User login
New-onset atrial fibrillation, or NOAF, occurred in nearly a third of 138 patients who underwent transcatheter aortic valve implantation in a prospective study, and the condition was associated with a significantly higher rate of cardioembolic events at 30-day and 12-month follow-up.
NOAF occurred in 44 patients at a median of 48 hours after transcatheter aortic valve implantation (TAVI), with 10 episodes resolving spontaneously within 12 hours, and 34 episodes requiring pharmacologic intervention. The rate of the combined end point of stroke and systemic embolism was 13.6% at 30 days in the NOAF group, compared with 3.2% in those who did not experience NOAF (odds ratio, 4.79); the rate was 15.9% vs. 3.2% at 12 months (OR, 5.0), Dr. Ignacio J. Amat-Santos of Laval University, Quebec City, and his colleagues reported online on Dec. 14 the Journal of the American College of Cardiology.
Significant independent predictors of NOAF included left atrial size (OR of 1.21/each increase of 1 mm/m2) and use of the transapical approach (OR, 4.08). An atrial size of 27 mm/m2 or greater as measured by echocardiography was identified as the cutoff point with the best sensitivity and specificity for predicting NOAF within 30 days of TAVI, the investigators said (J. Am. Coll. Cardiol. 2011 [doi:10/1016/j.jacc.2011.09.061]).
Furthermore, the incidence of NOAF in those with an atrial size of 27 mm/m2 or greater undergoing TAVI by the transapical approach vs. the transfemoral approach was 57% vs. 12%, respectively, they noted.
Mortality, which was 16% and 21% in those with and without NOAF at 12 months, respectively, did not differ significantly between the groups at either follow-up, they noted.
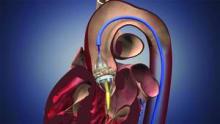
Patients in the study had severe symptomatic aortic stenosis, but no history of chronic/paroxysmal atrial fibrillation. They underwent TAVI with a balloon-expandable valve by either the transapical or transfemoral approach, were enrolled consecutively between May 2007 and May 2011, and underwent continuous electrocardiographic monitoring during hospitalization. NOAF was defined as any episode of AF lasting longer than 30 seconds.
NOAF is a known complication in patients undergoing cardiovascular interventions, but this is one of the first studies to verify an increased risk of the condition in patients undergoing TAVI, which has emerged as an alternative treatment for patients with severe symptomatic aortic stenosis and high or prohibitive operative risk. The study is also among the first to characterize predictive factors for NOAF.
"The occurrence of cerebrovascular events is probably the most worrisome complication associated with TAVI, with an incidence of about 4%, one of the highest ever reported in the field of interventional cardiology," the investigators said, noting that the fact that more than 50% of the complications occur several days after TAVI suggests that "mechanisms other than those directly related to the procedure may be involved."
Indeed, the findings of this study suggest NOAF may be an important mechanism for late neurological events after TAVI, and if confirmed in larger studies, the findings may have implications for the development of prevention trials.
"Knowing the predictive factors of NOAF following TAVI should allow us to select the patients at higher risk for NOAF preventive studies in the setting of TAVI," they investigators said.
Also of note, some of the cardioembolic events in this study seemed to be related to the non-initiation of anticoagulant therapy, the investigators said, adding that the risk of a cardioembolic event was as high as 40% in those who had NOAF and who did not receive anticoagulant therapy.
This underscores the clinical relevance of optimizing antithrombotic treatment in this high-risk subset of patients, they concluded.
Dr. Amat-Santos disclosed that he received support from the Institute of Heart Sciences. Other authors disclosed having served as consultants for Edwards Lifesciences, and/or St. Jude Medical.
The research by Dr. Amat-Santos and his colleagues deserves attention because of its originality and because of its potential implications for managing TAVI patients, according to Dr. Bernard Iung, Dr. Dominique Himbert, and Dr. Alex Vahanian.
In an accompanying editorial, they note that besides frequency and predictive factors of NOAF in patients who undergo TAVI, one of the most clinically relevant issues addressed by the study is the assessment of its impact following the procedure. While the findings should be interpreted with caution given the small number of embolic events, they represent a "relevant contribution in the analysis of the potential causes of embolic events after TAVI," they said (J. Am. Coll. Cardiol. 2012 [doi:10.1016/j.jacc2011.11.005]).
