined as adherent clot after irrigation, a bleeding, oozing or spurting vessel, or a nonbleeding visible vessel. Rebleeding was defined as hematemesis, melena, or a bloody nasogastric aspirate in the presence of shock or a decrease in hemoglobin of 2 g/dL or more.
Patients who had a modified Blatchford risk score of <1 were found to have a lower likelihood of high-risk stigmata on endoscopy and were at a low risk for rebleeding (5%). Patients who had high-risk stigmata on endoscopy but an mBRS score of <1 were also found to have low rebleeding rates. The mBRS seemed to a better predictor than the Rockall score for high-risk stigmata and for rebleeding rates.
Patients with nonvariceal upper gastrointestinal tract bleeding may be identified as low risk for re-bleeding if they are normotensive, not tachycardic, not anemic, and do not have active melena, liver disease, or heart failure. It is conceivable that if endoscopy were not available, these patients could be sent home on high-dose proton pump inhibitor and asked to return for outpatient upper endoscopy within a few days.
The study certainly raises interesting questions. Whether it is acceptable practice to discharge a “low-risk” patient with an upper gastrointestinal hemorrhage on a high-dose proton pump inhibitor with good social support and close outpatient follow-up, but without diagnostic endoscopy is still unclear.
The study is limited by the fact that it is a retrospective analysis; however, it does examine a large cohort of patients. The authors acknowledge this, and this work could lead to a prospective randomized trial that would help answer this question. In the meantime, the mBRS may be a helpful tool to help risk stratify patients admitted for nonvariceal upper gastrointestinal bleeding.
References
- Cipolletta L, Bianco M, Rotondano G, et al. Outpatient management for low-risk nonvariceal upper GI bleeding: a randomized controlled trial. Gastrointest Endosc. 2002;55(1):1-5.
Lumbar Puncture to Reduce Adverse Events
Straus SE, Thorpe KE, Holroyd-Leduc J. How do I perform a lumbar puncture and analyze the results to diagnose bacterial meningitis? JAMA. 2006 Oct 25;296(16):2012-2022.
Lumbar punctures (LPs) remain a common diagnostic test performed by physicians to rule out meningitis. This procedure may be associated with adverse events, with headache and backache the most commonly reported. This systematic review and meta-analysis sought to review the evidence regarding diagnostic lumbar puncture techniques that might reduce the risk of adverse events, and to examine the accuracy of cerebrospinal fluid (CSF) analysis in the diagnosis of bacterial meningitis.
Studies were identified through searches of the Cochrane Library (www3.interscience.wiley.com/cgi-bin/mrwhome/106568753/AboutCochrane.html), MEDLINE from 1966 to January 2006, and EMBASE from 1980 to January 2006 (without language restrictions) to identify relevant studies. Bibliographies of retrieved articles were also used as data sources.
Randomized controlled trials of patients 18 or older undergoing lumbar puncture testing interventions to facilitate a successful diagnostic procedure or reduce adverse events were identified and selected. As a secondary outcome, trials that assessed the accuracy of CSF biochemical analysis for the diagnosis of bacterial meningitis were also identified and included. Trials that studied spinal anesthesia or myelography were excluded.
Study appraisals for quality (randomization, blinding, and outcome assessment) and data extraction were performed by two investigators independently. Fifteen randomized trials of interventions to reduce adverse events met criteria for inclusion, and four studies of the diagnostic test characteristics of CSF analysis met criteria and were included.
Meta-analysis with a random effects model of five studies (total of 587 patients) comparing atraumatic needles with standard needles yielded a nonsignificant decrease in the odds of headache with an atraumatic needle (absolute risk reduction [ARR], 12.3%; 95% confidence interval [CI], –1.72% to 26.2%). A single study of reinsertion of the stylet before needle removal (600 patients) showed a decreased risk of headache (ARR, 11.3%; 95% CI, 6.50%-16.2%). Meta-analysis of four studies (717 patients) revealed a nonsignificant decrease in headache in patients mobilized after LP (ARR 2.9%; 95% CI, –3.4 to 9.3%).
Data from the diagnostic test studies yielded the following likelihood ratios for diagnosing bacterial meningitis: A CSF–blood glucose ratio of 0.4 or less with a likelihood ratio of 18 (95% CI, 12-27); CSF white blood cell count of 500/µL or higher with a likelihood ratio of 15 (95% CI, 10-22); and CSF lactate level of >31.53 mg/dL with a likelihood ration of 21 (95% CI, 14-32) in accurately diagnosed bacterial meningitis.
