User login
Metacognitive training (MCT) is effective in reducing positive and negative symptoms of schizophrenia, new research suggests.
MCT for psychosis is a brief intervention that “combines psychoeducation, cognitive bias modification, and strategy teaching but does not directly target psychosis symptoms.”
Additionally, MCT led to improvement in self-esteem and functioning, and all benefits were maintained up to 1 year post intervention.
“Our study demonstrates the effectiveness and durability of a brief, nonconfrontational intervention in the reduction of serious and debilitating symptoms of schizophrenia,” study investigator Danielle Penney, a doctoral candidate at the University of Montreal, told this news organization.
“Our results were observed in several treatment contexts and suggest that MCT can be successfully delivered by a variety of mental health practitioners [and] provide solid evidence to consider MCT in international treatment guidelines for schizophrenia spectrum disorders,” Ms. Penney said.
The findings were published online in JAMA Psychiatry.
‘Novel contribution’
MCT is a brief intervention consisting of eight to 16 modules that can be delivered in a group setting or on an individual basis. Instead of directly targeting psychotic symptoms, it uses an “indirect approach by promoting awareness of cognitive biases,” the investigators note.
Such biases include maladaptive thinking styles common to psychosis, such as jumping to conclusions, belief inflexibility, and overconfidence in judgments.
It is hypothesized that these biases “contribute to the formation and maintenance of positive symptoms, particularly delusions,” the researchers write.
MCT “aims to plant doubt in delusional beliefs through raising awareness of cognitive biases and aims to raise service engagement by proposing work on this less-confrontational objective first, which is likely to facilitate the therapeutic alliance and more direct work on psychotic symptoms,” they add.
Previous studies of MCT for psychosis yielded inconsistent results. Of the eight previous meta-analyses that analyzed MCT for psychosis, “none investigated the long-term effects of the intervention on directly targeted treatment outcomes,” such as delusions and cognitive biases, Ms. Penney said.
She added that “to our knowledge, no meta-analysis has examined the effectiveness of important indirectly targeted outcomes,” including self-esteem and functioning.
“These important gaps in the literature,” along with a large increase in recently conducted MCT efficacy trials, “provided the motivation for the current study,” said Ms. Penney.
To investigate, the researchers searched 11 databases, beginning with data from 2007, which was when the first report of MCT was published. Studies included participants with schizophrenia spectrum and related psychotic disorders.
Outcomes for the current review and meta-analysis were organized according to a “proximal-distal framework.” Proximal outcomes were those directly targeted by MCT, while distal outcomes were those not directly targeted by MCT but that were associated with improvement in proximal outcomes, either directly or indirectly.
The investigators examined these outcomes quantitatively and qualitatively from preintervention to postintervention and follow-up, “which, to our knowledge, is a novel contribution,” they write.
The review included 43 studies, of which 30 (70%) were randomized controlled trials (RCTs), 11 (25%) were non-RCTs, and two (5%) were quantitative descriptive studies. Of these, 40 reports (n = 1,816 participants) were included in the meta-analysis, and six were included in the narrative review.
Transdiagnostic treatment?
Results showed a “small to moderate” effect size (ES) in global proximal outcomes (g = .39; 95% confidence interval, .25-.53; P < .001; 38 reports).
When proximal outcomes were analyzed separately, the largest ES was found for delusions; smaller ES values were found for hallucinations and cognitive biases.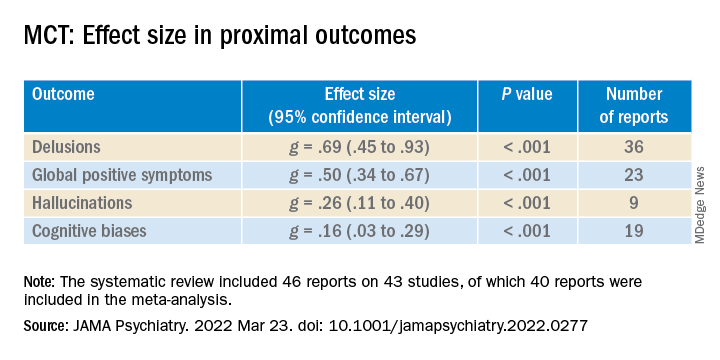
Newer studies reported higher ES values for hallucinations, compared with older studies (β = .04; 95% CI, .00-.07).
