User login
Emricasan, a caspase inhibitor, achieves a significant reduction in portal pressure among patients with cirrhosis and severe portal hypertension, according to the abstract for a proof-of-concept study that will be presented as a late-breaker at the annual meeting of the American Association for the Study of Liver Disease (AASLD).
The results of this multicenter, open-label study are consistent with benefits in animal models of portal hypertension in which emricasan has not only lowered pressure but improved survival, according to Dr. Guadalupe Garcia-Tsao, director, Clinical and Translational Core, Yale Liver Center, Yale University, New Haven, Conn.
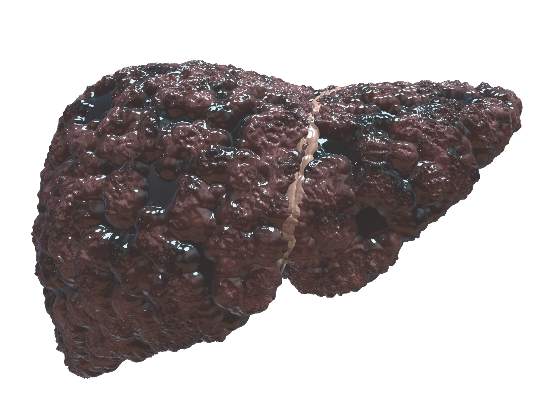
The study enrolled 23 patients with compensated cirrhosis and portal hypertension, defined as a hepatic venous pressure gradient (HVPG) greater than 5 mm Hg. The underlying etiology for the cirrhosis in most patients was nonalcoholic steatohepatitis (NASH) or hepatitis C viral (HCV) infection. The median MELD (model for end-stage liver disease) score was 8 but ranged as high as 15. Nearly 90% were in Child-Pugh class A.
Patients received 25 mg emricasan orally twice per day for 28 days. The primary outcome was change in HVPG, which was evaluated with a standardized protocol. A single expert read all HVPG tracings.
Although the median HVPG values for the study population overall were not changed significantly when baseline and end-of-treatment measures were compared (13.5 vs. 13.0 mm Hg), a significant reduction was observed in those with the most severe portal hypertension as defined by a HVPG score greater than or equal to 12 mm Hg. Among the 12 patients with this degree of severity, the mean decrease of 3.7 mm Hg represented a 17.2% reduction (P less than .003) from baseline. All had at least a 10% reduction and four of the 12 had a reduction greater than 20%.
In those with severe portal hypertension achieving pressure reductions as well as in the overall study population, emricasan was associated with significant reductions in levels of the liver enzymes aspartate aminotransferase and alanine aminotransferase. In addition, emricasan treatment was associated with significant declines in the serum levels of cCk18 and caspase 3/7, which are markers of apoptosis. These findings are consistent with the mechanism of benefit suggested by studies previously undertaken in murine models of portal hypertension.
“Caspases play a central role in apoptosis and inflammation. They produce hemodynamically active, proinflammatory microparticles that appear to contribute to the vasodilation that maintains and enhances portal hypertension in cirrhosis,” Dr. Garcia-Tsao explained. She suggested that the reduction in liver enzymes also suggests an intrahepatic anti-inflammatory effect.
Further study of emricasan, which was characterized as a “pan-caspase inhibitor” is encouraged by the acceptable tolerability observed in this study. Although one participant did leave the study early because of a side effect, it was considered not serious. It cannot be determined from this study whether the benefits observed in those with severe portal hypertension were due to protective effects on liver cells rather than a hemodynamic mechanism, but the potential for this agent to prevent microvascular remodeling has implications for preventing progression and end-stage events.
Dr. Garcia-Tsao reported financial relationships with AbbVie and FibroGen.
Emricasan, a caspase inhibitor, achieves a significant reduction in portal pressure among patients with cirrhosis and severe portal hypertension, according to the abstract for a proof-of-concept study that will be presented as a late-breaker at the annual meeting of the American Association for the Study of Liver Disease (AASLD).
The results of this multicenter, open-label study are consistent with benefits in animal models of portal hypertension in which emricasan has not only lowered pressure but improved survival, according to Dr. Guadalupe Garcia-Tsao, director, Clinical and Translational Core, Yale Liver Center, Yale University, New Haven, Conn.
The study enrolled 23 patients with compensated cirrhosis and portal hypertension, defined as a hepatic venous pressure gradient (HVPG) greater than 5 mm Hg. The underlying etiology for the cirrhosis in most patients was nonalcoholic steatohepatitis (NASH) or hepatitis C viral (HCV) infection. The median MELD (model for end-stage liver disease) score was 8 but ranged as high as 15. Nearly 90% were in Child-Pugh class A.
Patients received 25 mg emricasan orally twice per day for 28 days. The primary outcome was change in HVPG, which was evaluated with a standardized protocol. A single expert read all HVPG tracings.
