User login
The ongoing mumps epidemic in the Midwestern US is a stark reminder of how fast and easily an epidemic can still occur. It serves as a warning that we need to remain vigilant in maintaining high immunization levels among our patients. The morbidity and mortality resulting from this outbreak will depend on the soundness and response of the public health infrastructure.
We family physicians need to be prepared to detect and prevent mumps among our patients and staff. While it may not be immediately apparent, if we fulfill our roles competently the outbreak will be less severe.
The start of an epidemic
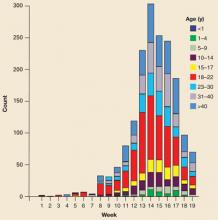
As of May 15, 1765 cases of mumps had been reported to the Iowa Department of Public Health.1 The median age of those infected was 22 years, with more than one third of cases occurring in those aged 16 to 22 years (FIGURE). College students accounted for 20% of cases.
By the middle of April, at least 8 other states were also investigating possible mumps cases. More states will likely become involved: 2 people who were probably infectious traveled on 9 commercial airline flights in a 1-week period in late March.2 The number of fellow travelers infected is under investigation.
In Iowa, investigation has shown that 5% of those infected reported no history of mumps immunization, 13% reported only 1 MMR vaccine, and in 30% the vaccine status was unknown. A majority of cases (51%) had received the recommended 2 MMR vaccines.1 These numbers are consistent with what would be expected with a vaccine that has 90% to 95% effectiveness in a highly immunized population. In such conditions, most cases occur among the vaccinated even though their rate of infection is far lower than the unvaccinated.
The strain of mumps virus isolated in this outbreak is the same one responsible for a recent large outbreak in Great Britain, where there have been more than 70,000 cases in the past 3 years.3 In contrast to measles—which has resulted in few secondary cases and practically no prolonged transmission in the US after importation from abroad4 —this introduction of mumps has resulted in more cases and multiple generations. Given that mumps and measles vaccine are usally given together in MMR, the reasons for this difference are not clear and include several possibilities:
- The mumps vaccine appears to be less effective than measles vaccine. The mumps vaccine is reported to be 80% effective after the first dose and 90% after the second,3 where measles vaccine effectiveness approaches 98% after 2 doses.
- The number of persons with atypical or asymptomatic mumps presentations is significant and complicates control efforts.
- There is possibly a lower level of immunity to mumps in older age groups. The pre-vaccine epidemiology of measles and mumps were different, with virtually everyone born before 1957 having contracted measles naturally. This artificial cutoff date has also been used to set an age limit for mumps vaccine, although those born before 1957 may not be universally immune to mumps from natural infection.
- Later adoption of routine mumps immunization (1970s) vs routine measles immunization (1960s).
FIGURE
Age distribution of mumps cases in Iowa
Source: Data from the Iowa Department of Public Health website.1
The public health response: Controlling the outbreak
Mumps vaccine is not effective until 2 to 4 weeks after it is administered, so it is not useful as postexposure prophylaxis. However, it is effective in stopping population-based outbreaks after 1 or 2 generations. MMR vaccine should be given to all who cannot provide evidence of immunity, which includes laboratory evidence of prior mumps infection, birth before 1957, or history of 1 dose of mumps-containing vaccine. Health care workers and students (including college students) should receive a second dose of vaccine.
At schools with documented cases, students and staff without proof of mumps immunity should be excluded until they receive a mumps vaccine (MMR) or provide proof of immunity. Exclusion should be until 25 days after the onset of parotitis in the last person with mumps at the institution. Anyone with mumps should be isolated until 9 days after onset of symptoms.
Laboratory confirmation of mumps involves positive mumps immunoglobulin M (IgM), a 4-fold rise in mumps IgG titers between acute and 2-week convalescent serum, or detection of virus by culture or polymerase chain reaction (PCR) in urine or throat swab specimens. Laboratory results can be confusing in those previously vaccinated; mumps IgM titers may not be detectable, a 4-fold rise in IgG titers my not occur, and the acute IgG titer may be high. False-positive IgM results can occur because of infection with parainfluenza viruses.7
Transmission of the mumps virus occurs through the saliva or respiratory droplets of an infected person. The incubation period is usually 16 to 18 days but can range from 12 to 25 days. A person is infectious up to 2 days before symptoms begin and until 9 days after. Symptoms include myalgia, malaise, fever, and headache followed by tender swelling of parotid or other salivary glands (sublingual, submaxillary). Up to 50% of those infected can present atypically and 20% can be asymptomatic, which compicates disease control efforts.
