User login
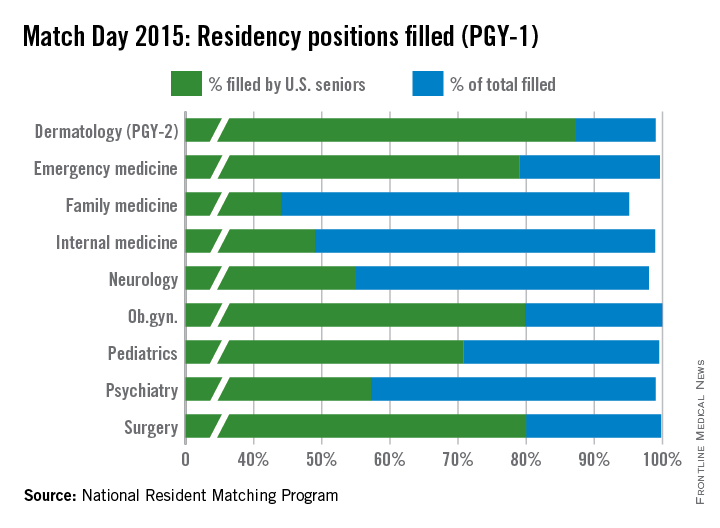
Medical school seniors continue to show an increasing interest in primary care, according to the results of the 2015 Main Residency Match.
And for the third year in a row a record number of first- and second-year residency positions were offered – 30,212 positions, up from the 29,671 positions in 2014, according to the National Resident Matching Program (NRMP).
Family medicine residency programs offered a total of 3,195 positions in the 2105 match, up from 3,109 last year. Greater than 95% of those positions were filled; 44% were filled by U.S. medical school graduates, the NRMP announced March 20.
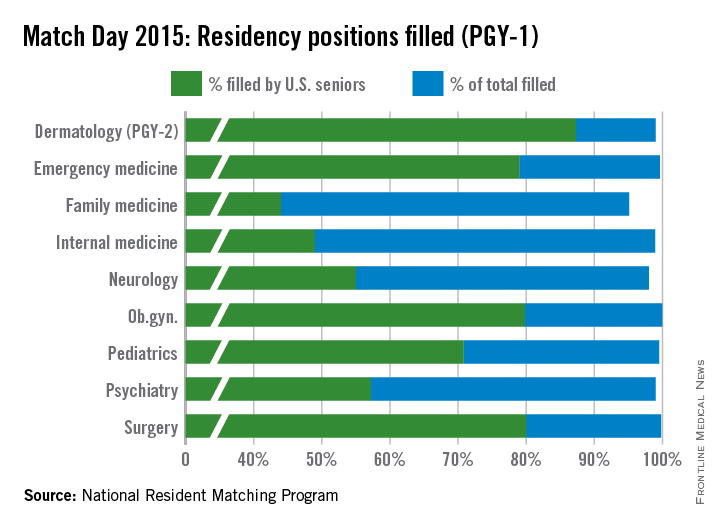
Numbers were similar in internal medicine, where residency programs offered 6,770 positions this year, up from 6,542 in 2014. Just under 99% of positions were filled, with 49% filled by U.S. medical school graduates.
The match results demonstrate “stability in the number of individuals going into internal medicine,” Dr. Patrick Alguire, senior vice president for medical education at the American College of Physicians, said in an interview. “We’re impressed that there were more students in this year’s match and there were more training positions available in this year’s match as well and yet despite that, we were able to continue to fill most of the programs.”
Dr. Robert Wergin, president of the American Academy of Family Physicians expressed some concern about the number of U.S. medical school graduates matching to family medicine.
“We saw a consistent and increasing growth in U.S. medical students matching to family medicine during the implementation of health system reforms that emphasized the importance of comprehensive primary medical care,” Dr. Wergin said in a statement. “That has slowed as policy makers have pulled back from supporting primary medical care.”
Pediatric positions saw a slight increase in the total number of positions offered to 2,668 from 2,640. U.S. graduates matched to 71% of the 2,654 positions filled. The 1,889 positions filled by U.S. medical school students is up from the 1,818 slots filled in 2014, suggesting last year’s decline was just a blip in a 5-year trend that has been increasing each year in general.
The increase in primary care positions also caught the eye of NRMP President and CEO Mona Signer.