ES was small to moderate for distal outcomes (g = .31; 95% CI, .19-.44; P < .001; 26 reports). “Small but significant” ES values were shown for self-esteem and negative symptoms, small to moderate for functioning, and small but nonsignificant for quality of life (QOL).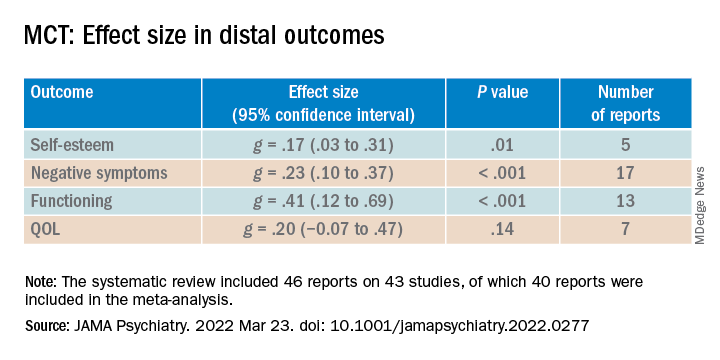
The researchers also analyzed RCTs by comparing differences between the treatment and control groups in scores from follow-up to post-treatment. Although the therapeutic gains made by the experimental group were “steadily maintained, the ES values were “small” and nonsignificant.
When the difference in scores between follow-up and baseline were compared in both groups, small to moderate ES values were found for proximal as well as distal outcomes.
“These results further indicate that net therapeutic gains remain significant even 1 year following MCT,” the investigators note.
Lower-quality studies showed significantly lower ES values for distal (between-group comparison, P = .05) but not proximal outcomes.
Overall, the findings suggest that MCT is a “beneficial and durable low-threshold intervention that can be flexibly delivered at minimal cost in a variety of contexts to individuals with psychotic disorders,” the researchers write.
They note that MCT has also been associated with positive outcomes in other patient populations, including patients with borderline personality disorder, depression, and obsessive-compulsive disorder. Future research “might consider investigating MCT as a transdiagnostic treatment,” they add.
Consistent beneficial effects
Commenting on the study, Philip Harvey, PhD, Leonard M. Miller Professor of Psychiatry and Behavioral Sciences and director of the Division of Psychology, University of Miami Miller School of Medicine, noted that self-awareness and self-assessment are critically important features in patients with serious mental illness.
Impairments in these areas “can actually have a greater impact on everyday functioning than cognitive deficits,” said Dr. Harvey, who is also the editor-in-chief of Schizophrenia Research: Cognition. He was not involved with the current meta-analysis.
He noted that the current results show that “MCT has consistent beneficial effects.”
“This is an intervention that should be considered for most people with serious mental illness, with a specific focus on those with specific types of delusions and more global challenges in self-assessment,” Dr. Harvey concluded.
Funding was provided by the Canada First Research Excellence Fund, awarded through the Healthy Brains, Healthy Lives initiative at McGill University. Ms. Penney reported no relevant financial relationships. Disclosures for the other investigators are listed in the original article. Dr. Harvey reported being a reviewer of the article but that he was not involved in its authorship.
A version of this article first appeared on Medscape.com.
Metacognitive training (MCT) is effective in reducing positive and negative symptoms of schizophrenia, new research suggests.
MCT for psychosis is a brief intervention that “combines psychoeducation, cognitive bias modification, and strategy teaching but does not directly target psychosis symptoms.”
Additionally, MCT led to improvement in self-esteem and functioning, and all benefits were maintained up to 1 year post intervention.
“Our study demonstrates the effectiveness and durability of a brief, nonconfrontational intervention in the reduction of serious and debilitating symptoms of schizophrenia,” study investigator Danielle Penney, a doctoral candidate at the University of Montreal, told this news organization.
“Our results were observed in several treatment contexts and suggest that MCT can be successfully delivered by a variety of mental health practitioners [and] provide solid evidence to consider MCT in international treatment guidelines for schizophrenia spectrum disorders,” Ms. Penney said.
The findings were published online in JAMA Psychiatry.
‘Novel contribution’
MCT is a brief intervention consisting of eight to 16 modules that can be delivered in a group setting or on an individual basis. Instead of directly targeting psychotic symptoms, it uses an “indirect approach by promoting awareness of cognitive biases,” the investigators note.
Such biases include maladaptive thinking styles common to psychosis, such as jumping to conclusions, belief inflexibility, and overconfidence in judgments.
It is hypothesized that these biases “contribute to the formation and maintenance of positive symptoms, particularly delusions,” the researchers write.