Compications of mumps caninclude orchitis (in 20% of postpubertal males), oophoritis, mastitis (30% of postpubertal females), pancreatitis (4%), deafness (5/100,000), encephalitis (2/10,000), and spontaneous abortion 25% of first-trimester pregnancies.5,6
How can you help bring this outbreak under control?
Appropriate steps can be grouped into office infection control practices, diagnosis and reporting, and community infection control measures (TABLE).
Office infection control. Office infection control (subject of a Practice Alert8) is critical so that health care settings do not become a major source of disease transmission. Make sure you and your staff have immunity to mumps. Health care workers should receive 2 doses of MMR vaccine at least a month apart. If mumps occurs in your area, consider requiring proof of immunity, even for those born before 1957.
Make sure that tissues and hand sanitizers are available for patients in the waiting areas, and that signs are posted advising respiratory hygiene. Instruct your front-office staff to ask patients to cover their mouths and noses when they cough and sneeze. Make masks available to any patient who is unable or unwilling to comply; surgical masks are sufficient. Health care staff should be familiar with and use recommended hand sanitation practices.
Don’t let patients with parotid gland swelling sit in the waiting area—place them in an examination room and ask them to wear a mask.
Diagnosis and reporting. When you suspect mumps, collect any specimens requested by the local health department. This probably includes an immediate serum sample for IgM or IgG and possibly a convalescent serum for IgG; it may include a throat swab or urine sample for viral isolation. You should know the phone number of the local health department or have access to their Web site so that current recommendations for specimen collection and analysis can be obtained quickly.
Community infection control. If you suspect a patient has mumps, report it to the local health department and instruct the patient to remain in isolation for 9 days after the start of symptoms. Family members and close contacts should be assisted in assuring they are immune to mumps.
Review with each patient their immunization status; encourage those without documented immunity to mumps to receive the vaccine, if they have no contraindications.
TABLE
Family physicians’ role in controlling mumps
| OFFICE INFECTION CONTROL |
| Post respiratory hygiene notices |
| Make readily available for patients and staff tissues, tissue disposal containers, and hand sanitizers |
| Instruct office staff to request patients use respiratory hygiene |
| Have masks available for those who cannot or refuse to comply with respiratory hygiene |
| Train staff to place patients suspected to have mumps in an examine room immediately and to provide them a mask |
| Instruct staff to use recommended hand sanitation methods |
| Insure that staff are immunized |
| DIAGNOSING AND REPORTING |
| Maintain a high index of suspicion for mumps |
| Collect recommended laboratory specimens |
| COMMUNITY INFECTION CONTROL |
| Report suspected mumps cases to the local public health department |
| Advise those infected to remain in isolation until 9 days after the start of symptoms |
| Help insure families and close contacts of those infected are immunized against mumps |
| Check mumps immunization status of all patients |
1. Iowa mumps update. Available at: www.idph.state.ia.us/adper/common/pdf/mumps/mumps_update_051606.pdf. Accessed on May 16, 2006.
2. Centers for Disease Control and Prevention (CDC). Exposure to mumps during air travel—United States, April 2006. MMWR 2006;55:401-402.
3. CDC Health Advisory. Multi-state mumps outbreak. Available at: www.phppo.cdc.gov/HAN/ArchiveSys/ViewMsgV.asp?AlertNum=00243. Accessed on May 16, 2006.
4. CDC. Measles history. Available at: www.cdc.gov/nip/diseases/measles/history.htm. Accessed on May 16, 2006.
5. Heyman DL. Control of Communicable Diseases Manual 18th ed. Washington, DC: American Public Health Association; 2004.
6. Zimmerman L, Reef S, Wharton M. Mumps. Chapter 7 in Manual for the Surveillance of Vaccine-Preventable Diseases. 3rd ed. Washington, DC: National Immunization Program; 2002. Available at: www.cdc.gov/nip/publications/surv-manual/chpt07_mumps.pdf. Accessed on May 16, 2006.
7. CDC. Laboratory testing for mumps infection. Available at: www.cdc.gov/nip/diseases/mumps/lab-test-faqs.htm. Accessed on May 16, 2006.