These data support the reinsertion of the stylet before needle removal to reduce the risk of headache after lumbar puncture and that patients do not require bed rest after diagnostic lumbar puncture. Biochemical analyses, including CSF-blood glucose ratio, CSF leukocyte count and lactate level are useful in diagnosing bacterial meningitis.
This Rational Clinical Examination systematic review and meta-analysis provides a nice review of the available data on optimizing diagnostic lumbar puncture technique to reduce adverse events. It is somewhat remarkable so little has changed in our knowledge about this long-standing diagnostic procedure. Post-lumbar puncture headaches remain a challenge that may affect patient satisfaction as well as hospital (or observation unit) course particularly for patients who do not have evidence of bacterial meningitis once the analysis is complete.
This review seems to provide some useful answers for physicians performing lumbar puncture, who should consider selecting a small gauge needle and reinserting the stylet prior to removal. Future studies of other maneuvers to reduce post-procedure adverse events should be considered for the question of atraumatic needles, which may be technically more difficult to use. The review confirms and helps quantify the utility of CSF biochemical analysis in the diagnosis of bacterial meningitis.
Who’s Performing Procedures?
Wigton RS, Alguire P. The declining number and variety of procedures done by general internists: a resurvey of members of the American College of Physicians. Ann Intern Med. 2007 Mar 6;146(5):355-360. Comment in Ann Intern Med. 2007 Mar 6; 146(5):392-393.
Prior surveys of physicians documented that general internists performed a variety and significant number of procedures in their practice. Much has changed since those prior assessments, including physician training, practice settings, availability of subspecialists, and regulatory requirements that have altered physician’s practice with regard to procedures. This study sought to reassess the volume and variety of procedures performed by general internists compared with the prior survey of 1986. The final sample included 990 completed surveys from general internists from 1,389 returned questionnaires for a successful completion rate of 39.6%.
The median number of different procedures performed in practice decreased from 16 in 1986 to seven in 2004. Internists who practiced in smaller hospitals or smaller towns reported performing almost twice as many procedures as physicians in the largest hospitals and cities. Hours spent in the care of hospitalized patients were also associated with an increased number of different procedures—in particular mechanical ventilation, central venous catheter placement, and thoracentesis. For all but one of the 34 procedures common to both surveys, fewer general internists performed them in 2004 compared with 1986. Remarkably, for 22 of the 34 procedures, a greater than 50% reduction in the proportion of respondents who performed the procedure was noted.
In the 1986 survey, the majority of internists performed all but one of the six procedures required by the American Board of Internal Medicine (ABIM) for certification (abdominal paracentesis, arterial puncture for blood gases, central venous catheter placement, joint aspiration, lumbar puncture, and thoracentesis). Except for joint aspiration, in 2004 these required procedures were performed by 25% or fewer of the respondents.
The 2004 survey demonstrated a striking reduction in the number of different procedures performed by general internists, and a decrease in the proportion of internists who do most procedures. These reductions may stem from a variety of changes in physician practices, including the emergence of hospitalists, availability of subspecialty physicians and proceduralists, and changes in technology and regulatory environments.
Regardless of the forces behind these changes, internal medicine residents’ training in procedures should be re-examined.
Many of those in academic hospital medicine have noted a decline in procedures performed by general internists at large academic centers. This study affirms this trend overall and in particular for physicians in large urban settings or in the largest hospitals. The emergence of hospital medicine may have played a role in reducing the procedures performed by primary care (outpatient) physicians who now spend less time caring for medically ill hospitalized patients.
Residency programs now must consider how to incorporate procedure skills and training to align with the needs of internists. The rising interest in careers in hospital medicine (as opposed to outpatient primary care) necessitates a new approach and individualized plans for gaining procedural skills to match career goals and practice settings. The new ABIM policy acknowledges this greater variability in the procedures performed by internists in practice, and takes steps to more closely align procedure requirements and core manual skills with physician practice.
