User login
ANSWER
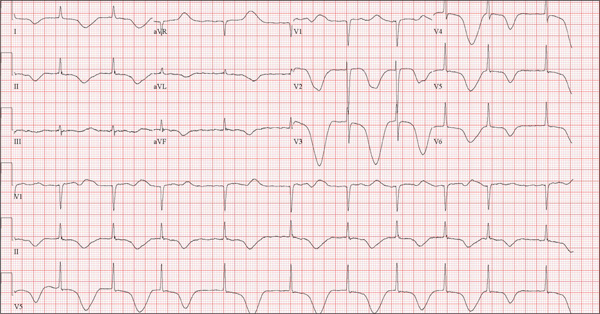
The correct interpretation of this ECG includes atrial fibrillation and ST- and T-wave changes consistent with a central nervous system hemorrhage, as well as a markedly prolonged QT interval.
The most common ECG alterations seen in cases of acute subarachnoid hemorrhage include repolarization abnormalities due to imbalance of autonomic cardiovascular control. While ST depression is more common in patients with poor outcomes, it is not predictive.
ANSWER
The correct interpretation of this ECG includes atrial fibrillation and ST- and T-wave changes consistent with a central nervous system hemorrhage, as well as a markedly prolonged QT interval.
The most common ECG alterations seen in cases of acute subarachnoid hemorrhage include repolarization abnormalities due to imbalance of autonomic cardiovascular control. While ST depression is more common in patients with poor outcomes, it is not predictive.
ANSWER
The correct interpretation of this ECG includes atrial fibrillation and ST- and T-wave changes consistent with a central nervous system hemorrhage, as well as a markedly prolonged QT interval.
The most common ECG alterations seen in cases of acute subarachnoid hemorrhage include repolarization abnormalities due to imbalance of autonomic cardiovascular control. While ST depression is more common in patients with poor outcomes, it is not predictive.
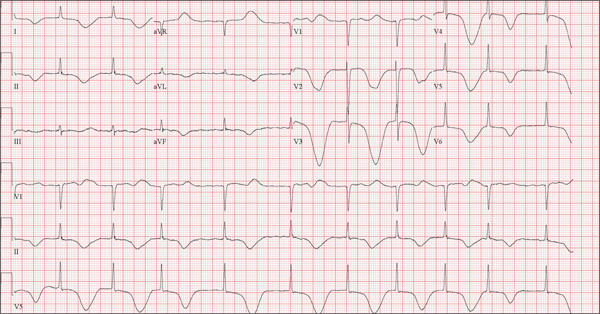
A 68-year-old man was found on his knees, vomiting, in his backyard by a neighbor early this morning. When asked if he was OK, the patient responded that he suddenly felt nauseated and had a headache. The neighbor helped him to his feet and, noticing that his left leg and arm were weak, called 911. During that time, the neighbor observed slurred speech. As they waited for the ambulance to arrive, the patient was able to say that this was the worst headache he’d ever had. When the paramedics arrived, they recorded a blood pressure of 198/120 mm Hg, consistent in both arms. Medical history is remarkable for hypertension, paroxysmal atrial fibrillation, adult-onset diabetes, and nephrolithiasis. Surgical history is remarkable for appendectomy, cholecystectomy, and lithotripsy. The patient is a retired civil engineer who lives at home alone. His wife died three years ago of complications from uterine cancer. He has one adult son who is in excellent health but lives on the opposite coast. The patient has never smoked and drinks approximately one six-pack of beer per month. Current medications include hydrochlorothiazide, metformin, and rivaroxaban. He is allergic to sulfa-containing medications. A complete review of systems is not obtained, given the patient’s slurred speech and progressive aphasia. He is able to nod yes or no to specific questions, and no significant symptoms or findings are identified. At the hospital, the patient is agitated and in apparent distress, with severe headache and aphasia. Vital signs include a blood pressure of 180/110 mm Hg; pulse, 60 beats/min; respiratory rate, 14 breaths/min; and temperature, 98.4°F. The O2 saturation is 96.4% on room air. Pertinent physical findings include aphasia, oculomotor nerve palsy, nuchal rigidity, and findings of a left-sided (right hemispheric) progressive hemiparesis. The remainder of the physical examination is noncontributory. Samples are drawn for laboratory testing, and an ECG is obtained prior to the patient’s transfer to radiology for CT of the head. The ECG findings include a ventricular rate of 62 beats/min; QRS duration, 88 ms; QT/QTc interval, 718/728 ms; P axis, not measured; R axis, 35°; and T axis, 209°. What is your interpretation of this ECG?