User login
ANSWER
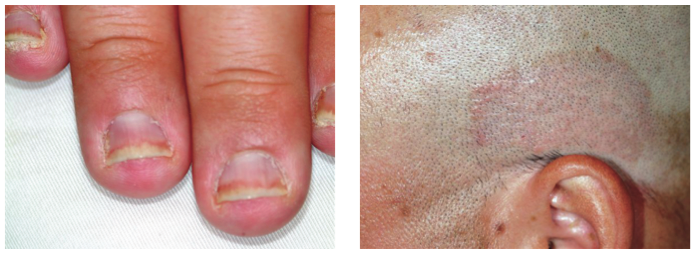
The correct answer is psoriasis (choice “d”), which often involves nail and skin changes such as those seen in this case. There was no particular reason to think this patient had an infection of any kind, but, as is often the case, the original provider considered only one diagnostic possibility.
DISCUSSION
Nail disease can be problematic for both patient and provider. Arguably the biggest issue with it, initially, is “the one-item differential”—the idea that all nail disease can be classified as “fungal infection” simply because neither the patient nor the provider considers any other explanation for the changes seen. This case illustrates that dilemma nicely.
Psoriasis affects more than 2% of the US population, making it a common skin disorder. As this case illustrates, it may affect several areas with diverse but predictable morphologic presentations, all appearing at the same time.
The key diagnostic points from this case include:
• Stress is a known trigger for psoriasis vulgaris.
• The patient’s nails failed to respond to terbinafine treatment.
• There was no obvious source of fungal infection (eg, contact with animals) or reason for him to have a yeast infection (eg, diabetes) or develop mold “infection” in the nails (eg, trauma from digging in soil).
• Fungal infections are about 18 times less likely to occur in the fingernails than in the toenails.
• A unifying explanation for simultaneous nail and skin changes was needed.
• The nail and skin changes seen here are quite typical for psoriasis.
Most important, though, is the need to overcome the urge to hop on the “fungal bandwagon” by first considering other diagnostic possibilities.
Continue for the treatment of this condition >>
TREATMENT
Unfortunately, there is no good treatment for this patient’s nails. However, there is an excellent chance that his scalp psoriasis will respond to short-term use of fluocinolone 0.05% cream.
This patient was also counseled about the role of stress in his condition and the benefits of modest increases in UV exposure. During follow-up, it will be important to ask about joint pain, since up to 30% of psoriasis patients will eventually develop psoriatic arthritis.
If the patient’s current treatment does not produce sufficient results, other options include calcipotriene ointment, oral methotrexate, or even one of the biologics (etanercept or adalimumab).
ANSWER
The correct answer is psoriasis (choice “d”), which often involves nail and skin changes such as those seen in this case. There was no particular reason to think this patient had an infection of any kind, but, as is often the case, the original provider considered only one diagnostic possibility.
DISCUSSION
Nail disease can be problematic for both patient and provider. Arguably the biggest issue with it, initially, is “the one-item differential”—the idea that all nail disease can be classified as “fungal infection” simply because neither the patient nor the provider considers any other explanation for the changes seen. This case illustrates that dilemma nicely.
Psoriasis affects more than 2% of the US population, making it a common skin disorder. As this case illustrates, it may affect several areas with diverse but predictable morphologic presentations, all appearing at the same time.
The key diagnostic points from this case include:
• Stress is a known trigger for psoriasis vulgaris.
• The patient’s nails failed to respond to terbinafine treatment.
• There was no obvious source of fungal infection (eg, contact with animals) or reason for him to have a yeast infection (eg, diabetes) or develop mold “infection” in the nails (eg, trauma from digging in soil).
• Fungal infections are about 18 times less likely to occur in the fingernails than in the toenails.
• A unifying explanation for simultaneous nail and skin changes was needed.
• The nail and skin changes seen here are quite typical for psoriasis.