"Despite the number of mechanisms that may be involved in stroke after TAVI, the particularly strong relationship between post-procedural AF and stroke occurring after 24 h suggests that a cardioembolic origin significantly contributes to stroke after TAVI," they added, noting that the association raises questions about the most appropriate post-procedure antithrombotic therapy, and highlights the need for larger randomized trials to optimize antithrombotic therapy in TAVI patients.
The association also highlights the need for improving the identification of patients at risk, and testing pharmacological approaches to reducing atrial fibrillation incidence, they concluded.
Dr. Iung, Dr. Himbert, and Dr. Vahanian are with Bichat Hospital, Paris. Dr. Iung disclosed that he has received consulting fees from Servier, Boehringer Ingelheim, Bayer, Valtech, and Abbott, as well as speakers fees from Edwards Lifesciences, St. Jude Medical, and Sanofi-Aventis. Dr. Himbert disclosed receiving proctoring fees from Edwards Lifesciences and Medtronic. Dr. Vahanian disclosed serving as an advisory board member for Medtronic, Abbott, Valtech, and Boehringer Ingelheim, and receiving speakers fees from Edwards Lifesciences and Siemens.
The research by Dr. Amat-Santos and his colleagues deserves attention because of its originality and because of its potential implications for managing TAVI patients, according to Dr. Bernard Iung, Dr. Dominique Himbert, and Dr. Alex Vahanian.
In an accompanying editorial, they note that besides frequency and predictive factors of NOAF in patients who undergo TAVI, one of the most clinically relevant issues addressed by the study is the assessment of its impact following the procedure. While the findings should be interpreted with caution given the small number of embolic events, they represent a "relevant contribution in the analysis of the potential causes of embolic events after TAVI," they said (J. Am. Coll. Cardiol. 2012 [doi:10.1016/j.jacc2011.11.005]).
"Despite the number of mechanisms that may be involved in stroke after TAVI, the particularly strong relationship between post-procedural AF and stroke occurring after 24 h suggests that a cardioembolic origin significantly contributes to stroke after TAVI," they added, noting that the association raises questions about the most appropriate post-procedure antithrombotic therapy, and highlights the need for larger randomized trials to optimize antithrombotic therapy in TAVI patients.
The association also highlights the need for improving the identification of patients at risk, and testing pharmacological approaches to reducing atrial fibrillation incidence, they concluded.
Dr. Iung, Dr. Himbert, and Dr. Vahanian are with Bichat Hospital, Paris. Dr. Iung disclosed that he has received consulting fees from Servier, Boehringer Ingelheim, Bayer, Valtech, and Abbott, as well as speakers fees from Edwards Lifesciences, St. Jude Medical, and Sanofi-Aventis. Dr. Himbert disclosed receiving proctoring fees from Edwards Lifesciences and Medtronic. Dr. Vahanian disclosed serving as an advisory board member for Medtronic, Abbott, Valtech, and Boehringer Ingelheim, and receiving speakers fees from Edwards Lifesciences and Siemens.
The research by Dr. Amat-Santos and his colleagues deserves attention because of its originality and because of its potential implications for managing TAVI patients, according to Dr. Bernard Iung, Dr. Dominique Himbert, and Dr. Alex Vahanian.
In an accompanying editorial, they note that besides frequency and predictive factors of NOAF in patients who undergo TAVI, one of the most clinically relevant issues addressed by the study is the assessment of its impact following the procedure. While the findings should be interpreted with caution given the small number of embolic events, they represent a "relevant contribution in the analysis of the potential causes of embolic events after TAVI," they said (J. Am. Coll. Cardiol. 2012 [doi:10.1016/j.jacc2011.11.005]).
"Despite the number of mechanisms that may be involved in stroke after TAVI, the particularly strong relationship between post-procedural AF and stroke occurring after 24 h suggests that a cardioembolic origin significantly contributes to stroke after TAVI," they added, noting that the association raises questions about the most appropriate post-procedure antithrombotic therapy, and highlights the need for larger randomized trials to optimize antithrombotic therapy in TAVI patients.
The association also highlights the need for improving the identification of patients at risk, and testing pharmacological approaches to reducing atrial fibrillation incidence, they concluded.