8. Campos-Outcalt D. Infection control in the outpatient settings. J Fam Pract 2004;53:485-488.
The ongoing mumps epidemic in the Midwestern US is a stark reminder of how fast and easily an epidemic can still occur. It serves as a warning that we need to remain vigilant in maintaining high immunization levels among our patients. The morbidity and mortality resulting from this outbreak will depend on the soundness and response of the public health infrastructure.
We family physicians need to be prepared to detect and prevent mumps among our patients and staff. While it may not be immediately apparent, if we fulfill our roles competently the outbreak will be less severe.
The start of an epidemic
As of May 15, 1765 cases of mumps had been reported to the Iowa Department of Public Health.1 The median age of those infected was 22 years, with more than one third of cases occurring in those aged 16 to 22 years (FIGURE). College students accounted for 20% of cases.
By the middle of April, at least 8 other states were also investigating possible mumps cases. More states will likely become involved: 2 people who were probably infectious traveled on 9 commercial airline flights in a 1-week period in late March.2 The number of fellow travelers infected is under investigation.
In Iowa, investigation has shown that 5% of those infected reported no history of mumps immunization, 13% reported only 1 MMR vaccine, and in 30% the vaccine status was unknown. A majority of cases (51%) had received the recommended 2 MMR vaccines.1 These numbers are consistent with what would be expected with a vaccine that has 90% to 95% effectiveness in a highly immunized population. In such conditions, most cases occur among the vaccinated even though their rate of infection is far lower than the unvaccinated.
The strain of mumps virus isolated in this outbreak is the same one responsible for a recent large outbreak in Great Britain, where there have been more than 70,000 cases in the past 3 years.3 In contrast to measles—which has resulted in few secondary cases and practically no prolonged transmission in the US after importation from abroad4 —this introduction of mumps has resulted in more cases and multiple generations. Given that mumps and measles vaccine are usally given together in MMR, the reasons for this difference are not clear and include several possibilities:
- The mumps vaccine appears to be less effective than measles vaccine. The mumps vaccine is reported to be 80% effective after the first dose and 90% after the second,3 where measles vaccine effectiveness approaches 98% after 2 doses.
- The number of persons with atypical or asymptomatic mumps presentations is significant and complicates control efforts.
- There is possibly a lower level of immunity to mumps in older age groups. The pre-vaccine epidemiology of measles and mumps were different, with virtually everyone born before 1957 having contracted measles naturally. This artificial cutoff date has also been used to set an age limit for mumps vaccine, although those born before 1957 may not be universally immune to mumps from natural infection.
- Later adoption of routine mumps immunization (1970s) vs routine measles immunization (1960s).
FIGURE
Age distribution of mumps cases in Iowa
Source: Data from the Iowa Department of Public Health website.1
The public health response: Controlling the outbreak
Mumps vaccine is not effective until 2 to 4 weeks after it is administered, so it is not useful as postexposure prophylaxis. However, it is effective in stopping population-based outbreaks after 1 or 2 generations. MMR vaccine should be given to all who cannot provide evidence of immunity, which includes laboratory evidence of prior mumps infection, birth before 1957, or history of 1 dose of mumps-containing vaccine. Health care workers and students (including college students) should receive a second dose of vaccine.
At schools with documented cases, students and staff without proof of mumps immunity should be excluded until they receive a mumps vaccine (MMR) or provide proof of immunity. Exclusion should be until 25 days after the onset of parotitis in the last person with mumps at the institution. Anyone with mumps should be isolated until 9 days after onset of symptoms.
Laboratory confirmation of mumps involves positive mumps immunoglobulin M (IgM), a 4-fold rise in mumps IgG titers between acute and 2-week convalescent serum, or detection of virus by culture or polymerase chain reaction (PCR) in urine or throat swab specimens. Laboratory results can be confusing in those previously vaccinated; mumps IgM titers may not be detectable, a 4-fold rise in IgG titers my not occur, and the acute IgG titer may be high. False-positive IgM results can occur because of infection with parainfluenza viruses.7
Transmission of the mumps virus occurs through the saliva or respiratory droplets of an infected person. The incubation period is usually 16 to 18 days but can range from 12 to 25 days. A person is infectious up to 2 days before symptoms begin and until 9 days after. Symptoms include myalgia, malaise, fever, and headache followed by tender swelling of parotid or other salivary glands (sublingual, submaxillary). Up to 50% of those infected can present atypically and 20% can be asymptomatic, which compicates disease control efforts.
