User login
SAN FRANCISCO – Single-nucleotide polymorphisms in genes for interleukin 10 and human leukocyte antigen are significantly associated with both systemic lupus erythematosus (SLE) and diffuse large B-cell lymphoma, according to a meta-analysis of data from three genome-wide association studies.
The findings add to existing data that exonerates immunosuppressive medications as the main causes of lymphoma in patients with SLE, said lead investigator Dr. Sasha Bernatsky of McGill University, Montreal, in an interview. “People with lupus may have a slight increase in risk for lymphoma because of genetic factors, which would be reassuring,” she said. “It may even mean that if you take your baseline risk of lupus and you control the inflammation, perhaps you can modify that small increase in risk of lymphoma and make it more like the risk in the general population.”
Diffuse large B-cell lymphoma (DLBCL) is the most common type of non-Hodgkin lymphoma, with an incidence of about one case in 3,000 person-years in the general population and about one case in 1,000 person-years in patients with SLE, Dr. Bernatsky noted. To look for shared genetic risk factors for both diseases, she and her colleagues analyzed pooled data from three genome-wide association studies conducted by the International Lymphoma Epidemiology Consortium. Using data from 3,857 patients with DLBCL and 7,666 controls, the investigators calculated the odds of DLBCL for each of 28 SNPs that are known genetic risk variants for SLE. “If there’s an overlap there, that might be the key,” Dr. Bernatsky said at the annual meeting of the American College of Rheumatology.
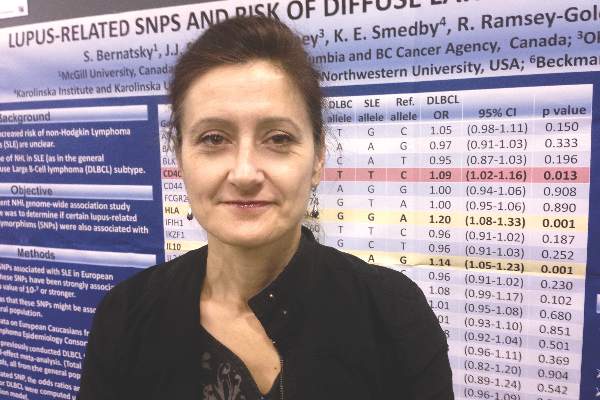
In fact, two SLE-related SNPs were clearly linked to an increased risk for DLBCL – rs3024505, a variant allele of the gene for interleukin 10 on chromosome 1 (odds ratio, 1.14; 95% confidence interval, 1.05-1.23; P = .001), and rs1270942, a variant of the gene for human leukocyte antigen on chromosome 6 (OR, 1.2; 95% CI, 1.08-1.33; P = .0007). Both SNPs seem plausible – interleukin 10 induces the bcl-2 protein, which prevents the spontaneous death of germinal center B cells, and some evidence has linked HLA polymorphisms to DLBCL, Dr. Bernatsky said.
The study also linked two other SLE-related SNPs to increased risk for DLBCL, although the associations were not as strong. The first was rs4810485 on the CD40 gene (OR, 1.09; 95% CI, 1.02-1.16; P = .013), and the second was rs2205960 on the TNFSF4 gene, which encodes a cytokine from the tumor necrosis factor–superfamily (OR, 1.08; 95% CI, 1.02-1.15; P = .044). “These findings kind of make sense, because tumor necrosis factor is a very important inflammatory cytokine, and CD40 is a lymphocyte marker,” Dr. Bernatsky said. “It is possible that some genetic factor that controls their expression or function might be associated with lymphoma.”
Rheumatologists have long debated why patients with lupus are at increased risk for lymphoma, and have repeatedly asked whether immunomodulatory drugs are to blame. “We can exercise some caution, but still be aware that most people who use these drugs never end up developing cancer,” Dr. Bernatsky emphasized. In past studies, the absolute risk of lymphoma in patients with SLE remained below 1%, and those patients who did develop lymphoma often had never received drugs such as azathioprine, she noted. The exception was cyclophosphamide, which caused various severe adverse effects, including blood cancers (Ann Rheum Dis. 2013 Jan 8. doi: 10.1136/annrheumdis-2012-202099). “Although we need to use cyclophosphamide for very severe cases of autoimmune disease, it’s clearly a drug that we should use almost as a last resort,” she said.
