User login
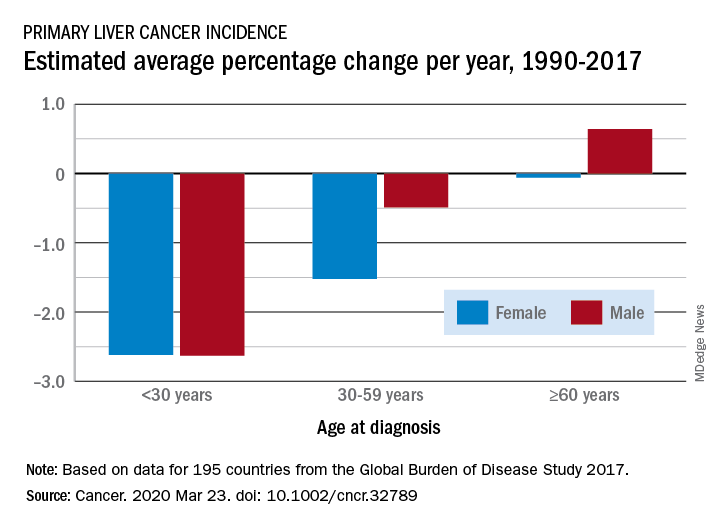
Liver cancer rates have been increasing, but a new analysis finds that the increase has occurred primarily in men older than 60 years in developed countries.
The findings come from an analysis of data from the Global Burden of Disease (GBD) Study 2017, published online March 23 in Cancer.
From 1990 to 2017, the number of cancer cases increased nearly threefold in older men and more than twofold in older women (aged 60 years or more). This increase was driven mainly by an increase in liver cancer caused by nonalcoholic steatohepatitis (NASH), also termed fatty liver disease, note the authors.
In contrast, the incidence of liver cancer among men and women who are younger than 30 years and those aged 30 to 59 years declined during this period.
The decreases seen in younger adults were largely ascribed to hepatitis B virus (HBV) vaccination and were consistent in most regions except in developed countries, where liver cancer rates increased irrespective of sex and age.
“Our findings suggest a lack of attention for older people in current liver cancer prevention efforts and highlight the emerging concern of obesity as a risk factor for liver cancer,” lead author Xingdong Chen, MD, PhD, Fudan University, China, said in a statement.
“Liver cancer prevention strategies in both developing and developed countries should be tailored and updated,” he added.
The authors point out that liver cancer was previously considered to be rare in the Western hemisphere.
“However, we found a significant increase in primary liver cancer incidence – regardless of etiology, sex, or age – in most of these countries over the last few decades,” they observe.
The fact that the most pronounced increase in liver cancer was caused by NASH suggests that more attention should be paid to weight management and obesity control as primary prevention strategies in these regions, they suggest.
Study design
Annual incidence data were collected from 1990 to 2017 and were categorized by sex, region, country, age group, and etiology.
“Data from a total of 195 countries and territories were available,” the investigators note, “and these countries and territories were categorized into 5 regions in terms of sociodemographic index (SDI),” they add.
Data were also retrieved regarding five etiologies of liver cancer: HBV infection, hepatitis C virus (HCV) infection, alcohol use, NASH, and others.
The authors note that age-standardized incidence rates of primary liver cancer caused by those five etiologies increased significantly in Australasia, Western Europe, and high-income regions of North America. The most significant increase was found in liver cancer caused by NASH in the Netherlands (in men) and in Finland (in women).
An increasing trend was observed in most countries for primary liver cancer among people aged 60 years or older, the authors note. They suggest that population expansion, aging, and increasing prevalence of obesity and diabetes might partly explain the marked increase, especially the dramatic increase in the number of cases among older people. Additionally, the “lag effect” of the large HBV infection reservoir in several countries might also contribute to the increase, the authors state. They explain that people infected with HBV early in life may experience progression to liver cancer as they age.
Primary prevention
Prevention of HBV infection – the primary cause of liver cancer – has been possible since the introduction of the HBV vaccine in 1982.
“By the end of 2017, 187 countries had introduced the HBV vaccine into their national immunization schedules, with global coverage with 3 doses of the hepatitis B vaccine ... estimated at 84%,” the authors point out.
This has “dramatically” reduced both the prevalence of HBV infection and the incidence of liver cancer caused by it among younger people in high-risk countries, they comment.
The investigators also observed a significant decrease in the incidence of liver cancer caused by HBV infection in people aged 30 to 59 years, although the decline was smaller than it was for those younger than 30.
Moreover, HCV infection has emerged as a concerning cause of liver cancer among those who used to be at low risk for HCV infection.
Although there is optimism that global control of HCV infection can be achieved through direct-acting antiviral agents, “the high cost, drug resistance, and reinfection rates are still major obstacles to fulfilling this ambitious goal,” Chen and colleagues point out.