Most important, though, is the need to overcome the urge to hop on the “fungal bandwagon” by first considering other diagnostic possibilities.
Continue for the treatment of this condition >>
TREATMENT
Unfortunately, there is no good treatment for this patient’s nails. However, there is an excellent chance that his scalp psoriasis will respond to short-term use of fluocinolone 0.05% cream.
This patient was also counseled about the role of stress in his condition and the benefits of modest increases in UV exposure. During follow-up, it will be important to ask about joint pain, since up to 30% of psoriasis patients will eventually develop psoriatic arthritis.
If the patient’s current treatment does not produce sufficient results, other options include calcipotriene ointment, oral methotrexate, or even one of the biologics (etanercept or adalimumab).
ANSWER
The correct answer is psoriasis (choice “d”), which often involves nail and skin changes such as those seen in this case. There was no particular reason to think this patient had an infection of any kind, but, as is often the case, the original provider considered only one diagnostic possibility.
DISCUSSION
Nail disease can be problematic for both patient and provider. Arguably the biggest issue with it, initially, is “the one-item differential”—the idea that all nail disease can be classified as “fungal infection” simply because neither the patient nor the provider considers any other explanation for the changes seen. This case illustrates that dilemma nicely.
Psoriasis affects more than 2% of the US population, making it a common skin disorder. As this case illustrates, it may affect several areas with diverse but predictable morphologic presentations, all appearing at the same time.
The key diagnostic points from this case include:
• Stress is a known trigger for psoriasis vulgaris.
• The patient’s nails failed to respond to terbinafine treatment.
• There was no obvious source of fungal infection (eg, contact with animals) or reason for him to have a yeast infection (eg, diabetes) or develop mold “infection” in the nails (eg, trauma from digging in soil).
• Fungal infections are about 18 times less likely to occur in the fingernails than in the toenails.
• A unifying explanation for simultaneous nail and skin changes was needed.
• The nail and skin changes seen here are quite typical for psoriasis.
Most important, though, is the need to overcome the urge to hop on the “fungal bandwagon” by first considering other diagnostic possibilities.
Continue for the treatment of this condition >>
TREATMENT
Unfortunately, there is no good treatment for this patient’s nails. However, there is an excellent chance that his scalp psoriasis will respond to short-term use of fluocinolone 0.05% cream.
This patient was also counseled about the role of stress in his condition and the benefits of modest increases in UV exposure. During follow-up, it will be important to ask about joint pain, since up to 30% of psoriasis patients will eventually develop psoriatic arthritis.
If the patient’s current treatment does not produce sufficient results, other options include calcipotriene ointment, oral methotrexate, or even one of the biologics (etanercept or adalimumab).

After finishing a month-long course of terbinafine (250 mg), a 27-year-old man is dismayed to see that the fingernail changes he first noted a year ago have not improved. He had been told in no uncertain terms by his primary care provider that his fingernail condition—and accompanying scalp rash—represented fungal infection. When topical antifungal creams failed to help his scalp condition, the oral medication was prescribed. Now it, too, appears to have been unhelpful. At this point, the patient requests referral to dermatology. His primary concern is that he represents a “contagious threat” to his wife and children, although none of them has shown any signs of this condition. The patient denies any skin problems prior to the nail changes and the scalp rash that manifested shortly afterward, which occurred more than a year ago. Shortly before the onset of these problems, he lost his job and had to replace it with two lower-paying part-time jobs. He denies any family history of skin disease or joint pain. There are no new pets in the house, and the patient does not work with animals. Examination reveals that the distal portions of all 10 fingernails are uniformly dystrophic and mildly onycholytic and have numerous longitudinal dark streaks. Several fingernails also have tiny scattered pits in them. The toenails are unaffected. Elsewhere, the man is observed to have salmon-pink scaly patches on the scalp and over both ears, and smaller, round plaques on the forehead, with prominent white tenacious scale. KOH prep of these latter lesions is negative for fungal elements.