MCT “aims to plant doubt in delusional beliefs through raising awareness of cognitive biases and aims to raise service engagement by proposing work on this less-confrontational objective first, which is likely to facilitate the therapeutic alliance and more direct work on psychotic symptoms,” they add.
Previous studies of MCT for psychosis yielded inconsistent results. Of the eight previous meta-analyses that analyzed MCT for psychosis, “none investigated the long-term effects of the intervention on directly targeted treatment outcomes,” such as delusions and cognitive biases, Ms. Penney said.
She added that “to our knowledge, no meta-analysis has examined the effectiveness of important indirectly targeted outcomes,” including self-esteem and functioning.
“These important gaps in the literature,” along with a large increase in recently conducted MCT efficacy trials, “provided the motivation for the current study,” said Ms. Penney.
To investigate, the researchers searched 11 databases, beginning with data from 2007, which was when the first report of MCT was published. Studies included participants with schizophrenia spectrum and related psychotic disorders.
Outcomes for the current review and meta-analysis were organized according to a “proximal-distal framework.” Proximal outcomes were those directly targeted by MCT, while distal outcomes were those not directly targeted by MCT but that were associated with improvement in proximal outcomes, either directly or indirectly.
The investigators examined these outcomes quantitatively and qualitatively from preintervention to postintervention and follow-up, “which, to our knowledge, is a novel contribution,” they write.
The review included 43 studies, of which 30 (70%) were randomized controlled trials (RCTs), 11 (25%) were non-RCTs, and two (5%) were quantitative descriptive studies. Of these, 40 reports (n = 1,816 participants) were included in the meta-analysis, and six were included in the narrative review.
Transdiagnostic treatment?
Results showed a “small to moderate” effect size (ES) in global proximal outcomes (g = .39; 95% confidence interval, .25-.53; P < .001; 38 reports).
When proximal outcomes were analyzed separately, the largest ES was found for delusions; smaller ES values were found for hallucinations and cognitive biases.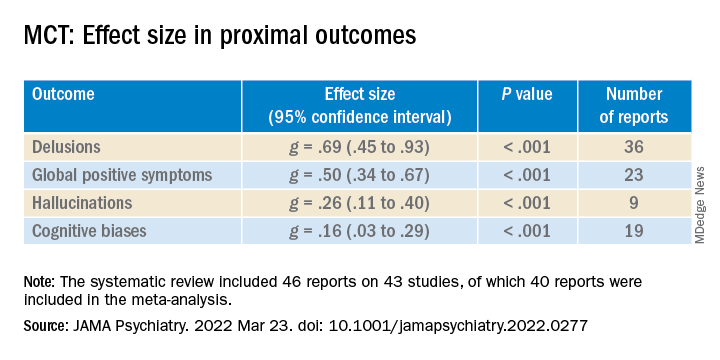
Newer studies reported higher ES values for hallucinations, compared with older studies (β = .04; 95% CI, .00-.07).
ES was small to moderate for distal outcomes (g = .31; 95% CI, .19-.44; P < .001; 26 reports). “Small but significant” ES values were shown for self-esteem and negative symptoms, small to moderate for functioning, and small but nonsignificant for quality of life (QOL).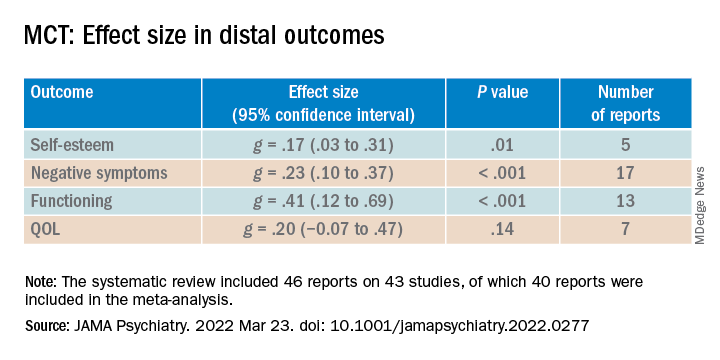
The researchers also analyzed RCTs by comparing differences between the treatment and control groups in scores from follow-up to post-treatment. Although the therapeutic gains made by the experimental group were “steadily maintained, the ES values were “small” and nonsignificant.
When the difference in scores between follow-up and baseline were compared in both groups, small to moderate ES values were found for proximal as well as distal outcomes.
“These results further indicate that net therapeutic gains remain significant even 1 year following MCT,” the investigators note.
Lower-quality studies showed significantly lower ES values for distal (between-group comparison, P = .05) but not proximal outcomes.
