User login
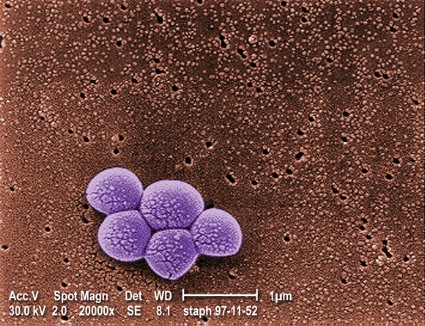
SAN DIEGO – Polymerase chain reaction testing recovered methicillin-resistant Staphylococcus aureus significantly more frequently than did nasal swab culture in hospitalized patients receiving antibiotics concurrently, a study has shown.
All of the patients studied had a history of MRSA colonization. "Because close to 50% of hospitalized patients receive antibiotics, it’s important to know whether or not your MRSA screening test is going to be accurate in detecting persistent colonization," Dr. Erica S. Shenoy said in an interview during a poster session at IDWeek, the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Dr. Shenoy of Massachusetts General Hospital’s division of infectious diseases and infection control unit, Boston, and her associates compared the effect of concurrent administration of antibiotics with activity against MRSA on detection from nasal surveillance swabs. The study population included 259 patients who were admitted to Massachusetts General Hospital between Dec. 6, 2010, and Sept. 16, 2011, with a history of MRSA colonization, but no culture more recent than 90 days who underwent simultaneous screening for nasal carriage of MRSA with both culture and commercial PCR testing. Samples obtained within 2 days after administration of select antibiotics were considered to be obtained in the presence of "concurrent antibiotics." The list of select antibiotics included trimethoprim/sulfamethoxazole, mupirocin, ciprofloxacin, clindamycin, daptomycin, doxycycline, levofloxacin, linezolid, nitrofurantoin, quinupristin/dalfopristin, rifampin, tetracycline, tigecycline, and intravenous vancomycin.
Dr. Shenoy reported that 132 of the 259 paired samples were obtained in the presence of antibiotics while the remaining 127 were not. In the absence of antibiotics, the concordance rate between culture and PCR was 94%, with neither test being significantly more likely to yield a positive result. However, in the presence of antibiotics, the concordance rate between paired samples was 91%, with a significantly greater tendency for PCR to yield positive results compared with culture, suggesting to the researchers better performance of PCR testing in the setting of antibiotic exposure.
"These findings are important for clinicians and hospitals interested in an efficient approach to determining colonization status," Dr. Shenoy said. "In populations exposed to antibiotics with activity against MRSA, culture assays may miss true positives."
She emphasized that while PCR is more expensive than nasal swab culture on a per-test basis, the "cost of the capital equipment investment and the personnel time to actually do the swabbing is potentially dwarfed by the downstream impact on the patient and the hospital overall." For example, studies have shown that inpatients on contact precautions "see their doctors fewer times, have more preventable adverse events, and more dissatisfaction with care, and thus we should strive to only place patients on contact precautions if they remain colonized," Dr. Shenoy said. "In an ongoing pilot study at our institution, we’ve transitioned to using PCR to document clearance and discontinue contact precautions in eligible patients."
In their poster, the researchers acknowledged certain limitations of the study, including its single-center design and the fact that "it was not possible to randomize subjects in the study to receipt or nonreceipt of antibiotics, and thus we do not know if subjects in both groups differed on unobservable characteristics."
The study was supported by a 2010 Massachusetts General Hospital Clinical Innovation Award, a National Institute of Allergy and Infectious Diseases Training Grant, the Harvard Catalyst, and Harvard University. Cepheid provided reagents and a loaner GeneXpert for the randomized trial free of charge. Dr. Shenoy said she and her associates had no relevant financial conflicts to disclose.
SAN DIEGO – Polymerase chain reaction testing recovered methicillin-resistant Staphylococcus aureus significantly more frequently than did nasal swab culture in hospitalized patients receiving antibiotics concurrently, a study has shown.
All of the patients studied had a history of MRSA colonization. "Because close to 50% of hospitalized patients receive antibiotics, it’s important to know whether or not your MRSA screening test is going to be accurate in detecting persistent colonization," Dr. Erica S. Shenoy said in an interview during a poster session at IDWeek, the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Dr. Shenoy of Massachusetts General Hospital’s division of infectious diseases and infection control unit, Boston, and her associates compared the effect of concurrent administration of antibiotics with activity against MRSA on detection from nasal surveillance swabs. The study population included 259 patients who were admitted to Massachusetts General Hospital between Dec. 6, 2010, and Sept. 16, 2011, with a history of MRSA colonization, but no culture more recent than 90 days who underwent simultaneous screening for nasal carriage of MRSA with both culture and commercial PCR testing. Samples obtained within 2 days after administration of select antibiotics were considered to be obtained in the presence of "concurrent antibiotics." The list of select antibiotics included trimethoprim/sulfamethoxazole, mupirocin, ciprofloxacin, clindamycin, daptomycin, doxycycline, levofloxacin, linezolid, nitrofurantoin, quinupristin/dalfopristin, rifampin, tetracycline, tigecycline, and intravenous vancomycin.
