User login
Many physicians continue to be frustrated and confused by the meaningful use criteria that spell out how they can receive incentive payments from Medicare and Medicaid for their use of electronic health records.
With that uncertainty, physicians are not jumping in with both feet to participate in the incentive program, even if they have purchased EHR systems. The Medical Group Management Association (MGMA) surveyed its members in April and found that 80% of those who already had adopted an EHR system said that they intended to participate. But at that time, only about 14% said that they were able to meet all of the criteria.
The American Medical Association held a special session on meaningful use at its House of Delegates meeting in June. When the speaker – Dr. Michael L. Hodgkins, an AMA chief medical information officer – asked how many physicians were confused about what was expected of them, more than half raised their hands.
Physicians in smaller practices are especially challenged, Dr. Hodgkins said, citing data that some 300,000 doctors are in practices of 10 or fewer physicians. Among those, fewer than 15% have implemented an EHR system, and most are not yet capable of meeting the meaningful use criteria.
According to Dr. Hodgkins, there are many obstacles to meeting meaningful use, including selecting from the more than 400 EHR products certified by the federal Office of the National Coordinator (ONC) for Health Information Technology, part of the Health and Human Services department.
Another problem: "Aggressive" timelines set by the government, according to Dr. Steve Waldren, director of the Center for Health Information Technology at the American Academy of Family Physicians (AAFP).
Dr. Waldren says it takes generally 6-18 months from purchase to active meaningful use of a system.
It’s been a tough road, he said. Physicians who don’t have EHRs or who have just gotten on board are struggling to get them operational and to achieve meaningful use. Those who have owned systems for awhile may face upgrades in order to meet the meaningful use criteria.
Meanwhile, there’s the system’s financial cost, training, and maintenance issues, and workflow changes once a system is in place.
The Long-Time User
Some physicians aren’t in a panic about the impending deadlines. Dr. Michael Mirro of Ft. Wayne (Ind.) Cardiology, a 24-physician group, said that his practice has been using health IT since 1996.
"We knew that we had to ultimately modernize our practice," Dr. Mirro said in an interview. Their current system has improved efficiency and quality, and has "supported a higher level of coding and reimbursement."
The system has "pretty much complete functionality," said Dr. Mirro. It provides the EHR, offers e-prescribing and decision-support tools, and can be used for direct quality reporting to the American College of Cardiology’s PINNACLE registry.
The system is web based, which reduces maintenance costs and IT headaches. The practice does not own the servers; it merely has local computers that interact with the vendor’s servers and software. The system is certified by the Certification Commission for Health Information Technology and was updated to ensure that the practice would meet the meaningful use criteria. One helpful tool, according to Dr. Mirro: A meaningful use "meter" that tells the physicians how well they are meeting the goals.
Ft. Wayne Cardiology has already attested to the government that it was a meaningful user and has received the maximum $18,000 per physician incentive for 2011, Dr. Mirro said.
The annual cost is about $2,000 per physician per year. That’s low, said Dr. Mirro, because his practice is owned by a hospital. The system is already somewhat ahead of the curve, as it already incorporates a patient web portal (a stage 2 goal).
He said that he is sympathetic to physicians who are just getting started.
"Any time you adopt technology at the point of care, it’s going to require a change in workflow," he said. That was definitely the case at Ft. Wayne Cardiology. For example, because some of the practice’s physicians still don’t know how to type, the system has templates that require point-and-click data entry to avoid errors.
Dr. Mirro said that physicians who are looking to buy or expand their health IT should talk with one of the 60 regional extension centers established by the ONC. These centers have been charged to help rural physicians and primary care physicians especially, and they offer vendor recommendations, practice audits, and other advice for free.
Dr. Mirro said that he believes most cardiologists will be forced to purchase an EHR sooner rather than later. With the decline in reimbursement (particularly for imaging services), cardiologists are increasingly being employed by hospitals. Those institutions – which themselves are facing a huge penalty if they don’t comply with meaningful use by 2017 – will want to have a lot of connectivity with the physician practice.