These changes and new flexibility in requirements provide another opportunity for academic hospital medicine programs to provide leadership, and help shape the training of inpatient physicians. TH
Thrombocytopenia Reaction to Vancomycin
Von Drygalski A, Curtis BR, Bougie DW, et al. Vancomycin-induced immune thrombocytopenia. N Engl J Med. 2007 Mar 1;356(9):904-910
The use of vancomycin has grown exponentially in the past 20 years.1 Physicians have become increasingly aware of its major side effects, such as red man syndrome, hypersensitivity, neutropenia, and nephrotoxicity. But there have been only a few case reports of thrombocytopenia associated with this drug. This article looked at cases of thrombocytopenia in patients referred for clinical suspicion of vancomycin-induced thrombocytopenia.
From 2001-2005, serum samples were sent to the Platelet and Neutrophil Immunology Laboratory at the BloodCenter of Wisconsin in Milwaukee for testing for vancomycin-dependent antibodies from several sites. Clinical information regarding these patients was obtained from their referring physicians and one of the authors. Platelet reactive antibodies were detected by flow cytometry.
IgG and IgM vancomycin-dependent antibodies were detected in 34 patients. It was found that platelets dropped an average of 93% from pretreatment levels, and the average nadir occurred on day eight. The mean platelet count was 13,600. After vancomycin was discontinued, the platelet count returned to normal in all patients except for the three who died. The average time for resolution of thrombocytopenia was 7.5 days.
Unlike other drug-induced thrombocytopenia, these cases of thrombocytopenia associated with vancomycin appear to be more prone to significant hemorrhage. In this group 34% were found to have had severe hemorrhage defined in this study as florid petechial hemorrhages, ecchymoses, and oozing form the buccal mucosa. Three patients who had renal insufficiency were found to be profoundly thrombocytopenic for a longer duration, presumably due to delayed clearance of vancomycin in this setting.
Based on this study, it appears thrombocytopenia is a significant adverse reaction that can be attributed to vancomycin. Unlike other drug-induced thrombocytopenias, it appears to be associated with a higher likelihood of significant hemorrhage, as well.
Thrombocytopenia is a common occurrence in the acutely ill hospitalized patient and has been linked to increased hospital mortality and increased length of stay.2 Many drugs and diseases that hospitalists treat are associated with thrombocytopenia. The indications for usage of vancomycin continues to grow with the increasing number of patients with prosthetic devices and intravascular access, and the increasing prevalence of MRSA. This study raises awareness of a significant side effect that can be associated with vancomycin.
References
- Ena J, Dick RW, Jones RN, et al. The epidemiology of intravenous vancomycin usage in a university hospital: a 10-year study. JAMA. 1993 Feb 3;269(5):598-602. Comment in JAMA. 1993 Sep 22-29;270(12):1426.
- Crowther MA, Cook DJ, Meade M, et al. Thrombocytopenia in medical-surgical critically ill patients: prevalence, incidence, and risk factors. J Crit Care. 2005 Dec;20(4):248-253.
Can the mBRS Stratify Pts Admitted for Nonvariceal Upper GI Bleeds?
Romagnuolo J, Barkun AN, Enns R, et al. Simple clinical predictors may obviate urgent endoscopy in selected patients with nonvariceal upper gastrointestinal tract bleeding. Arch Intern Med. 2007 Feb 12;167(3):265-270.
Nonvariceal upper gastrointestinal bleeding is one of the top 10 admission diagnoses based on reviews of diagnosis-related groups. Patients with low-risk lesions on endoscopy, such as ulcers with a clean base, esophagitis, gastritis, duodenitis, or Mallory-Weiss tears, are felt to have less than a 5% chance of recurrent bleeding. In some instances, these patients can be treated successfully and discharged to home.1
Unfortunately, endoscopy is not always available—especially late at night and on weekends. It would be helpful to have a clinical prediction rule to identify patients at low risk for bleeding who could be safely discharged to get endoscopy within a few days.
In the study, 1,869 patients who had undergone upper endoscopy for upper gastrointestinal bleeding were entered into a Canadian national Registry for Upper GI Bleeding and Endoscopy (RUGBE). A modified Blatchford risk score (mBRS) was calculated to see if it could predict the presence of high-risk stigmata of bleeding, rebleeding rates, and mortality.