The study was funded by the Canadian Institutes for Health Research; the Fonds du recherche du Québec; Santé, the Research Institute of the McGill University Health Centre; and the Singer Family Fund for Lupus Research. Dr. Bernatsky and her coinvestigators had no disclosures.
SAN FRANCISCO – Single-nucleotide polymorphisms in genes for interleukin 10 and human leukocyte antigen are significantly associated with both systemic lupus erythematosus (SLE) and diffuse large B-cell lymphoma, according to a meta-analysis of data from three genome-wide association studies.
The findings add to existing data that exonerates immunosuppressive medications as the main causes of lymphoma in patients with SLE, said lead investigator Dr. Sasha Bernatsky of McGill University, Montreal, in an interview. “People with lupus may have a slight increase in risk for lymphoma because of genetic factors, which would be reassuring,” she said. “It may even mean that if you take your baseline risk of lupus and you control the inflammation, perhaps you can modify that small increase in risk of lymphoma and make it more like the risk in the general population.”
Diffuse large B-cell lymphoma (DLBCL) is the most common type of non-Hodgkin lymphoma, with an incidence of about one case in 3,000 person-years in the general population and about one case in 1,000 person-years in patients with SLE, Dr. Bernatsky noted. To look for shared genetic risk factors for both diseases, she and her colleagues analyzed pooled data from three genome-wide association studies conducted by the International Lymphoma Epidemiology Consortium. Using data from 3,857 patients with DLBCL and 7,666 controls, the investigators calculated the odds of DLBCL for each of 28 SNPs that are known genetic risk variants for SLE. “If there’s an overlap there, that might be the key,” Dr. Bernatsky said at the annual meeting of the American College of Rheumatology.
In fact, two SLE-related SNPs were clearly linked to an increased risk for DLBCL – rs3024505, a variant allele of the gene for interleukin 10 on chromosome 1 (odds ratio, 1.14; 95% confidence interval, 1.05-1.23; P = .001), and rs1270942, a variant of the gene for human leukocyte antigen on chromosome 6 (OR, 1.2; 95% CI, 1.08-1.33; P = .0007). Both SNPs seem plausible – interleukin 10 induces the bcl-2 protein, which prevents the spontaneous death of germinal center B cells, and some evidence has linked HLA polymorphisms to DLBCL, Dr. Bernatsky said.
The study also linked two other SLE-related SNPs to increased risk for DLBCL, although the associations were not as strong. The first was rs4810485 on the CD40 gene (OR, 1.09; 95% CI, 1.02-1.16; P = .013), and the second was rs2205960 on the TNFSF4 gene, which encodes a cytokine from the tumor necrosis factor–superfamily (OR, 1.08; 95% CI, 1.02-1.15; P = .044). “These findings kind of make sense, because tumor necrosis factor is a very important inflammatory cytokine, and CD40 is a lymphocyte marker,” Dr. Bernatsky said. “It is possible that some genetic factor that controls their expression or function might be associated with lymphoma.”
Rheumatologists have long debated why patients with lupus are at increased risk for lymphoma, and have repeatedly asked whether immunomodulatory drugs are to blame. “We can exercise some caution, but still be aware that most people who use these drugs never end up developing cancer,” Dr. Bernatsky emphasized. In past studies, the absolute risk of lymphoma in patients with SLE remained below 1%, and those patients who did develop lymphoma often had never received drugs such as azathioprine, she noted. The exception was cyclophosphamide, which caused various severe adverse effects, including blood cancers (Ann Rheum Dis. 2013 Jan 8. doi: 10.1136/annrheumdis-2012-202099). “Although we need to use cyclophosphamide for very severe cases of autoimmune disease, it’s clearly a drug that we should use almost as a last resort,” she said.
The study was funded by the Canadian Institutes for Health Research; the Fonds du recherche du Québec; Santé, the Research Institute of the McGill University Health Centre; and the Singer Family Fund for Lupus Research. Dr. Bernatsky and her coinvestigators had no disclosures.
SAN FRANCISCO – Single-nucleotide polymorphisms in genes for interleukin 10 and human leukocyte antigen are significantly associated with both systemic lupus erythematosus (SLE) and diffuse large B-cell lymphoma, according to a meta-analysis of data from three genome-wide association studies.