A Model For Her Peers
In 2005, Dr. Jennifer Brull figured that she needed to get on board with health IT, even though it might be expensive and difficult for a family physician in a rural Kansas solo practice. A younger physician with whom she was collaborating suggested that having an EHR was the wave of the future, and would likely be a necessity going forward. She also had a practice-sharing arrangement with another physician, who was older. He wasn’t as sure, said Dr. Brull in an interview.
But they moved ahead and spent 3 years selecting, buying, and implementing an EHR system that they could all use, said Dr. Brull, who practices in Plainview. She took out a loan for $50,000 to buy the equipment; her colleagues contributed to the software and other costs.
Because they practice in a rural area, there was no possibility of using a web-based model; broadband access in her area is still not robust enough, said Dr. Brull. So she has a server onsite at her office, and recently purchased a second server for $3,000. The net cost so far has been about $30,000 per physician, Dr. Brull said.
The first 6 months were a challenge, she said. "Anytime you do something that’s a complete paradigm shift, it’s hard. It’s hard mentally to think about all those changes, hard physically because you’re investing more time and effort, and hard emotionally because your staff gets freaked out."
In addition to allowing the practice to meet meaningful use criteria, the system also has a patient portal. The physicians are preparing to be able to participate in the state’s health information exchange.
Dr. Brull said that she disagrees with physicians who say that adopting an EHR interrupts the workflow or comes between the physician and patient.
"I’ve found it easier to be more collaborative [with my patients]," she said. One example: She recently used an EHR-generated graph to show a patient that she had gained 40 pounds over 3 years. The graph made much more of an impression on the patient than Dr. Brull could have done by reading numbers off a paper chart, she said.
"This whole project has resulted in dramatic quality improvement for my practice," Dr. Brull added.
Another example: She implemented a quality measure on breast cancer screening. Just by having a flag in the EHR, she went from screening 50% of patients to almost 100%. "Having the data at your fingertips makes you aware of where you do a good job and where you don’t," Dr. Brull said.
In April, Dr. Brull collected the full Medicare incentive payment for 2011. Her colleagues weren’t ready, but that didn’t matter. Physicians can choose to attest to meaningful use on their own time frame, regardless of where their colleagues might be, she said.
Dr. Brull has become an evangelist for the power of the EHR and meaningful use. She was chosen to speak at a CMS press conference announcing the first round of Medicare incentive payments. And she is a member of the regional extension center in Kansas. The ONC also named her a "MUVer" – someone who serves as a local leader and adviser.
The Reluctant Adopter
Dr. Michael Machen is one of the physicians who consulted with Dr. Brull. He practices with four other family physicians in nearby Quinter, Kan. (population, 980). The impetus for taking on an EHR came from his younger partners, Dr. Machen said in an interview. They were also motivated by the meaningful use program, and got started in July 2010.
One junior partner became the EHR champion, doing much of the legwork to find appropriate vendors and systems. The physicians also attended seminars and webinars offered by the Kansas Medical Society and the Kansas chapter of the AAFP. A team from the regional extension center visited their practice too, Dr. Machen said.
They borrowed $75,000 to purchase hardware and software. The biggest cost is the $2,000-$4,000 they spend monthly on IT support – a necessity when there is no one with such expertise in the practice or locally. The IT help comes from more than an hour away. Dr. Machen and his colleagues house the server themselves; broadband is no better in Quinter than it is in Plainview.
Dr. Machen said that the younger physicians have all done well with the system, but he is struggling.
"I’m not technically inclined, and I have very little computer knowledge," he said.
It has also been difficult for his nurse, who is spending more time on data entry and less on interacting with patients, Dr. Machen said, adding that they are both in their late 50s and are more frustrated with the system than are their younger colleagues.
His staff has been happy; there’s no more searching for charts, and coding is easier, he said. And he does see the potential for improving quality, especially with the data-collection effort, warnings about drug interactions, and prompts for screening tests.
But for the time being, "it’s horrible with the workflow and the patient flow." On days of 15-20 patient visits, using the EHR is not as much of an issue. But on days of 30 patient visits, "it’s not doable," he said.
So far, patients haven’t been wild about the transition, either. They don’t like the physician to be working on a computer during the visit, he said. And "I don’t like it much, either," said Dr. Machen. "When I was in medical school, I was taught that the second you enter the exam room, the patient has your undivided attention." That’s not really possible with an EHR, at least the way he sees it currently, although he also can see possible solutions, such as having a scribe.