Compications of mumps caninclude orchitis (in 20% of postpubertal males), oophoritis, mastitis (30% of postpubertal females), pancreatitis (4%), deafness (5/100,000), encephalitis (2/10,000), and spontaneous abortion 25% of first-trimester pregnancies.5,6
How can you help bring this outbreak under control?
Appropriate steps can be grouped into office infection control practices, diagnosis and reporting, and community infection control measures (TABLE).
Office infection control. Office infection control (subject of a Practice Alert8) is critical so that health care settings do not become a major source of disease transmission. Make sure you and your staff have immunity to mumps. Health care workers should receive 2 doses of MMR vaccine at least a month apart. If mumps occurs in your area, consider requiring proof of immunity, even for those born before 1957.
Make sure that tissues and hand sanitizers are available for patients in the waiting areas, and that signs are posted advising respiratory hygiene. Instruct your front-office staff to ask patients to cover their mouths and noses when they cough and sneeze. Make masks available to any patient who is unable or unwilling to comply; surgical masks are sufficient. Health care staff should be familiar with and use recommended hand sanitation practices.
Don’t let patients with parotid gland swelling sit in the waiting area—place them in an examination room and ask them to wear a mask.
Diagnosis and reporting. When you suspect mumps, collect any specimens requested by the local health department. This probably includes an immediate serum sample for IgM or IgG and possibly a convalescent serum for IgG; it may include a throat swab or urine sample for viral isolation. You should know the phone number of the local health department or have access to their Web site so that current recommendations for specimen collection and analysis can be obtained quickly.
Community infection control. If you suspect a patient has mumps, report it to the local health department and instruct the patient to remain in isolation for 9 days after the start of symptoms. Family members and close contacts should be assisted in assuring they are immune to mumps.
Review with each patient their immunization status; encourage those without documented immunity to mumps to receive the vaccine, if they have no contraindications.
TABLE
Family physicians’ role in controlling mumps
| OFFICE INFECTION CONTROL |
| Post respiratory hygiene notices |
| Make readily available for patients and staff tissues, tissue disposal containers, and hand sanitizers |
| Instruct office staff to request patients use respiratory hygiene |
| Have masks available for those who cannot or refuse to comply with respiratory hygiene |
| Train staff to place patients suspected to have mumps in an examine room immediately and to provide them a mask |
| Instruct staff to use recommended hand sanitation methods |
| Insure that staff are immunized |
| DIAGNOSING AND REPORTING |
| Maintain a high index of suspicion for mumps |
| Collect recommended laboratory specimens |
| COMMUNITY INFECTION CONTROL |
| Report suspected mumps cases to the local public health department |
| Advise those infected to remain in isolation until 9 days after the start of symptoms |
| Help insure families and close contacts of those infected are immunized against mumps |
| Check mumps immunization status of all patients |
The ongoing mumps epidemic in the Midwestern US is a stark reminder of how fast and easily an epidemic can still occur. It serves as a warning that we need to remain vigilant in maintaining high immunization levels among our patients. The morbidity and mortality resulting from this outbreak will depend on the soundness and response of the public health infrastructure.
We family physicians need to be prepared to detect and prevent mumps among our patients and staff. While it may not be immediately apparent, if we fulfill our roles competently the outbreak will be less severe.
The start of an epidemic
As of May 15, 1765 cases of mumps had been reported to the Iowa Department of Public Health.1 The median age of those infected was 22 years, with more than one third of cases occurring in those aged 16 to 22 years (FIGURE). College students accounted for 20% of cases.
By the middle of April, at least 8 other states were also investigating possible mumps cases. More states will likely become involved: 2 people who were probably infectious traveled on 9 commercial airline flights in a 1-week period in late March.2 The number of fellow travelers infected is under investigation.
In Iowa, investigation has shown that 5% of those infected reported no history of mumps immunization, 13% reported only 1 MMR vaccine, and in 30% the vaccine status was unknown. A majority of cases (51%) had received the recommended 2 MMR vaccines.1 These numbers are consistent with what would be expected with a vaccine that has 90% to 95% effectiveness in a highly immunized population. In such conditions, most cases occur among the vaccinated even though their rate of infection is far lower than the unvaccinated.