“It’s a good trend for health manpower in general that there are more primary care physicians because, obviously, if you’ve done any reading at all, you know that primary care is where a shortage is anticipated,” Ms. Signer said in an interview.
Concerns still remain regarding whether future primary care workforce needs will be met. Key obstacles include sizable medical school debt and the hassles of owning a medical practice, Dr Alguire said. “I have a feeling that unless those are addressed head on with a national strategy for improving the physician workforce in the United States, these problems will continue.”
He added that the geographic distribution of the physician workforce is problematic, too.
“If you look at the distribution of many physicians, they tend to congregate in cities and there are fewer primary care physicians in the areas of greater need in rural areas and I think we need to address that strategically rather than simply hoping that physicians will go to those areas of great need and begin to practice primary care,” Dr. Alguire said.
Dr. Wergin added that the increases need to speed “dramatically” to ensure necessary access to primary care.
Medical school seniors continue to show an increasing interest in primary care, according to the results of the 2015 Main Residency Match.
And for the third year in a row a record number of first- and second-year residency positions were offered – 30,212 positions, up from the 29,671 positions in 2014, according to the National Resident Matching Program (NRMP).
Family medicine residency programs offered a total of 3,195 positions in the 2105 match, up from 3,109 last year. Greater than 95% of those positions were filled; 44% were filled by U.S. medical school graduates, the NRMP announced March 20.
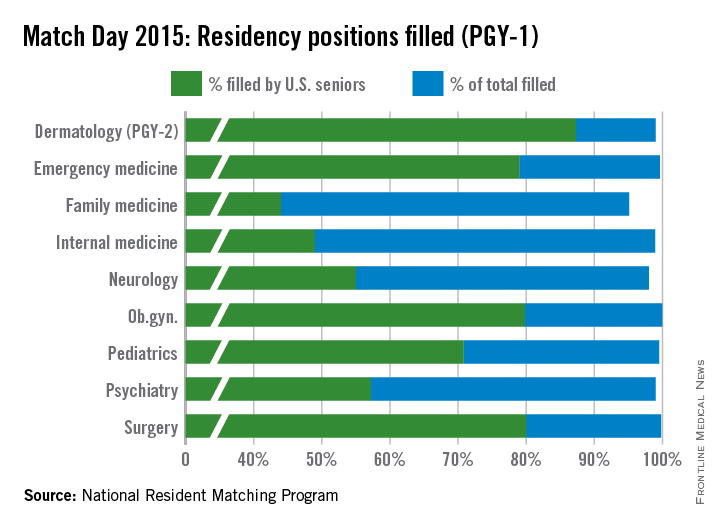
Numbers were similar in internal medicine, where residency programs offered 6,770 positions this year, up from 6,542 in 2014. Just under 99% of positions were filled, with 49% filled by U.S. medical school graduates.
The match results demonstrate “stability in the number of individuals going into internal medicine,” Dr. Patrick Alguire, senior vice president for medical education at the American College of Physicians, said in an interview. “We’re impressed that there were more students in this year’s match and there were more training positions available in this year’s match as well and yet despite that, we were able to continue to fill most of the programs.”
Dr. Robert Wergin, president of the American Academy of Family Physicians expressed some concern about the number of U.S. medical school graduates matching to family medicine.
“We saw a consistent and increasing growth in U.S. medical students matching to family medicine during the implementation of health system reforms that emphasized the importance of comprehensive primary medical care,” Dr. Wergin said in a statement. “That has slowed as policy makers have pulled back from supporting primary medical care.”
Pediatric positions saw a slight increase in the total number of positions offered to 2,668 from 2,640. U.S. graduates matched to 71% of the 2,654 positions filled. The 1,889 positions filled by U.S. medical school students is up from the 1,818 slots filled in 2014, suggesting last year’s decline was just a blip in a 5-year trend that has been increasing each year in general.
The increase in primary care positions also caught the eye of NRMP President and CEO Mona Signer.
“It’s a good trend for health manpower in general that there are more primary care physicians because, obviously, if you’ve done any reading at all, you know that primary care is where a shortage is anticipated,” Ms. Signer said in an interview.
Concerns still remain regarding whether future primary care workforce needs will be met. Key obstacles include sizable medical school debt and the hassles of owning a medical practice, Dr Alguire said. “I have a feeling that unless those are addressed head on with a national strategy for improving the physician workforce in the United States, these problems will continue.”