Overall, the findings suggest that MCT is a “beneficial and durable low-threshold intervention that can be flexibly delivered at minimal cost in a variety of contexts to individuals with psychotic disorders,” the researchers write.
They note that MCT has also been associated with positive outcomes in other patient populations, including patients with borderline personality disorder, depression, and obsessive-compulsive disorder. Future research “might consider investigating MCT as a transdiagnostic treatment,” they add.
Consistent beneficial effects
Commenting on the study, Philip Harvey, PhD, Leonard M. Miller Professor of Psychiatry and Behavioral Sciences and director of the Division of Psychology, University of Miami Miller School of Medicine, noted that self-awareness and self-assessment are critically important features in patients with serious mental illness.
Impairments in these areas “can actually have a greater impact on everyday functioning than cognitive deficits,” said Dr. Harvey, who is also the editor-in-chief of Schizophrenia Research: Cognition. He was not involved with the current meta-analysis.
He noted that the current results show that “MCT has consistent beneficial effects.”
“This is an intervention that should be considered for most people with serious mental illness, with a specific focus on those with specific types of delusions and more global challenges in self-assessment,” Dr. Harvey concluded.
Funding was provided by the Canada First Research Excellence Fund, awarded through the Healthy Brains, Healthy Lives initiative at McGill University. Ms. Penney reported no relevant financial relationships. Disclosures for the other investigators are listed in the original article. Dr. Harvey reported being a reviewer of the article but that he was not involved in its authorship.
A version of this article first appeared on Medscape.com.
Metacognitive training (MCT) is effective in reducing positive and negative symptoms of schizophrenia, new research suggests.
MCT for psychosis is a brief intervention that “combines psychoeducation, cognitive bias modification, and strategy teaching but does not directly target psychosis symptoms.”
Additionally, MCT led to improvement in self-esteem and functioning, and all benefits were maintained up to 1 year post intervention.
“Our study demonstrates the effectiveness and durability of a brief, nonconfrontational intervention in the reduction of serious and debilitating symptoms of schizophrenia,” study investigator Danielle Penney, a doctoral candidate at the University of Montreal, told this news organization.
“Our results were observed in several treatment contexts and suggest that MCT can be successfully delivered by a variety of mental health practitioners [and] provide solid evidence to consider MCT in international treatment guidelines for schizophrenia spectrum disorders,” Ms. Penney said.
The findings were published online in JAMA Psychiatry.
‘Novel contribution’
MCT is a brief intervention consisting of eight to 16 modules that can be delivered in a group setting or on an individual basis. Instead of directly targeting psychotic symptoms, it uses an “indirect approach by promoting awareness of cognitive biases,” the investigators note.
Such biases include maladaptive thinking styles common to psychosis, such as jumping to conclusions, belief inflexibility, and overconfidence in judgments.
It is hypothesized that these biases “contribute to the formation and maintenance of positive symptoms, particularly delusions,” the researchers write.
MCT “aims to plant doubt in delusional beliefs through raising awareness of cognitive biases and aims to raise service engagement by proposing work on this less-confrontational objective first, which is likely to facilitate the therapeutic alliance and more direct work on psychotic symptoms,” they add.
Previous studies of MCT for psychosis yielded inconsistent results. Of the eight previous meta-analyses that analyzed MCT for psychosis, “none investigated the long-term effects of the intervention on directly targeted treatment outcomes,” such as delusions and cognitive biases, Ms. Penney said.
She added that “to our knowledge, no meta-analysis has examined the effectiveness of important indirectly targeted outcomes,” including self-esteem and functioning.
“These important gaps in the literature,” along with a large increase in recently conducted MCT efficacy trials, “provided the motivation for the current study,” said Ms. Penney.
To investigate, the researchers searched 11 databases, beginning with data from 2007, which was when the first report of MCT was published. Studies included participants with schizophrenia spectrum and related psychotic disorders.
Outcomes for the current review and meta-analysis were organized according to a “proximal-distal framework.” Proximal outcomes were those directly targeted by MCT, while distal outcomes were those not directly targeted by MCT but that were associated with improvement in proximal outcomes, either directly or indirectly.
The investigators examined these outcomes quantitatively and qualitatively from preintervention to postintervention and follow-up, “which, to our knowledge, is a novel contribution,” they write.
The review included 43 studies, of which 30 (70%) were randomized controlled trials (RCTs), 11 (25%) were non-RCTs, and two (5%) were quantitative descriptive studies. Of these, 40 reports (n = 1,816 participants) were included in the meta-analysis, and six were included in the narrative review.