Dr. Iung, Dr. Himbert, and Dr. Vahanian are with Bichat Hospital, Paris. Dr. Iung disclosed that he has received consulting fees from Servier, Boehringer Ingelheim, Bayer, Valtech, and Abbott, as well as speakers fees from Edwards Lifesciences, St. Jude Medical, and Sanofi-Aventis. Dr. Himbert disclosed receiving proctoring fees from Edwards Lifesciences and Medtronic. Dr. Vahanian disclosed serving as an advisory board member for Medtronic, Abbott, Valtech, and Boehringer Ingelheim, and receiving speakers fees from Edwards Lifesciences and Siemens.
New-onset atrial fibrillation, or NOAF, occurred in nearly a third of 138 patients who underwent transcatheter aortic valve implantation in a prospective study, and the condition was associated with a significantly higher rate of cardioembolic events at 30-day and 12-month follow-up.
NOAF occurred in 44 patients at a median of 48 hours after transcatheter aortic valve implantation (TAVI), with 10 episodes resolving spontaneously within 12 hours, and 34 episodes requiring pharmacologic intervention. The rate of the combined end point of stroke and systemic embolism was 13.6% at 30 days in the NOAF group, compared with 3.2% in those who did not experience NOAF (odds ratio, 4.79); the rate was 15.9% vs. 3.2% at 12 months (OR, 5.0), Dr. Ignacio J. Amat-Santos of Laval University, Quebec City, and his colleagues reported online on Dec. 14 the Journal of the American College of Cardiology.
Significant independent predictors of NOAF included left atrial size (OR of 1.21/each increase of 1 mm/m2) and use of the transapical approach (OR, 4.08). An atrial size of 27 mm/m2 or greater as measured by echocardiography was identified as the cutoff point with the best sensitivity and specificity for predicting NOAF within 30 days of TAVI, the investigators said (J. Am. Coll. Cardiol. 2011 [doi:10/1016/j.jacc.2011.09.061]).
Furthermore, the incidence of NOAF in those with an atrial size of 27 mm/m2 or greater undergoing TAVI by the transapical approach vs. the transfemoral approach was 57% vs. 12%, respectively, they noted.
Mortality, which was 16% and 21% in those with and without NOAF at 12 months, respectively, did not differ significantly between the groups at either follow-up, they noted.
Patients in the study had severe symptomatic aortic stenosis, but no history of chronic/paroxysmal atrial fibrillation. They underwent TAVI with a balloon-expandable valve by either the transapical or transfemoral approach, were enrolled consecutively between May 2007 and May 2011, and underwent continuous electrocardiographic monitoring during hospitalization. NOAF was defined as any episode of AF lasting longer than 30 seconds.
NOAF is a known complication in patients undergoing cardiovascular interventions, but this is one of the first studies to verify an increased risk of the condition in patients undergoing TAVI, which has emerged as an alternative treatment for patients with severe symptomatic aortic stenosis and high or prohibitive operative risk. The study is also among the first to characterize predictive factors for NOAF.
"The occurrence of cerebrovascular events is probably the most worrisome complication associated with TAVI, with an incidence of about 4%, one of the highest ever reported in the field of interventional cardiology," the investigators said, noting that the fact that more than 50% of the complications occur several days after TAVI suggests that "mechanisms other than those directly related to the procedure may be involved."
Indeed, the findings of this study suggest NOAF may be an important mechanism for late neurological events after TAVI, and if confirmed in larger studies, the findings may have implications for the development of prevention trials.
"Knowing the predictive factors of NOAF following TAVI should allow us to select the patients at higher risk for NOAF preventive studies in the setting of TAVI," they investigators said.
Also of note, some of the cardioembolic events in this study seemed to be related to the non-initiation of anticoagulant therapy, the investigators said, adding that the risk of a cardioembolic event was as high as 40% in those who had NOAF and who did not receive anticoagulant therapy.
This underscores the clinical relevance of optimizing antithrombotic treatment in this high-risk subset of patients, they concluded.
Dr. Amat-Santos disclosed that he received support from the Institute of Heart Sciences. Other authors disclosed having served as consultants for Edwards Lifesciences, and/or St. Jude Medical.