He added that the geographic distribution of the physician workforce is problematic, too.
“If you look at the distribution of many physicians, they tend to congregate in cities and there are fewer primary care physicians in the areas of greater need in rural areas and I think we need to address that strategically rather than simply hoping that physicians will go to those areas of great need and begin to practice primary care,” Dr. Alguire said.
Dr. Wergin added that the increases need to speed “dramatically” to ensure necessary access to primary care.
Medical school seniors continue to show an increasing interest in primary care, according to the results of the 2015 Main Residency Match.
And for the third year in a row a record number of first- and second-year residency positions were offered – 30,212 positions, up from the 29,671 positions in 2014, according to the National Resident Matching Program (NRMP).
Family medicine residency programs offered a total of 3,195 positions in the 2105 match, up from 3,109 last year. Greater than 95% of those positions were filled; 44% were filled by U.S. medical school graduates, the NRMP announced March 20.
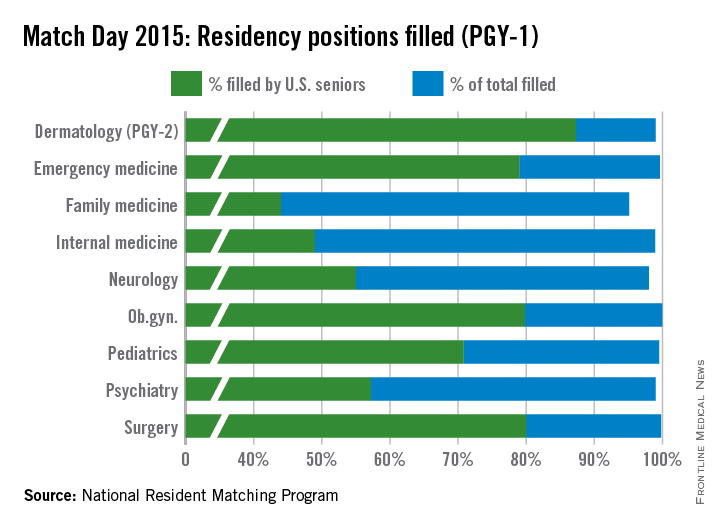
Numbers were similar in internal medicine, where residency programs offered 6,770 positions this year, up from 6,542 in 2014. Just under 99% of positions were filled, with 49% filled by U.S. medical school graduates.
The match results demonstrate “stability in the number of individuals going into internal medicine,” Dr. Patrick Alguire, senior vice president for medical education at the American College of Physicians, said in an interview. “We’re impressed that there were more students in this year’s match and there were more training positions available in this year’s match as well and yet despite that, we were able to continue to fill most of the programs.”
Dr. Robert Wergin, president of the American Academy of Family Physicians expressed some concern about the number of U.S. medical school graduates matching to family medicine.
“We saw a consistent and increasing growth in U.S. medical students matching to family medicine during the implementation of health system reforms that emphasized the importance of comprehensive primary medical care,” Dr. Wergin said in a statement. “That has slowed as policy makers have pulled back from supporting primary medical care.”
Pediatric positions saw a slight increase in the total number of positions offered to 2,668 from 2,640. U.S. graduates matched to 71% of the 2,654 positions filled. The 1,889 positions filled by U.S. medical school students is up from the 1,818 slots filled in 2014, suggesting last year’s decline was just a blip in a 5-year trend that has been increasing each year in general.
The increase in primary care positions also caught the eye of NRMP President and CEO Mona Signer.
“It’s a good trend for health manpower in general that there are more primary care physicians because, obviously, if you’ve done any reading at all, you know that primary care is where a shortage is anticipated,” Ms. Signer said in an interview.
Concerns still remain regarding whether future primary care workforce needs will be met. Key obstacles include sizable medical school debt and the hassles of owning a medical practice, Dr Alguire said. “I have a feeling that unless those are addressed head on with a national strategy for improving the physician workforce in the United States, these problems will continue.”
He added that the geographic distribution of the physician workforce is problematic, too.
“If you look at the distribution of many physicians, they tend to congregate in cities and there are fewer primary care physicians in the areas of greater need in rural areas and I think we need to address that strategically rather than simply hoping that physicians will go to those areas of great need and begin to practice primary care,” Dr. Alguire said.
Dr. Wergin added that the increases need to speed “dramatically” to ensure necessary access to primary care.