The strain of mumps virus isolated in this outbreak is the same one responsible for a recent large outbreak in Great Britain, where there have been more than 70,000 cases in the past 3 years.3 In contrast to measles—which has resulted in few secondary cases and practically no prolonged transmission in the US after importation from abroad4 —this introduction of mumps has resulted in more cases and multiple generations. Given that mumps and measles vaccine are usally given together in MMR, the reasons for this difference are not clear and include several possibilities:
- The mumps vaccine appears to be less effective than measles vaccine. The mumps vaccine is reported to be 80% effective after the first dose and 90% after the second,3 where measles vaccine effectiveness approaches 98% after 2 doses.
- The number of persons with atypical or asymptomatic mumps presentations is significant and complicates control efforts.
- There is possibly a lower level of immunity to mumps in older age groups. The pre-vaccine epidemiology of measles and mumps were different, with virtually everyone born before 1957 having contracted measles naturally. This artificial cutoff date has also been used to set an age limit for mumps vaccine, although those born before 1957 may not be universally immune to mumps from natural infection.
- Later adoption of routine mumps immunization (1970s) vs routine measles immunization (1960s).
FIGURE
Age distribution of mumps cases in Iowa
Source: Data from the Iowa Department of Public Health website.1
The public health response: Controlling the outbreak
Mumps vaccine is not effective until 2 to 4 weeks after it is administered, so it is not useful as postexposure prophylaxis. However, it is effective in stopping population-based outbreaks after 1 or 2 generations. MMR vaccine should be given to all who cannot provide evidence of immunity, which includes laboratory evidence of prior mumps infection, birth before 1957, or history of 1 dose of mumps-containing vaccine. Health care workers and students (including college students) should receive a second dose of vaccine.
At schools with documented cases, students and staff without proof of mumps immunity should be excluded until they receive a mumps vaccine (MMR) or provide proof of immunity. Exclusion should be until 25 days after the onset of parotitis in the last person with mumps at the institution. Anyone with mumps should be isolated until 9 days after onset of symptoms.
Laboratory confirmation of mumps involves positive mumps immunoglobulin M (IgM), a 4-fold rise in mumps IgG titers between acute and 2-week convalescent serum, or detection of virus by culture or polymerase chain reaction (PCR) in urine or throat swab specimens. Laboratory results can be confusing in those previously vaccinated; mumps IgM titers may not be detectable, a 4-fold rise in IgG titers my not occur, and the acute IgG titer may be high. False-positive IgM results can occur because of infection with parainfluenza viruses.7
Transmission of the mumps virus occurs through the saliva or respiratory droplets of an infected person. The incubation period is usually 16 to 18 days but can range from 12 to 25 days. A person is infectious up to 2 days before symptoms begin and until 9 days after. Symptoms include myalgia, malaise, fever, and headache followed by tender swelling of parotid or other salivary glands (sublingual, submaxillary). Up to 50% of those infected can present atypically and 20% can be asymptomatic, which compicates disease control efforts.
Compications of mumps caninclude orchitis (in 20% of postpubertal males), oophoritis, mastitis (30% of postpubertal females), pancreatitis (4%), deafness (5/100,000), encephalitis (2/10,000), and spontaneous abortion 25% of first-trimester pregnancies.5,6
How can you help bring this outbreak under control?
Appropriate steps can be grouped into office infection control practices, diagnosis and reporting, and community infection control measures (TABLE).
Office infection control. Office infection control (subject of a Practice Alert8) is critical so that health care settings do not become a major source of disease transmission. Make sure you and your staff have immunity to mumps. Health care workers should receive 2 doses of MMR vaccine at least a month apart. If mumps occurs in your area, consider requiring proof of immunity, even for those born before 1957.
Make sure that tissues and hand sanitizers are available for patients in the waiting areas, and that signs are posted advising respiratory hygiene. Instruct your front-office staff to ask patients to cover their mouths and noses when they cough and sneeze. Make masks available to any patient who is unable or unwilling to comply; surgical masks are sufficient. Health care staff should be familiar with and use recommended hand sanitation practices.
Don’t let patients with parotid gland swelling sit in the waiting area—place them in an examination room and ask them to wear a mask.