The authors have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
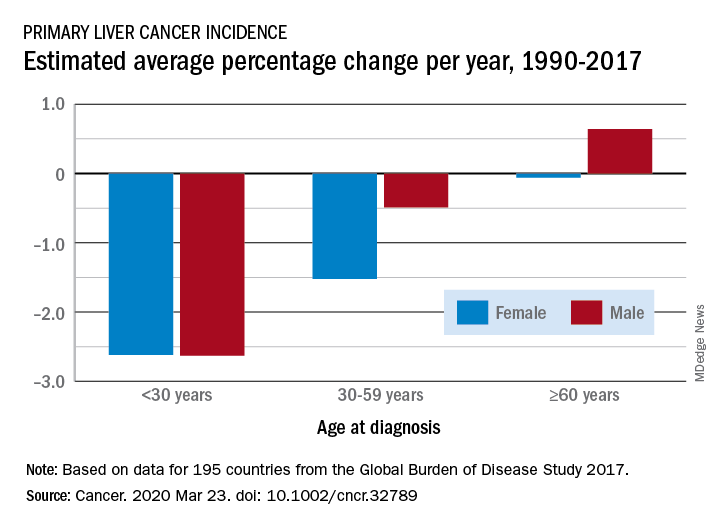
Liver cancer rates have been increasing, but a new analysis finds that the increase has occurred primarily in men older than 60 years in developed countries.
The findings come from an analysis of data from the Global Burden of Disease (GBD) Study 2017, published online March 23 in Cancer.
From 1990 to 2017, the number of cancer cases increased nearly threefold in older men and more than twofold in older women (aged 60 years or more). This increase was driven mainly by an increase in liver cancer caused by nonalcoholic steatohepatitis (NASH), also termed fatty liver disease, note the authors.
In contrast, the incidence of liver cancer among men and women who are younger than 30 years and those aged 30 to 59 years declined during this period.
The decreases seen in younger adults were largely ascribed to hepatitis B virus (HBV) vaccination and were consistent in most regions except in developed countries, where liver cancer rates increased irrespective of sex and age.
“Our findings suggest a lack of attention for older people in current liver cancer prevention efforts and highlight the emerging concern of obesity as a risk factor for liver cancer,” lead author Xingdong Chen, MD, PhD, Fudan University, China, said in a statement.
“Liver cancer prevention strategies in both developing and developed countries should be tailored and updated,” he added.
The authors point out that liver cancer was previously considered to be rare in the Western hemisphere.
“However, we found a significant increase in primary liver cancer incidence – regardless of etiology, sex, or age – in most of these countries over the last few decades,” they observe.
The fact that the most pronounced increase in liver cancer was caused by NASH suggests that more attention should be paid to weight management and obesity control as primary prevention strategies in these regions, they suggest.
Study design
Annual incidence data were collected from 1990 to 2017 and were categorized by sex, region, country, age group, and etiology.
“Data from a total of 195 countries and territories were available,” the investigators note, “and these countries and territories were categorized into 5 regions in terms of sociodemographic index (SDI),” they add.
Data were also retrieved regarding five etiologies of liver cancer: HBV infection, hepatitis C virus (HCV) infection, alcohol use, NASH, and others.
The authors note that age-standardized incidence rates of primary liver cancer caused by those five etiologies increased significantly in Australasia, Western Europe, and high-income regions of North America. The most significant increase was found in liver cancer caused by NASH in the Netherlands (in men) and in Finland (in women).
An increasing trend was observed in most countries for primary liver cancer among people aged 60 years or older, the authors note. They suggest that population expansion, aging, and increasing prevalence of obesity and diabetes might partly explain the marked increase, especially the dramatic increase in the number of cases among older people. Additionally, the “lag effect” of the large HBV infection reservoir in several countries might also contribute to the increase, the authors state. They explain that people infected with HBV early in life may experience progression to liver cancer as they age.
Primary prevention
Prevention of HBV infection – the primary cause of liver cancer – has been possible since the introduction of the HBV vaccine in 1982.
“By the end of 2017, 187 countries had introduced the HBV vaccine into their national immunization schedules, with global coverage with 3 doses of the hepatitis B vaccine ... estimated at 84%,” the authors point out.
This has “dramatically” reduced both the prevalence of HBV infection and the incidence of liver cancer caused by it among younger people in high-risk countries, they comment.
The investigators also observed a significant decrease in the incidence of liver cancer caused by HBV infection in people aged 30 to 59 years, although the decline was smaller than it was for those younger than 30.
Moreover, HCV infection has emerged as a concerning cause of liver cancer among those who used to be at low risk for HCV infection.
Although there is optimism that global control of HCV infection can be achieved through direct-acting antiviral agents, “the high cost, drug resistance, and reinfection rates are still major obstacles to fulfilling this ambitious goal,” Chen and colleagues point out.