This mBRS was also compared with another scoring system—the Rockall score. The mBRS uses clinical and laboratory data to risk assess nonvariceal bleeding. The variables included in the scoring system include hemoglobin, systolic blood pressure, heart rate, melena, liver disease, and heart failure. High-risk endoscopic stigmata were defined as adherent clot after irrigation, a bleeding, oozing or spurting vessel, or a nonbleeding visible vessel. Rebleeding was defined as hematemesis, melena, or a bloody nasogastric aspirate in the presence of shock or a decrease in hemoglobin of 2 g/dL or more.
Patients who had a modified Blatchford risk score of <1 were found to have a lower likelihood of high-risk stigmata on endoscopy and were at a low risk for rebleeding (5%). Patients who had high-risk stigmata on endoscopy but an mBRS score of <1 were also found to have low rebleeding rates. The mBRS seemed to a better predictor than the Rockall score for high-risk stigmata and for rebleeding rates.
Patients with nonvariceal upper gastrointestinal tract bleeding may be identified as low risk for re-bleeding if they are normotensive, not tachycardic, not anemic, and do not have active melena, liver disease, or heart failure. It is conceivable that if endoscopy were not available, these patients could be sent home on high-dose proton pump inhibitor and asked to return for outpatient upper endoscopy within a few days.
The study certainly raises interesting questions. Whether it is acceptable practice to discharge a “low-risk” patient with an upper gastrointestinal hemorrhage on a high-dose proton pump inhibitor with good social support and close outpatient follow-up, but without diagnostic endoscopy is still unclear.
The study is limited by the fact that it is a retrospective analysis; however, it does examine a large cohort of patients. The authors acknowledge this, and this work could lead to a prospective randomized trial that would help answer this question. In the meantime, the mBRS may be a helpful tool to help risk stratify patients admitted for nonvariceal upper gastrointestinal bleeding.
References
- Cipolletta L, Bianco M, Rotondano G, et al. Outpatient management for low-risk nonvariceal upper GI bleeding: a randomized controlled trial. Gastrointest Endosc. 2002;55(1):1-5.
Lumbar Puncture to Reduce Adverse Events
Straus SE, Thorpe KE, Holroyd-Leduc J. How do I perform a lumbar puncture and analyze the results to diagnose bacterial meningitis? JAMA. 2006 Oct 25;296(16):2012-2022.
Lumbar punctures (LPs) remain a common diagnostic test performed by physicians to rule out meningitis. This procedure may be associated with adverse events, with headache and backache the most commonly reported. This systematic review and meta-analysis sought to review the evidence regarding diagnostic lumbar puncture techniques that might reduce the risk of adverse events, and to examine the accuracy of cerebrospinal fluid (CSF) analysis in the diagnosis of bacterial meningitis.
Studies were identified through searches of the Cochrane Library (www3.interscience.wiley.com/cgi-bin/mrwhome/106568753/AboutCochrane.html), MEDLINE from 1966 to January 2006, and EMBASE from 1980 to January 2006 (without language restrictions) to identify relevant studies. Bibliographies of retrieved articles were also used as data sources.
Randomized controlled trials of patients 18 or older undergoing lumbar puncture testing interventions to facilitate a successful diagnostic procedure or reduce adverse events were identified and selected. As a secondary outcome, trials that assessed the accuracy of CSF biochemical analysis for the diagnosis of bacterial meningitis were also identified and included. Trials that studied spinal anesthesia or myelography were excluded.
Study appraisals for quality (randomization, blinding, and outcome assessment) and data extraction were performed by two investigators independently. Fifteen randomized trials of interventions to reduce adverse events met criteria for inclusion, and four studies of the diagnostic test characteristics of CSF analysis met criteria and were included.
Meta-analysis with a random effects model of five studies (total of 587 patients) comparing atraumatic needles with standard needles yielded a nonsignificant decrease in the odds of headache with an atraumatic needle (absolute risk reduction [ARR], 12.3%; 95% confidence interval [CI], –1.72% to 26.2%). A single study of reinsertion of the stylet before needle removal (600 patients) showed a decreased risk of headache (ARR, 11.3%; 95% CI, 6.50%-16.2%). Meta-analysis of four studies (717 patients) revealed a nonsignificant decrease in headache in patients mobilized after LP (ARR 2.9%; 95% CI, –3.4 to 9.3%).