Although the median HVPG values for the study population overall were not changed significantly when baseline and end-of-treatment measures were compared (13.5 vs. 13.0 mm Hg), a significant reduction was observed in those with the most severe portal hypertension as defined by a HVPG score greater than or equal to 12 mm Hg. Among the 12 patients with this degree of severity, the mean decrease of 3.7 mm Hg represented a 17.2% reduction (P less than .003) from baseline. All had at least a 10% reduction and four of the 12 had a reduction greater than 20%.
In those with severe portal hypertension achieving pressure reductions as well as in the overall study population, emricasan was associated with significant reductions in levels of the liver enzymes aspartate aminotransferase and alanine aminotransferase. In addition, emricasan treatment was associated with significant declines in the serum levels of cCk18 and caspase 3/7, which are markers of apoptosis. These findings are consistent with the mechanism of benefit suggested by studies previously undertaken in murine models of portal hypertension.
“Caspases play a central role in apoptosis and inflammation. They produce hemodynamically active, proinflammatory microparticles that appear to contribute to the vasodilation that maintains and enhances portal hypertension in cirrhosis,” Dr. Garcia-Tsao explained. She suggested that the reduction in liver enzymes also suggests an intrahepatic anti-inflammatory effect.
Further study of emricasan, which was characterized as a “pan-caspase inhibitor” is encouraged by the acceptable tolerability observed in this study. Although one participant did leave the study early because of a side effect, it was considered not serious. It cannot be determined from this study whether the benefits observed in those with severe portal hypertension were due to protective effects on liver cells rather than a hemodynamic mechanism, but the potential for this agent to prevent microvascular remodeling has implications for preventing progression and end-stage events.
Dr. Garcia-Tsao reported financial relationships with AbbVie and FibroGen.
Emricasan, a caspase inhibitor, achieves a significant reduction in portal pressure among patients with cirrhosis and severe portal hypertension, according to the abstract for a proof-of-concept study that will be presented as a late-breaker at the annual meeting of the American Association for the Study of Liver Disease (AASLD).
The results of this multicenter, open-label study are consistent with benefits in animal models of portal hypertension in which emricasan has not only lowered pressure but improved survival, according to Dr. Guadalupe Garcia-Tsao, director, Clinical and Translational Core, Yale Liver Center, Yale University, New Haven, Conn.
The study enrolled 23 patients with compensated cirrhosis and portal hypertension, defined as a hepatic venous pressure gradient (HVPG) greater than 5 mm Hg. The underlying etiology for the cirrhosis in most patients was nonalcoholic steatohepatitis (NASH) or hepatitis C viral (HCV) infection. The median MELD (model for end-stage liver disease) score was 8 but ranged as high as 15. Nearly 90% were in Child-Pugh class A.
Patients received 25 mg emricasan orally twice per day for 28 days. The primary outcome was change in HVPG, which was evaluated with a standardized protocol. A single expert read all HVPG tracings.
Although the median HVPG values for the study population overall were not changed significantly when baseline and end-of-treatment measures were compared (13.5 vs. 13.0 mm Hg), a significant reduction was observed in those with the most severe portal hypertension as defined by a HVPG score greater than or equal to 12 mm Hg. Among the 12 patients with this degree of severity, the mean decrease of 3.7 mm Hg represented a 17.2% reduction (P less than .003) from baseline. All had at least a 10% reduction and four of the 12 had a reduction greater than 20%.
In those with severe portal hypertension achieving pressure reductions as well as in the overall study population, emricasan was associated with significant reductions in levels of the liver enzymes aspartate aminotransferase and alanine aminotransferase. In addition, emricasan treatment was associated with significant declines in the serum levels of cCk18 and caspase 3/7, which are markers of apoptosis. These findings are consistent with the mechanism of benefit suggested by studies previously undertaken in murine models of portal hypertension.
“Caspases play a central role in apoptosis and inflammation. They produce hemodynamically active, proinflammatory microparticles that appear to contribute to the vasodilation that maintains and enhances portal hypertension in cirrhosis,” Dr. Garcia-Tsao explained. She suggested that the reduction in liver enzymes also suggests an intrahepatic anti-inflammatory effect.
Further study of emricasan, which was characterized as a “pan-caspase inhibitor” is encouraged by the acceptable tolerability observed in this study. Although one participant did leave the study early because of a side effect, it was considered not serious. It cannot be determined from this study whether the benefits observed in those with severe portal hypertension were due to protective effects on liver cells rather than a hemodynamic mechanism, but the potential for this agent to prevent microvascular remodeling has implications for preventing progression and end-stage events.
Dr. Garcia-Tsao reported financial relationships with AbbVie and FibroGen.
FROM THE LIVER MEETING 2015
Key clinical point: The experimental caspase inhibitor emricasan significantly reduced portal pressure in patients with compensated cirrhosis and severe portal hypertension in a proof-of-concept study.
Major finding: The association between reduced portal pressure and markers of apoptosis and liver cell injury are consistent with an intrahepatic effect that may inhibit microvascular remodeling.
Data source: Multicenter open-label study.
Disclosures: Dr. Garcia-Tsao reported financial relationships with AbbVie and FibroGen.