Dr. Machen also said he has concerns about whether it’s possible to truly secure an EHR, and, whether the systems will truly improve patient outcomes. The jury is still out on that, he said.
But, he added, "I don’t want to be a naysayer." He said that he’s "on the upward slope of the learning curve," and expects to get more comfortable eventually.
In September, he’ll begin his 90-day period of meaningful use, with the aim of receiving an incentive payment by the end of the year.
Medicare and Medicaid Incentives
The ONC provides the central leadership for the Medicare and Medicaid EHR incentive programs. The HITECH (Health Information Technology for Economic and Clinical Health) Act directly appropriated $2 billion to the ONC to spend on incentives and administration of the program. The federal regulation governing the incentive program (some 800 pages) was issued in July 2010.
This year – 2011 – is the first year in which physicians can participate; they have until Oct. 1 to attest that they are meaningful users. To be eligible for incentive payments, physicians have to meet the meaningful use criteria for 90 consecutive days.
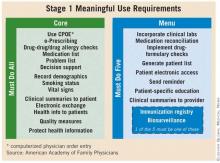
The criteria are being introduced in stages over the next 4-5 years. Stage 1 outlines what is expected in 2011 and 2012. Stage 2 was expected to be put into place in 2013, but in June, the Health IT Policy Committee of the Centers for Medicare and Medicaid Services voted to delay implementation until 2014, but only for physicians who were already participating. Physicians who wait until 2012 or later would still be expected to meet stage 2 criteria in 2013.
Physicians who want to participate have to choose between the Medicare or Medicaid incentive program. Those who take part in the Medicare program are eligible to receive incentive payments of $44,000 over 5 years. However, the payments will be made only through 2016. Physicians who wait until 2012 to start would still earn the $44,000 maximum; those who start later would receive prorated payments.
Physicians who practice in designated Health Professional Shortage Areas (HPSA) may be eligible for an additional 10% in each year’s incentive payment.
Importantly, Medicare begins to penalize nonparticipating physicians starting in 2016.
The Medicaid incentives are more generous: A total of $63,750 can be paid out over 6 years. And there’s a longer time frame. Eligible professionals can wait until 2016 to start participating and still receive the maximum payout over a 6-year period.
In late May, the CMS announced that $75 million in Medicare incentives had been awarded to physicians and hospitals in the first 2 weeks of the program. Some states began paying out Medicaid incentives in January. By late May, $83 million had been issued.
Meaningful use of EHRs is critical, according to Dr. Farzad Mostashari, the National Coordinator, who testified to the House Small Business Committee’s Subcommittee on Healthcare and Technology in June.
"If all we do is put an EHR in every provider’s office or hospital, we will have failed to realize health IT’s full potential," he said. "Instead, doctors, hospitals, and other providers need to use robust EHR technology in a meaningful and interoperable way to improve care."
Many physicians continue to be frustrated and confused by the meaningful use criteria that spell out how they can receive incentive payments from Medicare and Medicaid for their use of electronic health records.
With that uncertainty, physicians are not jumping in with both feet to participate in the incentive program, even if they have purchased EHR systems. The Medical Group Management Association (MGMA) surveyed its members in April and found that 80% of those who already had adopted an EHR system said that they intended to participate. But at that time, only about 14% said that they were able to meet all of the criteria.
The American Medical Association held a special session on meaningful use at its House of Delegates meeting in June. When the speaker – Dr. Michael L. Hodgkins, an AMA chief medical information officer – asked how many physicians were confused about what was expected of them, more than half raised their hands.
Physicians in smaller practices are especially challenged, Dr. Hodgkins said, citing data that some 300,000 doctors are in practices of 10 or fewer physicians. Among those, fewer than 15% have implemented an EHR system, and most are not yet capable of meeting the meaningful use criteria.
According to Dr. Hodgkins, there are many obstacles to meeting meaningful use, including selecting from the more than 400 EHR products certified by the federal Office of the National Coordinator (ONC) for Health Information Technology, part of the Health and Human Services department.
Another problem: "Aggressive" timelines set by the government, according to Dr. Steve Waldren, director of the Center for Health Information Technology at the American Academy of Family Physicians (AAFP).
