User login
CHICAGO – Emergency department visits are projected to increase annually by more than 2 million visits with expansion of Medicaid eligibility under the Affordable Care Act, Christina M. Cutter reported at the annual meeting of the American College of Emergency Physicians.
Similarly, primary care–treatable ED visits – visits that require immediate care but could be treated in an outpatient setting – are projected to increase by nearly 1 million visits nationally among new adult Medicaid beneficiaries.
The projections, based on results from the Oregon Health Insurance Experiment (OHIE), amplify concerns that the nation’s already strained ED system will be further challenged by Medicaid expansion under the ACA, said Ms. Cutter, a medical student at the University of Colorado, Aurora.
To estimate ED utilization by Medicaid beneficiaries following the expansion of Medicaid eligibility under the Affordable Care Act, Ms. Cutter and her colleague Dr. Arjun K. Venkatesh, of Yale University in New Haven, Conn., conducted a cross-sectional analysis of population-level data derived from the American Community Survey, National Hospital Ambulatory Medical Care Survey, and Kaiser Family Foundation.

Initially, they approximated baseline ED visits at the state-level by adults aged 18-64 years with Medicaid. To estimate state and national changes in ED visitation and state-level increases in primary care–treatable conditions, the researchers assumed that all states expanding Medicaid would have increases in ED visits that were proportionate to those observed in the OHIE.
Primary care–treatable ED visits were defined using the N.Y.U. Billings Algorithm. State-level data on measures of emergency care access were obtained from the Centers for Medicare & Medicaid Services Hospital Compare file, AMA Physician Professional file, Health Resources and Sservices Administration Geospatial Data Warehouse, and the American College of Emergency Physicians Emergency Care Environment Report Card. States expanding Medicaid coverage were compared with those not expanding Medicaid.
Based on these measures, the researchers estimated a total of 80,819,573 ED visits in 2012 for the U.S. adult population, of which 25,054,068 were adults with Medicaid. They estimated 8,749,000 additional adult enrollees in the 28 states expanding Medicaid eligibility.
Based on projections using the OHIE, ED visits will increase by 2,143,260 visits in states expanding eligibility and primary care–treatable ED visits will increase by 943,034 nationally among new adult Medicaid beneficiaries, according to the researchers.
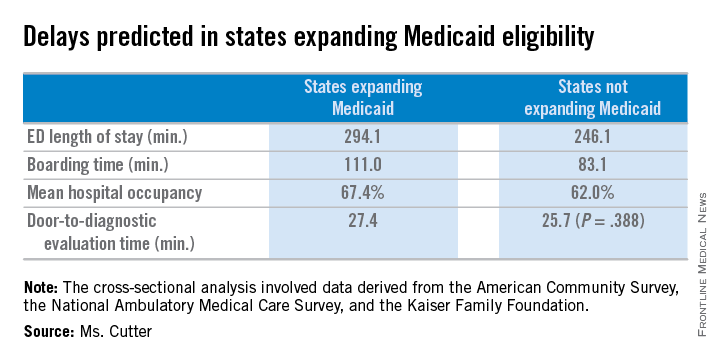
States expanding Medicaid eligibility have longer ED length of stay (294.1 vs. 246.1 minutes, P = .007), longer boarding time (111.0 vs. 83.1 minutes, P = .007), and higher mean hospital occupancy (67.4 vs. 62.0 per 100 staffed beds, P = .012), but no difference in door-to-diagnostic evaluation time (27.4 vs. 25.7 minutes, P = .388).
States expanding eligibility also have fewer EDs (14.8 vs. 24.0/1,000,000 population, P = .004), but are less likely to have shortages of mental health provider shortages (0.6 vs. 1.0 needed full-time equivalents, P = .021) and have no difference in psychiatric beds (24.4 vs. 28.2/100,000 population, P = .557). States expanding Medicaid also have a greater supply of emergency physicians (15 vs. 11.7/100,000 population, P = .004), Ms. Cutter reported.
CHICAGO – Emergency department visits are projected to increase annually by more than 2 million visits with expansion of Medicaid eligibility under the Affordable Care Act, Christina M. Cutter reported at the annual meeting of the American College of Emergency Physicians.
Similarly, primary care–treatable ED visits – visits that require immediate care but could be treated in an outpatient setting – are projected to increase by nearly 1 million visits nationally among new adult Medicaid beneficiaries.
The projections, based on results from the Oregon Health Insurance Experiment (OHIE), amplify concerns that the nation’s already strained ED system will be further challenged by Medicaid expansion under the ACA, said Ms. Cutter, a medical student at the University of Colorado, Aurora.
To estimate ED utilization by Medicaid beneficiaries following the expansion of Medicaid eligibility under the Affordable Care Act, Ms. Cutter and her colleague Dr. Arjun K. Venkatesh, of Yale University in New Haven, Conn., conducted a cross-sectional analysis of population-level data derived from the American Community Survey, National Hospital Ambulatory Medical Care Survey, and Kaiser Family Foundation.