Dr. Shenoy reported that 132 of the 259 paired samples were obtained in the presence of antibiotics while the remaining 127 were not. In the absence of antibiotics, the concordance rate between culture and PCR was 94%, with neither test being significantly more likely to yield a positive result. However, in the presence of antibiotics, the concordance rate between paired samples was 91%, with a significantly greater tendency for PCR to yield positive results compared with culture, suggesting to the researchers better performance of PCR testing in the setting of antibiotic exposure.
"These findings are important for clinicians and hospitals interested in an efficient approach to determining colonization status," Dr. Shenoy said. "In populations exposed to antibiotics with activity against MRSA, culture assays may miss true positives."
She emphasized that while PCR is more expensive than nasal swab culture on a per-test basis, the "cost of the capital equipment investment and the personnel time to actually do the swabbing is potentially dwarfed by the downstream impact on the patient and the hospital overall." For example, studies have shown that inpatients on contact precautions "see their doctors fewer times, have more preventable adverse events, and more dissatisfaction with care, and thus we should strive to only place patients on contact precautions if they remain colonized," Dr. Shenoy said. "In an ongoing pilot study at our institution, we’ve transitioned to using PCR to document clearance and discontinue contact precautions in eligible patients."
In their poster, the researchers acknowledged certain limitations of the study, including its single-center design and the fact that "it was not possible to randomize subjects in the study to receipt or nonreceipt of antibiotics, and thus we do not know if subjects in both groups differed on unobservable characteristics."
The study was supported by a 2010 Massachusetts General Hospital Clinical Innovation Award, a National Institute of Allergy and Infectious Diseases Training Grant, the Harvard Catalyst, and Harvard University. Cepheid provided reagents and a loaner GeneXpert for the randomized trial free of charge. Dr. Shenoy said she and her associates had no relevant financial conflicts to disclose.
SAN DIEGO – Polymerase chain reaction testing recovered methicillin-resistant Staphylococcus aureus significantly more frequently than did nasal swab culture in hospitalized patients receiving antibiotics concurrently, a study has shown.
All of the patients studied had a history of MRSA colonization. "Because close to 50% of hospitalized patients receive antibiotics, it’s important to know whether or not your MRSA screening test is going to be accurate in detecting persistent colonization," Dr. Erica S. Shenoy said in an interview during a poster session at IDWeek, the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Dr. Shenoy of Massachusetts General Hospital’s division of infectious diseases and infection control unit, Boston, and her associates compared the effect of concurrent administration of antibiotics with activity against MRSA on detection from nasal surveillance swabs. The study population included 259 patients who were admitted to Massachusetts General Hospital between Dec. 6, 2010, and Sept. 16, 2011, with a history of MRSA colonization, but no culture more recent than 90 days who underwent simultaneous screening for nasal carriage of MRSA with both culture and commercial PCR testing. Samples obtained within 2 days after administration of select antibiotics were considered to be obtained in the presence of "concurrent antibiotics." The list of select antibiotics included trimethoprim/sulfamethoxazole, mupirocin, ciprofloxacin, clindamycin, daptomycin, doxycycline, levofloxacin, linezolid, nitrofurantoin, quinupristin/dalfopristin, rifampin, tetracycline, tigecycline, and intravenous vancomycin.
Dr. Shenoy reported that 132 of the 259 paired samples were obtained in the presence of antibiotics while the remaining 127 were not. In the absence of antibiotics, the concordance rate between culture and PCR was 94%, with neither test being significantly more likely to yield a positive result. However, in the presence of antibiotics, the concordance rate between paired samples was 91%, with a significantly greater tendency for PCR to yield positive results compared with culture, suggesting to the researchers better performance of PCR testing in the setting of antibiotic exposure.
"These findings are important for clinicians and hospitals interested in an efficient approach to determining colonization status," Dr. Shenoy said. "In populations exposed to antibiotics with activity against MRSA, culture assays may miss true positives."
She emphasized that while PCR is more expensive than nasal swab culture on a per-test basis, the "cost of the capital equipment investment and the personnel time to actually do the swabbing is potentially dwarfed by the downstream impact on the patient and the hospital overall." For example, studies have shown that inpatients on contact precautions "see their doctors fewer times, have more preventable adverse events, and more dissatisfaction with care, and thus we should strive to only place patients on contact precautions if they remain colonized," Dr. Shenoy said. "In an ongoing pilot study at our institution, we’ve transitioned to using PCR to document clearance and discontinue contact precautions in eligible patients."
In their poster, the researchers acknowledged certain limitations of the study, including its single-center design and the fact that "it was not possible to randomize subjects in the study to receipt or nonreceipt of antibiotics, and thus we do not know if subjects in both groups differed on unobservable characteristics."
The study was supported by a 2010 Massachusetts General Hospital Clinical Innovation Award, a National Institute of Allergy and Infectious Diseases Training Grant, the Harvard Catalyst, and Harvard University. Cepheid provided reagents and a loaner GeneXpert for the randomized trial free of charge. Dr. Shenoy said she and her associates had no relevant financial conflicts to disclose.
AT IDWEEK