Dr. Waldren says it takes generally 6-18 months from purchase to active meaningful use of a system.
It’s been a tough road, he said. Physicians who don’t have EHRs or who have just gotten on board are struggling to get them operational and to achieve meaningful use. Those who have owned systems for awhile may face upgrades in order to meet the meaningful use criteria.
Meanwhile, there’s the system’s financial cost, training, and maintenance issues, and workflow changes once a system is in place.
The Long-Time User
Some physicians aren’t in a panic about the impending deadlines. Dr. Michael Mirro of Ft. Wayne (Ind.) Cardiology, a 24-physician group, said that his practice has been using health IT since 1996.
"We knew that we had to ultimately modernize our practice," Dr. Mirro said in an interview. Their current system has improved efficiency and quality, and has "supported a higher level of coding and reimbursement."
The system has "pretty much complete functionality," said Dr. Mirro. It provides the EHR, offers e-prescribing and decision-support tools, and can be used for direct quality reporting to the American College of Cardiology’s PINNACLE registry.
The system is web based, which reduces maintenance costs and IT headaches. The practice does not own the servers; it merely has local computers that interact with the vendor’s servers and software. The system is certified by the Certification Commission for Health Information Technology and was updated to ensure that the practice would meet the meaningful use criteria. One helpful tool, according to Dr. Mirro: A meaningful use "meter" that tells the physicians how well they are meeting the goals.
Ft. Wayne Cardiology has already attested to the government that it was a meaningful user and has received the maximum $18,000 per physician incentive for 2011, Dr. Mirro said.
The annual cost is about $2,000 per physician per year. That’s low, said Dr. Mirro, because his practice is owned by a hospital. The system is already somewhat ahead of the curve, as it already incorporates a patient web portal (a stage 2 goal).
He said that he is sympathetic to physicians who are just getting started.
"Any time you adopt technology at the point of care, it’s going to require a change in workflow," he said. That was definitely the case at Ft. Wayne Cardiology. For example, because some of the practice’s physicians still don’t know how to type, the system has templates that require point-and-click data entry to avoid errors.
Dr. Mirro said that physicians who are looking to buy or expand their health IT should talk with one of the 60 regional extension centers established by the ONC. These centers have been charged to help rural physicians and primary care physicians especially, and they offer vendor recommendations, practice audits, and other advice for free.
Dr. Mirro said that he believes most cardiologists will be forced to purchase an EHR sooner rather than later. With the decline in reimbursement (particularly for imaging services), cardiologists are increasingly being employed by hospitals. Those institutions – which themselves are facing a huge penalty if they don’t comply with meaningful use by 2017 – will want to have a lot of connectivity with the physician practice.
A Model For Her Peers
In 2005, Dr. Jennifer Brull figured that she needed to get on board with health IT, even though it might be expensive and difficult for a family physician in a rural Kansas solo practice. A younger physician with whom she was collaborating suggested that having an EHR was the wave of the future, and would likely be a necessity going forward. She also had a practice-sharing arrangement with another physician, who was older. He wasn’t as sure, said Dr. Brull in an interview.
But they moved ahead and spent 3 years selecting, buying, and implementing an EHR system that they could all use, said Dr. Brull, who practices in Plainview. She took out a loan for $50,000 to buy the equipment; her colleagues contributed to the software and other costs.
Because they practice in a rural area, there was no possibility of using a web-based model; broadband access in her area is still not robust enough, said Dr. Brull. So she has a server onsite at her office, and recently purchased a second server for $3,000. The net cost so far has been about $30,000 per physician, Dr. Brull said.
The first 6 months were a challenge, she said. "Anytime you do something that’s a complete paradigm shift, it’s hard. It’s hard mentally to think about all those changes, hard physically because you’re investing more time and effort, and hard emotionally because your staff gets freaked out."
In addition to allowing the practice to meet meaningful use criteria, the system also has a patient portal. The physicians are preparing to be able to participate in the state’s health information exchange.
Dr. Brull said that she disagrees with physicians who say that adopting an EHR interrupts the workflow or comes between the physician and patient.