The findings add to existing data that exonerates immunosuppressive medications as the main causes of lymphoma in patients with SLE, said lead investigator Dr. Sasha Bernatsky of McGill University, Montreal, in an interview. “People with lupus may have a slight increase in risk for lymphoma because of genetic factors, which would be reassuring,” she said. “It may even mean that if you take your baseline risk of lupus and you control the inflammation, perhaps you can modify that small increase in risk of lymphoma and make it more like the risk in the general population.”
Diffuse large B-cell lymphoma (DLBCL) is the most common type of non-Hodgkin lymphoma, with an incidence of about one case in 3,000 person-years in the general population and about one case in 1,000 person-years in patients with SLE, Dr. Bernatsky noted. To look for shared genetic risk factors for both diseases, she and her colleagues analyzed pooled data from three genome-wide association studies conducted by the International Lymphoma Epidemiology Consortium. Using data from 3,857 patients with DLBCL and 7,666 controls, the investigators calculated the odds of DLBCL for each of 28 SNPs that are known genetic risk variants for SLE. “If there’s an overlap there, that might be the key,” Dr. Bernatsky said at the annual meeting of the American College of Rheumatology.
In fact, two SLE-related SNPs were clearly linked to an increased risk for DLBCL – rs3024505, a variant allele of the gene for interleukin 10 on chromosome 1 (odds ratio, 1.14; 95% confidence interval, 1.05-1.23; P = .001), and rs1270942, a variant of the gene for human leukocyte antigen on chromosome 6 (OR, 1.2; 95% CI, 1.08-1.33; P = .0007). Both SNPs seem plausible – interleukin 10 induces the bcl-2 protein, which prevents the spontaneous death of germinal center B cells, and some evidence has linked HLA polymorphisms to DLBCL, Dr. Bernatsky said.
The study also linked two other SLE-related SNPs to increased risk for DLBCL, although the associations were not as strong. The first was rs4810485 on the CD40 gene (OR, 1.09; 95% CI, 1.02-1.16; P = .013), and the second was rs2205960 on the TNFSF4 gene, which encodes a cytokine from the tumor necrosis factor–superfamily (OR, 1.08; 95% CI, 1.02-1.15; P = .044). “These findings kind of make sense, because tumor necrosis factor is a very important inflammatory cytokine, and CD40 is a lymphocyte marker,” Dr. Bernatsky said. “It is possible that some genetic factor that controls their expression or function might be associated with lymphoma.”
Rheumatologists have long debated why patients with lupus are at increased risk for lymphoma, and have repeatedly asked whether immunomodulatory drugs are to blame. “We can exercise some caution, but still be aware that most people who use these drugs never end up developing cancer,” Dr. Bernatsky emphasized. In past studies, the absolute risk of lymphoma in patients with SLE remained below 1%, and those patients who did develop lymphoma often had never received drugs such as azathioprine, she noted. The exception was cyclophosphamide, which caused various severe adverse effects, including blood cancers (Ann Rheum Dis. 2013 Jan 8. doi: 10.1136/annrheumdis-2012-202099). “Although we need to use cyclophosphamide for very severe cases of autoimmune disease, it’s clearly a drug that we should use almost as a last resort,” she said.
The study was funded by the Canadian Institutes for Health Research; the Fonds du recherche du Québec; Santé, the Research Institute of the McGill University Health Centre; and the Singer Family Fund for Lupus Research. Dr. Bernatsky and her coinvestigators had no disclosures.
AT THE ACR ANNUAL MEETING
Key clinical point: Two genetic risk variants for systemic lupus erythematosus also were clearly linked to risk of diffuse large B-cell lymphoma.
Major finding: The single-nucleotide polymorphisms were rs3024505 on chromosome 1 (OR, 1.14; P = .001), and rs1270942 on chromosome 6 (OR, 1.2; P = .0007).
Data source: A fixed-effect meta-analysis of 28 SLE-related SNPs from 3,857 patients with diffuse large B-cell lymphoma and 7,666 controls.
Disclosures: The study was funded by the Canadian Institutes for Health Research; the Fonds du recherche du Québec; Santé, the Research Institute of the McGill University Health Centre; and the Singer Family Fund for Lupus Research. Dr. Bernatsky and her coinvestigators had no disclosures.