The authors have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
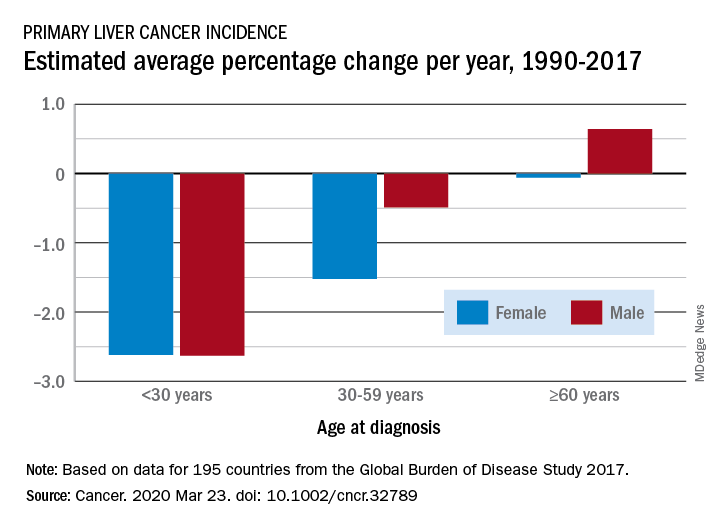
Liver cancer rates have been increasing, but a new analysis finds that the increase has occurred primarily in men older than 60 years in developed countries.
The findings come from an analysis of data from the Global Burden of Disease (GBD) Study 2017, published online March 23 in Cancer.
From 1990 to 2017, the number of cancer cases increased nearly threefold in older men and more than twofold in older women (aged 60 years or more). This increase was driven mainly by an increase in liver cancer caused by nonalcoholic steatohepatitis (NASH), also termed fatty liver disease, note the authors.
In contrast, the incidence of liver cancer among men and women who are younger than 30 years and those aged 30 to 59 years declined during this period.
The decreases seen in younger adults were largely ascribed to hepatitis B virus (HBV) vaccination and were consistent in most regions except in developed countries, where liver cancer rates increased irrespective of sex and age.
“Our findings suggest a lack of attention for older people in current liver cancer prevention efforts and highlight the emerging concern of obesity as a risk factor for liver cancer,” lead author Xingdong Chen, MD, PhD, Fudan University, China, said in a statement.
“Liver cancer prevention strategies in both developing and developed countries should be tailored and updated,” he added.
The authors point out that liver cancer was previously considered to be rare in the Western hemisphere.
“However, we found a significant increase in primary liver cancer incidence – regardless of etiology, sex, or age – in most of these countries over the last few decades,” they observe.
The fact that the most pronounced increase in liver cancer was caused by NASH suggests that more attention should be paid to weight management and obesity control as primary prevention strategies in these regions, they suggest.
Study design
Annual incidence data were collected from 1990 to 2017 and were categorized by sex, region, country, age group, and etiology.
“Data from a total of 195 countries and territories were available,” the investigators note, “and these countries and territories were categorized into 5 regions in terms of sociodemographic index (SDI),” they add.
Data were also retrieved regarding five etiologies of liver cancer: HBV infection, hepatitis C virus (HCV) infection, alcohol use, NASH, and others.
The authors note that age-standardized incidence rates of primary liver cancer caused by those five etiologies increased significantly in Australasia, Western Europe, and high-income regions of North America. The most significant increase was found in liver cancer caused by NASH in the Netherlands (in men) and in Finland (in women).
An increasing trend was observed in most countries for primary liver cancer among people aged 60 years or older, the authors note. They suggest that population expansion, aging, and increasing prevalence of obesity and diabetes might partly explain the marked increase, especially the dramatic increase in the number of cases among older people. Additionally, the “lag effect” of the large HBV infection reservoir in several countries might also contribute to the increase, the authors state. They explain that people infected with HBV early in life may experience progression to liver cancer as they age.
Primary prevention
Prevention of HBV infection – the primary cause of liver cancer – has been possible since the introduction of the HBV vaccine in 1982.
“By the end of 2017, 187 countries had introduced the HBV vaccine into their national immunization schedules, with global coverage with 3 doses of the hepatitis B vaccine ... estimated at 84%,” the authors point out.
This has “dramatically” reduced both the prevalence of HBV infection and the incidence of liver cancer caused by it among younger people in high-risk countries, they comment.
The investigators also observed a significant decrease in the incidence of liver cancer caused by HBV infection in people aged 30 to 59 years, although the decline was smaller than it was for those younger than 30.
Moreover, HCV infection has emerged as a concerning cause of liver cancer among those who used to be at low risk for HCV infection.
Although there is optimism that global control of HCV infection can be achieved through direct-acting antiviral agents, “the high cost, drug resistance, and reinfection rates are still major obstacles to fulfilling this ambitious goal,” Chen and colleagues point out.
The authors have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.