"I’ve found it easier to be more collaborative [with my patients]," she said. One example: She recently used an EHR-generated graph to show a patient that she had gained 40 pounds over 3 years. The graph made much more of an impression on the patient than Dr. Brull could have done by reading numbers off a paper chart, she said.
"This whole project has resulted in dramatic quality improvement for my practice," Dr. Brull added.
Another example: She implemented a quality measure on breast cancer screening. Just by having a flag in the EHR, she went from screening 50% of patients to almost 100%. "Having the data at your fingertips makes you aware of where you do a good job and where you don’t," Dr. Brull said.
In April, Dr. Brull collected the full Medicare incentive payment for 2011. Her colleagues weren’t ready, but that didn’t matter. Physicians can choose to attest to meaningful use on their own time frame, regardless of where their colleagues might be, she said.
Dr. Brull has become an evangelist for the power of the EHR and meaningful use. She was chosen to speak at a CMS press conference announcing the first round of Medicare incentive payments. And she is a member of the regional extension center in Kansas. The ONC also named her a "MUVer" – someone who serves as a local leader and adviser.
The Reluctant Adopter
Dr. Michael Machen is one of the physicians who consulted with Dr. Brull. He practices with four other family physicians in nearby Quinter, Kan. (population, 980). The impetus for taking on an EHR came from his younger partners, Dr. Machen said in an interview. They were also motivated by the meaningful use program, and got started in July 2010.
One junior partner became the EHR champion, doing much of the legwork to find appropriate vendors and systems. The physicians also attended seminars and webinars offered by the Kansas Medical Society and the Kansas chapter of the AAFP. A team from the regional extension center visited their practice too, Dr. Machen said.
They borrowed $75,000 to purchase hardware and software. The biggest cost is the $2,000-$4,000 they spend monthly on IT support – a necessity when there is no one with such expertise in the practice or locally. The IT help comes from more than an hour away. Dr. Machen and his colleagues house the server themselves; broadband is no better in Quinter than it is in Plainview.
Dr. Machen said that the younger physicians have all done well with the system, but he is struggling.
"I’m not technically inclined, and I have very little computer knowledge," he said.
It has also been difficult for his nurse, who is spending more time on data entry and less on interacting with patients, Dr. Machen said, adding that they are both in their late 50s and are more frustrated with the system than are their younger colleagues.
His staff has been happy; there’s no more searching for charts, and coding is easier, he said. And he does see the potential for improving quality, especially with the data-collection effort, warnings about drug interactions, and prompts for screening tests.
But for the time being, "it’s horrible with the workflow and the patient flow." On days of 15-20 patient visits, using the EHR is not as much of an issue. But on days of 30 patient visits, "it’s not doable," he said.
So far, patients haven’t been wild about the transition, either. They don’t like the physician to be working on a computer during the visit, he said. And "I don’t like it much, either," said Dr. Machen. "When I was in medical school, I was taught that the second you enter the exam room, the patient has your undivided attention." That’s not really possible with an EHR, at least the way he sees it currently, although he also can see possible solutions, such as having a scribe.
Dr. Machen also said he has concerns about whether it’s possible to truly secure an EHR, and, whether the systems will truly improve patient outcomes. The jury is still out on that, he said.
But, he added, "I don’t want to be a naysayer." He said that he’s "on the upward slope of the learning curve," and expects to get more comfortable eventually.
In September, he’ll begin his 90-day period of meaningful use, with the aim of receiving an incentive payment by the end of the year.
Medicare and Medicaid Incentives
The ONC provides the central leadership for the Medicare and Medicaid EHR incentive programs. The HITECH (Health Information Technology for Economic and Clinical Health) Act directly appropriated $2 billion to the ONC to spend on incentives and administration of the program. The federal regulation governing the incentive program (some 800 pages) was issued in July 2010.
This year – 2011 – is the first year in which physicians can participate; they have until Oct. 1 to attest that they are meaningful users. To be eligible for incentive payments, physicians have to meet the meaningful use criteria for 90 consecutive days.
The criteria are being introduced in stages over the next 4-5 years. Stage 1 outlines what is expected in 2011 and 2012. Stage 2 was expected to be put into place in 2013, but in June, the Health IT Policy Committee of the Centers for Medicare and Medicaid Services voted to delay implementation until 2014, but only for physicians who were already participating. Physicians who wait until 2012 or later would still be expected to meet stage 2 criteria in 2013.