New-onset atrial fibrillation, or NOAF, occurred in nearly a third of 138 patients who underwent transcatheter aortic valve implantation in a prospective study, and the condition was associated with a significantly higher rate of cardioembolic events at 30-day and 12-month follow-up.
NOAF occurred in 44 patients at a median of 48 hours after transcatheter aortic valve implantation (TAVI), with 10 episodes resolving spontaneously within 12 hours, and 34 episodes requiring pharmacologic intervention. The rate of the combined end point of stroke and systemic embolism was 13.6% at 30 days in the NOAF group, compared with 3.2% in those who did not experience NOAF (odds ratio, 4.79); the rate was 15.9% vs. 3.2% at 12 months (OR, 5.0), Dr. Ignacio J. Amat-Santos of Laval University, Quebec City, and his colleagues reported online on Dec. 14 the Journal of the American College of Cardiology.
Significant independent predictors of NOAF included left atrial size (OR of 1.21/each increase of 1 mm/m2) and use of the transapical approach (OR, 4.08). An atrial size of 27 mm/m2 or greater as measured by echocardiography was identified as the cutoff point with the best sensitivity and specificity for predicting NOAF within 30 days of TAVI, the investigators said (J. Am. Coll. Cardiol. 2011 [doi:10/1016/j.jacc.2011.09.061]).
Furthermore, the incidence of NOAF in those with an atrial size of 27 mm/m2 or greater undergoing TAVI by the transapical approach vs. the transfemoral approach was 57% vs. 12%, respectively, they noted.
Mortality, which was 16% and 21% in those with and without NOAF at 12 months, respectively, did not differ significantly between the groups at either follow-up, they noted.
Patients in the study had severe symptomatic aortic stenosis, but no history of chronic/paroxysmal atrial fibrillation. They underwent TAVI with a balloon-expandable valve by either the transapical or transfemoral approach, were enrolled consecutively between May 2007 and May 2011, and underwent continuous electrocardiographic monitoring during hospitalization. NOAF was defined as any episode of AF lasting longer than 30 seconds.
NOAF is a known complication in patients undergoing cardiovascular interventions, but this is one of the first studies to verify an increased risk of the condition in patients undergoing TAVI, which has emerged as an alternative treatment for patients with severe symptomatic aortic stenosis and high or prohibitive operative risk. The study is also among the first to characterize predictive factors for NOAF.
"The occurrence of cerebrovascular events is probably the most worrisome complication associated with TAVI, with an incidence of about 4%, one of the highest ever reported in the field of interventional cardiology," the investigators said, noting that the fact that more than 50% of the complications occur several days after TAVI suggests that "mechanisms other than those directly related to the procedure may be involved."
Indeed, the findings of this study suggest NOAF may be an important mechanism for late neurological events after TAVI, and if confirmed in larger studies, the findings may have implications for the development of prevention trials.
"Knowing the predictive factors of NOAF following TAVI should allow us to select the patients at higher risk for NOAF preventive studies in the setting of TAVI," they investigators said.
Also of note, some of the cardioembolic events in this study seemed to be related to the non-initiation of anticoagulant therapy, the investigators said, adding that the risk of a cardioembolic event was as high as 40% in those who had NOAF and who did not receive anticoagulant therapy.
This underscores the clinical relevance of optimizing antithrombotic treatment in this high-risk subset of patients, they concluded.
Dr. Amat-Santos disclosed that he received support from the Institute of Heart Sciences. Other authors disclosed having served as consultants for Edwards Lifesciences, and/or St. Jude Medical.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Major Finding: NOAF occurred in 44 patients at a median of 48 hours after transcatheter aortic valve implantation (TAVI), with 10 episodes resolving spontaneously within 12 hours, and 34 requiring pharmacologic intervention. The rate of the combined end point of stroke and systemic embolism was 13.6% at 30 days in the NOAF group, compared with 3.2% (odds ratio 4.79) in those who did not experience NOAF; the rate was 15.9% vs. 3.2% at 12 months (odds ratio 5.0).
Data Source: A prospective study of 138 patients undergoing TAVI.
Disclosures: Dr. Amat-Santos disclosed that he received support from the Institute of Heart Sciences. Other authors disclosed that they have consulted for Edwards Lifesciences Inc., and/or St. Jude Medical.