Initially, they approximated baseline ED visits at the state-level by adults aged 18-64 years with Medicaid. To estimate state and national changes in ED visitation and state-level increases in primary care–treatable conditions, the researchers assumed that all states expanding Medicaid would have increases in ED visits that were proportionate to those observed in the OHIE.
Primary care–treatable ED visits were defined using the N.Y.U. Billings Algorithm. State-level data on measures of emergency care access were obtained from the Centers for Medicare & Medicaid Services Hospital Compare file, AMA Physician Professional file, Health Resources and Sservices Administration Geospatial Data Warehouse, and the American College of Emergency Physicians Emergency Care Environment Report Card. States expanding Medicaid coverage were compared with those not expanding Medicaid.
Based on these measures, the researchers estimated a total of 80,819,573 ED visits in 2012 for the U.S. adult population, of which 25,054,068 were adults with Medicaid. They estimated 8,749,000 additional adult enrollees in the 28 states expanding Medicaid eligibility.
Based on projections using the OHIE, ED visits will increase by 2,143,260 visits in states expanding eligibility and primary care–treatable ED visits will increase by 943,034 nationally among new adult Medicaid beneficiaries, according to the researchers.
States expanding Medicaid eligibility have longer ED length of stay (294.1 vs. 246.1 minutes, P = .007), longer boarding time (111.0 vs. 83.1 minutes, P = .007), and higher mean hospital occupancy (67.4 vs. 62.0 per 100 staffed beds, P = .012), but no difference in door-to-diagnostic evaluation time (27.4 vs. 25.7 minutes, P = .388).
States expanding eligibility also have fewer EDs (14.8 vs. 24.0/1,000,000 population, P = .004), but are less likely to have shortages of mental health provider shortages (0.6 vs. 1.0 needed full-time equivalents, P = .021) and have no difference in psychiatric beds (24.4 vs. 28.2/100,000 population, P = .557). States expanding Medicaid also have a greater supply of emergency physicians (15 vs. 11.7/100,000 population, P = .004), Ms. Cutter reported.
CHICAGO – Emergency department visits are projected to increase annually by more than 2 million visits with expansion of Medicaid eligibility under the Affordable Care Act, Christina M. Cutter reported at the annual meeting of the American College of Emergency Physicians.
Similarly, primary care–treatable ED visits – visits that require immediate care but could be treated in an outpatient setting – are projected to increase by nearly 1 million visits nationally among new adult Medicaid beneficiaries.
The projections, based on results from the Oregon Health Insurance Experiment (OHIE), amplify concerns that the nation’s already strained ED system will be further challenged by Medicaid expansion under the ACA, said Ms. Cutter, a medical student at the University of Colorado, Aurora.
To estimate ED utilization by Medicaid beneficiaries following the expansion of Medicaid eligibility under the Affordable Care Act, Ms. Cutter and her colleague Dr. Arjun K. Venkatesh, of Yale University in New Haven, Conn., conducted a cross-sectional analysis of population-level data derived from the American Community Survey, National Hospital Ambulatory Medical Care Survey, and Kaiser Family Foundation.

Initially, they approximated baseline ED visits at the state-level by adults aged 18-64 years with Medicaid. To estimate state and national changes in ED visitation and state-level increases in primary care–treatable conditions, the researchers assumed that all states expanding Medicaid would have increases in ED visits that were proportionate to those observed in the OHIE.
Primary care–treatable ED visits were defined using the N.Y.U. Billings Algorithm. State-level data on measures of emergency care access were obtained from the Centers for Medicare & Medicaid Services Hospital Compare file, AMA Physician Professional file, Health Resources and Sservices Administration Geospatial Data Warehouse, and the American College of Emergency Physicians Emergency Care Environment Report Card. States expanding Medicaid coverage were compared with those not expanding Medicaid.
Based on these measures, the researchers estimated a total of 80,819,573 ED visits in 2012 for the U.S. adult population, of which 25,054,068 were adults with Medicaid. They estimated 8,749,000 additional adult enrollees in the 28 states expanding Medicaid eligibility.
Based on projections using the OHIE, ED visits will increase by 2,143,260 visits in states expanding eligibility and primary care–treatable ED visits will increase by 943,034 nationally among new adult Medicaid beneficiaries, according to the researchers.
States expanding Medicaid eligibility have longer ED length of stay (294.1 vs. 246.1 minutes, P = .007), longer boarding time (111.0 vs. 83.1 minutes, P = .007), and higher mean hospital occupancy (67.4 vs. 62.0 per 100 staffed beds, P = .012), but no difference in door-to-diagnostic evaluation time (27.4 vs. 25.7 minutes, P = .388).
States expanding eligibility also have fewer EDs (14.8 vs. 24.0/1,000,000 population, P = .004), but are less likely to have shortages of mental health provider shortages (0.6 vs. 1.0 needed full-time equivalents, P = .021) and have no difference in psychiatric beds (24.4 vs. 28.2/100,000 population, P = .557). States expanding Medicaid also have a greater supply of emergency physicians (15 vs. 11.7/100,000 population, P = .004), Ms. Cutter reported.
AT ACEP 2014
Key clinical point: ED lengths of stay are predicted to become longer as more states expand Medicaid coverage.
Major finding: States expanding Medicaid eligibility have longer mean ED lengths of stay (294.1 vs. 246.1 minutes, P = .007), longer mean boarding time (111.0 vs. 83.1 minutes, P = .007), and higher mean hospital occupancy (67.4 vs. 62.0 per 100 staffed beds, P = .012).
Data source: Historical data from the Oregon Health Insurance Experiment.
Disclosures: Ms. Cutter had no relevant financial disclosures.