Physicians who want to participate have to choose between the Medicare or Medicaid incentive program. Those who take part in the Medicare program are eligible to receive incentive payments of $44,000 over 5 years. However, the payments will be made only through 2016. Physicians who wait until 2012 to start would still earn the $44,000 maximum; those who start later would receive prorated payments.
Physicians who practice in designated Health Professional Shortage Areas (HPSA) may be eligible for an additional 10% in each year’s incentive payment.
Importantly, Medicare begins to penalize nonparticipating physicians starting in 2016.
The Medicaid incentives are more generous: A total of $63,750 can be paid out over 6 years. And there’s a longer time frame. Eligible professionals can wait until 2016 to start participating and still receive the maximum payout over a 6-year period.
In late May, the CMS announced that $75 million in Medicare incentives had been awarded to physicians and hospitals in the first 2 weeks of the program. Some states began paying out Medicaid incentives in January. By late May, $83 million had been issued.
Meaningful use of EHRs is critical, according to Dr. Farzad Mostashari, the National Coordinator, who testified to the House Small Business Committee’s Subcommittee on Healthcare and Technology in June.
"If all we do is put an EHR in every provider’s office or hospital, we will have failed to realize health IT’s full potential," he said. "Instead, doctors, hospitals, and other providers need to use robust EHR technology in a meaningful and interoperable way to improve care."
Many physicians continue to be frustrated and confused by the meaningful use criteria that spell out how they can receive incentive payments from Medicare and Medicaid for their use of electronic health records.
With that uncertainty, physicians are not jumping in with both feet to participate in the incentive program, even if they have purchased EHR systems. The Medical Group Management Association (MGMA) surveyed its members in April and found that 80% of those who already had adopted an EHR system said that they intended to participate. But at that time, only about 14% said that they were able to meet all of the criteria.
The American Medical Association held a special session on meaningful use at its House of Delegates meeting in June. When the speaker – Dr. Michael L. Hodgkins, an AMA chief medical information officer – asked how many physicians were confused about what was expected of them, more than half raised their hands.
Physicians in smaller practices are especially challenged, Dr. Hodgkins said, citing data that some 300,000 doctors are in practices of 10 or fewer physicians. Among those, fewer than 15% have implemented an EHR system, and most are not yet capable of meeting the meaningful use criteria.
According to Dr. Hodgkins, there are many obstacles to meeting meaningful use, including selecting from the more than 400 EHR products certified by the federal Office of the National Coordinator (ONC) for Health Information Technology, part of the Health and Human Services department.
Another problem: "Aggressive" timelines set by the government, according to Dr. Steve Waldren, director of the Center for Health Information Technology at the American Academy of Family Physicians (AAFP).
Dr. Waldren says it takes generally 6-18 months from purchase to active meaningful use of a system.
It’s been a tough road, he said. Physicians who don’t have EHRs or who have just gotten on board are struggling to get them operational and to achieve meaningful use. Those who have owned systems for awhile may face upgrades in order to meet the meaningful use criteria.
Meanwhile, there’s the system’s financial cost, training, and maintenance issues, and workflow changes once a system is in place.
The Long-Time User
Some physicians aren’t in a panic about the impending deadlines. Dr. Michael Mirro of Ft. Wayne (Ind.) Cardiology, a 24-physician group, said that his practice has been using health IT since 1996.
"We knew that we had to ultimately modernize our practice," Dr. Mirro said in an interview. Their current system has improved efficiency and quality, and has "supported a higher level of coding and reimbursement."
The system has "pretty much complete functionality," said Dr. Mirro. It provides the EHR, offers e-prescribing and decision-support tools, and can be used for direct quality reporting to the American College of Cardiology’s PINNACLE registry.
The system is web based, which reduces maintenance costs and IT headaches. The practice does not own the servers; it merely has local computers that interact with the vendor’s servers and software. The system is certified by the Certification Commission for Health Information Technology and was updated to ensure that the practice would meet the meaningful use criteria. One helpful tool, according to Dr. Mirro: A meaningful use "meter" that tells the physicians how well they are meeting the goals.