Diagnosis and reporting. When you suspect mumps, collect any specimens requested by the local health department. This probably includes an immediate serum sample for IgM or IgG and possibly a convalescent serum for IgG; it may include a throat swab or urine sample for viral isolation. You should know the phone number of the local health department or have access to their Web site so that current recommendations for specimen collection and analysis can be obtained quickly.
Community infection control. If you suspect a patient has mumps, report it to the local health department and instruct the patient to remain in isolation for 9 days after the start of symptoms. Family members and close contacts should be assisted in assuring they are immune to mumps.
Review with each patient their immunization status; encourage those without documented immunity to mumps to receive the vaccine, if they have no contraindications.
TABLE
Family physicians’ role in controlling mumps
| OFFICE INFECTION CONTROL |
| Post respiratory hygiene notices |
| Make readily available for patients and staff tissues, tissue disposal containers, and hand sanitizers |
| Instruct office staff to request patients use respiratory hygiene |
| Have masks available for those who cannot or refuse to comply with respiratory hygiene |
| Train staff to place patients suspected to have mumps in an examine room immediately and to provide them a mask |
| Instruct staff to use recommended hand sanitation methods |
| Insure that staff are immunized |
| DIAGNOSING AND REPORTING |
| Maintain a high index of suspicion for mumps |
| Collect recommended laboratory specimens |
| COMMUNITY INFECTION CONTROL |
| Report suspected mumps cases to the local public health department |
| Advise those infected to remain in isolation until 9 days after the start of symptoms |
| Help insure families and close contacts of those infected are immunized against mumps |
| Check mumps immunization status of all patients |
1. Iowa mumps update. Available at: www.idph.state.ia.us/adper/common/pdf/mumps/mumps_update_051606.pdf. Accessed on May 16, 2006.
2. Centers for Disease Control and Prevention (CDC). Exposure to mumps during air travel—United States, April 2006. MMWR 2006;55:401-402.
3. CDC Health Advisory. Multi-state mumps outbreak. Available at: www.phppo.cdc.gov/HAN/ArchiveSys/ViewMsgV.asp?AlertNum=00243. Accessed on May 16, 2006.
4. CDC. Measles history. Available at: www.cdc.gov/nip/diseases/measles/history.htm. Accessed on May 16, 2006.
5. Heyman DL. Control of Communicable Diseases Manual 18th ed. Washington, DC: American Public Health Association; 2004.
6. Zimmerman L, Reef S, Wharton M. Mumps. Chapter 7 in Manual for the Surveillance of Vaccine-Preventable Diseases. 3rd ed. Washington, DC: National Immunization Program; 2002. Available at: www.cdc.gov/nip/publications/surv-manual/chpt07_mumps.pdf. Accessed on May 16, 2006.
7. CDC. Laboratory testing for mumps infection. Available at: www.cdc.gov/nip/diseases/mumps/lab-test-faqs.htm. Accessed on May 16, 2006.
8. Campos-Outcalt D. Infection control in the outpatient settings. J Fam Pract 2004;53:485-488.
1. Iowa mumps update. Available at: www.idph.state.ia.us/adper/common/pdf/mumps/mumps_update_051606.pdf. Accessed on May 16, 2006.
2. Centers for Disease Control and Prevention (CDC). Exposure to mumps during air travel—United States, April 2006. MMWR 2006;55:401-402.
3. CDC Health Advisory. Multi-state mumps outbreak. Available at: www.phppo.cdc.gov/HAN/ArchiveSys/ViewMsgV.asp?AlertNum=00243. Accessed on May 16, 2006.
4. CDC. Measles history. Available at: www.cdc.gov/nip/diseases/measles/history.htm. Accessed on May 16, 2006.
5. Heyman DL. Control of Communicable Diseases Manual 18th ed. Washington, DC: American Public Health Association; 2004.
6. Zimmerman L, Reef S, Wharton M. Mumps. Chapter 7 in Manual for the Surveillance of Vaccine-Preventable Diseases. 3rd ed. Washington, DC: National Immunization Program; 2002. Available at: www.cdc.gov/nip/publications/surv-manual/chpt07_mumps.pdf. Accessed on May 16, 2006.
7. CDC. Laboratory testing for mumps infection. Available at: www.cdc.gov/nip/diseases/mumps/lab-test-faqs.htm. Accessed on May 16, 2006.
8. Campos-Outcalt D. Infection control in the outpatient settings. J Fam Pract 2004;53:485-488.