User login
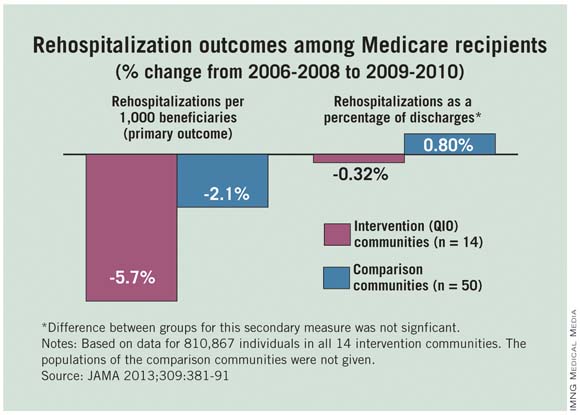
Hospitalizations and 30-day readmissions fell for Medicare patients in 14 communities when providers there worked with local quality improvement organizations to smooth and coordinate transitions between care settings, researchers from the Colorado Foundation for Medical Care and the Centers for Medicare and Medicaid Services reported Jan. 23 in JAMA.
Atlanta, Miami, Pittsburgh, and the other communities that participated in the 2-year CMS project saw mean reductions of 5.74% in hospitalizations and 5.70% in 30-day readmissions per 1,000 Medicare fee-for-service patients during 2009-2010. Fifty control communities saw smaller reductions: 3.17% in hospitalizations and 2.05% in readmissions (JAMA 2013;309:381-91).
"Our results provide evidence of a ... significant association between care transitions improvement interventions initiated by 14 [quality improvement organizations] and reductions in rehospitalizations and hospitalizations" as well as "evidence of a background national decline in hospitalizations and rehospitalizations for Medicare beneficiaries since 2008," the researchers said.
Each state typically has one nonprofit quality improvement organization (QIO) that contracts with CMS to improve beneficiary care.
The goal of the project was to "implement evidence-based improvements in care transitions by community organizing, technical assistance, and monitoring of participation, implementation, effectiveness, and adverse effects," according to the investigators.
But CMS left it up to each community to decide how best to do that. QIOs guided the efforts, working with hospitals, nursing facilities, home care agencies, hospices, social service agencies, clinicians, and others to improve a range of areas, including discharge standardization, medication reconciliation, chronic disease care planning, palliative care counseling, elder care services, and patient self-management.
Each community used three or more evidence-based approaches such as Interventions to Reduce Acute Care Transfers, Re-Engineered Discharges, Transitional Care Nursing, the Care Transitions Program, and the Best Practices Intervention Packages on transitional care.
With such a variety of approaches, the project "can only begin to guide predictions about effective combinations of context and interventions, optimal replication strategies, and effective plans for sustainability. Local community context was clearly relevant," the investigators said.
QIOs bid to be part of the efforts, and were selected by CMS based on application quality and their community’s contribution to geographic, market, and utilization diversity. The agency spent on average about $12 million annually to support their efforts. Medicare fee-for-service populations were quite varied among the 14 communities, ranging from about 22,000 to 90,000.
The investigators disclosed lecture fees, honoraria, or travel expenses from several sources, including the Alliance for Home Health Quality and Innovation, Lilly, and Insignia Health.
"Attempts to optimize care transitions will need to recognize that there is no single solution to address all the issues contributing to patient rehospitalization," wrote Dr. Mark V. Williams in an editorial (JAMA 2013;309:394-6).
"Efforts moving forward should involve implementation of broad patient-centered approaches that engage all members of a care team, especially front-line clinicians, and use proven quality improvement methods ... to identify helpful interventions. As achieved by the quality improvement organization initiative, engaging the community in caring for a patient can facilitate enhanced connections with better care coordination, and may help deliver higher-quality care more cost efficiently – optimizing value," he said.
Dr. Williams is chief of the division of medicine–hospital medicine at the Northwestern University, Chicago.He reported no relevant conflicts of interest.
"Attempts to optimize care transitions will need to recognize that there is no single solution to address all the issues contributing to patient rehospitalization," wrote Dr. Mark V. Williams in an editorial (JAMA 2013;309:394-6).
"Efforts moving forward should involve implementation of broad patient-centered approaches that engage all members of a care team, especially front-line clinicians, and use proven quality improvement methods ... to identify helpful interventions. As achieved by the quality improvement organization initiative, engaging the community in caring for a patient can facilitate enhanced connections with better care coordination, and may help deliver higher-quality care more cost efficiently – optimizing value," he said.
Dr. Williams is chief of the division of medicine–hospital medicine at the Northwestern University, Chicago.He reported no relevant conflicts of interest.
"Attempts to optimize care transitions will need to recognize that there is no single solution to address all the issues contributing to patient rehospitalization," wrote Dr. Mark V. Williams in an editorial (JAMA 2013;309:394-6).
"Efforts moving forward should involve implementation of broad patient-centered approaches that engage all members of a care team, especially front-line clinicians, and use proven quality improvement methods ... to identify helpful interventions. As achieved by the quality improvement organization initiative, engaging the community in caring for a patient can facilitate enhanced connections with better care coordination, and may help deliver higher-quality care more cost efficiently – optimizing value," he said.
Dr. Williams is chief of the division of medicine–hospital medicine at the Northwestern University, Chicago.He reported no relevant conflicts of interest.