Ft. Wayne Cardiology has already attested to the government that it was a meaningful user and has received the maximum $18,000 per physician incentive for 2011, Dr. Mirro said.
The annual cost is about $2,000 per physician per year. That’s low, said Dr. Mirro, because his practice is owned by a hospital. The system is already somewhat ahead of the curve, as it already incorporates a patient web portal (a stage 2 goal).
He said that he is sympathetic to physicians who are just getting started.
"Any time you adopt technology at the point of care, it’s going to require a change in workflow," he said. That was definitely the case at Ft. Wayne Cardiology. For example, because some of the practice’s physicians still don’t know how to type, the system has templates that require point-and-click data entry to avoid errors.
Dr. Mirro said that physicians who are looking to buy or expand their health IT should talk with one of the 60 regional extension centers established by the ONC. These centers have been charged to help rural physicians and primary care physicians especially, and they offer vendor recommendations, practice audits, and other advice for free.
Dr. Mirro said that he believes most cardiologists will be forced to purchase an EHR sooner rather than later. With the decline in reimbursement (particularly for imaging services), cardiologists are increasingly being employed by hospitals. Those institutions – which themselves are facing a huge penalty if they don’t comply with meaningful use by 2017 – will want to have a lot of connectivity with the physician practice.
A Model For Her Peers
In 2005, Dr. Jennifer Brull figured that she needed to get on board with health IT, even though it might be expensive and difficult for a family physician in a rural Kansas solo practice. A younger physician with whom she was collaborating suggested that having an EHR was the wave of the future, and would likely be a necessity going forward. She also had a practice-sharing arrangement with another physician, who was older. He wasn’t as sure, said Dr. Brull in an interview.
But they moved ahead and spent 3 years selecting, buying, and implementing an EHR system that they could all use, said Dr. Brull, who practices in Plainview. She took out a loan for $50,000 to buy the equipment; her colleagues contributed to the software and other costs.
Because they practice in a rural area, there was no possibility of using a web-based model; broadband access in her area is still not robust enough, said Dr. Brull. So she has a server onsite at her office, and recently purchased a second server for $3,000. The net cost so far has been about $30,000 per physician, Dr. Brull said.
The first 6 months were a challenge, she said. "Anytime you do something that’s a complete paradigm shift, it’s hard. It’s hard mentally to think about all those changes, hard physically because you’re investing more time and effort, and hard emotionally because your staff gets freaked out."
In addition to allowing the practice to meet meaningful use criteria, the system also has a patient portal. The physicians are preparing to be able to participate in the state’s health information exchange.
Dr. Brull said that she disagrees with physicians who say that adopting an EHR interrupts the workflow or comes between the physician and patient.
"I’ve found it easier to be more collaborative [with my patients]," she said. One example: She recently used an EHR-generated graph to show a patient that she had gained 40 pounds over 3 years. The graph made much more of an impression on the patient than Dr. Brull could have done by reading numbers off a paper chart, she said.
"This whole project has resulted in dramatic quality improvement for my practice," Dr. Brull added.
Another example: She implemented a quality measure on breast cancer screening. Just by having a flag in the EHR, she went from screening 50% of patients to almost 100%. "Having the data at your fingertips makes you aware of where you do a good job and where you don’t," Dr. Brull said.
In April, Dr. Brull collected the full Medicare incentive payment for 2011. Her colleagues weren’t ready, but that didn’t matter. Physicians can choose to attest to meaningful use on their own time frame, regardless of where their colleagues might be, she said.
Dr. Brull has become an evangelist for the power of the EHR and meaningful use. She was chosen to speak at a CMS press conference announcing the first round of Medicare incentive payments. And she is a member of the regional extension center in Kansas. The ONC also named her a "MUVer" – someone who serves as a local leader and adviser.
The Reluctant Adopter
Dr. Michael Machen is one of the physicians who consulted with Dr. Brull. He practices with four other family physicians in nearby Quinter, Kan. (population, 980). The impetus for taking on an EHR came from his younger partners, Dr. Machen said in an interview. They were also motivated by the meaningful use program, and got started in July 2010.
One junior partner became the EHR champion, doing much of the legwork to find appropriate vendors and systems. The physicians also attended seminars and webinars offered by the Kansas Medical Society and the Kansas chapter of the AAFP. A team from the regional extension center visited their practice too, Dr. Machen said.