Transdiagnostic treatment?
Results showed a “small to moderate” effect size (ES) in global proximal outcomes (g = .39; 95% confidence interval, .25-.53; P < .001; 38 reports).
When proximal outcomes were analyzed separately, the largest ES was found for delusions; smaller ES values were found for hallucinations and cognitive biases.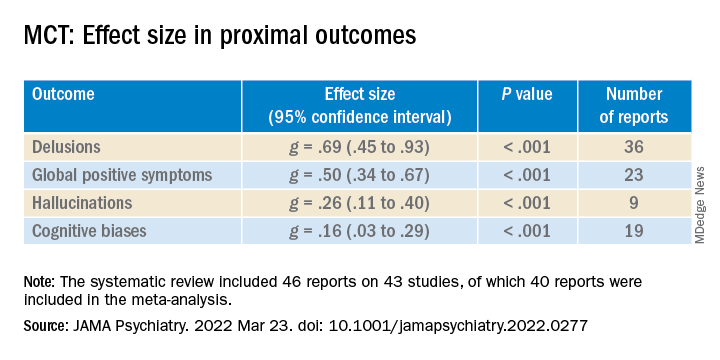
Newer studies reported higher ES values for hallucinations, compared with older studies (β = .04; 95% CI, .00-.07).
ES was small to moderate for distal outcomes (g = .31; 95% CI, .19-.44; P < .001; 26 reports). “Small but significant” ES values were shown for self-esteem and negative symptoms, small to moderate for functioning, and small but nonsignificant for quality of life (QOL).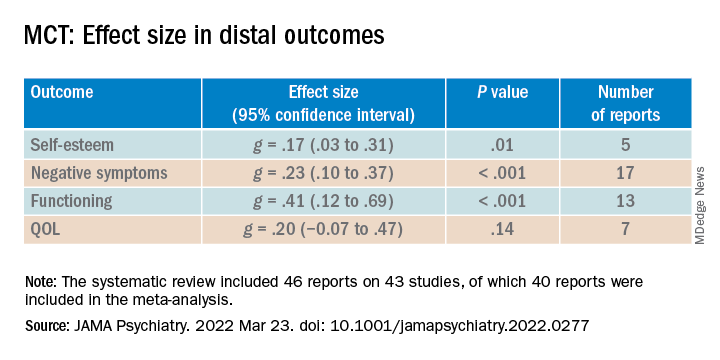
The researchers also analyzed RCTs by comparing differences between the treatment and control groups in scores from follow-up to post-treatment. Although the therapeutic gains made by the experimental group were “steadily maintained, the ES values were “small” and nonsignificant.
When the difference in scores between follow-up and baseline were compared in both groups, small to moderate ES values were found for proximal as well as distal outcomes.
“These results further indicate that net therapeutic gains remain significant even 1 year following MCT,” the investigators note.
Lower-quality studies showed significantly lower ES values for distal (between-group comparison, P = .05) but not proximal outcomes.
Overall, the findings suggest that MCT is a “beneficial and durable low-threshold intervention that can be flexibly delivered at minimal cost in a variety of contexts to individuals with psychotic disorders,” the researchers write.
They note that MCT has also been associated with positive outcomes in other patient populations, including patients with borderline personality disorder, depression, and obsessive-compulsive disorder. Future research “might consider investigating MCT as a transdiagnostic treatment,” they add.
Consistent beneficial effects
Commenting on the study, Philip Harvey, PhD, Leonard M. Miller Professor of Psychiatry and Behavioral Sciences and director of the Division of Psychology, University of Miami Miller School of Medicine, noted that self-awareness and self-assessment are critically important features in patients with serious mental illness.
Impairments in these areas “can actually have a greater impact on everyday functioning than cognitive deficits,” said Dr. Harvey, who is also the editor-in-chief of Schizophrenia Research: Cognition. He was not involved with the current meta-analysis.
He noted that the current results show that “MCT has consistent beneficial effects.”
“This is an intervention that should be considered for most people with serious mental illness, with a specific focus on those with specific types of delusions and more global challenges in self-assessment,” Dr. Harvey concluded.
Funding was provided by the Canada First Research Excellence Fund, awarded through the Healthy Brains, Healthy Lives initiative at McGill University. Ms. Penney reported no relevant financial relationships. Disclosures for the other investigators are listed in the original article. Dr. Harvey reported being a reviewer of the article but that he was not involved in its authorship.
A version of this article first appeared on Medscape.com.