Hospitalizations and 30-day readmissions fell for Medicare patients in 14 communities when providers there worked with local quality improvement organizations to smooth and coordinate transitions between care settings, researchers from the Colorado Foundation for Medical Care and the Centers for Medicare and Medicaid Services reported Jan. 23 in JAMA.
Atlanta, Miami, Pittsburgh, and the other communities that participated in the 2-year CMS project saw mean reductions of 5.74% in hospitalizations and 5.70% in 30-day readmissions per 1,000 Medicare fee-for-service patients during 2009-2010. Fifty control communities saw smaller reductions: 3.17% in hospitalizations and 2.05% in readmissions (JAMA 2013;309:381-91).
"Our results provide evidence of a ... significant association between care transitions improvement interventions initiated by 14 [quality improvement organizations] and reductions in rehospitalizations and hospitalizations" as well as "evidence of a background national decline in hospitalizations and rehospitalizations for Medicare beneficiaries since 2008," the researchers said.
Each state typically has one nonprofit quality improvement organization (QIO) that contracts with CMS to improve beneficiary care.
The goal of the project was to "implement evidence-based improvements in care transitions by community organizing, technical assistance, and monitoring of participation, implementation, effectiveness, and adverse effects," according to the investigators.
But CMS left it up to each community to decide how best to do that. QIOs guided the efforts, working with hospitals, nursing facilities, home care agencies, hospices, social service agencies, clinicians, and others to improve a range of areas, including discharge standardization, medication reconciliation, chronic disease care planning, palliative care counseling, elder care services, and patient self-management.
Each community used three or more evidence-based approaches such as Interventions to Reduce Acute Care Transfers, Re-Engineered Discharges, Transitional Care Nursing, the Care Transitions Program, and the Best Practices Intervention Packages on transitional care.
With such a variety of approaches, the project "can only begin to guide predictions about effective combinations of context and interventions, optimal replication strategies, and effective plans for sustainability. Local community context was clearly relevant," the investigators said.
QIOs bid to be part of the efforts, and were selected by CMS based on application quality and their community’s contribution to geographic, market, and utilization diversity. The agency spent on average about $12 million annually to support their efforts. Medicare fee-for-service populations were quite varied among the 14 communities, ranging from about 22,000 to 90,000.
The investigators disclosed lecture fees, honoraria, or travel expenses from several sources, including the Alliance for Home Health Quality and Innovation, Lilly, and Insignia Health.
Hospitalizations and 30-day readmissions fell for Medicare patients in 14 communities when providers there worked with local quality improvement organizations to smooth and coordinate transitions between care settings, researchers from the Colorado Foundation for Medical Care and the Centers for Medicare and Medicaid Services reported Jan. 23 in JAMA.
Atlanta, Miami, Pittsburgh, and the other communities that participated in the 2-year CMS project saw mean reductions of 5.74% in hospitalizations and 5.70% in 30-day readmissions per 1,000 Medicare fee-for-service patients during 2009-2010. Fifty control communities saw smaller reductions: 3.17% in hospitalizations and 2.05% in readmissions (JAMA 2013;309:381-91).
"Our results provide evidence of a ... significant association between care transitions improvement interventions initiated by 14 [quality improvement organizations] and reductions in rehospitalizations and hospitalizations" as well as "evidence of a background national decline in hospitalizations and rehospitalizations for Medicare beneficiaries since 2008," the researchers said.
Each state typically has one nonprofit quality improvement organization (QIO) that contracts with CMS to improve beneficiary care.
The goal of the project was to "implement evidence-based improvements in care transitions by community organizing, technical assistance, and monitoring of participation, implementation, effectiveness, and adverse effects," according to the investigators.
But CMS left it up to each community to decide how best to do that. QIOs guided the efforts, working with hospitals, nursing facilities, home care agencies, hospices, social service agencies, clinicians, and others to improve a range of areas, including discharge standardization, medication reconciliation, chronic disease care planning, palliative care counseling, elder care services, and patient self-management.
Each community used three or more evidence-based approaches such as Interventions to Reduce Acute Care Transfers, Re-Engineered Discharges, Transitional Care Nursing, the Care Transitions Program, and the Best Practices Intervention Packages on transitional care.
With such a variety of approaches, the project "can only begin to guide predictions about effective combinations of context and interventions, optimal replication strategies, and effective plans for sustainability. Local community context was clearly relevant," the investigators said.
QIOs bid to be part of the efforts, and were selected by CMS based on application quality and their community’s contribution to geographic, market, and utilization diversity. The agency spent on average about $12 million annually to support their efforts. Medicare fee-for-service populations were quite varied among the 14 communities, ranging from about 22,000 to 90,000.
The investigators disclosed lecture fees, honoraria, or travel expenses from several sources, including the Alliance for Home Health Quality and Innovation, Lilly, and Insignia Health.
FROM JAMA
Major finding: Communities that worked with local QIOs to improve care transitions saw mean reductions of 5.74% in hospitalizations and 5.70% in 30-day readmissions per 1,000 Medicare fee-for-service patients during 2009-2010.
Data source: Two-year CMS quality improvement project in 14 communities
Disclosures: CMS funded the project. The investigators disclosed lecture fees, honoraria, or travel expenses from several sources, including the Alliance for Home Health Quality and Innovation, Lilly, and Insignia Health.