They borrowed $75,000 to purchase hardware and software. The biggest cost is the $2,000-$4,000 they spend monthly on IT support – a necessity when there is no one with such expertise in the practice or locally. The IT help comes from more than an hour away. Dr. Machen and his colleagues house the server themselves; broadband is no better in Quinter than it is in Plainview.
Dr. Machen said that the younger physicians have all done well with the system, but he is struggling.
"I’m not technically inclined, and I have very little computer knowledge," he said.
It has also been difficult for his nurse, who is spending more time on data entry and less on interacting with patients, Dr. Machen said, adding that they are both in their late 50s and are more frustrated with the system than are their younger colleagues.
His staff has been happy; there’s no more searching for charts, and coding is easier, he said. And he does see the potential for improving quality, especially with the data-collection effort, warnings about drug interactions, and prompts for screening tests.
But for the time being, "it’s horrible with the workflow and the patient flow." On days of 15-20 patient visits, using the EHR is not as much of an issue. But on days of 30 patient visits, "it’s not doable," he said.
So far, patients haven’t been wild about the transition, either. They don’t like the physician to be working on a computer during the visit, he said. And "I don’t like it much, either," said Dr. Machen. "When I was in medical school, I was taught that the second you enter the exam room, the patient has your undivided attention." That’s not really possible with an EHR, at least the way he sees it currently, although he also can see possible solutions, such as having a scribe.
Dr. Machen also said he has concerns about whether it’s possible to truly secure an EHR, and, whether the systems will truly improve patient outcomes. The jury is still out on that, he said.
But, he added, "I don’t want to be a naysayer." He said that he’s "on the upward slope of the learning curve," and expects to get more comfortable eventually.
In September, he’ll begin his 90-day period of meaningful use, with the aim of receiving an incentive payment by the end of the year.
Medicare and Medicaid Incentives
The ONC provides the central leadership for the Medicare and Medicaid EHR incentive programs. The HITECH (Health Information Technology for Economic and Clinical Health) Act directly appropriated $2 billion to the ONC to spend on incentives and administration of the program. The federal regulation governing the incentive program (some 800 pages) was issued in July 2010.
This year – 2011 – is the first year in which physicians can participate; they have until Oct. 1 to attest that they are meaningful users. To be eligible for incentive payments, physicians have to meet the meaningful use criteria for 90 consecutive days.
The criteria are being introduced in stages over the next 4-5 years. Stage 1 outlines what is expected in 2011 and 2012. Stage 2 was expected to be put into place in 2013, but in June, the Health IT Policy Committee of the Centers for Medicare and Medicaid Services voted to delay implementation until 2014, but only for physicians who were already participating. Physicians who wait until 2012 or later would still be expected to meet stage 2 criteria in 2013.
Physicians who want to participate have to choose between the Medicare or Medicaid incentive program. Those who take part in the Medicare program are eligible to receive incentive payments of $44,000 over 5 years. However, the payments will be made only through 2016. Physicians who wait until 2012 to start would still earn the $44,000 maximum; those who start later would receive prorated payments.
Physicians who practice in designated Health Professional Shortage Areas (HPSA) may be eligible for an additional 10% in each year’s incentive payment.
Importantly, Medicare begins to penalize nonparticipating physicians starting in 2016.
The Medicaid incentives are more generous: A total of $63,750 can be paid out over 6 years. And there’s a longer time frame. Eligible professionals can wait until 2016 to start participating and still receive the maximum payout over a 6-year period.
In late May, the CMS announced that $75 million in Medicare incentives had been awarded to physicians and hospitals in the first 2 weeks of the program. Some states began paying out Medicaid incentives in January. By late May, $83 million had been issued.
Meaningful use of EHRs is critical, according to Dr. Farzad Mostashari, the National Coordinator, who testified to the House Small Business Committee’s Subcommittee on Healthcare and Technology in June.
"If all we do is put an EHR in every provider’s office or hospital, we will have failed to realize health IT’s full potential," he said. "Instead, doctors, hospitals, and other providers need to use robust EHR technology in a meaningful and interoperable way to improve care."