Data from the diagnostic test studies yielded the following likelihood ratios for diagnosing bacterial meningitis: A CSF–blood glucose ratio of 0.4 or less with a likelihood ratio of 18 (95% CI, 12-27); CSF white blood cell count of 500/µL or higher with a likelihood ratio of 15 (95% CI, 10-22); and CSF lactate level of >31.53 mg/dL with a likelihood ration of 21 (95% CI, 14-32) in accurately diagnosed bacterial meningitis.
These data support the reinsertion of the stylet before needle removal to reduce the risk of headache after lumbar puncture and that patients do not require bed rest after diagnostic lumbar puncture. Biochemical analyses, including CSF-blood glucose ratio, CSF leukocyte count and lactate level are useful in diagnosing bacterial meningitis.
This Rational Clinical Examination systematic review and meta-analysis provides a nice review of the available data on optimizing diagnostic lumbar puncture technique to reduce adverse events. It is somewhat remarkable so little has changed in our knowledge about this long-standing diagnostic procedure. Post-lumbar puncture headaches remain a challenge that may affect patient satisfaction as well as hospital (or observation unit) course particularly for patients who do not have evidence of bacterial meningitis once the analysis is complete.
This review seems to provide some useful answers for physicians performing lumbar puncture, who should consider selecting a small gauge needle and reinserting the stylet prior to removal. Future studies of other maneuvers to reduce post-procedure adverse events should be considered for the question of atraumatic needles, which may be technically more difficult to use. The review confirms and helps quantify the utility of CSF biochemical analysis in the diagnosis of bacterial meningitis.
Who’s Performing Procedures?
Wigton RS, Alguire P. The declining number and variety of procedures done by general internists: a resurvey of members of the American College of Physicians. Ann Intern Med. 2007 Mar 6;146(5):355-360. Comment in Ann Intern Med. 2007 Mar 6; 146(5):392-393.
Prior surveys of physicians documented that general internists performed a variety and significant number of procedures in their practice. Much has changed since those prior assessments, including physician training, practice settings, availability of subspecialists, and regulatory requirements that have altered physician’s practice with regard to procedures. This study sought to reassess the volume and variety of procedures performed by general internists compared with the prior survey of 1986. The final sample included 990 completed surveys from general internists from 1,389 returned questionnaires for a successful completion rate of 39.6%.
The median number of different procedures performed in practice decreased from 16 in 1986 to seven in 2004. Internists who practiced in smaller hospitals or smaller towns reported performing almost twice as many procedures as physicians in the largest hospitals and cities. Hours spent in the care of hospitalized patients were also associated with an increased number of different procedures—in particular mechanical ventilation, central venous catheter placement, and thoracentesis. For all but one of the 34 procedures common to both surveys, fewer general internists performed them in 2004 compared with 1986. Remarkably, for 22 of the 34 procedures, a greater than 50% reduction in the proportion of respondents who performed the procedure was noted.
In the 1986 survey, the majority of internists performed all but one of the six procedures required by the American Board of Internal Medicine (ABIM) for certification (abdominal paracentesis, arterial puncture for blood gases, central venous catheter placement, joint aspiration, lumbar puncture, and thoracentesis). Except for joint aspiration, in 2004 these required procedures were performed by 25% or fewer of the respondents.
The 2004 survey demonstrated a striking reduction in the number of different procedures performed by general internists, and a decrease in the proportion of internists who do most procedures. These reductions may stem from a variety of changes in physician practices, including the emergence of hospitalists, availability of subspecialty physicians and proceduralists, and changes in technology and regulatory environments.
Regardless of the forces behind these changes, internal medicine residents’ training in procedures should be re-examined.
Many of those in academic hospital medicine have noted a decline in procedures performed by general internists at large academic centers. This study affirms this trend overall and in particular for physicians in large urban settings or in the largest hospitals. The emergence of hospital medicine may have played a role in reducing the procedures performed by primary care (outpatient) physicians who now spend less time caring for medically ill hospitalized patients.
Residency programs now must consider how to incorporate procedure skills and training to align with the needs of internists. The rising interest in careers in hospital medicine (as opposed to outpatient primary care) necessitates a new approach and individualized plans for gaining procedural skills to match career goals and practice settings. The new ABIM policy acknowledges this greater variability in the procedures performed by internists in practice, and takes steps to more closely align procedure requirements and core manual skills with physician practice.
These changes and new flexibility in requirements provide another opportunity for academic hospital medicine programs to provide leadership, and help shape the training of inpatient physicians. TH